Abstract
Objective
This review explores the series of published analyses from Massachusetts General Hospital (MGH) to better understand how changes in medical specialization of burn medicine likely enabled the most important increase in survival from burns in the past 70 years.
Background
Seventy years ago, survival from the most serious burn injuries was not possible even in the most advanced countries until critical advances were introduced. Insights into those few medical advances that actually impacted survival might be better understood from the consideration of a continuous series of survival analyses over seven decades at MGH.
Methods
Mortality data from previously reported probit and logit analyses from thousands of patients treated at MGH were reviewed. A comparison of mortality from these prior mortality analyses from a more recent multi-center study and a national dataset was performed.
Results
The only giant leap forward in survival occurred during the 1970s with no improvement either during the preceding or subsequent 30-year intervals. Despite the many modern advances that have been added to the care of these patients since 1984, although these may have represented medical progress, these advances did not impact survival.
Conclusions
Survival rates from burn injury may have been maximized by current treatment approaches within medical centers of excellence in burn medicine. Further efforts to improve the burn survivor’s quality of life should ultimately have very favorable impact upon the long-term outcomes in these patients who now survive such devastating injuries.
Introduction
Survival from the most serious burn injuries has come to be expected in developed and many developing countries. Seventy years ago, this expectation was not possible even in the most advanced countries until critical advances, which enabled these dramatic survival rates, were introduced in the 1970s. Although a multitude of medical advances, each representing progress, have been introduced into burn medicine, the overall survival benefit from most of these medical advances has been only incremental at best. Significant insights into those few medical advances that actually enabled survival might be gleaned from the consideration of an almost continuous series of publications providing detailed statistical analyses of burn patients treated over 70 years at the Massachusetts General Hospital (MGH).1–6 Independently and taken together, these publications show that the entire survival improvement at the MGH was associated with the changes introduced into burn medicine during the 1970s. Intriguingly, this era was one in which multiple medical innovations were introduced. Centers of excellence for burns, first for children then for adults, were organized during the 1970s. At the time, these centers were characterized by at least four essential features: (1) an organized and fully integrated surgical and surgical critical care service; (2) a patient care services team comprised of a group of healthcare providers dedicated to the field of burn medicine; (3) a treatment strategy that focused upon early excision of the wound and immediate wound closure; and (4) a myriad of medical and surgical colleagues (e.g. in reconstructive plastic surgery, pediatric critical care, anesthesia, and infectious disease), who were also knowledgeable and dedicated with special interest in treating this unique surgical population. This review explores the series of published analyses from the MGH to better understand how these changes in the medical specialization of burn medicine might have enabled the most important increase in survival rate over the past 70 years for these critically injured patients.
Organization and Delivery of Burn Care at the MGH from 1939–1969
The first two publications reporting probit statistical analyses of burn injured patients at the MGH segmented the initial 30-year experience at MGH (1939–1969) into four distinct periods: 1939–1942, 1943–1947, 1948–1954, and 1955–1969.1,2 The 1939–1942 period was, at the time described1 as an era of “primitive care of burns” using tanning methods and spontaneous eschar separation together with systemic antibiotic therapy limited to sulfa drugs and rudimentary intravenous therapy in the resuscitation phase of post-injury care.
During this earliest period (1939–1942) however, a disastrous fire at the Cocoanut Grove Night Club, a former speakeasy turned Boston’s top night club in the post-prohibition era, occurred November 28, 1942 resulting in 491 burn-injured deaths.7,8 One hundred and fourteen patients were brought to the MGH within minutes of the disaster; 75 victims either were dead on arrival or died shortly after arrival from carbon monoxide poisoning. Thirty-nine patients were admitted to MGH and treated with state-of-the-art treatments, new protocols, and multiple innovations. Because of this experience, the surgeons and physicians at the MGH identified multiple problems and implemented many solutions that in retrospect, turned out to be very forward thinking. An Annals of Surgery monograph was published in June 1943, and included sixteen articles9–21 with a foreword7 by Dr. Oliver Cope. Many of these problems and solutions are described in the monograph, and include: disaster preparedness,8 acute grief disorder (later known as post-traumatic stress disorder, PTSD),9 airway management in carbon monoxide poisoning and shock,10 radiology and pathophysiology of pulmonary consequences of burns,11–13 surface treatment of burns (soft therapy with boric petroleum and a dry voluminous dressing),14 infections and the usage of antibiotics (sulfonamide and penicillin),15 rehabilitation of hand burns,16 physical therapy,17 fluid management of burn shock and pulmonary damage,18 role of the blood bank and plasma therapy,19 and the metabolic changes seen in burn injury.20,21 This publication was particularly timely as the world was in the midst of a war and the Office of Scientific Research and Development of the United States Government, a forerunner of the National Institutes of Health, had awarded contracts to the MGH to study two topics highly relevant to the war effort—infections in compound wounds and the physiology of burns.7 Even today, each of the topics in this monograph remains relevant to further improvements in burn medicine.
As a result of the Cocoanut Grove disaster that had highlighted the needs of this unique patient population, a small group of highly talented surgeons became interested and involved in the care of these patients during this 15-year period (1943–1955).1 These surgeons include multiple surgical giants: Drs. Edward Churchill, Bradford Cannon, Francis Moore, George Nardi, and John Raker. Although medical specialization was only in its infancy at the time, their specialties would be general, plastic, and thoracic surgery. One could say that the Cocoanut Grove disaster was the birth of burn medicine specialization at the MGH.
The second period of 1943–1947 was described,1 at the time, as an increasingly modern era in burn care in which fluid and antibiotic therapies were further refined whereas the third period, 1948–1954, was characterized1 as one of expanded use of antibiotics and nutritional therapy. The fourth period, 1955–1969, represented a further, gradual maturation of these concepts of fluid, antibiotic, and nutritional therapies in burn medicine.2
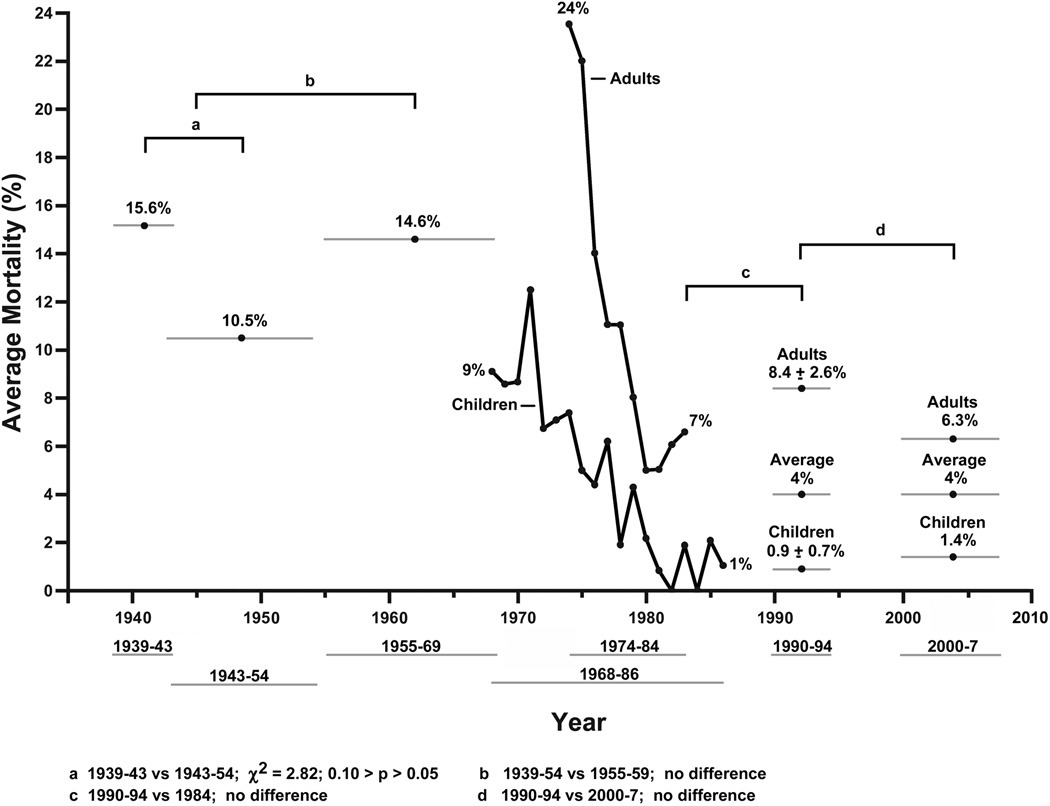
Burn Mortality in 1939–1954 and 1955–1970
In a probit analysis describing the initial 15-year experience, there was a trend of declining overall mortality between 1939–1942 and 1943–1954 from 15.6% to 10.5% (Fig. 1).1 This survival benefit might have been consistent with the improved therapies introduced after the experience in the care of the Cocoanut Grove fire victims. However, this decline in mortality rate was only a trend of borderline significance (χ2=2.82; 0.10>p>0.05). Although there was a collection of doctors and specialized nurses dedicated to the burn patient population during this period (1943–1955), the impact on survival fell short of statistical significance. Despite this shortfall in expectation, this survival trend may have triggered the beginning of a center for burns at MGH.
Figure 1. Seventy-year mortality from burns at MGH.
Average annual mortality rates or average mortality rates for an indicated time period from a series of published statistical analyses1–5 and improved survival rates from burn injury 2000–2007 (unpublished results) at the MGH over 70 years. The 30-year period prior to the 1970s was a combined mortality rate for both children and adults whereas the 30-year period after the early 1980s was segregated mortality rates for children and adults. a 1939–1943 vs. 1943–1954, χ2=2.82, 0.10 > p > 0.051 ; b 1939–1954 vs. 1955–1969, no difference2 ; c 1990–1994 vs. 1984, no difference5 ; d 1990–1994 vs. 2000–2007, no difference (unpublished results)
From this analysis,1 it is interesting to note the age groups benefiting most from these medical advances and the factors determining fatality from burn injury. The favorable trend in survival in this study had been limited to those 16–35 years of age, which at the time was explained as “a reflection of the vigor and physiological fitness of individuals in the prime of their life.”1 The youngest (0–15 years) and the two older age groups (36–55 and 56–100 years) failed to show improvements in survival. The major determinants for mortality during this period were age, extent of burn, and “many countless unrelated factors including those identified: lapse of time between injury and therapy, presence of inter-current infections, associated degenerative diseases, development of drug resistant organisms, prior nutrition, transfusion reactions, allergic reactions to drugs, immune response of the patient, severity of sepsis, nursing care, and professional judgment”.1 Although the “many countless unrelated factors” are better compensated by current medical therapies, even today, these factors continue to contribute to morbidity and mortality from burn injury.
In the second publication, the LA50 for the next 15-year period (1955–1970) was not statistically different when compared to that of the prior 15-year period, 1939–1954 (Fig. 1).2 It appeared that the trend toward a reduction in mortality rate during 1943–1952 had been short-lived because it disappeared during the subsequent 15-year period (1955–1970). Perhaps this might have been the result of events during this second 15-year period in which the burn patients at MGH were moved to a single ward, primarily to isolate their microbial flora from spread to other patient populations, and they were assigned to general care in a surgical service that specialized in plastic surgery.
Taken together, this combined overall 30-year MGH experience from 1939 to 1970 turns out to be completely consistent with that of all other reporting hospitals as shown in an extensive comparison of LA50 values in seventeen statistical analyses from contemporary institutions; there were no statistical differences found among these other medical centers including the MGH.2 For a point of general reference regarding the state-of-the-art during this 30-year period, the representative LA50 at MGH for various age groups was dismal: 0–15 years, 49% TBSA; 16–35 years, 56% TBSA; 36–55 years, 43% TBSA; and 56–100 years, 23% TBSA. Although mortality rates had not improved over this 30-year period, there was a suggestion that perhaps incremental progress in burn treatment had been made because there had been a decrease in the lengths of stay of those who were discharged alive and an increase in the number of days to death in those patients who ultimately died during the initial hospital admission.2
The Era of Burn Centers at MGH
Beginning in November 1968 at MGH, all children (<18 years) with burn injuries were admitted to the Shriners Burns Institute (SBI), which became fully functional by 1970 as a newly organized pediatric burn center under the direction of Dr. John Francis Burke. The first 200 children with burns 10–65% TBSA were treated with topical silver nitrate therapy with either prompt excision of the burn eschar and immediate wound closure or spontaneous eschar separation with delayed or subsequent wound closure.4 After this initial clinical trial ended in 1972, all children were subsequently treated with silver nitrate topically and prompt eschar excision with immediate wound closure. Based on these results, Dr. Burke established an adult burn center at the MGH in July 1974 using this same surgical treatment approach.3
Burn Mortality in Adults and Children from 1974–1984
Adults
In the new adult burn center, overall mortality was reduced from 24% in 1974 to an average of 7% for the years 1979–1984 (Fig. 1).3 In a logit analysis,3 1,103 adults in two time periods (1974–1977 and 1978–1984) were compared to identify previously unknown factors determining mortality in addition to the known significant factors of burn size and age (p<0.001). After controlling for burn size and age, the treatment comprising prompt excision and immediate wound closure system was also statistically significant (p<0.001). Exploring these data further, all adult age groups, which included the elderly, had statistically significant improvements in survival with the middle-aged patients (40–60 years) experiencing the greatest improvement. Improvement was so significant in the young adults (20–40 years) that age no longer was statistically correlated with mortality. However, age remained an important determinant of mortality for patients aged 50 or older.
Children
Dramatic improvements in survival were also seen in a logit analysis4 of 1,696 children admitted from 1968–1986 to the new pediatric burn center at SBI. Under this new treatment system supporting the strategy of prompt eschar excision with immediate wound closure, overall mortality declined from an average of 9% in the initial few years of the new center (1968–1972) to 1% in the 1980s (Fig. 1). Moreover, mortality in children was essentially eliminated in moderate (14–49%) and large (50–69%) burns and the mortality rate was markedly reduced for massive (≥70%) burns. In the latter years, the deaths of children were only those who suffered from massive burns. For the first time, young children, including infants, survived burn injuries at least as well as young adults. This latter finding reversed the broadly held concept that the very young were at a disadvantage to survival from burn injury. Certainly, the creation of a burn center with pediatric and other burn care clinicians to the problem of treatment of pediatric burns likely enabled these significant and important advances.
The overall mortality rate when the two new burn centers were first organized was likely no better than it had been during the 30 years prior to the early 1970s. The overall mortality rate at the MGH (adults) was 24% (1974–1976) and at the SBI (children) was 9–10% (1968–1972) (Fig. 1). An estimated combined adult and pediatric mortality rate that assumes a comparable number of hospitalized children and adults would be essentially no different than the mortality rates seen in the prior periods at MGH.
Burn Mortality in 1990–1994 and 2000–2007
Survival rates from burn injury in 1990–1994 were no better than the rate that had already been achieved in 1984 at the MGH. In a follow-up study,5 1,665 patients at MGH (755 adults) and SBI (910 children) were analyzed during the period 1990–1994 (Fig. 1). The overall mortality rate for the entire group was 4%. The mortality rate for adults was 8.4±2.6% and for children was 0.9±0.7%. In evaluating the study, we examined how the mortality rate differed in 1990–1994 from 1984. Statistically comparing the 1990–1994 results with the mortality rate previously modeled for the year, 1984, there was no difference. We also evaluated the predominant risk factors for death in this more modern study. In the study, these risk factors were age >60 years, TBSA >40%, and presence of inhalation injury all of which can be easily identified at the time of admission. Although more explicitly defined in this study, these had been previously recognized as the most important risk factors to determine mortality in previous decades and have remained important determinants even today.
In a more recent analysis (unpublished data) at MGH (1,378 adults) and SBI (1,276 children) of those admitted and treated during the years 2000–07, overall mortality was unchanged at 4% from the previous results for 1990–94 (Fig. 1). The mortality rates were 6.3% (adults) and 1.4% (children). By logit analysis, these mortality rates were statistically no different from those in 1990–1994 and therefore, no further survival improvements had occurred beyond those results already achieved in 1984 even in this new millennium of burn medicine.
Comparison with a Large-scale Collaborative Project – “Inflammation and the Host Response to Injury” from 2000–2009
A prospective, clinical study6,22,23 involving six U.S. burn centers was conducted in the large-scale collaborative project entitled “Inflammation and the Host Response to Injury” (Glue Grant) funded by the National Institutes of Health – General Medical Sciences (NIGMS). This multi-center study followed published standard operating procedures23 and in addition to these patients with burn injuries and in addition followed a parallel cohort of patients with severe blunt trauma.24 These six centers, which included MGH, are a group of organized burn centers that have been verified by the American Burn Association/American College of Surgeons (ABA/ACS) Burn Center Verification Program26. In the Glue Grant study,6,22,23 541 patients (300 adults, 241 children) during the period 2003–2010 were admitted with burns >20% TBSA requiring one or more operations. The adult mortality rates were 14.1% (17–55 years) and 38.5% (≥ 55 years) and the pediatric mortality rate was 7.9% (<17 years). These mortality rates were higher because the study inclusion criteria for patients in this multi-center study had excluded all of the smaller, non-fatal burn injuries.
These multi-center results6 were statistically compared to those at the MGH and SBI for the period 1990–1994. The Flora’s score, based upon the prior MGH and SBI series, predicted 74.09 deaths in the Glue Grant study compared to the 74 deaths that were actually observed in the Glue Grant study (z= −0.01, p=0.9895). In summary, when comparing the results of this multi-center clinical trial with prior published results at the MGH, there were no statistical differences to those previous published for 1984, 1990–1994, and 2000–2007.6
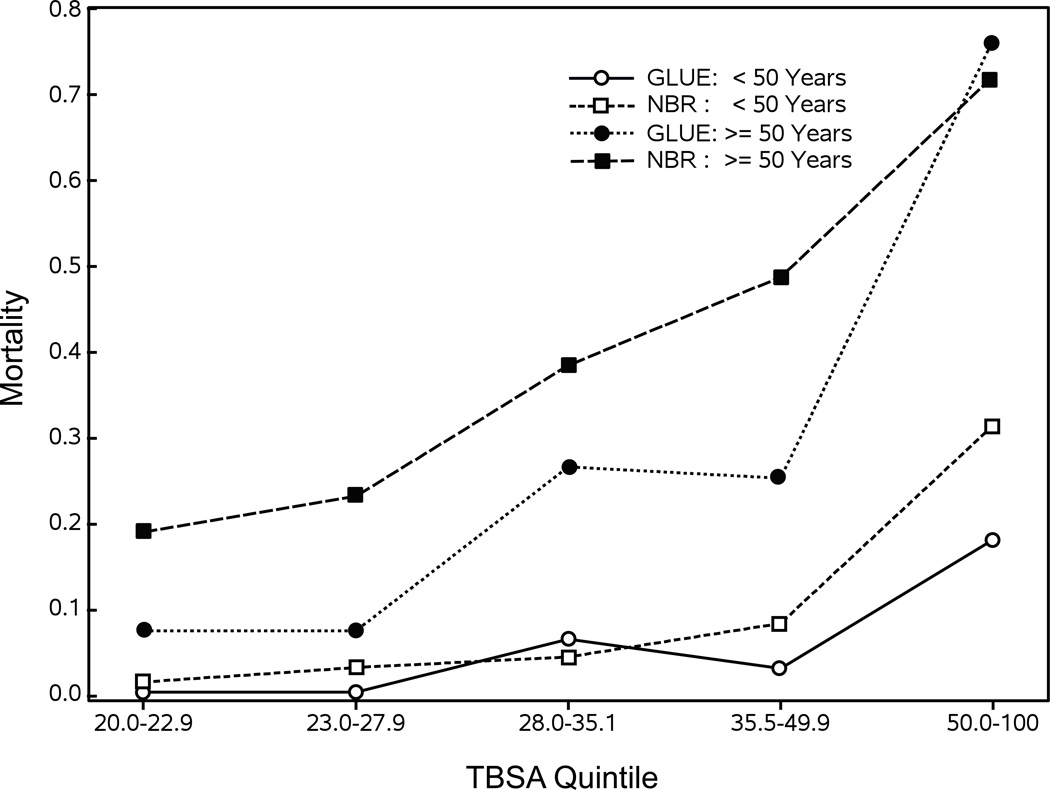
Comparison with the National Burn Repository from 2000–2007
Significant differences were seen when comparing the results of the Glue Grant clinical trial to those published in the National Burn Repository (NBR).6 The NBR dataset used for comparison was comprised of 201,174 records from burn centers not including the data from the six verified Glue Grant burn centers. Of ninety-one centers contributing records to the NBR in 2013, twenty-eight centers (31%) were self-reported burn centers that have not been verified by the ABA/ACS Burn Center Verification Program.26 After the study inclusion and exclusion criteria were applied to the NBR dataset, the remaining records were used for comparison. Results show that younger patients (< 50 years) in the Glue Grant study with moderate to massive burns (35.5–100% TBSA) had statistically significant lower mortality rates, whereas older patients (≥ 50 years) in the Glue Grant study with smaller and moderate sized burns (20–50% TBSA) also had lower mortality rates (Fig. 2). These analyses6 show that even today, opportunities remain to improve survival rates for burn injuries for these very important patient subpopulations in a portion of NBR burn centers.
Figure 2. Mortality for Glue Grant versus NBR patients.
Comparisons of mortality rates by TBSA quintile and age group (<50 years old versus ≥50 years old) for those patients in the Glue Grant with those in the NBR are shown.6 For young patient (<50 years), improved survival rates were seen for >35.5 TBSA injuries, whereas for older patients (≥50 years) improved survival rates were seen in 20–49.9% TBSA injuries. Manuscript in press at time of this manuscript submission: Reprinted from Annals of Surgery, day/month/year, volume #, issue #, pp #. Wolters Kluwer Health Lippincott Williams & Wilkins©
American Burn Association/American College of Surgeons (ABA/ACS) Burn Center Verification Program
It is assumed that the organization of these and other new burn centers likely enabled the remarkable survival improvements seen after the 1970s. The ABA/ACS Burn Center Verification Program25 has been developed to define the important essential as well as desirable components of a hospital to be defined as a burn center. These features might not include only those elements enabling survival that were introduced with the conception of burn centers in the 1970s, but also include the other modern medical advances that are currently considered desirable or essential to raise the quality of lives of those who survive. The current-day burn centers at MGH and SBI are ABA/ACS verified centers and can be characterized by specialized medical personnel (surgeons, anesthesiologists, pediatricians, psychiatrists, among others) and personnel from nursing, rehabilitation, and other important services (social workers, pharmacists, respiratory therapists, nutritional services personnel) with particular specialized knowledge, experience, and keen interest in this unique patient population. For burn patients, the surgical approach of prompt excision and immediate wound closure requires a system that addresses meticulous care and attention to the patient’s physiologic, metabolic, immunologic, and nutritional status. Although it is impossible to determine which individual components are the most important to contribute to improved survival rates, all of these features are considered essential and their existence at a hospital can be confirmed by the ABA/ACS Burn Center Verification Program.25
The introduction of burn centers of excellence into clinical medicine described here has paralleled those efforts in many other fields of medicine like transplantation, cardiac, cancer, vascular, and stroke centers of excellence to name a few. In all cases, medical specialization systems approaches may have served to optimize both the survival and outcomes of multiple specialized patient populations as it has with the burn-injured patient.
Conclusions and the Future
This review represents a published series1–6 of statistical analyses of the mortalities resulting from burn injuries in patients treated at MGH, taken together and compared to a multi-center study and national datasets. Over the entire 70-year period, at least at this one institution, the only giant leap forward in survival occurred during the 1970s with no improvement in survival either during the preceding or subsequent 30-year intervals. During the first 30 years of this 70-year review, the studies indicate that despite many improvements being implemented as a direct response to the Cocoanut Grove experience, there was no demonstrable sustainable improvement in survival. After the Cocoanut Grove disaster, highly talented surgeons1 focused on the needs of this particular patient population and possibly as a result, a trend in improvement1 toward survival developed. However, this trend rapidly faded over the subsequent period of 1955–1969 when these patients with special needs moved into a general patient population.2 Despite the many modern advances that have been added to the care of these patients since 1984, although these may have represented medical progress, the advances have not improved survival.
Furthermore, when comparing the MGH results in a multi-center trial6 and a national dataset,6 the survival rates in the very recent multi-centered burn injury study were no better than those seen at the MGH from 1984, 1990–1994, and 2000–2007. However, a serious concern remains in the fact that there were NBR reporting centers with survival statistics that fell short of the current benchmark published by the multi-center study as well as those previously published MGH results. These comparisons show that the need exists for further improvement in the survival of younger patients with large to massive burns and older patients with moderate to large burns, at least at a portion of burn centers reporting to the NBR. Patients with these characteristics are those who benefit most from treatment in centers of excellence for burns.
The dramatic advance in survival rates that occurred during the 1970s at MGH coincided with the formation of two new burn centers, one for children4 and one for adults.3 This was an era when the medical specialization of care included dedicated general and surgical critical care surgeons and reconstructive plastic surgeons together with medical colleagues including anesthesiology, pediatrics, infectious disease, psychiatry, and other specialties with knowledge, experience, and interest in burn medicine. The burn care system as exemplified by the Verification Program provides the foundation that has enabled the current acute care environment to ensure such a consistently high rate of survival even from otherwise devastating injuries. Perhaps in addition to the verification of the personnel, programs, and facilities that are essential to verifiable burn centers,25 the verification program should consider the addition of quantitative outcome measures such as the survival benchmark studies5,6 described here. In the future, these outcomes could include those outcomes measure that define the quality of life resulting from these injuries.27
Given that survival rates may have been maximized by current treatment approaches, attention to improvements in the burn survivor’s quality of life is warranted.27 In the early post-discharge period for many patients, the quality of the wound healing process can be adversely affected by tension created by their burn wound healing process. These effects are likely influenced by the patient’s propensity to scar, which differs depending upon their genomic makeup. In these patients, considerable opportunities exist to offer improvements in the cosmesis and functionality of their healed wounds. All-in-all, attention to these and the other needs of this unique patient population will ultimately have very favorable impact upon the long-term outcomes in these patients who survive such devastating injuries.
Looking to the future, it appears that survival rates may have reached their maximum using current treatment approaches. Fortunately, data and knowledge from the Glue Grant28,29 have led to new insights into both the genomic and proteomic changes seen after serious injury from burns, which include the metabolic consequences of insulin resistance, mitochondrial dysfunction, and skeletal muscle cachexia, as well as the dramatically up regulated components of the innate immune system. These new insights promise to lead to medical advances that may limit the harmful components of the innate immune response and control the multiple metabolic consequences of burn injury. Critical advances in these areas of research offer tremendous opportunity to further improve survival and reduce morbidity after burn injury in future burn patients.
Table 1.
Six Participating ABA/ACS Verified Burn Centers in the NIGMS multi-center study
| University of Washington School of Medicine and Harborview Medical Center |
| Loyola University School of Medicine |
| Parkland Memorial Hospital, University of Texas, Southwestern Medical Center |
| University of Texas Medical Branch – Galveston |
| Shriners Burns Institute – Galveston |
| Massachusetts General Hospital, Harvard Medical School |
Acknowledgements
This study was supported by the following grants from the National Institute of General Medical Sciences: P50GM021700, T32GM007035, U54GM062119, R24GM102656, and R01GM101401
Source of Funding: None were declared
Footnotes
Conflicts of Interest: None were declared
References
- 1.Mortality of Burns at the Massachusetts General Hospital 1939–1954. Ann Surg. 1957;145:210–222. doi: 10.1097/00000658-195702000-00010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Barnes BA, Constable JD, Burke JF. Mortality of burns at the Massachusetts General Hospital 1955–69. In: Matter P, Barclay JL, editors. Transactions of the 3rd International Congress on Research in Burns. Research in Burns. Bern: Hans Huber Publishers; 1971. pp. 430–433. [Google Scholar]
- 3.Tompkins RG, Burke JF, Schoenfeld DA, et al. Prompt eschar excision: A treatment system contributing to reduced burn mortality. Ann Surg. 1986;204:272–281. doi: 10.1097/00000658-198609000-00006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Tompkins RG, Remensnyder JP, Burke JF, et al. Significant reductions in mortality for children with burn injuries through the use of prompt eschar excision. Ann Surg. 1988;208:577–585. doi: 10.1097/00000658-198811000-00006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Ryan CM, Schoenfeld DA, Thorpe WP, et al. Objective estimates of the probability of death from burn injuries. N Engl J Med. 1998;338:362–366. doi: 10.1056/NEJM199802053380604. [DOI] [PubMed] [Google Scholar]
- 6.Klein MB, Goverman J, Hayden DL, et al. Benchmarking outcomes in the critically injured burn patient. Ann Surg. 2014 doi: 10.1097/SLA.0000000000000438. in press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Cope O. Management of the Cocoanut Grove burns at the Massachusetts General Hospital. Foreword. Ann Surg. 1943;117:801–802. [PMC free article] [PubMed] [Google Scholar]
- 8.Faxon NW. The problems of the hospital administration. Ann Surg. 1943;117:803–808. doi: 10.1097/00000658-194306000-00002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Cobb S, Lindemann E. Neuropsychiatric observations. Ann Surg. 1943;117:814–824. doi: 10.1097/00000658-194311760-00004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Beecher HK. Resuscitation and sedation of patients with burns which include the airway. Ann Surg. 1943;117:825–833. doi: 10.1097/00000658-194306000-00005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Aub JC, Pittman H, Brues AM. The pulmonary complications: A clinical description. Ann Surg. 1943;117:834–840. doi: 10.1097/00000658-194311760-00006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Schatzki R. Roentgenologic report of the pulmonary lesions. Ann Surg. 1943;117:841–864. doi: 10.1097/00000658-194306000-00007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Mallory TB, Brickley WJ. Pathology: With special reference to the pulmonary lesions. Ann Surg. 1943;117:865–884. doi: 10.1097/00000658-194311760-00008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Cope T. The treatment of the surface burns. Ann Surg. 1943;117:885–893. doi: 10.1097/00000658-194306000-00009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Lyons C. Problems of infection and chemotherapy. Ann Surg. 1943;117:894–902. doi: 10.1097/00000658-194306000-00010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Cannon B. Procedures in rehabilitation of the severely burned hand. Ann Surg. 1943;117:903–910. doi: 10.1097/00000658-194306000-00011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Watkins AL. A note on physical therapy. Ann Surg. 1943;117:911–914. doi: 10.1097/00000658-194306000-00012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Cope O, Rhinelander FW. The problem of burn shock complicated by pulmonary damage. Ann Surg. 1943;117:915–928. doi: 10.1097/00000658-194306000-00013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Soutter L. A note on the blood bank. Ann Surg. 1943;117:928–931. doi: 10.1097/00000658-194306000-00014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Moore FD. A note on the thrombophlebitis encountered. Ann Surg. 1943;117:931–936. doi: 10.1097/00000658-194311760-00015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Cope O, Nathanson IT, Rourke GM, Wilson H. Metabolic observations. Ann Surg. 1943;117:937–958. [PMC free article] [PubMed] [Google Scholar]
- 22.Klein MD, Hayden D, Elson C, et al. The association between fluid administration and outcome following major burn: a multicenter study. Ann Surg. 2007;245:622–628. doi: 10.1097/01.sla.0000252572.50684.49. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Silver GM, Klein MB, Herndon DN, et al. Standard operating procedures for the clinical management of patients enrolled in a prospective study of Inflammation and the Host Response to Thermal Injury. J Burn Care Res. 2007;28:222–230. doi: 10.1097/BCR.0B013E318031AA44. [DOI] [PubMed] [Google Scholar]
- 24.Cuschieri J, Johnson JL, Sperry J, et al. Benchmarking outcomes in the critically injured trauma patient and the effect of implementing standard operating procedures. Ann Surg. 2012;255:993–999. doi: 10.1097/SLA.0b013e31824f1ebc. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.American Burn Association; 2006. [on 12/4/2013]. Guidelines for the Operation of Burn Centers. Downloaded at http://www.ameriburn.org/verification_about.php. [DOI] [PubMed] [Google Scholar]
- 26.Chicago, IL: American Burn Association; [on 11/15/2013]. 2013 National Burn Repository Report: Report of Data from 2003–2012. Downloaded at www.ameriburn.org/NBR.php. [Google Scholar]
- 27.Tompkins RG, Liang MH, Lee AF, et al. The American Burn Association/Shriners Hospitals for Children burn outcomes program: A progress report at 15 years. J Trauma Acute Care Surg. 2012;73:S173–S178. doi: 10.1097/TA.0b013e318265c53e. [DOI] [PubMed] [Google Scholar]
- 28.Xiao WZ, Mindrinos MN, Seok JH, et al. A genomic storm in critically injured humans. J Exp Med. 2011;208:2581–2590. doi: 10.1084/jem.20111354. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Seok JH, Warren HS, Cuenca AG, et al. Genomic responses in mouse models poorly mimic human inflammatory diseases. Proc Natl Acad Sci USA. 2013;110:3507–3512. doi: 10.1073/pnas.1222878110. [DOI] [PMC free article] [PubMed] [Google Scholar]