Abstract
Background
This research examines student evaluations of their experience and attitudes in an 11 week mind-body skills course for first year medical students.
Aims
The aim is to understand the impact of this course on students’ self-awareness, self-reflection, and self-care as part of their medical education experience.
Methods
This study uses a qualitative content analysis approach to data analysis. The data are 492 verbatim responses from 82 students to six open-ended questions about the students’ experiences and attitudes after a mind-body skills course. These questions queried students’ attitudes about mind-body medicine, complementary medicine, and their future as physicians using these approaches.
Results
The data revealed five central themes in students’ responses: connections, self discovery, stress relief, learning, and medical education.
Conclusions
Mind-body skills groups represent an experiential approach to teaching mind-body techniques that can enable students to achieve self-awareness and self-reflection in order to engage in self-care and to gain exposure to mind-body medicine while in medical school.
Introduction
Medical school is a challenging environment in which students are confronted with multiple psychological and physical stressors; teaching students how to deal with these stressors is important for their health and well-being. Training physicians to focus on self-awareness, self-reflection and self-care may produce more reflective and well balanced doctors who may provide better patient care.
One approach to helping students to deal with the stressors of medical school focuses on teaching mind-body skills (MBS) that promote self-awareness, self-reflection and self-care. While medical teaching on self-reflection and professionalism is more wide spread in the UK (Maudsley & Fryer-Edwards 2003), curricula focusing on MBS and the promotion of self-awareness and self-reflection is less well established in medical schools in the United States (Dannoff & Corbet 2005). The learning objectives of self-awareness and reflection are often challenging to integrate into a medical school curriculum and equally difficult to assess (Boenink et al. 2004). There have been a variety of interventions employed to help students alleviate stress, promote well-being and self-reflection, this paper describes the results of an experiential intervention focusing on MBS techniques to achieve these outcomes.
Medical students have been surveyed about the physical and psychological challenges of medical school since the early 1970s (Pitts et al. 1961; Linn & Zeppa 1984; Firth 1986; Wolf 1989; Mosley et al. 1994; Stewart et al. 1997). Findings of increased stress levels have motivated a variety of interventions designed to provide sensitivity training (Dashef et al. 1974; Hilberman et al. 1975), self-awareness (Cadden et al. 1969), self-reflection (Killion & Todnem 1991; Maudsley & Fryer-Edwards 2003; Boenink et al. 2004), sharing of feelings and well-being (Dashef et al. 1974; Coombs & Virshup 1994) discussion of roles as a physician improvement in health habits (Ball & Bax, 2002) and emotional competence (Flowers 2005) as mechanisms for reducing stress and improving coping skills. Observed outcomes included greater awareness of emotional issues in students, improved faculty/student communication (Cadden et al. 1969), less personal isolation and more sensitivity in communication among classmates (Dashef et al. 1974). As reported in a review article, Shapiro et al. (2000) indicates that there are a number of observed outcomes both biological and psychological including improved immunologic functioning, decreases in depression and anxiety, increased spirituality and empathy, enhanced knowledge of alternative therapies for future referrals, improved knowledge of the effects of stress, greater use of positive coping skills, and the ability to resolve role conflicts (Shapiro et al. 2000).
There have been several studies of mind-body interventions with medical students. Shapiro et al. (1998) studied a mind-body intervention named mindfulness-based stress reduction (MBSR) in medical and pre-medical students. Their findings showed a reduction in self-reported state and trait anxiety, and in the reports of overall psychological distress including depression as well as increased empathy score levels. The effects were sustained during the exam-period as compared to a wait list control group. Rosenzweig et al. (2003) examined how a MBSR intervention improved coping skills and reduced emotional distress in medical students, resulting in lower total mood disturbance scores, and improved tension-anxiety, confusion-bewilderment, fatigue-inertia, and vigor-activity measures. The body of research on the stressors of medical school underlies the importance of reforming the medical school curriculum to include MBS to help students manage the stressors they may experience.
The curricular initiative at Georgetown University School of Medicine (GUSOM), originally developed at The Center for Mind Body Medicine (CMBM) in Washington, DC (Gordon et al. 2004) focuses on MBS. This program concentrates on teaching skills that make use of connections among the brain, mind, body, and behavior, and on the powerful ways in which emotional, mental, social, and spiritual awareness promotes health and well-being. It regards as fundamental an approach that respects and enhances each person’s capacity for self-knowledge and self-care, and it emphasizes techniques that are grounded in this approach. Self-awareness is defined as students’ understanding of how their personal histories and current personal lives, as well as their values, attitudes, and biases, affect their care of patients, so that they can use their emotional responses in patient care to their own and their patients benefit. Self-care is defined as the students’ ability to care for themselves physically and emotionally (Novack et al. 1999). Self-reflection is a conscious thought process that enables individuals to correct beliefs and leads to revised interpretations of experiences and new behaviors (Mezirow 1990). MBS focus attention on the relationship between the brain, mind, and body through specific techniques such as meditation, relaxation, and guided imagery to affect psychological and physiological functioning (Pelletier 1992; Gordon 1996; Benson & Klipper 2000).
Reports of teaching complementary and alternative medicine (CAM) in U.S. medical schools have shown a rising trend from 75 schools in 1998 (Wetzel et al. 2003) to 98 schools in 2002–2003 (Barzansky & Etzel 2003). This trend is reflected in a recent report of the Institute of Medicine on CAM in the United States (IOM Report 2005) which underlines the importance of both education as well as research on CAM and names self care as an important component of CAM. However, only a handful of schools that are teaching CAM actually include specific courses on mind-body medicine or self-awareness. There may be a variety of reasons for the paucity of MBS in medical education including the resource intense nature of the teaching methods and the challenging nature of the assessment for skills such as self-awareness and self-reflection as well as the historical divide between complementary medicine and more traditional medical paradigms. The research and pedagogy on stress reduction and self-awareness promotion for medical students is still in its infancy. The research presented here illustrates students’ attitudes towards an experiential approach to learning mind-body skills techniques.
Methods
Development of mind body skills program
GUSOM was awarded an educational curriculum grant by the National Center for Complementary and Alternative Medicine (NCCAM) in 2001, in order to develop a program to integrate CAM and mind-body medicine (MBM) knowledge, skills, and attitudes into the undergraduate medical curriculum. An elective 11-week MBS course was designed to give students the opportunity to learn about and practice a variety of specific mind-body skills including: relaxation techniques; slow, deep breathing; autogenic training; biofeedback; guided imagery; and several forms of meditation as well as to use drawings and written exercises for self-awareness and self expression. The GUSOM faculty who were selected to lead the groups were trained by CMBM and initially supervised by CMBM trainers.
Starting in 2002, first year medical students were invited to apply to take the 11-week MBS course. Admission into the elective course was based on each student writing an email specifying why the student wanted to take the course. On average approximately 30% of the first year students apply to take the elective each year. All students who applied were accommodated into the elective. The course was offered during the second semester of the first year in order to introduce these MBS early in medical training, concurrent with basic science courses, and while students’ attitudes towards medicine were still in the formative stages.
Structure of mind body skills groups
MBS groups are comprised of 8–12 students led by two faculty facilitators for two hours each week. The MBS curriculum follows a specific format (see Figure 1) for each meeting beginning with an opening ritual (e.g., lighting a candle, meditation, ringing a chime). The next step is called the ‘check-in’ during which each member, including the facilitators, share insights about their personal self-discovery. For example, one might share details of daily experiences or more intimate thoughts and feelings. The opening ritual and check-in often take about one hour. Next, the facilitators introduce one mind-body skill with a brief rationale and the specifics of the technique. After this description, the group will practice this MBS (e.g., a drawing or journaling exercise). Following the practice, each member of the group is asked (but not compelled) to share aspects of the drawing or journal with the rest of the group to process the experience. Each session ends with a closing ritual or meditation. The second part of the session usually takes an hour as well.
Figure 1.
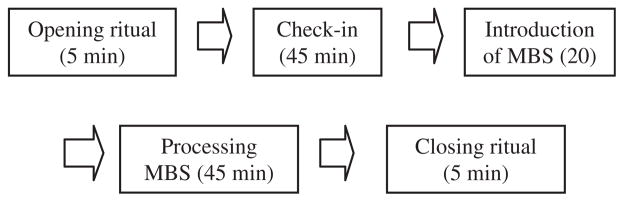
Structure of mind-body skills group session.
At the end of the 11-week program, students in the MBS course complete a packet of self-report questionnaires including six open-ended questions about the MBS course experience. This study focuses on these six open-ended questions developed by the research team at Georgetown to gain information about self discovery and stress reduction. Responses to open-ended questions are analysed using qualitative content analysis (Neuendorf 2002).
Subject demographics
We analysed open-ended questions from 82 students from the first three semesters of this program (Fall 2002, n =15, Spring 2002, n =25, and Spring 2003, n =42). In each semester the students were predominately female and all were first year students. While information on age was not collected for these specific students, the average age of the first year class is 23.1 years of age. The same six open-ended questions were administered to students at the end of the MBS course. The questions focused on students’ attitudes towards mind-body skills, complementary medicine, and the potential future use of these approaches by students as physicians. Open-ended questions allow for students to reflect on their experience and to describe the development of self-awareness. The questions are presented in Table 1.
Table 1.
List of open-ended questions.
| Open-ended questions |
|---|
| Q1. What did this course mean to you? |
| Q2. Has the course helped you as a medical student and as a person? If so, how? |
| Q3. Do you believe that it will contribute to your work as a physician? If so, how? |
| Q4. Has it changed your attitude toward medicine and healthcare? If so, how? |
| Q5. Has it changed your attitude toward medical school? If so, how? |
| Q6. Has it changed your relationship with your classmates? |
Analysis method
All responses were transcribed verbatim from survey forms to a qualitative analysis software program called NVivo (NVivo 1999–2003). This program is a database for sorting textual data by demographic dimensions such as gender or age as well as content-related themes. The analyst/coder read the textual data and coded each textual unit according to demographic or contextual dimensions. The analysis proceeded in a manner motivated by qualitative content analysis (Neuendorf 2002). That is, the coder read through the data and developed an initial set of relevant themes. The research team reviewed this initial list of themes and a consensus was obtained for a working list. The analyst then coded all the textual data according to this working list. Once all the data were coded the research team met again to review approximately 10% of the textual examples randomly selected from the 492 responses. When research team members and the coder did not agree on a classification of a response, a consensus classification was determined and all data falling into the original classification were recoded to reflect the consensus.
The qualitative analysis proceeded by a careful reading of the written responses. When a thematic grouping emerged, such as ‘connections’ or ‘learning’ it was called a ‘central theme’. When more than ten responses reflected a similar thread, this was established as a theme in the initial list. Themes were easily identifiable for each question, i.e., generally, students tended to respond along the same lines to each question. Often within a central theme, a sub-set of responses grouped together as a sub-theme, such as ‘isolation’ as part of ‘feeling connection with other students’. In addition to central and sub-themes, another category to emerge was ‘question-specific’ themes. Several open-ended questions consistently yielded very specific responses that directly answered the question that was asked. For example, most responses to the question ‘has this course changed your attitude towards medical school?’ were very direct and did not fall into a broader thematic category.
Results
A total of 492 responses from 82 individuals to six questions were analysed, yielding five central thematic categories: (1) connections, (2) self discovery, (3) learning, (4) stress relief, and (5) medical education. These themes were considered central because they appeared in student responses across the six open ended questions (i.e., not limited to one question). These central themes engendered a variety of sub-themes, as described below. In addition to these central and sub-themes, three question-specific themes were also identified. These three question-specific themes are (6) problems in health care, (7) awareness of CAM, and (8) attitudes towards medical school.
Central and sub-themes
1. Connections
This central theme captures students’ appreciation of the opportunity provided by the MBS group to meet other students and to make a meaningful connection. Many students expressed feeling isolated and alone in their medical school experience. They stated that the MBS group helped dispel these feelings, allowing them to get to know classmates they would not otherwise have a chance to meet due to differences in schedules, background and interests. The theme of connections includes several sub-themes: opportunity to express feelings, shared attitudes, and relationships.
Opportunity to express feelings
This sub-theme is evidenced in students’ experience of the MBS group as an opportunity to express their feelings. Students felt that the MBS group provided a safe place for students to express their feelings and share thoughts and ideas about themselves. Sharing in this non-judgmental setting appeared to be a powerful experience for these students. Expression of feelings about their medical school experience provided a much-needed outlet, as exemplified in the following example, where one student described her experience in the group as a valuable opportunity to discuss feelings:
It was an opportunity to talk amongst my peers as well as to practice the skills learned in class. I also found that I was more willing to share my emotions by the end of the course.
Shared attitudes
The second sub-theme relates to students learning how they are similar and different from their classmates. Understanding the similarities among themselves led to a sense of connection for these students. Students agreed that they do not get many opportunities to learn about their classmates in the regular class settings. One student expressed this sentiment in the following way:
I have realized that I’m not alone in my fears to succeed in med school, and the insecurities and self-doubts that have plagued me on and off this first year. I realize everyone faces these issues as they come up. We are never really alone, and this is a fact that we as a society need to become more aware of.
Relationships
The final sub-theme for connections reflects a basic need for people to connect to others in their lives. Students expressed the sense that sharing and learning about others was important, and that the medical school context is no exception to that rule. Students felt the MBS group provided an opportunity to connect with other people. One student described her experience as follows:
Yes. I have been trying via therapy and this group to learn to be better to myself. Part of that means having people to lean on, people who care about me too.
2. Self discovery
This second central theme reveals a process of self discovery stemming from students’ experience in the MBS group. They reported that the MBS group helped them to become more aware of their own priorities and limitations and enhanced their ability to be better people. Sub-themes of self discovery identified issues of changing priorities, reaffirmation, and the need to be open-minded.
Changing priorities
The first sub-theme arose from student reports that participating in the MBS group allowed them to change their priorities about their lifestyle and about their approach to being a medical student. One student expressed how the MBS group allowed her to see a disconnection between her own basic thoughts, feelings, and actions.
I feel that I have reached new levels of understanding myself, and in that vein I am painfully aware of the giant disconnect between my intentions and feelings and my actions. So, in that way, I can see more clearly what I need to do in my life.
Reaffirmation
The second sub-theme reflects the process of reaffirmation of currently held beliefs and practices. Students found that their experience in the MBS group clarified their current thoughts and feelings and helped them to refocus on attitudes and practices they had previously found to be helpful in their lives. One student described how the group experience reaffirmed her practice of exercise and meditation and introspection.
It has made me more dedicated to doing certain things I know I should be doing-exercise, meditation, etc. and although I’m usually somewhat introspective it has made me introspective in other areas.
Opened mindedness
Students’ statements about being more open minded yielded the third sub-theme of self discovery. These included open-mindedness about alternative therapies including the knowledge and skills of mind-body medicine (MBM) as well open mindedness toward other people. In this first example, one student explained that the MBS group helped him to be more open minded towards alternative therapies and open to new mind-body techniques.
It has broadened my perspective on new and unorthodox treatments (which might soon become more orthodox than not) to offer to patients as well as increasing my understanding of the interplay between the nervous, endocrine, immune, and organ systems. As a person, it has shown me new relaxation techniques.
3. Learning
The third central theme encompasses a variety of responses in which students expressed appreciation for what they learned during their MBS group. The sub-themes of learning are: learning mind-body skills and learning academic material.
Learning M-B skills
The first sub-theme reflects the core objectives of the MBS program. The MBS course presented instruction in meditation, autogenics and biofeedback, guided imagery, and journaling. Students described how these skills were useful and applicable in their daily life.
Yes! I listen to my body more; I’m more attentive to my state of mind. I feel that I have more control over myself.
Academic improvement
The second sub-theme highlights the relationship between the use of MBS and better performance in school. Students identified that a clear benefit of the MBS groups was learning skills which helped them to relax and thus perform better in school.
As a medical student, this course taught me ways to relax and focus. I actually have improved on my tests while reducing study time. Whether I have become more efficient at studying, a better test-taker, or simply more focused I am not sure. I like to think it is because I am more self-aware and relaxed-which is more important for my everyday existence as a person.
4. Stress relief
The fourth central theme describes students’ feelings that the MBS group provided them with a much-needed relief from the stresses of medical school. Students stated that the MBS group helped them physically and emotionally. They reported a positive impact on their academic and personal lives due to reduced stress levels. They saw the benefit in their personal and professional relationships.
This course has been about self-awareness for me. I have learned to better recognize what is going on for me physically and emotionally. I have also learned a new set of tools for dealing with the stresses in life.
5. Medical education
The final central theme arising from student responses was the broad appreciation and consciousness that the MBS group is a unique experience and a particularly valuable part of their medical education, one not generally available at other medical schools. Students lamented the paucity of courses with the mind-body medicine approach at GUSOM and expressed the hope that more MBM and CAM courses would be offered to them in the future.
It has made me more cognizant of the fact that med school as an environment does not foster healthy emotional life (…) as a normal quality. It has also made clear to me that I am responsible for my own relaxation during these years.
Question-specific themes
In addition to the five central themes, there are three themes which characterize students’ specific responses to questions 4 and 5.
1. Problems in the health care system
In response to Question 4 – ‘Has it (this course) changed your attitude toward medicine and healthcare? If so, how?’ students described their concerns about the problems with the current health care system.
I fully see, now, how lacking medicine (and especially healthcare), is in the whole person approach to well-being. I also feel like more of these things could help prevent more progression of serious disease in the world.
2. Awareness of MBM and CAM
Also in response to Question 4 – Has it (this course) changed your attitude toward medicine and healthcare? If so, how? students described their new awareness of the MBM and CAM approaches. One student expressed the importance of the doctor/patient relationship as revealed to them by their experience in the MBS group.
It has enabled me to think about healthcare more holistically and as a partnership between the physician and the patient.
3. Attitudes towards medical school
In response to Question 5 – ‘Has it (this course) changed your attitude toward medical school? If so, how’? most of the responses described the connections students make and the stress relief skills they acquire. However, one student specifically described how his attitude has changed towards the entire medical school experience.
It has changed my attitude in the sense of knowing that there are people who care about my well being as a student. And because I have received, I also want to give back.
Discussion and Conclusions
First year students at GUSOM who participated in the 11-week long MBS course offered reflective and intuitive comments about their experience as students, individuals, and future physicians. The central themes of connections, self discovery, learning, stress relief, and medical education as well as the question-specific themes of problems in health care, awareness of CAM, and attitudes toward medical school suggested that the MBS groups benefited students in several ways. These included making the stress of medical school more manageable; enhancing academic performance; presenting the opportunity for self care; improving a sense of community and social support among students; and promoting an openness towards MBS and CAM.
The central themes of self discovery and stress relief supported findings of previous studies of medical student stressors (Pitts et al. 1961; Linn & Zeppa 1984; Firth 1986; Wolf 1989; Mosley et al. 1994; Stewart 1997) showing that medical students do experience physical and psychological stress. Our findings also highlighted that the MBS program allowed for opportunities for making connections and learning which also related to stress reduction.
However, the participants in these elective courses, for which no course credits were given, were highly self-selected. We are in the process of seeking to demonstrate a more generalizable effect of the MBS experience on self-awareness and reflection for medical students in general, and in particular whether this translates to longer term outcomes such as professionalism and self-care. For example, a variety of for-credit courses focused on self-reflection and self-awareness, using MB skills techniques will be developed in the coming years for students throughout the undergraduate medical school curriculum at GUSOM.
Self-awareness and personal development are central goals of the growing MBS program at GUSOM. Student responses to open-ended questions about their experiences during the course point to heightened self-awareness and a greater understanding of the importance of self-care as well as development of coping skills to deal with the demands of medical school. Our results in this highly specific subpopula-tion of first year medical students suggest that MBS groups are a valuable and highly valued experiential approach to teaching and promoting self-awareness, self-reflection and self-care with an added benefit of an increased awareness of the effectiveness MBS and CAM modalities during the four years of the undergraduate medical school experience.
Acknowledgments
This research was supported by an educational curriculum grant (R25 AT 00419) from the National Center for Complementary and Alternative Medicine (NCCAM-NIH); M01 RR13297 from the National Center for Research Resources and NIMH 1 P20 MH068450 from the National Institute of Mental Health.
Biographies
Dr. PAMELA A. SAUNDERS is an Assistant Professor in the Neurology Department at Georgetown University School of Medicine. Her research interests include communication, aging, and Alzheimer’s disease. She has authored several articles on doctor/older patient communication. Currently, she is implementing curriculum with medical students about how to communicate with older patients.
Dr. ROCHELLE E. TRACTENBERG is an Assistant Professor in the Departments of Neurology, Biostatistics, and Psychiatry at Georgetown University School of Medicine. Her research interests include teaching and learning in post-baccalaureate education. She is the Director of Curriculum for a federally-funded Clinical Research Education program at Georgetown.
RANJANA CHATERJI received her M.S. in Physiology and Biophysics from Georgetown University and a B.S. in Biology from The Pennsylvania State University. She was employed by GUSOM as a Project Assistant for the CAM Educational Initiative for two years. Her contribution to the Initiative was developing an attitude assessment for the Mind-Body Medicine Program. In addition to data collection and survey design, she presented a poster and oral presentation at the AAMC Research In Medical Education Conference in 2003.
Dr. HAKIMA AMRI is Assistant Professor in the Physiology and Biophysics Departement at Georgetown University Medical Center; She is the Director of the physiology/complementary and alternative medicine Master’s program. Her research focuses on steroid metabolism in health and disease and the mechanisms of action of herbal products. Her research is funded by grants from NIH and the Samueli Institute.
NANCY HARAZDUK is an Adjunct Assistant Professor and the Director of the Mind-Body Medicine Program at Georgetown University School of Medicine. To integrate Mind-Body Medicine into the medical school curriculum, she conducts Mind-Body Medicine classes for first, second and third year medical students. As a presenter, facilitator and supervisor, Ms Harazduk has trained many health care professionals in Mind-Body Medicine. She maintains a psychotherapy practice specializing in Mind-Body Medicine therapies in Chevy Chase, Maryland.
JAMES S. GORDON, MD, is the Founder and Director of The Center for Mind-Body Medicine in Washington D.C. and is a Clinical Professor in the Departments of Psychiatry and Family Medicine at the Georgetown University School of Medicine. He and his colleagues developed the model of psychological self-care and self-expression, mind-body skills and group support that is described in this study and have been using it for 13 years with people with chronic illness and war traumatized populations in Bosnia, Kosovo Israel and Gaza.
AVIAD HARAMATI, Ph.D. is Professor and Director of Education in the Departments of Physiology & Biophysics and Medicine at Georgetown University School of Medicine. His research interests focus on two main areas: the regulation of renal and electrolyte physiology during growth; and the cardiovascular-renal-endocrine regulation of volume homeostasis in heart failure. Dr. Haramati was the principal investigator of a $ 1.7 million NIH grant that is funding a broad educational initiative aimed at incorporating complementary, alternative (CAM) and integrative medicine into the 4-year medical curriculum at Georgetown.
MICHAEL LUMPKIN teaches both medical students and lay audiences about all aspects of euroendicronology, neuroimmunology, stress and their associated disease states. His physiology laboratory primarily conducts studies in examining the regulatory relationships between the brain, endocrine glands, and the immune cells of the body, examining how stress or stressors disrupt the brain hormone systems that govern sexuality, growth, metabolism, and immunity, thereby causing chronic disease. He has extended these scientific investigations into understanding how certain complementary medications and mind-body techniques reduce stress and improve the hormonal and immune status of the body. Dr. Lumpkin also discovered and patented the use of a peptide hormone receptor binding compound to block the damaging effects of the HIV/AIDS virus on nerve cells in the hypothalamus of the brain and on cells of the pituitary gland.
References
- Ball S, Bax A. Self-care in medical education: Effectiveness of health-habits interventions for first-year medical students. Acad Med. 2002;77:911–917. doi: 10.1097/00001888-200209000-00023. [DOI] [PubMed] [Google Scholar]
- Barzansky B, Etzel SI. Educational programs in us medical schools, 2002–2003. J Amer Med Ass. 2003;290:1190–1196. doi: 10.1001/jama.290.9.1190. [DOI] [PubMed] [Google Scholar]
- Benson H, Klipper M. The Relaxation Response. New York: Harper Torch; 2000. [Google Scholar]
- Boenink AD, Oderwald AK, De Jonge P, Van Tilburg W, Smal JA. Assessing student reflection in medical practice. The development of an observer-rated instrument: Reliability, validity and initial experiences. Med Educ. 2004;38:368–377. doi: 10.1046/j.1365-2923.2004.01787.x. [DOI] [PubMed] [Google Scholar]
- Cadden JJ, Flach FF, Blakeslee S, Charlton RJR. Growth in medical students through group process. Amer J Psychiat. 1969;126:862–868. doi: 10.1176/ajp.126.6.862. [DOI] [PubMed] [Google Scholar]
- Coombs R, Virshup B. Enhancing the psychological health of medical students: The student well-being committee. Med Educ. 1994;28:47–54. doi: 10.1111/j.1365-2923.1994.tb02684.x. [DOI] [PubMed] [Google Scholar]
- Danoff D, Corbett E. Recommendations for clinical skills curricula for undergraduate medical education: Task force on the clinical skills education of medical students. Assoc Amer Med Colleges 2005 [Google Scholar]
- Dashef SS, Espey WM, Lazarus JA. Time-limited sensitivity groups for medical students. Amer J Psychiat. 1974;131:287–292. doi: 10.1176/ajp.131.3.287. [DOI] [PubMed] [Google Scholar]
- Firth J. Levels & sources of stress in medical students. Brit Med J Clinical Res Ed. 1986;292:1177–1180. doi: 10.1136/bmj.292.6529.1177. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Flowers LK. The missing curriculum: Experience with emotional competence education and training for premedical and medical students. [see comment] J Natl Med Assoc. 2005;97:1280–1287. [PMC free article] [PubMed] [Google Scholar]
- Gordon JS. Manifesto for a New Medicine: Your Guide to Healing Partnerships and the Wise use of Alternative Therapies. New York: Perseus Books; 1996. [Google Scholar]
- Gordon JS, Staples JK, Blyta A, Bytyqi M. Treatment of posttraumatic stress disorder in postwar Kosovo high school students using mind-body skills groups: A pilot study. J Trauma Stress. 2004;17:143–147. doi: 10.1023/B:JOTS.0000022620.13209.a0. [DOI] [PubMed] [Google Scholar]
- Hilberman E, Konanc J, Perez-Reyes M, Hunter R, Scagnelli J, Sanders S. Support groups for women in medical school: A first-year program. J Med Educ. 1975;50:867–875. doi: 10.1097/00001888-197509000-00004. [DOI] [PubMed] [Google Scholar]
- Killion J, Todnem G. A process for personal theory building. Educ Leadership. 1991;48:14–16. [Google Scholar]
- Linn BS, Zeppa R. Stress in junior medical students: Relationship to personality and performance. J Med Educ. 1984;59:7–12. [PubMed] [Google Scholar]
- Maudsley G, Fryer-Edwards K. Promoting reflection on professionalism: A comparison trial of educational interventions for medical students. Acad Med. 2003;78:742–747. doi: 10.1097/00001888-200307000-00018. [DOI] [PubMed] [Google Scholar]
- Mezirow J. Fostering Critical Reflection in Adulthood: A Guide to Transformative and Emancipatory Learning. San Francisco: Jossey-Bass Publishers; 1990. [Google Scholar]
- Mosley TH, Jr, Perrin SG, Neral SM, Dubbert PM, Grothues CA, Pinto BM. Stress, coping, and well-being among third-year medical students. Acad Med. 1994;69:765–767. doi: 10.1097/00001888-199409000-00024. [DOI] [PubMed] [Google Scholar]
- Neuendorf KA. The Content Analysis Guidebook. Thousand Oaks, CA: Sage; 2002. [Google Scholar]
- Novack DH, Epstein RM, Paulsen RH. Toward creating physician-healers: Fostering medical students’ self-awareness, personal growth, and well-being. Acad Med. 1999;74:516–520. doi: 10.1097/00001888-199905000-00017. [DOI] [PubMed] [Google Scholar]
- Nvivo. Sydney: QSR International; 1999–2003. [Google Scholar]
- Pelletier K. Mind as Healer, Mind as Slayer. New York: Delacorte and Delta; 1992. [Google Scholar]
- Pitts FN, Jr, Winokur G, Stewart MA. Psychiatric syndromes, anxiety symptoms and responses to stress in medical students. Am J Psychiatry. 1961;118:333–340. doi: 10.1176/ajp.118.4.333. [DOI] [PubMed] [Google Scholar]
- IOM (Institute of Medicine Report) Complementary and alternative medicine (CAM) in the United States. The National Academies Press; Washington, DC: Institute of Medicine of the National Academies; 2005. [Google Scholar]
- Rosenzweig S, Reibel DK, Greeson JM, Brainard GC, Hojat M. Mindfulness-based stress reduction lowers psychological distress in medical students. Teach Learn Med. 2003;15:88–92. doi: 10.1207/S15328015TLM1502_03. [DOI] [PubMed] [Google Scholar]
- Shapiro SL, Schwartz G, Bonner G. Effects of mindfulness-based stress reduction on medical and premedical students. J Behav Med. 1998;21:581–599. doi: 10.1023/a:1018700829825. [DOI] [PubMed] [Google Scholar]
- Shapiro SL, Shapiro DE, Schwartz G. Stress management in medical education: A review of the literature. Acad Med. 2000;75:748–759. doi: 10.1097/00001888-200007000-00023. [DOI] [PubMed] [Google Scholar]
- Stewart SM, Betson C, Lam TH, Marshall IB, Lee PW, Wong CM. Predicting stress in first year medical students: A longitudinal study. Med Educ. 1997;31:163–168. doi: 10.1111/j.1365-2923.1997.tb02560.x. [DOI] [PubMed] [Google Scholar]
- Wetzel MS, Kaptchuk TJ, Haramati A, Eisenberg DM. Complementary and alternative medical therapies: Implications for medical education. [see comment] Ann Intern Med. 2003;138:191–196. doi: 10.7326/0003-4819-138-3-200302040-00011. [DOI] [PubMed] [Google Scholar]
- Wolf TM, Elston RC, Kissling GE. Relationship of hassles, uplifts, and life events to psychological well-being of freshman medical students. Behav Med. 1989;15:37–45. doi: 10.1080/08964289.1989.9935150. [DOI] [PubMed] [Google Scholar]


