Abstract
Background
We recently developed and validated a prognostic model that accurately predicts the 2-year risk of emergent gallstone-related hospitalization in older patients presenting with symptomatic gallstones.
Study Design
We used 100% Texas Medicare data (2000-2011) to identify patients 66 and older with initial episode of symptomatic gallstones not requiring emergency hospitalization. At presentation, we calculated each patient's risk of 2-year gallstone-related emergent hospitalization using the previously validated model. Patients were placed into the following risk groups based on model estimates: <30%, 30-<60%, and ≥60%. Within each risk group, we calculated the percent of elective cholecystectomies (≤2.5 months from initial episode) performed.
Results
161,568 patients had an episode of symptomatic gallstones. The mean age was 76.5±7.3 years and 59.9% were female. The risk of 2-year risk of gallstone-related hospitalizations increased from 15.9% to 41.5% to 65.2% across risk groups. For the overall cohort, 22.3% in the low-risk group, 20.9% in the moderate-risk group, and 23.2% in the high-risk group underwent elective cholecystectomy in the 2.5 months after the initial symptomatic episode. In patients with no comorbidities, elective cholecystectomy rates decreased from 34.2% in the low-risk group to 26.7% in the high-risk group. In patients who did not undergo cholecystectomy, only 9.5% were seen by a surgeon in the 2.5 months following the initial episode.
Conclusions
The risk of recurrent acute biliary symptoms requiring hospitalization has no influence, or even a paradoxical negative influence, on the decision to perform elective cholecystectomy after an initial symptomatic episode. Translation of the risk prediction model into clinical practice can better align treatment with risk and improve outcomes in older patients with symptomatic gallstones.
INTRODUCTION
The prevalence of gallstones increases with age, from approximately 8% of people under 40 years to >50% of people 70 years and older.1 Gallbladder disease is the most common cause of acute abdominal pain in older patients and accounts for a third of abdominal operations in patients older than 65 years.1,2 Left untreated, approximately 1-4% of patients per year will develop symptoms due to their gallstones.3-11 Once symptoms occur, approximately 14% will develop acute cholecystitis, 5% will develop gallstone pancreatitis, and 5% will develop common duct stones within a year.12
Current guidelines recommend elective cholecystectomy to prevent gallstone-related complications in patients with symptomatic gallstones.12 Despite these recommendations, older patients are less likely to undergo cholecystectomy.13,14 This may be due to the increased morbidity and mortality of elective cholecystectomy in older patients. However, if cholecystectomy is not performed, older patients are at an increased risk of developing gallstone-related complications. In addition, older patients are more likely to present with life-threatening complications from their gallstones; greater than 20% of older patients with acute cholecystitis have gangrenous cholecystitis, empyema of the gallbladder, gallbladder perforation, or emphysematous cholecystitis at presentation.15,16 Once complications occur and urgent hospitalization and/or cholecystectomy is necessary, the morbidity and mortality are significantly increased.14,17-19
We recently developed and validated a nomogram, PREOP-Gallstones (Predicting Risk of Complications in Older Patients with Gallstones) that accurately predicts the 2-year risk of developing acute gallstone-related hospitalization in older patients who present with an initial symptomatic episode of gallstones.14 While the data demonstrate that fewer than a quarter of older patients with symptomatic gallstones undergo elective cholecysetctomy,14 it is not known if current decisions regarding elective cholecystectomy in this population are based on risk. The goals of this study were to apply the model in a unique cohort of older patients and evaluate if the decision to perform cholecystectomy was associated with the risk of 2-year gallstone-related hospitalization.
METHODS
This study was determined to be exempt from review by the Institutional Review Board at the University of Texas Medical Branch.
Data Source
We used 100% Texas Medicare claims data from 2000-2011 including inpatient claims (MEDPAR), physician billing claims (Carrier files), and outpatient claims (Outpatient Standard Analytic File, SAF).20 Medicare claims data include patient demographic information, enrollment information, outpatient visits, physician services, and hospital admissions.21
Cohort Selection
We used identical methodology to our previous paper to identify a cohort of older patients with symptomatic gallstones who were eligible for elective cholecystectomy.22 The cohort selection is illustrated in Figure 1. We identified all patients who were admitted to a hospital, saw a physician in the outpatient setting, or visited an emergency department (ED) for a primary diagnosis of gallstone disease between 2001 and 2009. International Classification of Diseases, 9th Edition, Clinical Modification (ICD-9-CM) codes 574* or 575* capture all gallstone disease (Table 1). A patient was considered to have gallstone pancreatitis if he or she had a primary diagnosis of acute pancreatitis (ICD-9-CM 577.0) and a secondary diagnosis of ICD-9-CM 574* or 575*, or vice versa.17 When patients had more than one claim for gallstones, the first claim was considered the “incident episode”.
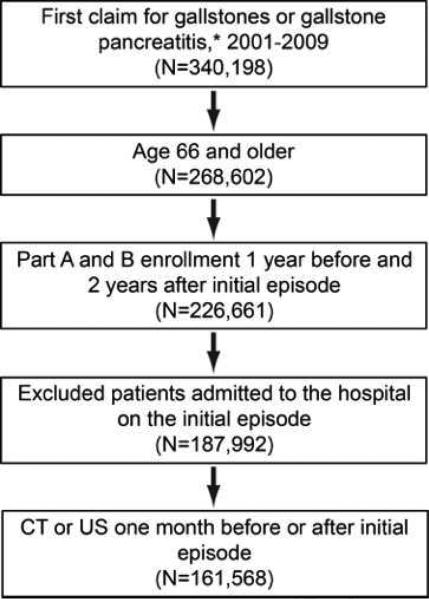
Figure 1.
Cohort selection. Inclusion criteria: 1) Symptomatic cholelithiasis defined by a) Primary diagnosis of ICD-9-CM code 574 of 575 or b) Primary diagnosis of acute pancreatitis (577.0) and a secondary diagnosis of 574 or 575; 2) Patients age 66 and older; 3) Patients with Medicare Part A and Part B 1 year before and 2 years after the initial episode; 4) Patients not admitted to the hospital on the incident episode; and 5) Patients who underwent CT and/or US in the month before or after diagnosis were included. US, ultrasound.
Table 1.
International Classification of Diseases, 9th Revision, Clinical Modification (ICD-9-CM) Diagnosis and Current Procedural Terminology Codes
| Description | ICD-9-CM Diagnosis Codes or CPT Procedure Codes |
|---|---|
| Cholecystectomy | CPT: 49310, 56340, 56342, 47562, 47564, 47600, 47610, 47612, 47620, 49311, 56341, 47563, 47605 |
| Initial diagnosis | |
| Gallstone pancreatitis | 577.0 and any secondary diagnosis starting with 574*/575* OR 574* or 575* and a secondary diagnosis code for pancreatitis |
| Acute cholecystitis | 574.0*, 574.1*, 575.0*, 575.1*, 575.2*, 575.3*, 575.4* |
| Common bile duct stones | 574.3*, 574.4*, 574.5*, 574.6*, 574.7*, 574.8*, 574.9* |
| Biliary colic/biliary dyskinesia | 575.8*, 574.2* |
| Diagnostic tests | |
| Computed tomography | CPT codes 74150, 74160, 74170 |
| Ultrasound | CPT codes 76705, 76700, 76770, 76705 |
| Evaluation and management | CPT Codes |
| Emergency room evaluation | 99281-99285 |
| Physician visit | 99201-99205, 99211-99215, 99241-99245 |
Denotes any number 0-9 in ICD-9-CM extension code, which further specifies the diagnosis.
Patients were included if they were aged 66 years or older and had Medicare Parts A and B fee-for-service and no HMO for one year prior and two years following the incident claim, or until death. This enabled us to identify incident cases (no cases in the previous year), to identify patient comorbidities from the claims data the year prior to the incident episode, and to follow all patients for at least two years after the date of the incident episode. We excluded patients who were admitted to a hospital or underwent cholecystectomy at the time of the incident episode.
To improve the specificity of our algorithm for identifying patients with symptomatic gallstones, we excluded patients if the diagnosis of gallstones was not associated with a claim for abdominal ultrasound (US) or computed tomography (CT) in the one month before or after the incident claim. CT and US were identified in the carrier and outpatient SAF claims files using Current Procedural Terminology (CPT) codes (Table 1).
Patient and Disease Characteristics
Patient age was classified as 60-69 years, 70-74 years, 75-79 years, and 80 years and older. We also calculated mean age (±SD). We recorded sex, race/ethnicity (non-Hispanic white, black, Hispanic, other), Elixhauser comorbidity index, and diagnosis at initial claim for symptomatic cholelithiasis (biliary colic/biliary dyskinesia, acute cholecystitis, common bile duct stones, and gallstone pancreatitis; Table 1). Diagnosis was classified in a hierarchical manner as follows: anny patient who had a primary code for pancreatitis and a secondary diagnosis code for gallstones or vice versa was classified as having gallstone pancreatitis. The remaining patients were classified as having common duct stones, acute cholecystitis, or biliary colic based on the codes listed in Table 1. The number of Elixhauser comorbidities was used as a measure for patient comorbidity.23 Type of initial visit was classified as ED or physician office visit based on the evaluation and management CPT codes for the visit (Table 1).
Risk Groups
We used our previously validated algorithm22 to calculate the expected 2-year risk of emergent gallstone-related hospitalization for each patient in the cohort. The model, called PREOP-Gallstones, uses patient sex, age group (66-69 years, 70-74 years, 75-79 years, 80 years and older), Elixhauser comorbidity score, diagnosis at the incident episode (biliary colic, acute cholecystitis, common duct stones, gallstone pancreatitis), race/ethnicity, and visit type (ED vs. physician visit) to predict the risk of gallstone-related readmissions.
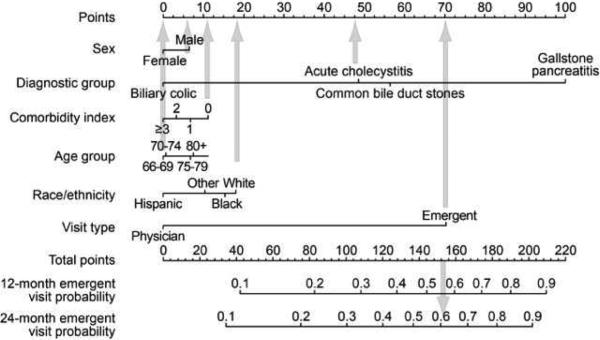
Risk was calculated using characteristics defined at the incident episode. For example, a patient who is male, had acute cholecystitis at the incident episode, no comorbidities, 60-69 years old, white, and was seen in an emergency room on the incident episode has a total score of 156, corresponding to a 2-year gallstone-related readmission risk of approximately 63% (Figure 2). Patients were then categorized into the following risk groups: <30% risk (low risk), 30-60% risk (moderate risk), and >60% risk (high risk). Risk groups were not chosen based on equal numbers of patients, but on clinical relevance.
Figure 2.
Sample of risk calculation using the PREOP-Gallstones model nomogram. To use the nomogram, a vertical line is drawn from each factor to the corresponding position on the “Points” line. Points are summed for each factor and a line is drawn (downward arrow) from this position on the “Points” line to the “Emergent Visit Probability” lines to determine a patient's 12-month and 24-month risk for developing emergent gallstone-related complications.
Outcome Variables
Our outcome of interest was elective cholecystectomy rates by risk group. Elective cholecystectomy was defined as cholecystectomy within 2.5 months of the incident episode as in the previous report.22 We identified all cholecystectomies in the 2-years after the initial episode. If cholecystectomy was performed in the outpatient or inpatient setting within 2.5 months that were not classified as urgent or emergent admission, the patient was classified as having undergone elective cholecystectomy. For each risk group, we calculated the percentage of patients who underwent elective cholecystectomy. We also calculated the percentage of patients who underwent elective cholecystectomy in the subgroup of patients who had no comorbidities. In patients who did not undergo cholecystectomy, we calculated the percentage of patients who were evaluated by a surgeon in the 2.5 months after the incident episode.
Statistical Analysis
All means are reported as mean ± SD and all categorical variables are reported as percentages. Chi square tests were used to compare cholecystectomy rates across patient characteristics and risk groups. To further validate the risk prediction model, we calculated the actual 2-year observed gallstone-related acute hospitalizations from the date of the incident episode in patients who did not undergo elective cholecystectomy. We also used cumulative incidence curves to calculate gallstone-related acute hospitalization, censoring patients who died or underwent delayed elective cholecystectomy (after 2.5 months) and who were no longer at risk for emergent gallstone-related hospitalization.
Logistic regression models were used to identify factors associated with surgical evaluation. Any patient who underwent elective cholecystectomy and any patient who did not undergo elective cholecystectomy but was evaluated by a surgeon in the 2.5 months after the incident episode were considered to have undergone surgical evaluation. All statistical analyses were performed using SAS version 9.3 (SAS Inc., Cary, NC, USA). Statistical significance was accepted at the p<0.05 level.
RESULTS
Patient Characteristics and Cholecystectomy Rates
We identified 161,568 Medicare beneficiaries with an incident episode of symptomatic gallstones who were not admitted to a hospital on the incident episode and were potential candidates for an elective cholecystectomy. The mean age of the cohort was 76.5±7.3 years. Sixty percent (59.9%) were female, 84.0% were white, and 15.9% had an Elixhauser comorbidity score of zero (Table 2).
Table 2.
Cohort Characteristics and Cholecystectomy Rates Based on Characteristics
| n (% of overall cohort) | Undergoing cholecystectomy, n (%) | p Value | |
|---|---|---|---|
| Overall cohort | 161,568 | 35,967 (22.3%) | ~ |
| Age, y, mean (SD) | 76.5 (7.3) | 74.1 (6.2) | <0.0001 |
| Age group, y | <0.0001 | ||
| 66-69 | 33,522 (20.8%) | 10,247 (30.6%) | |
| 70-74 | 38,966 (24.1%) | 10,521 (27.0%) | |
| 75-79 | 36,076 (22.3%) | 7,983 (22.1%) | |
| 80+ | 53,004 (32.8%) | 7,216 (13.6%) | |
| Sex | <0.0001 | ||
| Female | 96,809 (59.9%) | 23,261 (24.0%) | |
| Male | 64,759 (40.1%) | 12,706 (19.6%) | |
| Race | <0.0001 | ||
| White | 135,711 (84.0%) | 32,037 (23.6%) | |
| Black | 11,294 (7.0%) | 1,405 (12.4%) | |
| Hispanic | 11,316 (7.0%) | 1,998 (17.7%) | |
| Other | 3,247 (2.0%) | 527 (16.2%) | |
| Elixhauser Comorbidity Index | <0.0001 | ||
| 0 | 25,633 (15.9%) | 8,461 (33.0%) | |
| 1 | 31,991 (19.8%) | 9,919 (31.0%) | |
| 2 | 29,543 (18.3%) | 7,552 (25.6%) | |
| >=3 | 74,401 (46.1%) | 10,035 (13.5%) | |
| Initial diagnosis | <0.0001 | ||
| Biliary colic | 109,043 (67.5%) | 20,271 (18.6%) | |
| Acute cholecystitis | 40,980 (25.4%) | 13,534 (33.0%) | |
| Common bile duct stones | 7,143 (4.4%) | 1,259 (17.6%) | |
| Gallstone pancreatitis | 4,402 (2.7%) | 903 (20.5%) | |
| Location of initial visit | <0.0001 | ||
| Physician visit | 145,650 (90.2%) | 32,659 (22.4%) | |
| Emergency room visit | 15,918 (9.8%) | 3,308 (20.8%) |
Elective cholecystectomy within 2.5 months of the incident episode was performed in 35,967 patients (22.3%). Table 1 demonstrates cholecystectomy rates by patient characteristics. Patients who were younger, female, white, and had fewer Elixhauser comorbidities were slightly more likely to undergo cholecystectomy. Beneficiaries who were coded as having acute cholecystitis on the incident episode were the most likely to undergo elective cholecystectomy, followed by beneficiaries with gallstone pancreatitis, biliary colic, and common duct stones. Patients seen in an ED on the incident episode were less likely to undergo cholecystectomy than those evaluated by a physician in the outpatient setting.
Risk Groups and Model Validation
The PREOP-gallstones risk prediction model was applied to all patients in the cohort based on presenting characteristics during the incident episode. 147,950 patients (91.5%) had a model-predicted risk of 2-year gallstone related emergent hospitalization of <30%; 9,959 (6.2%) had a 30-60% 2-year risk and 3,659 (2.3%) had >60% 2-year risk.
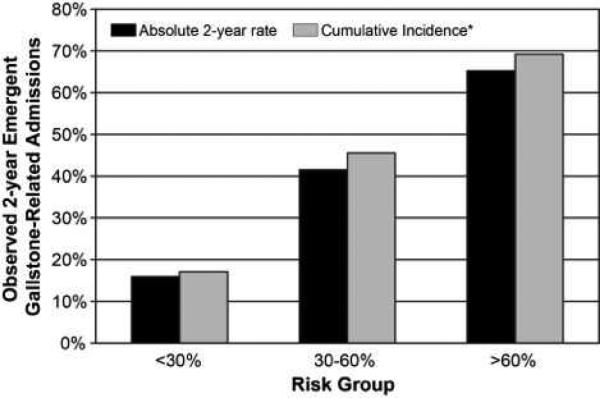
The risk distribution was similar for the 125,601 patients who did not undergo elective cholecystectomy; 114,908 patients were in the low risk group (91.5%), 7,880 (6.3%) in the moderate risk group, and 2,813 (2.2%) in the high risk group. Of these 125,601 patients, 23,418 (18.6%) had an acute gallstone-related hospital admission in the two years after the incident episode. The actual 2-year acute gallstone-related hospitalizations for these patients were 15.9% (N=18,315), 41.5% (N=3,269), and 65.2% (N=1,834) in the low, moderate, and high risk groups, respectively, confirming the predictive ability of the model (Figure 3). This increased to 17.1%, 45.5%, and 69.2% using cumulative incidence curves with patients censored at death or after elective cholecystectomy (Figure 3). The C-statistic in this cohort was identical to the original cohort (0.69). In patients who required emergent gallstone related readmission, the in-hospital mortality was 6.2% and the complication rate was 53.1% .
Figure 3.
Two-year gallstone-related hospitalization rates in the 125,601 patients who did not undergo elective cholecystectomy in the 2.5 months after the incident symptomatic episode. The black bars represent the actual rates and the gray bars represent the cumulative incidence censored for patient deaths and elective cholecystectomy, when patients were no longer at risk for emergent gallstone-related hospitalization.
Elective Cholecystectomy and Risk
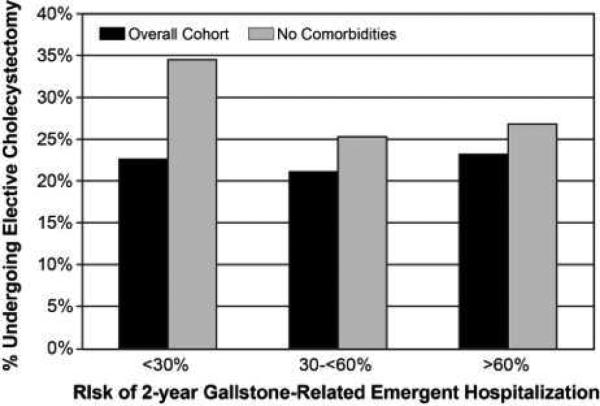
Receipt of cholecystectomy in older patients with symptomatic gallstones appeared to be independent of the risk of 2-year emergent gallstone-related hospital admission (Table 3). For the overall cohort, elective cholecystectomy was performed in 22.3% of the low risk group, 20.9% of the moderate risk group, and 23.2% of the high risk group (Figure 4, p=0.002).
Table 3.
Percent of Patients Undergoing Elective Cholecystectomy by 2-year Model-Predicted Risk of Requiring Gallstone-Related Hospitalization
| Risk group | Total, n | Undergoing elective cholecystectomy, n (%) | p Value |
|---|---|---|---|
| Overall cohort (n=161,568) | |||
| <30% | 147,950 | 33,042 (22.3%) | 0.002 |
| 30 to <60% | 9,959 | 2,079 (20.9%) | |
| ≥60% | 3,659 | 846 (23.2%) | |
| Patients with no comorbidities (n=25,633) | |||
| <30% | 22,257 | 7,597 (34.2%) | <0.0001 |
| 30 to <60% | 2,297 | 576 (25.2%) | |
| ≥60% | 1,079 | 288 (26.7%) |
Figure 4.
Percentage of patients undergoing cholecystectomy by risk group (<30%, 30-60%, >60%). The black bars represent the percentage of the overall cohort (N=161,568) and the gray bars represent the percentage of the 25,633 patients with no comorbidities undergoing cholecystectomy.
In a subset of patients with no Elixhauser comorbidities (N=25,633) and, therefore, no clear contraindication to cholecystectomy, cholecystectomy rates actually decreased with increasing risk of emergent admission. Cholecystectomy was performed in 34.2% of patients in the low risk group, 25.2% of patients in the moderate risk group, and 26.7% of patients in the high risk group (Figure 4).
Surgical evaluation, defined as elective cholecystectomy or surgeon visit within 2.5 months of surgery, was performed in 47,888 patients (29.5%). Only 11,921 of the 125,601 patients (9.5%) who did not undergo cholecystectomy were evaluated by a surgeon in the 2.5 months after the incident episode. This increased to only 13.8% in beneficiaries with no comorbidities.
Factors Predicting Surgical Evaluation
In a multivariable model (Table 4), increasing Elixhauser comorbidities, white race, and uncomplicated biliary colic at presentation were associated with lower rates of surgical evaluation, consistent with the factors associated with lower risk of acute gallstone-related hospitalization. However, the other associations in the model were counter to the risk prediction model. Patients who were male (OR 0.76, 95% CI 0.75-0.78), older (80 years and older vs. 66-69 years, OR 0.47, 95% CI 0.46-0.49), and seen in an emergency department on the incident episode (OR 0.75, 95% CI 0.72-0.77) were less likely to undergo surgical evaluation, despite increased risk in these situations.
Table 4.
Multivariable Logistic Regression Model: Factors Associated with Surgical Evaluation in Older Patients Presenting with Symptomatic Gallstones
| Factors associated with surgical evaluation*, odds ratio (95% CI) | |
|---|---|
| Age group, y | |
| 66-69 | 1.00 (REF) |
| 70-74 | 0.89 (0.87, 0.92) |
| 75-79 | 0.74 (0.71, 0.76) |
| 80+ | 0.47 (0.46, 0.49) |
| Sex | |
| Female | 1.00 (REF) |
| Male | 0.76 (0.75, 0.78) |
| Race | |
| White | 1.00 (REF) |
| Black | 0.59 (0.65, 0.62) |
| Hispanic | 0.85 (0.81, 0.89) |
| Other | 0.62 (0.57, 0.67) |
| Elixhauser comorbidities | |
| 0 | 1.00 (REF) |
| 1 | 0.93 (0.90, 0.96) |
| 2 | 0.74 (0.71, 0.77) |
| >=3 | 0.37 (0.36, 0.38) |
| Initial diagnosis | |
| Biliary colic | 1.00 (REF) |
| Acute cholecystitis | 2.26 (2.21, 2.32) |
| Common bile duct stones | 0.96 (0.90, 1.02) |
| Gallstone pancreatitis | 1.16 (1.08, 1.25) |
| Location of initial visit | |
| Physician visit | 1.00 (REF) |
| Emergency room visit | 0.75 (0.72, 0.77) |
DISCUSSION
Using the previously validated PREOP-Gallstones risk prediction model, our data demonstrate that current decision-making regarding receipt of elective cholecystectomy in older patients with symptomatic gallstones is independent of patients’ risk of requiring 2-year acute gallstone-related hospitalization. In the overall cohort, elective cholecystectomy was performed in fewer than 25% of patients in the low (<30%), moderate (30-60%), and high (>60%) risk groups. Even more striking, in older patients with no comorbidities and no clear contraindication to cholecystectomy, elective cholecystectomy was performed in 35% of patients at lowest risk and only 27% of patients at highest risk for acute hospitalization. Receipt of cholecystectomy seems largely determined at the level of the primary care physician or non-surgeon practitioners, as fewer than 10% of patients who did not undergo cholecystectomy were evaluated by a surgeon in the 2.5 months after the incident episode.
The 2002 Society of American Gastrointestinal and Endoscopic Surgeons (SAGES) guidelines include symptomatic cholelithiasis as an indication for laparoscopic cholecystectomy with few relative or absolute contraindications.”24 These recommendations are based on level II, Grade A evidence and supported by a later Cochrane review demonstrating decreased risk for conversion, operative time, and length with early vs. delayed cholecystectomy in the setting of symptomatic gallstones.12 Despite these guidelines, only 22% of fee-for-service Medicare beneficiaries in Texas underwent elective cholecystectomy after an initial episode of symptomatic gallstones, reflecting uncertainty about the risks and benefits of cholecystectomy in this population.
The PREOP-Gallstone nomogram accurately predicts the risk for 2-year gallstone-related acute hospitalization in patients with symptomatic gallstones. Created from a 5% national sample of Medicare patients, the model can be applied at the time of initial presentation in older patients with gallstones. In addition, the model is based on readily available patient characteristics: sex, age, race, comorbidity, diagnosis at initial presentation (biliary colic, acute cholecystitis, common duct stones, or gallstone pancreatitis) and whether the patient was seen by a physician or in an ED. The model performs well in this unique cohort of Texas Medicare beneficiaries with an observed 2-year hospitalization rate of 17%, 46%, and 69% in the <30%, 30-60%, and >60% risk groups.
In the PREOP-Gallstone model, the risk of gallstone-related hospitalization is largely driven by the diagnosis at initial presentation and the site of the initial visit, both of which are surrogates for the severity of the gallbladder disease. Consistent with the model, patients were more likely to be evaluated by a surgeon and undergo cholecystectomy if they had complicated disease on the initial presentation, suggesting that PCPs and surgeons recognize that the severity of disease increases the risk of future episodes. However, patients were less likely to be evaluated by a surgeon if they were seen in an ED on the incident episode. This seems counterintuitive and may represent a system problem, where patients seen in the ED are not provided adequate follow-up. Patients who were white and had more Elixhauser comorbidities were less likely to be evaluated by a surgeon, also consistent with the risk prediction model. However, surgical evaluation decreased with increasing age despite data that demonstrate increased probability of gallstone-related complications in older patients and poorer outcomes once complications occur.
Once cholecystectomy is performed in the acute setting, the morbidity and mortality rise sharply.14,18,19,25-29 While elective cholecystectomy can be performed safely in older patients, limited data in this population suggest higher rates of comorbid illness, higher conversion rates, longer lengths of stay, increased need for ICU care, and more complications in this population.18,19,30-34 In a recent study of 81 octogenarians, Lupinacci et al. reported a 34% mortality rate, 51% complication rate, and an 11-day mean length of stay when cholecystectomy was performed in the acute setting (N=30); 77% of these patients required ICU care and the mean ICU stay was 9.4 days. This is in contrast to elective/non-urgent cholecystectomy (N=51), where there was no mortality, a 12-14% complication rate, and a mean length of stay under three days. While 31% percent of patients in this group required ICU admission, the mean ICU stay was only one day. Likewise, Uecker et al.29 reported outcomes in 53 patients 80 and older who presented via the emergency room with acute complications of gallstones. 66% required open cholecystectomy. The mortality was 13% and 28% had complications, with a mean length of stay exceeding 11 days. We similarly observed significant morbidity and mortality in older patients admitted emergently after an initial symptomatic episode.
Based on these data, many authors recommend early, elective cholecystectomy in older patients as soon as they are found to be symptomatic. Our previous study14 as well as the current study demonstrate that this is not the current national practice. In addition, the data demonstrate that over 80% of older patients who do not undergo elective cholecystectomy in the first 2.5 months do not require emergent hospitalization in the two years after the incident episode. This suggests that not all older patients necessarily benefit from elective cholecystectomy, but outcomes in the subset at highest risk could be improved with early cholecystectomy.
Current decisions about cholecystectomy are seemingly independent of their risk of developing complications. In the era of patient-centered outcomes research, the PREOP-gallstones risk prediction model provides a starting point for individualized care and shared decision making in older patients with gallstones. Translation of this model into clinical practice, especially at the level of the primary care physician, has the potential to improve outcomes by increasing surgical referrals and elective cholecystectomy rates in the patients at highest risk for gallstone-related hospitalization. This can avoid the morbidity associated with subsequent complicated gallstone disease in this vulnerable population. Likewise, it would allow physicians to avoid cholecystectomy in patients who are high surgical risk and at low risk for developing complications from their gallstones. Finally, in patients who are low surgical risk and have low to moderate risk of complications, where the decision for cholecystectomy is preference-sensitive, this risk information can help patients make a decision in the context of their symptoms, the impact of their symptoms on their quality of life, and their personal preferences.
To achieve this long-term goal of targeted surgical therapy for patients with high-risk gallstone disease, qualitative studies exploring physicians’ decision making process regarding referral for (PCPs) or receipt of cholecystectomy (surgeons) are necessary to understand the current range of physician practice and preferences in treating gallstone disease. Further studies incorporating clinical data may improve the predictive ability of our model. Finally, input from primary care physicians, surgeons, and patients is needed to determine optimal strategies to incorporate the model into practice and to communicate individualized risk to patients.
Precis.
The risk of recurrent acute biliary symptoms requiring hospitalization has no influence, or even a paradoxical negative influence, on the decision to perform elective cholecystectomy after an initial symptomatic episode in older patients. Decision making in gallbladder disease in this vulnerable population should be guided by risk.
ACKNOWLEDGMENT
This paper is dedicated in memory of Suzanne Kneuper Linder, Ph.D. (January 8, 1977 – October 9, 2014). The co-authors recognize her for her contributions to this manuscript and the field of risk communication. She was a role model in her dedication to patient centered outcomes research and her desire to improve quality and delivery of care. She is missed.
Support: Study was supported by grants from the UTMB Clinical and Translational Science Award #UL1TR000071, NIH T-32 Grant # 5T32DK007639, and AHRQ Grant # 1R24HS022134. Drs Riall, Adhikari, Dimou, and Tamirisa are supported by the Cancer Prevention Research Institute of Texas, RP1400020.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Disclosure Information: Nothing to disclose.
Presented at the Southern Surgical Association 126th Annual Meeting, Palm Beach, FL, November 30–December 3, 2014.
REFERENCES
- 1.Hendrickson M, Naparst TR. Abdominal surgical emergencies in the elderly. Emerg Med Clin North Am. 2003;21:937–969. doi: 10.1016/s0733-8627(03)00072-5. [DOI] [PubMed] [Google Scholar]
- 2.Bugliosi TF, Meloy TD, Vukov LF. Acute abdominal pain in the elderly. Annals of emergency medicine. 1990;19(12):1383–1386. doi: 10.1016/s0196-0644(05)82602-2. [DOI] [PubMed] [Google Scholar]
- 3.Attili AF, De Santis A, Capri R, Repice AM, Maselli S. The natural history of gallstones: the GREPCO experience. The GREPCO Group. Hepatology. 1995;21(3):655–660. doi: 10.1002/hep.1840210309. [DOI] [PubMed] [Google Scholar]
- 4.Comfort MW, Gray HK, Wilson JM. The Silent Gallstone: A Ten to Twenty Year Follow-up Study of 112 Cases. Ann Surg. 1948;128(5):931–937. [PMC free article] [PubMed] [Google Scholar]
- 5.Festi D, Reggiani ML, Attili AF, et al. Natural history of gallstone disease: Expectant management or active treatment? Results from a population-based cohort study. Journal of gastroenterology and hepatology. 2010;25(4):719–724. doi: 10.1111/j.1440-1746.2009.06146.x. [DOI] [PubMed] [Google Scholar]
- 6.Friedman GD, Raviola CA, Fireman B. Prognosis of gallstones with mild or no symptoms: 25 years of follow-up in a health maintenance organization. J Clin Epidemiol. 1989;42(2):127–136. doi: 10.1016/0895-4356(89)90086-3. [DOI] [PubMed] [Google Scholar]
- 7.Gracie WA, Ransohoff DF. The natural history of silent gallstones: the innocent gallstone is not a myth. N Engl J Med. 1982;307(13):798–800. doi: 10.1056/NEJM198209233071305. [DOI] [PubMed] [Google Scholar]
- 8.Halldestam I, Enell EL, Kullman E, Borch K. Development of symptoms and complications in individuals with asymptomatic gallstones. Br J Surg. 2004;91(6):734–738. doi: 10.1002/bjs.4547. [DOI] [PubMed] [Google Scholar]
- 9.Lund J. Surgical indications in cholelithiasis: prophylactic choleithiasis: prophylactic cholecystectomy elucidated on the basis of long-term follow up on 526 nonoperated cases. Ann Surg. 1960;151:153–162. doi: 10.1097/00000658-196002000-00001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.McSherry CK, Ferstenberg H, Calhoun WF, Lahman E, Virshup M. The natural history of diagnosed gallstone disease in symptomatic and asymptomatic patients. Ann Surg. 1985;202(1):59–63. doi: 10.1097/00000658-198507000-00009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Thistle JL, Cleary PA, Lachin JM, Tyor MP, Hersh T. The natural history of cholelithiasis: the National Cooperative Gallstone Study. Ann Intern Med. 1984;101(2):171–175. doi: 10.7326/0003-4819-101-2-171. [DOI] [PubMed] [Google Scholar]
- 12.Gurusamy KS, Samraj K, Fusai G, Davidson BR. Early versus delayed laparoscopic cholecystectomy for biliary colic. Cochrane Database Syst Rev. 2008;(4):CD007196. doi: 10.1002/14651858.CD007196.pub2. [DOI] [PubMed] [Google Scholar]
- 13.Bergman S, Sourial N, Vedel I, et al. Gallstone disease in the elderly: are older patients managed differently? Surg Endosc. 2011;25(1):55–61. doi: 10.1007/s00464-010-1128-5. [DOI] [PubMed] [Google Scholar]
- 14.Parmar AD, Sheffield KM, Adhikari D, et al. PREOP-Gallstones: A prognostic nomogram for the management of symptomatic cholelithiasis in older patients. 2014 doi: 10.1097/SLA.0000000000000868. Epub ahead of print. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Bedirli A, Sakrak O, Sozuer EM, Kerek M, Guler I. Factors effecting the complications in the natural history of acute cholecystitis. Hepatogastroenterology. 2001;48(41):1275–1278. [PubMed] [Google Scholar]
- 16.Morrow DJ, Thompson J, Wilson SE. Acute cholecystitis in the elderly: a surgical emergency. Arch Surg. 1978;113(10):1149–1152. doi: 10.1001/archsurg.1978.01370220035006. [DOI] [PubMed] [Google Scholar]
- 17.Riall TS, Zhang D, Townsend CM, Kuo YF, Goodwin JS. Failure to perform cholecystectomy for acute cholecystitis in elderly patients is associated with increased morbidity, mortality, and cost. J Am Coll Surg. 2010;210(5):668–677, 677-669. doi: 10.1016/j.jamcollsurg.2009.12.031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Fukami Y, Kurumiya Y, Mizuno K, Sekoguchi E, Kobayashi S. Cholecystectomy in octogenarians: be careful. Updates in surgery. 2014 doi: 10.1007/s13304-014-0267-y. [DOI] [PubMed] [Google Scholar]
- 19.Lupinacci RM, Nadal LR, Rego RE, et al. Surgical management of gallbladder disease in the very elderly: are we operating them at the right time? Eur J Gastroenterol Hepatol. 2013;25(3):380–384. doi: 10.1097/MEG.0b013e32835b7124. [DOI] [PubMed] [Google Scholar]
- 20.Center for Medicare & Medicaid Services [December, 2012]; http://www.cms.gov/.
- 21.Research Statistics. [December, 2012];Data & Systems. http://www.cms.gov/Research-Statistics-Data-and-Systems/Research-Statistics-Data-and-Systems.html.
- 22.Parmar AD, Vargas GM, Tamirisa NP, Sheffield KM, Riall TS. Trajectory of care and use of multimodality therapy in older patients with pancreatic adenocarcinoma. Surgery. 2014;156(2):280–289. doi: 10.1016/j.surg.2014.03.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.van Walraven C, Austin PC, Jennings A, Quan H, Forster AJ. A modification of the Elixhauser comorbidity measures into a point system for hospital death using administrative data. Med Care. 2009;47(6):626–633. doi: 10.1097/MLR.0b013e31819432e5. [DOI] [PubMed] [Google Scholar]
- 24.SAGES [August 12, 2014];Guidelines for the Clinical Application of Laparoscopic Biliary Surgery. 2002 http://www.ncbi.nlm.nih.gov/pubmed/?term=fall+sickle+cell+disease+laparoscopic+cholecystectomy.
- 25.Chau CH, Tang CN, Siu WT, Ha JP, Li MK. Laparoscopic cholecystectomy versus open cholecystectomy in elderly patients with acute cholecystitis: retrospective study. Hong Kong medical journal = Xianggang yi xue za zhi / Hong Kong Academy of Medicine. 2002;8(6):394–399. [PubMed] [Google Scholar]
- 26.Guerriero O, D'Amore E, Di Meo E, et al. [Laparoscopic surgery for acute cholecystitis in the elderly. Our experience]. Chirurgia italiana. 2008;60(2):189–197. [PubMed] [Google Scholar]
- 27.Kirshtein B, Bayme M, Bolotin A, Mizrahi S, Lantsberg L. Laparoscopic cholecystectomy for acute cholecystitis in the elderly: is it safe? Surg Laparosc Endosc Percutan Tech. 2008;18(4):334–339. doi: 10.1097/SLE.0b013e318171525d. [DOI] [PubMed] [Google Scholar]
- 28.Moyson J, Thill V, Simoens C, Smets D, Debergh N, Mendes da Costa P. Laparoscopic cholecystectomy for acute cholecystitis in the elderly: a retrospective study of 100 patients. Hepatogastroenterology. 2008;55(88):1975–1980. [PubMed] [Google Scholar]
- 29.Uecker J, Adams M, Skipper K, Dunn E. Cholecystitis in the octogenarian: is laparoscopic cholecystectomy the best approach? Am Surg. 2001;67(7):637–640. [PubMed] [Google Scholar]
- 30.Arthur JD, Edwards PR, Chagla LS. Management of gallstone disease in the elderly. Ann R Coll Surg Engl. 2003;85(2):91–96. doi: 10.1308/003588403321219849. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Dubecz A, Langer M, Stadlhuber RJ, et al. Cholecystectomy in the very elderly--is 90 the new 70? J Gastrointest Surg. 2012;16(2):282–285. doi: 10.1007/s11605-011-1708-2. [DOI] [PubMed] [Google Scholar]
- 32.Hazzan D, Geron N, Golijanin D, Reissman P, Shiloni E. Laparoscopic cholecystectomy in octogenarians. Surg Endosc. 2003;17(5):773–776. doi: 10.1007/s00464-002-8529-z. [DOI] [PubMed] [Google Scholar]
- 33.Maxwell JG, Tyler BA, Rutledge R, Brinker CC, Maxwell BG, Covington DL. Cholecystectomy in patients aged 80 and older. Am J Surg. 1998;176(6):627–631. doi: 10.1016/s0002-9610(98)00282-7. [DOI] [PubMed] [Google Scholar]
- 34.Pavlidis TE, Marakis GN, Symeonidis N, et al. Considerations concerning laparoscopic cholecystectomy in the extremely elderly. J Laparoendosc Adv Surg Tech A. 2008;18(1):56–60. doi: 10.1089/lap.2007.0037. [DOI] [PubMed] [Google Scholar]