Abstract
Background
Influenza is a major complication in cancer and hematopoietic cell transplant (HCT) recipients. We set out to maximize influenza vaccination rates in healthcare personnel at our large ambulatory cancer center with high baseline compliance and to assess alternatives to mandatory policies.
Methods
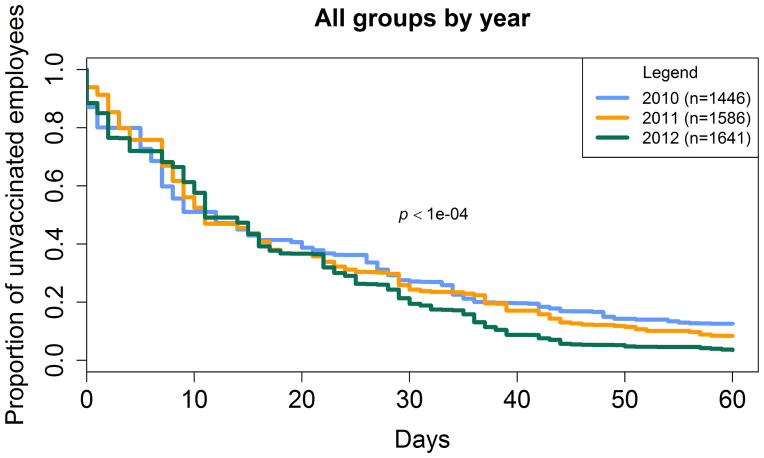
Baseline influenza vaccine compliance rates at our center were over 85%. In 2011 an incentive-based “carrot” campaign was implemented, and in 2012 a penalty-based “stick” approach to declining staff was required. Yearly approaches were compared using Kaplan-Meier survival estimates.
Results
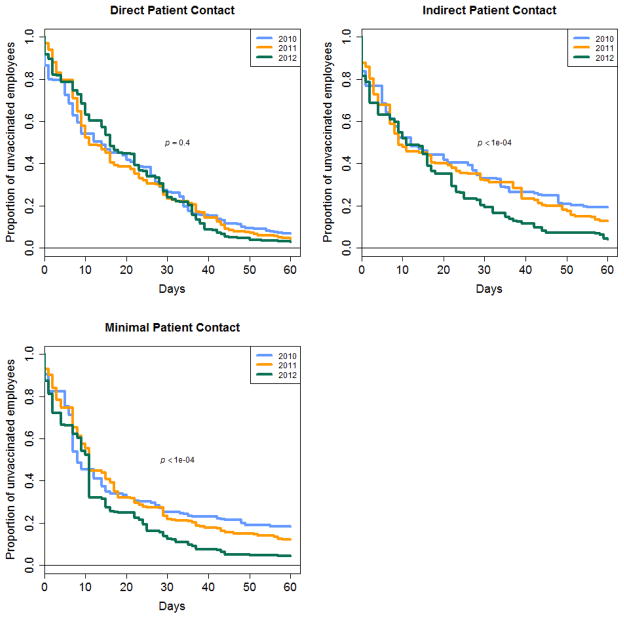
Both the incentive and penalty approaches significantly improved upon the baseline rates of vaccination (2010 vs. 2011 [p=0.0001]; 2010 vs. 2012 [p<0.0001), but 2012 significantly improved over 2011 (p<0.0001). Staff with direct patient contact had significantly higher rates of vaccination when compared to those with indirect and minimal contact in every campaign year, except in the penalty-driven campaign from 2012 (p<0.001, <0.001, 0.24, and p<0.001, <0.001, 0.17, respectively).
Conclusion
A multifaceted staff vaccination program that included education, training and active declination was more effective than one offering incentives. Improvements in vaccination rates in the penalty-driven campaign were driven by staff without direct care responsibilities. High compliance with system-wide influenza vaccination was achieved without requiring mandatory vaccination.
Keywords: Healthcare personnel, occupational health, influenza, vaccination
INTRODUCTION
Influenza is a major cause of morbidity and mortality in cancer and hematopoietic cell transplant (HCT) patients.1,2 These highly immunosuppressed patients present with fewer clinical symptoms, have prolonged viral shedding, are at increased risk for nosocomial transmission, are more apt to develop antiviral resistance and are more likely to progress to lower-tract disease.1 Although vaccination has been shown to be the most important intervention for influenza prevention, many of these patients mount attenuated or inadequate protective responses to influenza vaccine.2,3 In healthcare settings with large numbers of cancer, transplant and immunosuppressed patients, vaccination of healthcare personnel (HCP) is a critical component for influenza prevention.4
At our comprehensive ambulatory cancer care center, we historically have achieved high vaccination rates, but had plateaued at approximately 85% of staff accepting annual influenza vaccination despite robust and well marketed vaccine campaigns. In an effort to achieve a pre-specified goal of 95% vaccine coverage in our HCP population, we attempted two different staff vaccination strategies: one that assessed incentives (2011,“carrot”) and passive declination, and a second that required decliners to complete enhanced influenza vaccine education with a face-to-face active declination process (2012, “stick”). We compared vaccination rates between these strategies and baseline rates (2010) to determine which resulted in the highest rates of vaccine compliance. Additionally, we tracked vaccination rates between types of employees, conversion rates among previous decliners and assessed those who declined vaccination after previously being vaccinated by strategy year.
METHODS
Study Population
The study was performed at a large comprehensive cancer care center that provides ambulatory care to patients receiving treatment for hematologic and solid tumor malignancies, including a large number of patients undergoing HCT. Approximately 1500 employees and clinical staff are employed in the clinic, where there are over 70,000 outpatient visits per year. The vast majority of these patients are at high risk for influenza and influenza-related complications due to chemotherapy, transplant, disease-related immunosuppression, in addition to multiple other known risk factors for influenza.
The study population consisted of three employee cohorts based on HCP vaccination strategy per calendar year. All staff were eligible for inclusion in this study if they were employed at the cancer center for at least one of the annual vaccination campaigns during 2010–2012; individuals not employed for the entire duration of at least one vaccination campaign were excluded. Yearly cohorts based on influenza vaccine strategy were not mutually exclusive as the majority of employees worked during multiple vaccination campaigns. Employee vaccination status was collected and tracked by the Occupational Health Department during each season; any influenza vaccinations received outside of the campaign window were not considered for the purposes of these analyses. Demographic and vaccination data were then extracted from Occupational Health databases. All study components were approved by the center’s Institutional Review Board.
Vaccine Strategies
During all campaigns, vaccine was provided free of charge to all employees. Thimerosol-free vaccines and the live-attenuated nasal spray vaccine (FluMist®) were also available for staff requesting preservative-free or needle-free vaccination. Those receiving vaccines outside the center, at a physician’s office, pharmacy or at another facility, were required to bring documentation to Occupational Health to be credited as compliant with the center policy. A complete summary of the yearly vaccination strategies for 2010 through 2012 is included in Table 1.
Table 1.
Summary of employee influenza vaccination strategies by year
| Components | Year and Strategy Type | ||
|---|---|---|---|
| 2010 Baseline | 2011 Carrot | 2012 Stick | |
| Center-based Strategies | |||
| Free Vaccine | ✓ | ✓ | ✓ |
| Vaccine Clinics on Campus | ✓ | ✓ | ✓ |
| Mobile Carts | ✓ | ✓ | |
| Vaccine rounds with Infection Prevention Staff | ✓ | ✓ | |
| Centerwide advertising | ✓ | ✓ | ✓ |
| Centerwide Flu vaccine talk | ✓ | ✓ | |
| Email reminders | ✓ | ✓ | ✓ |
| Weekly updates to managers regarding non-compliant staff | ✓ | ✓ | ✓ |
| Center leadership support/involvement | ✓ | ✓ | ✓ |
| Incentives | |||
| $25 gift card if 95% vaccination rate achieved centerwide | ✓ | ||
| Declination process | |||
| Declination form | ✓ | ✓ | ✓ |
| Form faxed or emailed to OHS | ✓ | ||
| Form hand delivered to OHS | ✓ | ✓ | |
| Form completed in presence of OHS staff | ✓ | ||
| Online education and Post-test required for declination | ✓ | ||
| One-on-one peer counseling with OHS staff | ✓ | ||
| Required appointment for counseling and declination | ✓ | ||
| Medical opt-out of vaccination | ✓ | ✓ | ✓ |
| Filled out by employee and faxed or emailed to OHS | ✓ | ✓ | |
| Required physician note | ✓ | ||
| Consequences with non-compliance | |||
| Manager-initiated discussion | ✓ | ✓ | ✓ |
| Disciplinary letter into Employee file | ✓ | ||
| Increasing sanctions if not compliant | ✓ | ✓ | |
| Campaign length | |||
| Time from start of strategy | unspecified | 8 weeks | 6 weeks |
Baseline strategy (2010)
Two weeks prior to the campaign start, the vaccine availability was advertised via multiple modalities at the center, including; mass emails, newsletter articles, and intranet postings. All employees were required to either be vaccinated or to complete a one-page signed declination form acknowledging that they understood the risks of declining the vaccine in a setting with such high-risk patients. Employees were allowed to return the declination form via email, fax, or in-person. Influenza vaccine was provided at drop-in vaccine clinic locations throughout the center’s clinical and administrative areas; mobile vaccine carts provided additional opportunities for vaccination throughout the campaign. The vaccine campaign began September 22, 2010, but had a rolling/non-specific deadline.
Incentive-based strategy (2011 “Carrot”)
In addition to the baseline measures as described above, an “incentive” component was added to the 2011 vaccination campaign. This incentive was organized so that if 95% of all employees received the vaccine the entire staff would be rewarded with a $25 gift card. The incentive was advertised across the center, and weekly, department-level breakdowns of vaccination rates were posted on the center’s intranet and emailed to all managers and supervisors. The Infection Prevention department joined Occupational Health and visited clinical spaces with vaccine carts, to encourage program participation and promote vaccination. Additionally, the timeline of the vaccine campaign was shortened to eight weeks beginning on September 19, 2011.
The wording and content of the 2011 declination form mimicked the 2010 form; however employees were now required to return the declination form in-person to the Occupational Health RNs who had offices located one block away from the clinic. Employees declining for medical reasons were required to provide a note from a caregiver outside of the center specifying the rationale for influenza vaccine contraindication. Employees that did not comply with the policy were reprimanded by their manager in a face-to-face meeting and given deadlines for compliance.
Penalty-based strategy (2012 “Stick”)
During the 2012 campaign the policies were similar, except the incentive policy was replaced with a penalty-driven strategy for vaccine declination.5 Employees that opted to decline vaccination were required to: 1) complete a 30-minute online education module with post-test; 2) undergo one-on-one counseling session where an 11 point attestation statement (Table 2) was reviewed by Occupational Health or Infection Prevention staff and 3) sign this attestation in the presence of these staff (active declination). The declination process took over an hour, and required staff to schedule off-site counseling sessions within limited time blocks. Staff that did not meet campaign deadlines by either receiving or declining the vaccination were required to meet with their respective manager, and a disciplinary letter signed by Infection Prevention and center directors was placed in the employee’s personnel file. Employees that did not comply following these efforts were warned that they would receive additional penalties, including suspension from clinical care, leave without pay, and possible dismissal unless they became compliant with the policy by receiving or declining the vaccine.
Table 2.
Attestations that Employees Declining the Influenza Vaccine Reviewed and Signed in 2012
| 1 | I have received education about the effectiveness of the flu vaccine I understand that vaccination is the best way to prevent the flu. |
| 2 | I have been informed that the flu vaccination is strongly recommended by my employer and multiple national and international organizations to help prevent the spread of flu to patients, co-workers, family and others in the community. |
| 3 | I understand that patients at our oncology center are at the highest risk for major complications of the flu, including death. |
| 4 | I have been educated that if I contract the flu, I am contagious for 24 hours before I get sick, allowing me to transmit the virus before I develop symptoms of infection. |
| 5 | I understand that if I have flu, patients with whom I may come into contact could develop a life-threatening flu infection even if my infection is mild. |
| 6 | I understand that the flu virus changes almost every year, and that is why an annual flu shot is strongly recommended. |
| 7 | I cannot get the flu from the flu shot because it does not contain a live flu virus. |
| 8 | I have been given the opportunity to be vaccinated with the flu vaccine at no charge to myself and all my questions have been answered. |
| 9 | I understand that I may change my mind at any time and accept flu vaccination as long as the vaccine remains available. |
| 10 | I have been informed that flu vaccine may become mandatory (condition of employment) in the future. |
| 11 | I will not come to work with respiratory symptoms in an effort to prevent the spread of respiratory viruses to patients and other staff. |
Definitions and Statistical Analysis
Since common areas within the facility are frequented by both clinical and non-clinical staff (e.g. cafeteria, elevators), all employees at the facility were included in these campaigns. For the purposes of analysis, staff were categorized by their level of contact with patients as follows: 1) Direct - those that provide face-to-face clinical patient care (e.g. nursing, physicians) 2) Indirect - those employees with limited face-to-face contact with patients (e.g. reception desk, registration) and 3) Minimal - employees who entered and worked in facility but did not interact directly with patients during the course of their clinical care (e.g. administration, finance).
Following each campaign, eligible staff members were categorized as vaccinated, declined, or non-compliant, where non-compliant was defined as those persons who either did not receive or decline the vaccine within the specified time requirements of each calendar year’s vaccine campaign. Employees with medical waivers were excluded from the cohort for the purposes of analyses. Vaccine converters were defined as HCP who had previously been vaccine decliners and received vaccine the following year. New decliners were defined as those who had received vaccine previously and the subsequent year became vaccine decliners. In order to be considered a vaccine converter or a new decliner, HCP had to be employed in the center for at least two consecutive vaccination seasons.
Vaccination acceptance was assessed over the three year study period to compare campaign strategies. The probability of vaccination was estimated using Kaplan-Meier survival methods, where survival was defined as receipt of vaccine and survival time as the number of days from the start of the vaccine campaign to vaccine receipt. For purposes of analyses, data were compared from the start through the first 60 days of each campaign. The log rank test was used to compare survival (vaccination) by influenza strategy year. Additional comparisons were made after stratification by level of patient contact and compared using similar methods. Where applicable, categorical variables were compared using χ2 or Fisher’s exact tests, and continuous variables using the Wilcoxon rank-sum or Kruskal-Wallis tests. All analyses were performed using R statistical software package.6
RESULTS
Demographic characteristics for all eligible employees during each of the 2010–2012 influenza vaccination campaigns are presented in Table 3. The number of employees increased from 2010 (n=1446) to 2012 (n=1641), but the proportion of HCP in the three defined levels of patient care groups did not significantly change over time (p=0.27).
Table 3.
Demographics over three yearly healthcare personnel influenza vaccine campaigns from 2010–2013
| 2010–2011 | 2011–2012 | 2012–2013 | |
|---|---|---|---|
| n=1446 n (%) |
n=1586 n (%) |
n=1641 n (%) |
|
| Age | |||
| Median (IQR) | 41.2 (33–51.5) | 40.9 (32.5–51) | 41.5 (33–51.8) |
| < 26 | 68 (5.0) | 89 (6.1) | 85 (5.2) |
| 26 – 45 | 831 (57.5) | 909 (57.3) | 936 (57.0) |
| 46 – 60 | 443 (30.6) | 463 (29.2) | 459 (28.0) |
| > 60 | 104 (7.1) | 125 (7.9) | 161 (9.8) |
| Job category | |||
| Administration & Building | 413 (28.6) | 453 (28.6) | 487 (29.7) |
| Clinical Technologists | 67 (4.6) | 73 (4.6) | 75 (4.6) |
| Laboratory | 121 (8.3) | 135 (8.5) | 137 (8.4) |
| Medical Staff | 399 (27.6) | 443 (28) | 434 (26.5) |
| Nursing | 259 (18.0) | 260 (16.4) | 269 (16.4) |
| Patient Coordinators | 100 (6.9) | 117 (7.4) | 126 (7.7) |
| Supportive Care | 87 (6.0) | 105 (6.6) | 113 (6.9) |
| Level of contact with patients | |||
| Direct | 752 (52.0) | 801 (50.5) | 820 (50.0) |
| Indirect | 245 (16.1) | 282 (17.8) | 286 (17.4) |
| No patient contact | 449 (31.0) | 503 (31.7) | 535 (32.6) |
During the study period, there was a significant increase in the percentage of staff members vaccinated: 87% (1264/1446) in 2010, 92% (1453/1586) in 2011 and 96% (1583/1641) in 2012 (Figure 2, p<0.0001). Nearly all staff within differing job categories had improvements in vaccine coverage between 2010–2012, but the greatest improvements were seen in those other clinical staff (i.e. not Physicians, Physician’s Assistant, Nurse Practitioner, or Nurses), and those who were considered non-clinical personnel (e.g. administrative staff, budget, etc.) [Table 4]). The median days from start of each vaccination campaign to receipt of vaccine by employees was similar between years (2010 = 8 days, 2011 = 11, 2012 = 11, p = 0.81), and the point at which HCP reached 50% vaccine coverage occurred within the first two weeks of each campaign (2010 = 8 days, 2011 = 10, 2012 = 11, p= 0.79). In 2012, no staff opted to be vaccinated after completing the education module, as all went on to complete the entire declination process.
Figure 2.
Vaccination acceptance over the first 60 days by vaccination campaign year.
Table 4.
Percentage of healthcare personnel that receive vaccine by job category by campaign year
| 2010–2011 | 2011–2012 | 2012–2013 | |
|---|---|---|---|
| Job category | n=1446 | n=1586 | n=1641 |
| Physician | 96.4 | 97.5 | 98.8 |
| Nurse practitioner/Physician assistant | 100 | 100 | 100 |
| Nurse | 89.2 | 89.4 | 96.1 |
| Other Clinical Personnel* | 82.1 | 85.7 | 95.5 |
| Non-clinical Personnel | 84.9 | 90.1 | 92.3 |
other Clinical Personnel include staff included pharmacy, medical assistants, respiratory therapists, phlebotomy staff, etc.
When assessing differences between employees by level of patient contact, the intra-year probabilities of vaccination significantly improved between the 2010 and 2012 seasons in those with indirect and minimal patient contact groups (p < 0.0001 and p < 0.0001, respectively); no difference was seen in the direct patient care group (p =0.37) (Figure 2). When comparing HCP subgroups to each other, those with direct patient contact had significantly higher rates of vaccination to those with indirect and minimal contact for 2010 and 2011, but not in 2012 (p<0.001, <0.001, 0.24, and p<0.001, <0.001, 0.17, respectively). When those with indirect patient exposures were compared to those with minimal contact and there were no significant differences between any of the strategy years (p=0.76, 0.82, 1, respectively).
Vaccine Converters, New Decliners and Non-compliance
There was a non-significant increase in the percentage of vaccine converters when comparing the 2011 incentive strategy (49/132 [37.1%]) and the 2012 penalty-based strategy (36/71 [50.7%], p=0.074). Additionally, the number of HCP that were considered new decliners significantly decreased when comparing the 2011 campaign year (13/930 [1.4%]) and the 2012 campaign year (5/1081 [0.46%], p=0.032). The number of non-compliant staff declined during each season (2010: 26/1446 [1.7%], 2011: 2/1586 [<1%], and 2012: 0/1641 [0%]).
Discussion
In this study we set out to determine if either an incentive (“carrot”) or penalty-driven (“stick”) HCP influenza vaccine strategy could significantly improve influenza vaccination rates at our large outpatient cancer center. These data from influenza programs from 2010–2012 demonstrated that a penalty-based program (“stick”) was significantly better than an incentive-based strategy (“carrot”) for improving vaccination compliance. Major shifts in compliance based on this penalty-based program were seen among staff without direct patient care responsibilities, and appeared to be linked to the challenges of declining rather than educational components. These data demonstrate that even in an environment with high baseline compliance, we were able to improve our vaccination rates to >95% without the need for mandatory policies.
HCP vaccination has been made part of national patient safety priorities for healthcare centers.4,7 Vaccination of HCPs are an important part of respiratory virus prevention plans and are thought to help mitigate nosocomial transmission of influenza.8–11 For these reasons, Infection Prevention and Occupational Health programs are charged with developing programs that maximize vaccination rates within healthcare organizations. Such strategies for enhancing vaccination levels among healthcare institutions generally target two basic behavioral motivators: penalty (“stick”) and incentive-driven (“carrot”).12,13
A recent national survey of US hospitals found the most common penalty for vaccine refusal was to require unvaccinated staff to wear a surgical mask for the entire influenza season.14 Penalty-driven systems may also include dismissal or reassignment of HCP who are unwilling to undergo influenza vaccination. The literature often classifies both employment termination and mask accommodation policies as mandatory vaccination strategies.15,16 Such practices have been credited for improving influenza vaccination rates to above 95% compliance in many institutions.17,18
In contrast, proponents for incentive-based vaccination strategies argue that a system centered on penalties will weaken trust and decrease immunization participation.19 Incentive-based strategies are based on increasing awareness, understanding importance, and providing access to vaccine.20 Fewer studies have been published on incentive-based systems.17,21 Successes in this arena have fluctuated, but most centers have struggled to produce significant and sustainable increases in vaccine acceptance rates based solely on an incentive-based systems.18 Although recent studies argue against the use of incentives, suggesting the most important factor related to HCP vaccination are consequences for noncompliance13, few studies have compared these two approaches.
After three years of stable vaccine rates in our HCP, the Infection Prevention department evaluated different strategies to improve upon our high baseline influenza vaccine compliance rates. Mandatory vaccine policies were considered but not pursued. Masking decliners was not implemented as this was in conflict with our center’s employee sick policy which does not allow masks to be worn by staff to prevent employees from coming to work sick.22 Studies have also shown that masks negatively affect patient and caregiver interactions23, and such policies were also thought to potentially increase anxiety in patients at highest risk for respiratory virus complications. Our study instead evaluated two non-mandatory vaccination policies, one that offered incentives, and another that implemented an active declination process as our primary consequence for refusing vaccination.
Our incentive-based program in 2011 did demonstrate a moderate, 4% increase from baseline, but did not meet our pre-defined goal of >95% vaccination compliance. The following year, in 2012, we initiated a penalty-based program.5 This “stick” program required completion of influenza targeted education and an in-person declination process following one-on-one counseling with Occupational Health and Infection Prevention staff, essentially making the process of declination an active rather than a passive process. By promoting an increased focus on education and counseling this policy also addressed many of the major arguments for incentive policies, while avoiding associated incentive costs. Additionally, the effort and time needed to decline required multiple steps, planning and organization for these employees. This strategy produced a significant 9% increase in vaccine rates when compared to the baseline year, significantly increased vaccination rates when compared to our incentive-based strategy, and met our predetermined goal of >95% vaccine compliance. Data from our 2013 campaign using the same program, maintained stable vaccination rates over 95% (data not shown), indicating that such programs can also maintain high levels of compliance.
Importantly, our study found that the major improvements in vaccination rates with the penalty-driven strategy occurred in employees who did not have direct patient care responsibilities. Most vaccine strategies and studies of HCP are aimed at those that provide clinical care, although non-clinical staff are commonly found in both outpatient and inpatient environments. Since transmission can occur within 6 feet of persons infected with influenza25, non-clinical staff, even those with minimal exposure to patients, are capable of transmitting influenza when in close proximity through common areas within ambulatory clinics (e.g. waiting rooms, offices, elevators, cafeteria, etc.). Efforts to improve vaccine rates in non-clinical staff are important, and such penalty-driven strategies may provide motivation for these individuals. Interestingly, although the implementation of influenza education within the organization likely raised awareness in staff with limited patient exposures and knowledge about the benefits of vaccination, no staff underwent vaccination after completing the educational component of the policy. This suggests that the main effect was either the time burden of declining (the penalty), and or the requirement for active face-to-face declination with Infection Prevention and Occupational Health staff. Overall our center had high compliance rates, as vaccination rates achieved at our center for all three influenza seasons exceeded reported national vaccination rates among ambulatory HCPs (Table 4).24
It is also possible, that the duration of the campaign may have been another factor in the improved vaccine compliance. Our baseline study year (2010) included an open-ended vaccination deadline, while required compliance dates were set for study years 2011 and 2012. Shortened influenza vaccine campaigns can have substantial benefit for Occupational Health and Infection Prevention Departments, easing program time commitment and encouraging early vaccine uptake. Additionally, setting short deadlines improved tracking of employees, allowing Infection Prevention and Occupational Health staff to address HCPs who had not yet received or declined vaccination late in the season and avoid employee non-compliance. Interestingly, we found that regardless of vaccination program strategy, 50% of employees received vaccine in the first 14 days of each vaccine campaign. Understanding such timing and trends in HCP vaccination can also help ambulatory centers to better understand where and when to apply their limited resources and staff.
Our study has several important limitations. Since these vaccine campaigns occurred in succession of each other, there is the possibility that the high vaccine rates identified during the 2012 penalty-based campaign, were, in part, due to a cumulative effect of efforts to improve vaccination each year; such improvements have been seen nationally.24 Over the course of the study, each vaccine campaigns included multiple strategies and substantial overlap in many of the approaches, making it difficult to measure the specific effectiveness of all components of the strategies. As such, there is also the chance other unmeasured portions of these strategies impacted overall vaccination rates. It is also possible that the monetary incentive chosen for our 2011 campaign was too small to motivate change, but such data are difficult to gauge, may vary by individual and increase overall costs. More importantly, we could not address individual incentives which may have greater impact on personal vaccine choices than those that required system-wide improvements as described in this study. Fluctuating seasonal patterns and severity of influenza, may have affected rates of overall vaccine compliance in each strategy, and more importantly limited our ability to assess the impact that increased vaccination had on influenza rates in patients. Most importantly, it is difficult to know whether the vaccine strategies implemented at our center would produce an equivalent result in another healthcare organization/ambulatory clinic, particularly those with lower baseline rates of vaccine compliance.
Conclusions
Our study demonstrates that a non-mandatory, penalty-based (“stick”) influenza vaccine campaign produced the highest vaccination compliance rates. This policy allowed the center to reach >95% vaccination rates among staff and strongly supports the idea that penalty driven (“stick”) approaches to vaccination campaigns are more effective in raising the level of vaccination acceptance than incentive-based methods. The “stick” approach had the greatest impact on non-clinical staff and appeared to be driven by the penalty and or the active declination process, and not the incorporation of mandatory education. This low cost, time-limited vaccine strategy may provide centers with an effective alternate to mandatory vaccination.
Figure 3.
Comparison of vaccine acceptance by level of patient contact stratified by patient year.
Highlights.
Influenza vaccination of healthcare workers is of major importance at cancer centers.
We compared three influenza vaccine strategies at a center with high baseline vaccine compliance.
A penalty-based staff vaccination program was more effective than one offering incentives.
Improvements in vaccination rates were driven by staff without direct care responsibilities
System-wide influenza vaccination can be achieved without requiring mandatory vaccination.
Acknowledgments
Financial Support: S.A.P. is supported by NIH grant K23HL096831 and by the Washington Vaccine Alliance. C.C. is supported by NIH grant P30 CA015704
The authors would like to thank John Lynch, MD and Estella Whimbey, MD for their assistance in developing this healthcare worker vaccine program, and to the center’s dedicated Employee Health & Safety Staff.
Footnotes
Presentation of material in submitted manuscript: Data from this manuscript have been presented in part at Infectious Diseases Week 2013 in San Francisco, CA in October, 2013.
Disclosure of Conflicts of Interest: S.A.P. has received research support and has been a consultant from Merck and Optimer/Cubist Pharmaceuticals. C.C. has received research support and has been a consultant for Janssen Pharmaceuticals and is a member of the Scientific Advisory Board of Glaxo Smith Kline and TempTime.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Memoli M, Athota R. The Natural History of Influenza Infection in the Severely Immunocompromised vs Nonimmunocompromised Hosts. Clin Infect Dis. 2014:1–28. doi: 10.1093/cid/cit725. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Ljungman P, Avetisyan G. Influenza vaccination in hematopoietic SCT recipients. Bone Marrow Transplant. 2008;42:637–641. doi: 10.1038/bmt.2008.264. [DOI] [PubMed] [Google Scholar]
- 3.Baluch A, Pasikhova Y. Influenza vaccination in oncology patients. Curr Infect Dis Rep. 2013;15(6):486–90. doi: 10.1007/s11908-013-0368-7. [DOI] [PubMed] [Google Scholar]
- 4.Fiore AE, Shay DK, Broder K, et al. Prevention and control of seasonal influenza with vaccines: recommendations of the Advisory Committee on Immunization Practices (ACIP), 2009. MMWR Recomm Rep. 2009;58(RR-8):1–52. [PubMed] [Google Scholar]
- 5.Lynch J, Whimbey E, Mertens K, et al. ID Week. San Diego, CA: 2012. Abstract High Level Influenza Vaccination of Healthcare Workers using One-on-one Education. (abstract 449) Available at: https://idsa.confex.com/idsa/2012/webprogram/Paper37712.html. [Google Scholar]
- 6.R Core Team. R: A Language and Environment for Statistical Computing. 2014. [Google Scholar]
- 7.Immunization of health-care personnel: recommendations of the Advisory Committee on Immunization Practices (ACIP) [Accessed July 17, 2014];MMWR RecommRep. 2011 60(RR-7):1–45. Available at: http://www.ncbi.nlm.nih.gov/pubmed/22108587. [PubMed] [Google Scholar]
- 8.Nichol KL, D’Heilly SJ, Greenberg ME, Ehlinger E. Burden of influenza-like illness and effectiveness of influenza vaccination among working adults aged 50–64 years. Clin Infect Dis. 2009;48(3):292–8. doi: 10.1086/595842. [DOI] [PubMed] [Google Scholar]
- 9.Boulay BR, Murray CJ, Ptak J, Kirkland KB, Montero J, Talbot EA. An outbreak of pertussis in a hematology-oncology care unit: implications for adult vaccination policy. Infect Control Hosp Epidemiol. 2006;27:92–95. doi: 10.1086/500420. [DOI] [PubMed] [Google Scholar]
- 10.LaVela SL, Smith B, Weaver FM, Legro MW, Goldstein B, Nichol K. Attitudes and practices regarding influenza vaccination among healthcare workers providing services to individuals with spinal cord injuries and disorders. Infect Control Hosp Epidemiol. 2004;25:933–940. doi: 10.1086/502323. [DOI] [PubMed] [Google Scholar]
- 11.Lobo RD, Oliveira MS, Garcia CP, Caiaffa Filho HH, Levin AS. Pandemic 2009 H1N1 influenza among health care workers. Am J Infect Control. 2013;41(7):645–7. doi: 10.1016/j.ajic.2012.08.012. [DOI] [PubMed] [Google Scholar]
- 12.Salgado CD, Giannetta ET, Hayden FG, Farr BM. Preventing nosocomial influenza by improving the vaccine acceptance rate of clinicians. Infect Control Hosp Epidemiol. 2004;25(11):923–8. doi: 10.1086/502321. [DOI] [PubMed] [Google Scholar]
- 13.Hayward AC, Harling R, Wetten S, et al. Effectiveness of an influenza vaccine programme for care home staff to prevent death, morbidity, and health service use among residents: cluster randomised controlled trial. BMJ. 2006;333(7581):1241. doi: 10.1136/bmj.39010.581354.55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Heimberger T, Chang HG, Shaikh M, Crotty L, Morse D, Birkhead G. Knowledge and attitudes of healthcare workers about influenza: why are they not getting vaccinated? Infect Control Hosp Epidemiol. 1995;16(7):412–5. doi: 10.1086/647139. [DOI] [PubMed] [Google Scholar]
- 15.Miller BL, Ahmed F, Lindley MC, Wortley PM. Institutional requirements for influenza vaccination of healthcare personnel: results from a nationally representative survey of acute care hospitals--United States, 2011. Clin Infect Dis. 2011;53(11):1051–9. doi: 10.1093/cid/cir633. [DOI] [PubMed] [Google Scholar]
- 16.Babcock HM, Gemeinhart N, Jones M, Dunagan WC, Woeltje KF. Mandatory influenza vaccination of health care workers: translating policy to practice. Clin Infect Dis. 2010;50(4):459–64. doi: 10.1086/650752. [DOI] [PubMed] [Google Scholar]
- 17.Rebmann T, Wright KS, Anthony J, Knaup RC, Peters EB. Seasonal Influenza Vaccine Compliance among Hospital-Based and Nonhospital-Based Healthcare Workers. Infect Control Hosp Epidemiol. 2012;33:243–249. doi: 10.1086/664057. [DOI] [PubMed] [Google Scholar]
- 18.Poland GA. Mandating influenza vaccination for health care workers: putting patients and professional ethics over personal preference. [Accessed July 30, 2013];Vaccine. 2010 28(36):5757–9. doi: 10.1016/j.vaccine.2010.07.057. Available at: http://www.ncbi.nlm.nih.gov/pubmed/20705206. [DOI] [PubMed] [Google Scholar]
- 19.Zimmerman RK, Lin CJ, Raymund M, Bialor J, Sweeney PM, Nowalk MP. Hospital policies, state laws, and healthcare worker influenza vaccination rates. Infect Control Hosp Epidemiol. 2013;34(8):854–7. doi: 10.1086/671265. [DOI] [PubMed] [Google Scholar]
- 20.Lam P, Chambers LW, MacDougall DMP, McCarthy AE. Seasonal influenza vaccination campaigns for health care personnel: systematic review. CMAJ. 2010;182(12):E542–8. doi: 10.1503/cmaj.091304. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Lugo NR. Will carrots or sticks raise influenza immunization rates of health care personnel? Am J Infect Control. 2007;35:1–6. doi: 10.1016/j.ajic.2006.10.004. [DOI] [PubMed] [Google Scholar]
- 22.Chu HY, Englund JA, Podczervinski S, et al. Nosocomial transmission of respiratory syncytial virus in an outpatient cancer center. Biol Blood Marrow Transplant. 2014;20(6):844–51. doi: 10.1016/j.bbmt.2014.02.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Wong CKM, Yip BHK, Mercer S, et al. Effect of facemasks on empathy and relational continuity: a randomised controlled trial in primary care. BMC Fam Pract. 2013;14:200. doi: 10.1186/1471-2296-14-200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Centers for Disease Control. Influenza Vaccination Coverage Among Health-Care Personnel -- United States, 2012–2013 Influenza Season. MMWR Morb Mortal Wkly Rep. 2013;62(38):781–786. [PMC free article] [PubMed] [Google Scholar]
- 25.Nowalk MP, Lin CJ, Raymund M, Bialor J, Zimmerman RK. Impact of hospital policies on health care workers’ influenza vaccination rates. Am J Infect Control. 2013;41(8):697–701. doi: 10.1016/j.ajic.2012.11.011. [DOI] [PubMed] [Google Scholar]