Abstract
Background.
Positive patient–provider relationships have been associated with improved depression treatment outcomes. Little is known about how patient treatment beliefs influence patient–provider relationships, specifically treatment alliance and shared decision making in primary care (PC).
Objective.
We evaluated the relationship between patient treatment beliefs and patient–provider relationships by gender, race and current depression.
Methods.
We used a deductive parallel convergent mixed method design with cross-sectional data. Participants were 227 Black and White patients presenting with depression symptoms in PC settings. Individuals were randomized into either a quantitative survey (n = 198) or qualitative interview (n = 29) group. We used multiple ordinary least squares regression to evaluate the association between patient beliefs, as measured by the Treatment Beliefs Scale and the Medication Beliefs Scale, and treatment alliance or shared decision making. We concurrently conducted thematic analyses of qualitative semistructured interview data to explicate the nature of patient–provider relationships.
Results.
We found that patients who believed their provider would respectfully facilitate depression treatment reported greater bond, openness and shared decision making with their provider. We also identified qualitative themes of physicians listening to, caring about and respecting patients. Empathy and emotive expression increased patient trust in PC providers as facilitators of depression treatment.
Conclusions.
This work systematically demonstrated what many providers anecdotally believe: PC environments in which individuals feel safe sharing psychological distress are essential to early identification and treatment of depression. Interprofessional skills-based training in attentiveness and active listening may influence the effectiveness of depression intervention.
Key words. Depression/mood disorders, doctor–patient relationship, health disparities, primary care, quality of care.
Introduction
In the psychotherapeutic relationship, as theorized by Bordin (1), the treatment alliance between a provider and individual consists of tasks (what needs to be done to reach a goal), goals (what the individual hopes to gain) and bond (formed from the belief that the task will bring the individual closer to achieving those goals). Although less understood in the context of physicians and patients, the patient–provider relationship, through the collaborative bond and shared decision making regarding depression treatment (treatment alliance), is a predictor of better treatment engagement, adherence and outcomes in psychotherapy (2). Although providers may anecdotally identify factors that influence provider–patient relationship quality, how these relationships influence identification and use of mental health services in primary care (PC) is largely unexplored (3). Importantly, preliminary studies have suggested that factors in the patient–provider relationship may be as predictive of depression outcomes as treatment condition (psychotherapy, antidepressants, pill placebo) in PC (4). The aims of this work were to examine how (i) patient beliefs about depression treatment and (ii) provider qualities influence treatment alliance and shared decision making. Findings can inform PC depression screening, treatment planning and care management and improve depression outcomes in PC.
PC providers are often the first point of contact for the identification of mental distress in patients. Provider qualities have been identified as facilitating comfort on the part of the patient in disclosing their mental distress. Patients value certain provider attributes including professional expertise, patience, attentiveness, communication, representing client interests, truthfulness and respecting client preferences, with respect for patient autonomy most valued (5). Patients have identified communication (listening, partnership, information sharing) and personality and demeanour (friendliness, caring, supportiveness) as attributes of excellent providers (6). Providers’ gender and race may also affect patient–provider relationships. Female providers are more likely to explore a patient’s experience of symptoms and disease and provide a more satisfying experience, whereas male providers attempt to understand the person in their environment and are perceived to be more thorough in assessment (7). Different racial and ethnic groups may have different health decision-making processes (8). Although patient–provider race concordance may influence treatment alliance (9), it has not been found to affect respect or agreement regarding the aetiology of symptoms (10). Although some of these qualities are innate to the individual provider, others can be learned by emphasizing their identification for the training of future physicians.
Task, bond and goals also appear to influence the physician–patient relationship (1). However, the identified physician qualities merely facilitate the disclosure and possible acceptance of mental health diagnosis; other barriers may influence treatment. For example, patient beliefs about depression treatment affect patient–provider relationships; treatment effectiveness beliefs are crucial to treatment acceptance (11) and successful engagement in therapy (4) and are predictive of clinical improvement (12). This study explores what is less known—how patient beliefs about depression treatment affect patient–provider relationships in treatment of depression by PC physicians. Understanding both provider qualities and patient beliefs may help to better identify methods of engaging individuals experiencing mental distress in treatment.
Methods
Design
In this convergent parallel mixed method study (13) of cross-sectional survey and interview data, we evaluated the relationships between (i) patient beliefs and (ii) patient–provider relationships. Patient beliefs included (i) treatment and (ii) provider characteristics. Patient–provider relationships included (i) treatment alliance and (ii) shared decision making. Mixed methods were selected to triangulate quantitative data on patient beliefs regarding treatment with qualitative reports of patient beliefs related to provider characteristics. We used baseline data from an NIMH-funded R01 study examining the role of patient factors in establishing treatment alliance in the identification and treatment of depression in PC settings.
Quantitative
Measures
Surveys were used to evaluate whether patient beliefs about depression treatment were associated with patient–provider relationships. We hypothesized that beliefs that depression was an illness, the provider could help facilitate depression treatment, and counseling and medication could help treat depression would be associated with increased treatment alliance and shared decision making, whereas belief that God played a role in depression treatment would be associated with decreased treatment alliance and shared decision making. The 198 participants in the quantitative arm also completed a diagnostic interview based on the Structured Clinical Interview for DSM-IV and questionnaire.
Patient–provider relationships
The Agnew Relationship Measure (ARM) of treatment alliance (14) measured patient–provider relationships. The four subscales of the ARM measured bond with provider (ARM-Bond); confidence in provider (ARM-Conf); openness with provider (ARM-Open) and initiative in interactions with provider (ARM-Init). The ARM-Init subscale was omitted from the analysis because it did not meet minimum criteria for reliability (internal consistency less than 0.70). The Goldring Patient–Provider Scale of shared decision making (13) also measured patient–provider relationships. Confirmatory factor analysis suggested elimination of 2 of the 12 items for unidimensionality, resulting in a 10-item measure.
Patient beliefs
The Treatment Beliefs Scale (TBS) is a measure developed by the last author and tested in previous depression studies (Table 1) (15) that reflects a range of treatment beliefs affecting patient decisions regarding depression treatment (16). The four subscales of the TBS measured patient beliefs that God and faith play a role in depression treatment (TBS-God); depression is an illness (TBS-Dep); the provider believes the patient and can be trusted with depression treatment (TBS-Pro) and counselling is an effective treatment for depression (TBS-Cou). The TBS-Dep and TBS-Cou subscales were omitted from the analysis because they did not meet minimum criteria for reliability.
Table 1.
Treatment Beliefs Scale
| Provider believes patient and can be trusted with depression treatment—subscale (4 items): 1. I trust my primary care provider to act in my best interest. 2. My primary care provider listens to me. 3. My primary care provider recognizes when something is wrong with me emotionally. 4. My primary care provider believes my symptoms are real. Counselling is an effective treatment for depression—subscale (6 items): 5. If I were depressed, counselling would restore me to my usual level of functioning. 6. Counselling would help me just as much as antidepressants if I had depression. 7. I can afford treatment for mental health. 8. I have health insurance that will cover the costs of any mental health needs. 9. Talking about stress or emotional problems with a professional can be helpful. 10. People with depression do not need professional care. God and faith play a role in depression treatment—subscale (4 items): 11. Faith in God will heal my depression. 12. Prayer alone can heal depression. 13. Thanking God helps depression get better. 14. Asking God for forgiveness will help heal my depression. Depression is an illness—subscale (6 items) 15.If I had depression, an antidepressant would restore me to my normal levels of functioning. 16.People who have depression are not to blame. 17.Anyone can suffer from depression. 18.Depression is usually a sign of weakness of failure. 19.I would be embarrassed if others knew that I was getting help for depression. 20.I would not tell someone if I were depressed. MBS 1. Medication for depression is not the answer to problems in one’s life. 2. Medication for depression is a crutch. 3. I should be able to get by without medication for depression. 4. Antidepressants are not addictive. 5. My family would be supportive of me taking antidepressants for emotional problems. 6. I would not be able to work if I took medication for depression. 7. Medications for depression are overused. 8. Medication for depression should not be taken long-term. 9. Drugs providers prescribe for depression are safe. 10. Antidepressant medications are helpful for treating emotional problems. 11. Natural approaches to depression, such as exercise, nutrition and relaxation, are better than taking medications. 12. Medication for depression can prevent future emotional problems. 13. I would be embarrassed if my friends knew that I was taking medication for depression. 14. If I had depression, I think that an antidepressant would help me. 15. St. John’s Wort or other herbal remedies are useful for treating depression. |
The Medication Beliefs Scale (MBS) is another measure developed by the last author and tested in previous depression studies (Table 1) (15) that reflects a range of medication beliefs affecting patient decisions regarding depression treatment (16). The 12-item MBS was used to measure patient perceptions of the acceptability, role, safety and effectiveness of antidepressant medication.
All measures were rated on Likert Scales with response values summed for a total score. If participants responded to 75% or more of the measure items, we used an adjusted average score based on the available item responses; otherwise, the observation was treated as missing.
Analysis
We calculated Pearson’s product–moment correlations to evaluate the univariate relationships of all measures. We conducted multiple iterations of multiple regression or multiple ordinary least squares regressions in SAS Enterprise Guide 4.3 after comprehensive regression diagnostics to explore the relationship between patient treatment beliefs and patient–provider relationships. We added race, gender and current depression diagnosis as potential moderators. Multiple ordinary least squares regression models featured (i) all patient beliefs; (ii) patient beliefs with significant main effects; (iii) significant main effects, all potential moderators, and all potential interaction effects and (iv) significant main and interaction effects. We included moderators with significant main effects by moderator group in final models. Models and parameters were evaluated at a 0.05 significance level.
Qualitative
Measures
To complement quantitative findings and explicate the nature of the patient–provider relationship, the study team conducted semistructured interviews. The 29 participants completed interviews in their homes or a private university location. The interviews were designed to explore the experience of living with depression, anxiety, or both; coping strategies; medical provider qualities and interactions; and social support. The semistructured script was developed as a guide for both the facilitator and the interviewees (17). Interviews were conducted by four individuals (all women): two sociologists (five interviews each), one anthropologist (four interviews) and one social worker (15 interviews). All participants provided written consent prior to the interview.
Analysis
A professional transcriptionist transcribed all audio files verbatim. The second and third authors and a paid master’s-level social work student trained by the second author analysed the data. The research team discussed and adjusted the final code list to reduce overlap of concepts in codes; multiple research team members strengthen qualitative analyses because they have different ways of approaching the same subject results, which provides increased understanding of data and reduces bias (18). Atlas.ti was used to organize and code the data. Transcripts were reviewed and coded into specific and general themes using a deductive approach; qualitative concepts were used because our themes and codes were derived from concepts in the quantitative questions. Topics and themes were evaluated and further refined. Thematic analysis was used to guide data reduction, coding and construction of themes (19). Coding was systematic and sequential (17).
Integration
Quantitative and qualitative findings were compared to develop a comprehensive understanding of the role of patient beliefs about depression treatment and provider characteristics in establishing treatment alliance and shared decision making (20). Triangulation (21) is the use of comparative views to ensure both saturation and multiple perspectives occurred at the data, investigator and analyses levels by collecting multiple points of data from the larger pool of quantitative respondents and comparing different points of view across various patient types. Integrated results that capture survey data on patient beliefs are compared with qualitative views on how these beliefs affect patient perceptions and actions.
Results
Sample
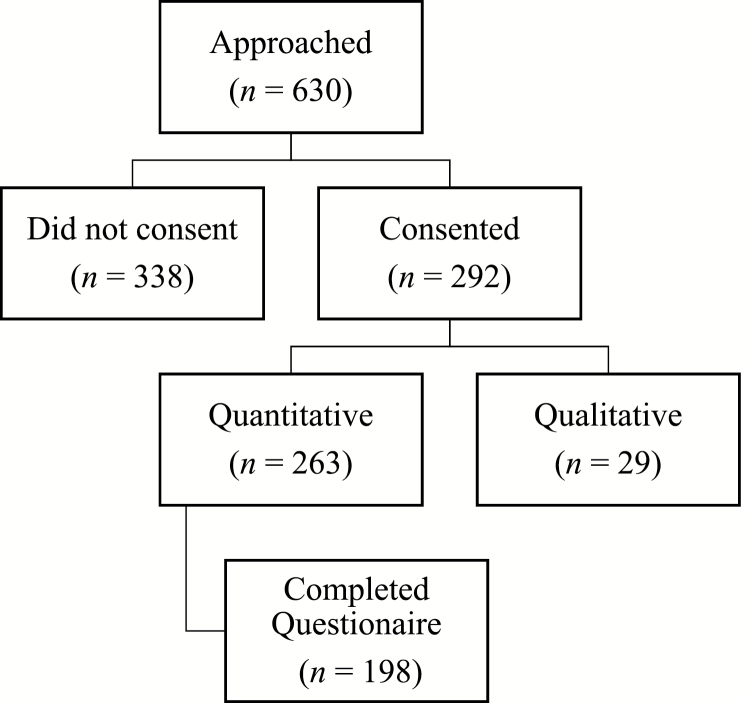
Study staff approached PC patients based on references to depression found in a review of the medical charts of 70 participating PC doctors. Of the 630 Black or White patients approached, 292 consented to participate; of those consenting, 263 were randomly assigned to the quantitative arm and 29 to the qualitative arm (Fig. 1). Consenters were more likely to be White. Of the 263 participants in the quantitative arm, 198 completed the mail-back questionnaire, including the patient belief and treatment alliance data used in this analysis. Questionnaire respondents were more likely to have insurance than non-respondents.
Figure 1.
Sampling flow diagram.
Quantitative
The final sample featured 227 Black and White individuals. A majority of participants were White, female and reported some college education. Nearly half were 45–64 years old, and slightly more than half of those in the quantitative arm had a diagnosis of major or minor depression (Table 2).
Table 2.
Black and White primary care patient demographics by study arm at baseline
| Variable | Quantitative (n = 198) | Qualitative (n = 29) | Total (N = 227) | |||
|---|---|---|---|---|---|---|
| n | % | n | % | n | % | |
| Age | ||||||
| 20–44 | 73 | 37 | 8 | 25 | 81 | 36 |
| 45–64 | 97 | 49 | 13 | 45 | 110 | 48 |
| 65+ | 27 | 14 | 3 | 10 | 30 | 13 |
| Missing | 1 | 1 | 4 | 14 | 5 | 2 |
| Gender | ||||||
| Female | 159 | 80 | 24 | 83 | 183 | 81 |
| Male | 39 | 20 | 5 | 17 | 44 | 19 |
| Race | ||||||
| Black | 88 | 44 | 16 | 55 | 104 | 46 |
| White | 110 | 56 | 13 | 45 | 123 | 54 |
| Marital status | ||||||
| Single | 76 | 38 | 11 | 38 | 87 | 38 |
| Married | 65 | 33 | 8 | 28 | 73 | 32 |
| Separated, divorced, widowed | 56 | 28 | 6 | 21 | 62 | 27 |
| Missing | 1 | 1 | 4 | 14 | 5 | 2 |
| Education | ||||||
| < High school | 24 | 12 | 3 | 10 | 27 | 12 |
| High school | 40 | 20 | 5 | 17 | 45 | 20 |
| Some college | 66 | 33 | 5 | 17 | 71 | 31 |
| College+ | 65 | 33 | 11 | 38 | 76 | 33 |
| Missing | 3 | 2 | 4 | 14 | 7 | 3 |
| Income | ||||||
| < $20000 | 58 | 29 | 7 | 24 | 65 | 29 |
| $20000–$49999 | 76 | 38 | 11 | 38 | 87 | 38 |
| $50000–$99999 | 34 | 17 | 3 | 10 | 37 | 16 |
| $100000+ | 21 | 11 | 2 | 7 | 23 | 10 |
| Missing | 9 | 5 | 4 | 14 | 13 | 6 |
| Employment | ||||||
| Full- or part-time | 94 | 47 | 8 | 28 | 102 | 45 |
| Student, homemaker, retired | 43 | 22 | 6 | 21 | 49 | 22 |
| Unemployed | 24 | 12 | 4 | 14 | 28 | 12 |
| Disabled | 36 | 18 | 6 | 21 | 42 | 19 |
| Missing | 1 | 1 | 4 | 14 | 5 | 2 |
| Insurance | ||||||
| Public | 39 | 20 | 8 | 28 | 47 | 21 |
| Private | 153 | 77 | 15 | 52 | 168 | 74 |
| None | 3 | 2 | 1 | 3 | 4 | 2 |
| Missing | 3 | 2 | 4 | 14 | 7 | 3 |
| Current depression | ||||||
| None | 93 | 47 | 93 | 41 | ||
| Minor | 21 | 11 | 21 | 9 | ||
| Major | 84 | 42 | 84 | 37 | ||
There were no significant (at P < 0.05) demographic differences between study arms.
Means, standard deviations, and minimum and maximum scores for all measures appear in Table 3. All subscales were interval-level measures with mild negative skew due to the presence of outliers. Spearman’s non-parametric correlations were consistent with Pearson’s product–moment correlations presented in Table 4.
Table 3.
Means, standard deviations and minimum and maximum scores for patient belief and treatment alliance measures for quantitative arm participants (n = 198)
| Measure | Items | Measure range | n | α | M | SD | Min | Max |
|---|---|---|---|---|---|---|---|---|
| MBS | 12 | 12–60 | 198 | 0.80 | 38 | 8 | 12 | 53 |
| TBS-God | 4 | 4–20 | 197 | 0.92 | 11 | 4 | 4 | 20 |
| TBS-Depressiona | 6 | 6–30 | 198 | 0.53 | 23 | 3 | 12 | 30 |
| TBS-Provider | 4 | 4–20 | 198 | 0.80 | 17 | 2 | 9 | 20 |
| TBS-Counsellinga | 6 | 6–30 | 198 | 0.52 | 21 | 3 | 12 | 30 |
| ARM-Bond | 6 | 6–30 | 196 | 0.83 | 26 | 3 | 14 | 30 |
| ARM-Confidence | 7 | 7–35 | 193 | 0.80 | 29 | 4 | 16 | 35 |
| ARM-Openness | 5 | 5–25 | 197 | 0.76 | 19 | 3 | 8 | 25 |
| ARM-Initiativea | 4 | 4–20 | 194 | 0.42 | 11 | 2 | 4 | 19 |
| GPPS | 10 | 10–50 | 197 | 0.89 | 39 | 6 | 21 | 50 |
GPPS, Goldring Patient–Provider Scale.
aSubscales with α < 0.70 were omitted from the analysis because they did not meet minimum criteria for reliability and any results including these scales would not be confidently interpreted.
Table 4.
Pearson’s r intercorrelations between patient belief and treatment alliance measures
| TBS-God | TBS-Provider | ARM-Bond | ARM-Confidence | ARM-Openness | GPPS | |
|---|---|---|---|---|---|---|
| MBS | −0.22 | 0.06 | −0.00 | 0.10 | 0.15 | 0.11 |
| TBS-God | −0.09 | −0.03 | −0.12 | −0.03 | −0.09 | |
| TBS-Provider | 0.66 | 0.75 | 0.48 | 0.66 | ||
| ARM-Bond | 0.79 | 0.52 | 0.59 | |||
| ARM-Confidence | 0.61 | 0.66 | ||||
| ARM-Open | 0.41 |
Figures in boldface are significant at P < 0.05. GPPS, Goldring Patient–Provider Scale.
Univariate analysis showed the more patients believed their provider could facilitate depression treatment—one aspect of patient treatment beliefs—the more open they were, the closer they felt, and the more confident they felt with the provider’s abilities to help them with their depression. Patients who believed medication would treat their depression also were more open with their providers. The ARM-Conf subscale was eliminated from further analysis due to its very high correlation (r ≥ 0.70) with the TBS-Pro and ARM-Bond subscales.
During the regression analysis, comprehensive diagnostics identified a few cases of potentially influential data for each regression model given their concurrently high-studentized residuals and leverage. Regression models were rerun without these potentially influential observations and the results were consistent (Table 5). Two aspects of treatment beliefs, patient beliefs that (i) their provider believed their depression symptoms were real and (ii) the provider could be trusted to facilitate depression treatment, significantly predicted all three measured components of patient–provider relationships: (i) bond, (ii) openness, and (iii) shared decision making. Current depression and the interaction of current depression with one aspect of treatment beliefs, belief in the provider as a facilitator of depression treatment, were only predictive of one component of patient–provider relationships, client openness with the provider.
Table 5.
Summary of multiple ordinary least squares regression analysis predicting treatment alliance subscale from patient beliefs
| Model | ARM-Bond | GPPS | ARM-Open | |||
|---|---|---|---|---|---|---|
| B | P | B | P | B | P | |
| Models with all treatment beliefs |
R
2 = 0.43 F(3, 191) = 47 P < 0.001 |
R
2 = 0.44 F(3, 191) = 48 P < 0.001 |
R
2 = 0.25 F(3, 192) = 21 P < 0.001 |
|||
| TBS-Provider | 0.90 | <0.001 | 1.49 | <0.001 | 0.65 | <0.001 |
| TBS-God | 0.02 | 0.691 | −0.02 | 0.751 | 0.05 | 0.414 |
| MBS | −0.00 | 0.918 | 0.03 | 0.562 | 0.09 | 0.025 |
| Models with significant treatment beliefs only |
R
2 = 0.44 F(1, 196) = 152 P < 0.001 |
R
2 = 0.44 F(1, 196) = 153 P < 0.001 |
R
2 = 0.24 F(2, 193) = 31 P < 0.001 |
|||
| TBS-Provider | 0.91 | <0.001 | 1.54 | <0.001 | 0.68 | <0.001 |
| MBS | 0.05 | 0.122 | ||||
| Models with potential moderators and interactions |
R
2 = 0.45 F(7, 196) = 22 P < 0.001 |
R
2 = 0.45 F(7, 196) = 22 P < 0.001 |
R
2 = 0.30 F(7, 197) = 12 P < 0.001 |
|||
| TBS-Provider | 0.92 | 0.001 | 1.50 | <0.001 | 0.40 | 0.072 |
| Depression | 0.35 | 0.892 | −2.56 | 0.562 | −6.84 | 0.290 |
| TBS-Provider × depression | −0.00 | 0.990 | 0.17 | 0.509 | 0.44 | 0.153 |
| Gender | −2.69 | 0.416 | 2.45 | 0.661 | −3.04 | 0.441 |
| TBS-Provider × gender | 0.15 | 0.434 | −0.08 | 0.797 | 0.07 | 0.723 |
| Race | 5.34 | 0.516 | −0.49 | 0.915 | −0.05 | 0.988 |
| TBS-Provider × race | −0.31 | 0.536 | 0.06 | 0.811 | 0.02 | 0.919 |
| Models with significant moderators and interactions |
R
2 = 0.44 F(1, 196) = 152 P < 0.001 |
R
2 = 0.44 F(1, 196) = 153 P < 0.001 |
R
2 = 0.26 F(3, 197) = 22 P < 0.001 |
|||
| TBS-Provider | 0.91 | <0.001 | 1.54 | <0.001 | 0.49 | <0.001 |
| Depression | −6.24 | 0.046 | ||||
| TBS-Provider × depression | 0.41 | 0.025 | ||||
Figures in boldface are significant at P < 0.05. B values for depression, gender, race and their related interactions were not interpreted as standard regression coefficients for categorical variables. See results narrative for additional explanation. GPPS, Goldring Patient–Provider Scale.
To further explore this interaction, we conducted regression analyses for openness with provider by current depression status, with patient treatment beliefs that the provider believed their symptoms and could facilitate depression treatment as the sole predictor. For patients with no current depression, belief that the provider could facilitate depression treatment predicted openness (explaining 39% of the variance). A similar effect was found for patients with current depression (explaining 12% of the variance). Current depression decreased but did not eliminate the predictive effect of patient beliefs that the provider could facilitate treatment on their openness with the provider, one component of patient–provider relationships.
Qualitative
Interviews with participants were audio recorded and each lasted from 45 to 90 minutes. Deductive analyses of transcripts resulted in two themes: (i) comfort and caring and (ii) empathy and respect.
Comfort and caring
Some individuals discussed how they had engaged with several providers before they settled on their current provider. Participants felt most connected to physicians whom they believed were good listeners and whom they perceived cared about them. Most individuals discussed the concept of feeling ‘heard’ and often described this concept as the physician being a good listener, explaining that feeling heard overwhelmingly contributed to their positive feelings towards the provider. One respondent said, ‘He listen[s] and he just, he has a feel about him to where it makes you feel as though it’s just not that bad. He gives you that hopefulness … you know, that, OK, we are going to get through this’.
Patients said they most wanted to be heard and understood. One participant’s statement sums up this sentiment: ‘The fact that she listened, her feedback. The answer that she gave me indicated that she wasn’t just brushing me off’. Because of the nature of mental illness and the complexity of diagnosis and treatment, many participants noted it was difficult to find a provider who would simply listen to what they were saying. Overall, listening provided an avenue to feeling heard and care for, increasing comfort with the provider.
Individuals repeatedly highlighted comfort as a key element of provider–patient relationships. Ease was expressed in various ways. One participant noted, ‘It makes people more comfortable with her because she just sits right down and just starts chatting with as if she was just anybody. I mean … she doesn’t come in and act all “doctorlike,” very stiff and very formal’. Another respondent described a different physician:
She make[s] me feel very comfortable and I could trust her with what I tell her. She was really concerned. She laid back and listened to me. Like I told her stories of things I went through growin’ up and stuff. I mean, she’s my primary doctor and to me, that what they’s suppose to do and to me, that’s what she did.
When participants felt heard and were approached in a manner that increased patient–provider mutuality, they said they felt more connected to providers, increasing their alliance and supporting continued provider–patient engagement, which is crucial to retaining patients in care.
Empathy and respect
Participants also said they viewed empathy and respect as important provider qualities. One participant said a doctor should be ‘not only a good listener, [but also] understanding … be open minded’. Another respondent said:
Because she was listening, looking at me, stopped writing, and responds to whatever I was sayin’ to her … get outta here … really? “Sounds like you had a difficult life” … you know? And whatever I said to her she was fine, like, with another question or … she responded, is what it was.
Feeling respected was often equated with being given the time participants felt they needed with the provider. As one person explained, ‘You are a patient, not just a number, not just another fifty dollars to Dr. [name]. He cares about you, feels like you’re a person’. Another person echoed this sentiment when speaking about a different provider:
I think it’s the way that she comes in and the way she looks right at you when she walks in the door and the way she actually knows your name. … You know, you don’t hear her mumbling to the nurse outside.
Several individuals described how the qualities and actions of providers indicated how much respect they have for patients. One person stated, ‘You can tell pretty quickly whether or not they’re gonna be able to go there and think about me in a holistic sense and see me as a whole person, not whether or not I’m being checked off’. Being cognizant of not being ‘too mechanical’, not making patients ‘feel like a number’ and exhibiting empathy and compassion were important qualities of providers.
Specific choices by physicians in terms of how they engaged with the patient made a significant difference in the patient’s experience. Patients said they felt aligned with their providers if they expressed understanding of their experiences and respect for their knowledge. Patients said they were then more willing to disclose new issues and barriers with their provider as they arose.
Discussion
The data from both arms of this study indicated that providers should acknowledge both the presence and nature of any disorders and exhibit an ability to listen to and understand the concerns of their patients. Although this may seem to be a basic and standard procedure, the results above indicate that it may be more the exception than the rule that providers are cognizant of the concerns and empathetic needs of patients. This offers a directive for providers regarding how they might best engage with patients dealing with mental health challenges.
Conclusions
The combined results regarding the nature of the relationships between specific aspects of patient beliefs and patient–provider relationships expanded our understanding of the role of patient–provider relationships beyond the psychotherapeutic and physical health context found in the existing literature. Patient beliefs about depression treatment had a targeted association with patient–provider relationships. Patient beliefs in their PC provider’s ability to respectfully and caringly recognize their depression and act in their best interest with respect to treatment were associated with all studied aspects of patient–provider relationships.
Current clinical depression affected patient comfort with disclosure but not with bonding or shared decision making with providers. It is possible that symptoms of depression subdued the effects of patient trust in their provider and openness in the patient–provider relationship due to both positive and negative symptomatology. Current depression did not eliminate the relationship between patient beliefs related to their provider’s openness. Further, the effect of treatment beliefs on provider bond and shared decision making was not affected; this suggests current depression has a relatively minor adverse effect on patient–provider relationships. As our qualitative data indicated, patients may view openness as a strategy to feel comfortable in relating their experiences, which may be a precursor to patient–provider relationships and shared decision making.
Comparison with existing literature
Patient treatment beliefs have been associated with patient–provider relationships in the literature (3,21). However, this study provided needed insight into what specific and potentially modifiable provider and patient factors may promote treatment alliance and shared decision making. Patient factors identified in the quantitative analysis included current depression status and belief in their PC provider as a trusted facilitator of depression treatment. Provider factors identified in the qualitative analysis included comfort, caring, empathy and respect. Amid conflicting studies (9,22), we found that patient–provider race and gender concordance did not play a significant role in treatment alliance or shared decision making.
Strengths and limitations
To our knowledge, this is the only study that has addressed how patient treatment beliefs about depression influence treatment alliance and shared decision making in PC. The use of mixed methods allowed us to triangulate quantitative data with qualitative experiences. However, our cross-sectional analysis of the relationship between patient beliefs and treatment alliance limited us to describing associations rather than causal relationships. Two subscale measures of patient beliefs were not reliable and therefore we could not explore additional patient beliefs. The use of more comprehensive and validated measures of patient beliefs over time may provide further insight into the relevant relationships between patient beliefs and treatment alliance.
Implications
Our findings suggest that an explicit statement from PC providers regarding their depression care philosophy may lay the foundation for belief in the provider’s ability to facilitate depression treatment. This statement could include the PC provider’s perspective on emotional well-being, awareness of emotional needs, depression symptoms, and related treatment planning and care delivery to patients.
Our findings also highlight modifiable factors which influence treatment alliance, such as creating a safe environment for patients to disclose their depressive symptoms and positively influencing depression treatment beliefs. Physicians must be able to create a comfortable environment for patients and utilize evidence-based skills (e.g. motivational interviewing) that help facilitate discussion of depressive symptoms. One approach to facilitating the development of these skills is interprofessional training facilitated through a recently formed joint accreditation programme (23,24). Interprofessional education allows physicians to share knowledge and skills with other professionals, allowing for more exposure and a better understanding on multiple discipline’s perspectives, and facilitates shared values; this results in strong individual and team skills (25). Given the importance of the physician’s qualities in facilitating discussion of depressive symptoms with patients and the potential that these skills were not part of their original medical training, continued education in interprofessional training may positively influence individual physician approaches through increased exposure and skills building in evidence-based approaches.
Declaration
Funding: The original research was supported by a grant from the National Institute of Mental Health (MH061992-03, principal investigator: JCC). Work on this manuscript was funded by the University of Southern California School of Social Work’s Postdoctoral Scholars program.
Ethical approval: analyses received exempt status from the first author’s institution; the last author’s institution provided oversight of the original study.
Conflict of interest: none.
Acknowledgements
The authors wish to acknowledge the providers and patients who participated in this study, as well as Lei Duan and Eric Lindberg for their consultation on the analysis and editing of this manuscript, respectively.
References
- 1. Bordin ES. The generalizability of the psychoanalytic concept of the working alliance. Psychother Theory Res Pract 1979; 16: 252–60. [Google Scholar]
- 2. Ursano AM, Sonnenberg SM, Ursano RJ. Physician–patient relationship. In: Tasman A, Kay J, Lieberman JA, First MB, Maj M. (eds). Psychiatry. 3rd edn New York, NY: John Wiley & Sons, 2008, pp. 20–32. [Google Scholar]
- 3. Greenberg RP, Constantino MJ, Bruce N. Are patient expectations still relevant for psychotherapy process and outcome? Clin Psychol Rev 2006; 26: 657–78. [DOI] [PubMed] [Google Scholar]
- 4. Krupnick JL, Sotsky SM, Simmens S, et al. The role of the therapeutic alliance in psychotherapy and pharmacotherapy outcome: findings in the National Institute of Mental Health Treatment of Depression Collaborative Research Program. J Consult Clin Psychol 1996; 64: 532–9. [DOI] [PubMed] [Google Scholar]
- 5. Schattner A, Rudin D, Jellin N. Good physicians from the perspective of their patients. BMC Health Serv Res 2004; 4: 26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Anderson R, Barbara A, Feldman S. What patients want: a content analysis of key qualities that influence patient satisfaction. J Med Pract Manage 2007; 22: 255–61. [PubMed] [Google Scholar]
- 7. Bertakis KD, Franks P, Epstein RM. Patient-centered communication in primary care: physician and patient gender and gender concordance. J Womens Health 2009; 18: 539–45. [DOI] [PubMed] [Google Scholar]
- 8. Whitley R. The implications of race and ethnicity for shared decision-making. Psychiatr Rehabil J 2009; 32: 227–30. [DOI] [PubMed] [Google Scholar]
- 9. Meghani SH, Brooks JM, Gipson-Jones T, Waite R, Whitfield-Harris L, Deatrick JA. Patient-provider race-concordance: does it matter in improving minority patients’ health outcomes? Ethn Health 2009; 14: 107–30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Beach MC, Roter DL, Wang NY, Duggan PS, Cooper LA. Are physicians’ attitudes of respect accurately perceived by patients and associated with more positive communication behaviors? Patient Educ Couns 2006; 62: 347–54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Westermann GM, Verheij F, Winkens B, Verhulst FC, Van Oort FV. Structured shared decision-making using dialogue and visualization: a randomized controlled trial. Patient Educ Couns 2013; 90: 74–81. [DOI] [PubMed] [Google Scholar]
- 12. Joyce AS, Ogrodniczuk JS, Piper WE, McCallum M. The alliance as mediator of expectancy effects in short-term individual therapy. J Consult Clin Psychol 2003; 71: 672–9. [DOI] [PubMed] [Google Scholar]
- 13. Goldring AB, Taylor SE, Kemeny ME, Anton PA. Impact of health beliefs, quality of life, and the physician-patient relationship on the treatment intentions of inflammatory bowel disease patients. Health Psychol 2002; 21: 219–28. [DOI] [PubMed] [Google Scholar]
- 14. Agnew-Davies R, Stiles WB, Hardy GE, Barkham M, Shapiro DA. Alliance structure assessed by the Agnew Relationship Measure (ARM). Br J Clin Psychol 1998; 37 (Pt 2): 155–72. [DOI] [PubMed] [Google Scholar]
- 15. Klinkman MS, Schwenk TL, Coyne JC. Depression in primary care–more like asthma than appendicitis: the Michigan Depression Project. Can J Psychiatry 1997; 42: 966–73. [DOI] [PubMed] [Google Scholar]
- 16. Jorm AF, Korten AE, Jacomb PA, Christensen H, Rodgers B, Pollitt P. Public beliefs about causes and risk factors for depression and schizophrenia. Soc Psychiatry Psychiatr Epidemiol 1997; 32: 143–8. [DOI] [PubMed] [Google Scholar]
- 17. Krueger RA, Casey MA. Focus Groups: A Practical Guide for Applied Research. 4th edn Thousand Oaks, CA: Sage, 2009. [Google Scholar]
- 18. Malterud K. Qualitative research: standards, challenges, and guidelines. Lancet 2001; 358: 483–8. [DOI] [PubMed] [Google Scholar]
- 19. Sandelowski M. Combining qualitative and quantitative sampling, data collection, and analysis techniques in mixed-method studies. Res Nurs Health 2000; 23: 246–55. [DOI] [PubMed] [Google Scholar]
- 20. Creswell JW, Plano Clark VL. Designing and Conducting Mixed Methods Research. 2nd edn Thousand Oaks, CA: Sage, 2011. [Google Scholar]
- 21. Tashakkori A, Teddlie C. Mixed Methodology: Combining Qualitative and Quantitative Approaches. Thousand Oaks, CA: Sage, 1998. [Google Scholar]
- 22. Connolly Gibbons MB, Crits-Christoph P, de la Cruz C, Barber JP, Siqueland L, Gladis M. Pretreatment expectations, interpersonal functioning, and symptoms in the prediction of the therapeutic alliance across supportive-expressive psychotherapy and cognitive therapy. Psychother Res 2003; 13: 59–76. [DOI] [PubMed] [Google Scholar]
- 23. Interprofessional Education Collaborative Expert Panel. Core Competencies for Interprofessional Collaborative Practice: Report of an Expert Panel Washington, DC: Interprofessional Education Collaborative, 2011. http://www.aacn.nche.edu/education-resources/ipecreport.pdf (accessed on 9 September 2014). [Google Scholar]
- 24. Robert Wood Johnson Foundation. Push for Interprofesional Education Picks Up Steam: Health Profession Accreditors Take Steps to Ensure Educational Programs Prepare Students to Participate in Team-Based Care; 2013. http://www.rwjf.org/en/about-rwjf/newsroom/newsroom-content/2013/11/push-for-interprofessional-education-picks-up-steam.html (accessed 1 September 2014).
- 25. Bridges DR, Davidson RA, Soule Odegard P, Maki IV, Tomkowiak J. Interprofessional collaboration: three best practice models of interprofessional education. Med Educ Online 2013; 16: 6035. [DOI] [PMC free article] [PubMed] [Google Scholar]