Abstract
Objective
To evaluate whether an existing vaginal birth after cesarean delivery (VBAC) prediction model validated for women with one prior cesarean delivery also accurately predicts the likelihood of VBAC in women with two prior cesarean deliveries.
Methods
We performed a secondary analysis of all women attempting trial of labor after cesarean (TOLAC) with a term singleton pregnancy and two prior cesarean deliveries in the Maternal-Fetal Medicine Units Network (MFMU) Cesarean Registry. Probability of VBAC was calculated for each participant using the MFMU VBAC prediction model. Women were considered to have a recurring indication for cesarean if the indication for either their first or second cesarean was arrest of dilation or descent. An ROC curve was used to assess the classification ability of the model and the predicted likelihood of VBAC success was compared to the actual likelihood using a calibration curve.
Results
Among 369 women with two prior cesareans undergoing TOLAC, the actual VBAC rate was 66% (95% CI 61, 71). The mean predicted probability of VBAC was higher among women with a successful TOLAC than those with a failed TOLAC (75% vs 59%, p<0.001). The area under the ROC curve for women with two prior cesareans was 0.74 (95% CI 0.69, 0.80). Within deciles of predicted probability >30%, predicted probabilities were similar to and contained actual probabilities within the 95% confidence interval.
Conclusions
The estimates of VBAC success based on the MFMU prediction model are similar to the actual rates observed among women with two prior cesareans.
Introduction
The Maternal-Fetal Medicine Units Network (MFMU) vaginal birth after cesarean delivery (VBAC) prediction model is used in clinical practice to counsel women regarding their likelihood of VBAC (1). This model uses demographic and clinical information available at the time of the first prenatal visit to predict the likelihood of VBAC. It was created for and subsequently has been validated in cohorts of women with only one prior cesarean (2–4).
The most recent American College of Obstetricians and Gynecologists Practice Bulletin states that it is “reasonable to consider” a TOLAC in women with two prior cesareans (5). The Practice Bulletin further notes that this decision should be made by weighing other factors which may influence the probability of success (5).
There are data to suggest an increased risk of morbidity in women with two prior cesareans undergoing TOLAC (6,7). The likelihood of VBAC may therefore weigh even more heavily in decision-making regarding TOLAC in women with two prior cesarean deliveries compared to women with only one prior cesarean. It remains unknown whether prediction models that were established in women with one prior cesarean accurately predict TOLAC success in women with two prior cesareans. We therefore aimed to evaluate whether the MFMU VBAC prediction model validated for women with one prior cesarean also accurately predicts the likelihood of VBAC in women with two prior cesareans.
Materials and Methods
This was a secondary analysis of the MFMU Cesarean Registry. The Cesarean Registry was a 5-year prospective observational study of vaginal birth after cesarean and cesarean deliveries occurring between January 1999 and December 2003 across 19 tertiary centers in the United States. A detailed description of the primary study has been previously published (8). For the purposes of this secondary analysis, we included all women with two prior cesarean deliveries undergoing a trial of labor after cesarean with a term (≥ 37 weeks gestation), cephalic fetus. Women were excluded if the fetus had known anomalies or was not alive. This analysis was deemed non-human subjects research by the Colorado Multiple Institutional Review Board since all data were de-identified.
Data on patient demographics including maternal age, prior vaginal delivery, prior VBAC, pre-pregnancy body mass index (BMI), race/ethnicity and history of recurring indication for prior cesarean (arrest of dilation or descent) were extracted from the Cesarean Registry dataset. The probability of successful VBAC was calculated for each participant using the MFMU VBAC prediction model that incorporates variables available at the first prenatal visit. This model is based on a logistic regression equation for predicted probability of successful VBAC where likelihood of VBAC success is equal to exp(w)/[1+exp(W)] and w=[3.766 - (0.039*maternal age) – (0.060*pre-pregnancy BMI) – (0.671*African American race) – (0.680*Hispanic race) + (0.888*history of vaginal delivery) + (1.003*history of successful VBAC) – (0.632*history of recurring indication)] (1). In the present analysis, women were considered to have a recurring indication for cesarean if the indication for either their first or second cesarean was arrest of dilation or descent.
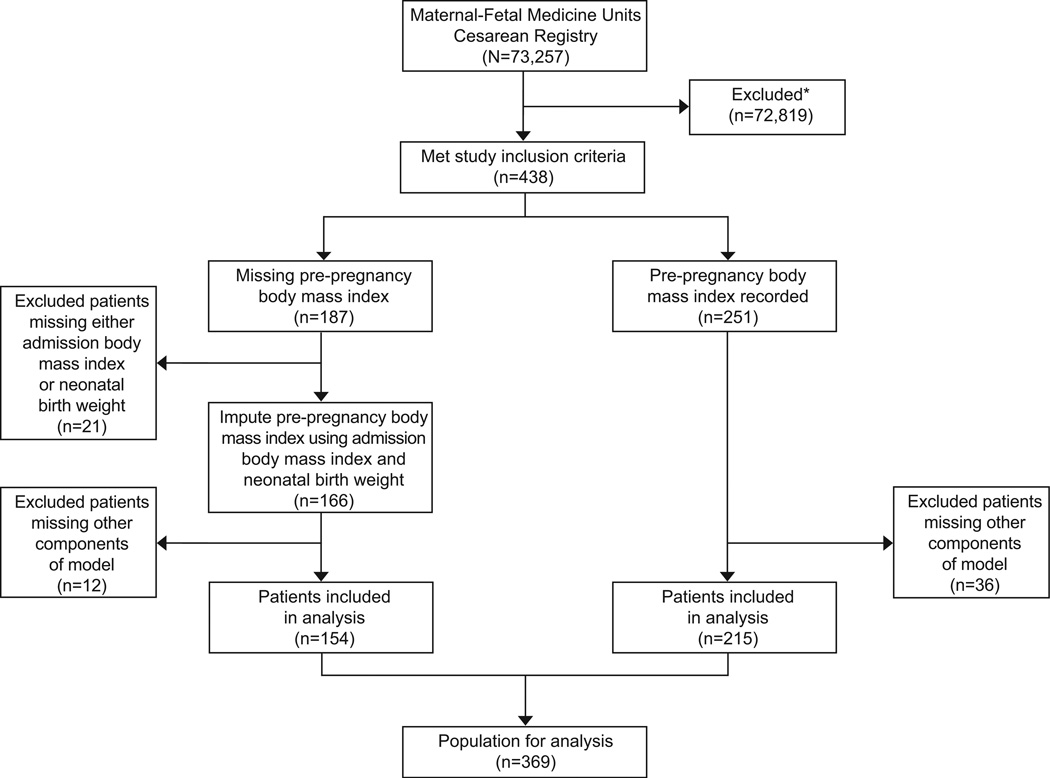
Pre-pregnancy BMI was missing for 43% of the population otherwise eligible for inclusion in this analysis. We imputed the pre-pregnancy BMI as a function of the delivery admission BMI and infant birth weight using the 251 women with a pre-pregnancy BMI. The final imputation model included a natural-log scale BMI (pre-pregnancy and at admission for delivery), a linear, quadratic and cubic BMI at admission for delivery, and linear neonatal birth weight. Predicted values for pre-pregnancy BMI were back transformed and then added to the dataset for the 187 women without a pre-pregnancy BMI recorded. If participants were missing data for any of the other variables in the MFMU VBAC model, they were excluded from the analysis. A flow diagram of the final study population is presented in Figure 1.
Figure 1.
Flow diagram of study participants. *Patients excluded include those with more than two prior cesarean deliveries or those with fewer than two prior cesarean deliveries; multiple gestation; malpresentation; prior classical, J, or T incision; preterm gestation (less than 37 weeks of gestation); antepartum stillbirth; or known fetal anomaly.
Women with a successful TOLAC were compared to those with a failed TOLAC based on demographic and clinical characteristics. Means with standard deviations or geometric means with a 95% geometric confidence interval were reported for continuous variables. Comparisons of demographics were made using exact Pearson chi-square for categorical measures or unequal-variance-two-sample-t-test (on the log scale if reporting geometric means) for continuous measures.
A receiver operating characteristic (ROC) curve was used to assess the classification ability of the model. The area under the curve (AUC) and 95% confidence intervals are reported. The overall likelihood of TOLAC success was compared between women with a successful VBAC and those with a failed TOLAC. In addition, the predicted likelihood of VBAC success was compared to the actual success rate using a calibration curve for each decile of predicted success probability with 95% confidence intervals. Strong agreement of predicted and observed rates was defined as when the predicted probability was similar to the observed rate, and a narrow 95% confidence interval for the predicted probability contained the observed rate. Whether the previously published algorithm would produce estimates that were in strong agreement with observed rates was assessed numerically by determining whether confidence interval limits contained observed estimates, and visually through depicting the observed and predicted rates through a calibration curve to assess the proximity of predicted rates and confidence intervals to the 45 degree line of agreement.
A p-value <0.05 was considered statistically significant. All analyses were performed in SAS.
Results
Of the 369 women who met inclusion criteria for the analysis and, after imputation, had complete data available for the VBAC model, 243 (66%, 95% CI 61, 71) had a successful TOLAC. When compared to women who had a failed TOLAC, women with a successful TOLAC had a lower mean BMI, were more likely to have a history of vaginal delivery or VBAC, and were less likely to have a history of recurring indication for cesarean or diabetes (Table 1).
Table 1.
Demographics of Study Population
| Characteristica,b | Successful TOLAC N=243 |
Failed TOLAC N=126 |
P valuec |
|---|---|---|---|
| Maternal age (years) | 29.5 (5.7) | 29.6 (5.3) | 0.85 |
| Pre-pregnancy BMI (kg/m2)d | 27.0 (26.3, 27.8) | 28.7 (27.5, 30.0) | 0.02 |
| Years since last cesarean | 4.0 (3.6, 4.5) | 3.5 (3.1, 4.0) | 0.11 |
| Race | |||
| African American | 127 (52.3) | 63 (50.0) | 0.86 |
| Caucasian | 85 (35.0) | 43 (34.1) | |
| Hispanic | 22 (9.1) | 15 (11.9) | |
| Other | 9 (3.7) | 5 (4.0) | |
| Recurring indication for either first or second cesarean | 103(42.4) | 79 (62.7) | <0.001 |
| Previous vaginal delivery | 154 (63.6) | 33 (26.2) | <0.001 |
| Previous vaginal birth after cesarean | 117 (52.9) | 24 (19.7) | <0.001 |
| Pre-existing diabetes mellitus | 7 (2.9) | 10 (7.9) | 0.04 |
| Other chronic medical conditione | 27 (11.1) | 16 (12.7) | 0.73 |
| Neonatal birth weight (grams) | 3291 (3232, 3351) | 3462 (3359, 3567) | 0.01 |
| Gestational age at delivery (days) | 276 (9) | 277 (10) | 0.17 |
TOLAC = trial of labor after cesarean
Number (%) reported for categorical variables
Mean with standard deviation or geometric mean and 95% geometric confidence interval reported for continuous variables
P-values from either exact Pearson chi-square for categorical measures or unequal-variance-two-sample-t-test (on the log scale if reporting geometric mean) for continuous measures
Pre-pregnancy body mass index (BMI) was imputed based on admission BMI and neonatal birth weight for n=105 of the successful TOLAC participants and n=49 of the failed TOLAC participants
Other chronic medical conditions included: chronic hypertension, other chronic cardiac disease, chronic renal disease, asthma, or connective tissue disorder
Using the MFMU VBAC calculator, the mean predicted probability of successful VBAC was 70% (95% CI 68, 72). The predicted probability of success was higher among women with a successful TOLAC (75%, 95% CI 73, 77) than those with a failed TOLAC (59%, 95% CI 55, 62). The overall difference in predicted success was 16% (95% CI 12, 21) (p<0.001).
The area under the ROC curve for prediction of VBAC for women with two prior cesareans was 0.74 (95% CI 0.69, 0.80), which is similar to that obtained for women with one prior cesarean (AUC in the original model among women with one prior cesarean delivery 0.75, 95% CI 0.74–0.77) (1). When only the women without an imputed BMI (n=251) were included in the analysis, the AUC remained high at 0.77 (0.70–0.83).
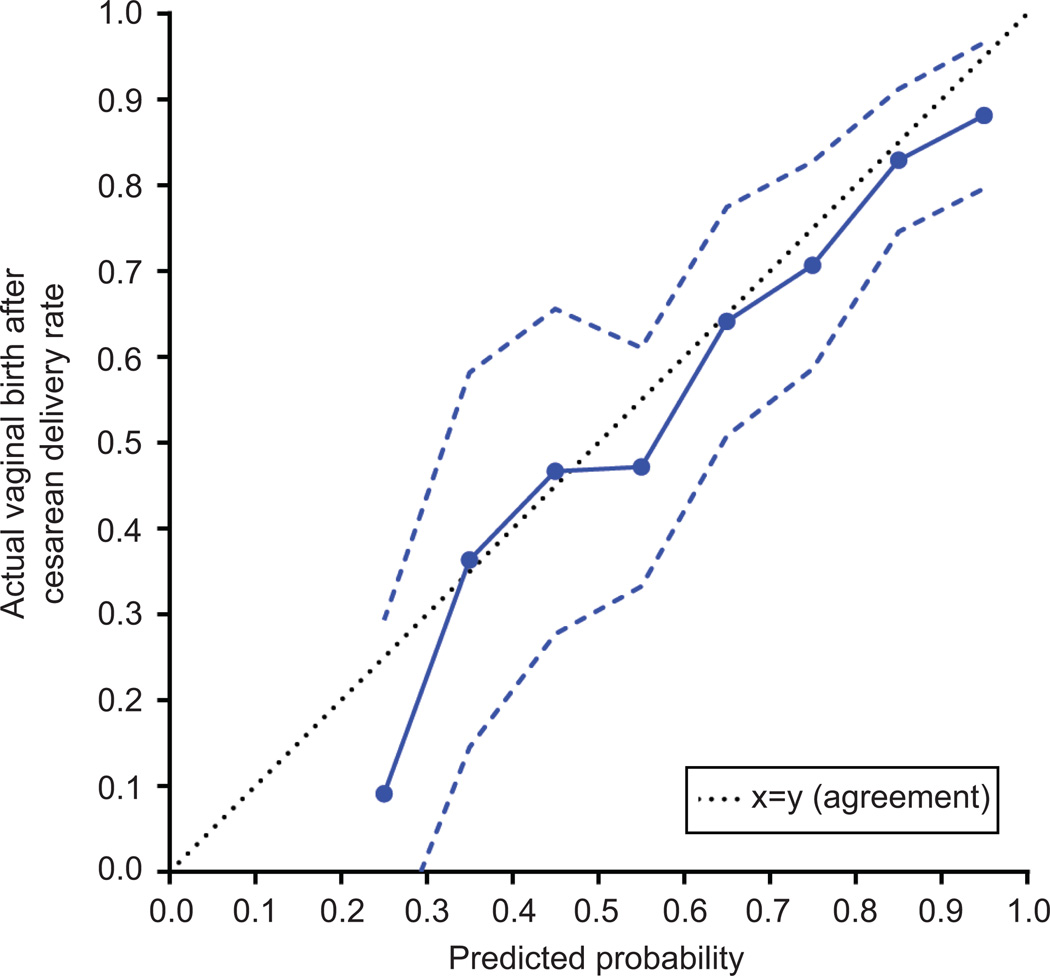
In addition, within each decile of predicted probability based on the MFMU VBAC prediction model (1), there was strong agreement between the predicted and actual probabilities of success (Figure 2, Table 2). For predicted probabilities of TOLAC success greater than 30% our sample size was adequate to demonstrate agreement with the actual probability of success within the 95% confidence interval of the calibration curve. Among women with a predicted probability of greater than 60% of TOLAC success, the confidence interval width narrowed to less than 10% indicating very good approximation of predicted with actual probabilities of success in this range.
Figure 2.
Calibration curve demonstrating the performance of the Maternal-Fetal Medicine Units Network vaginal birth after cesarean delivery (VBAC) prediction model in women with two prior cesarean deliveries. The mean rate of actual VBAC success within each decile of predicted probability is presented with 95% confidence intervals.
Table 2.
Performance of Maternal-Fetal Medicine Units Network (MFMU) vaginal birth after cesarean (VBAC) prediction model (1) in women with two prior cesarean deliveries
| MFMU VBAC Model Predicted Probability of VBAC Success |
Number of Women in Each Decile of Predicted VBAC Success |
Actual VBAC Success Ratea |
|---|---|---|
| .10-<.20 | 1 | 0 |
| .20-<.30 | 11 | 9.1 (11.2, 29.3) |
| .30-<.40 | 22 | 36.4 (14.5, 58.2) |
| .40-<.50 | 30 | 46.7 (27.7, 65.6) |
| .50-<.60 | 53 | 47.2 (33.3, 61.1) |
| .60-<.70 | 53 | 64.2 (50.8, 77.5) |
| .70-<.80 | 58 | 70.7 (58.6, 82.8) |
| .80-<.90 | 82 | 82.9 (74.6, 91.2) |
| .90-<1 | 59 | 88.1 (79.6, 96.6) |
VBAC = vaginal birth after cesarean
The mean rate of actual VBAC success within each decile of predicted probability with 95% confidence intervals
Discussion
We found that the MFMU VBAC prediction model (1) validated in women with one prior cesarean delivery also accurately predicts the likelihood of successful TOLAC in women with two prior cesarean deliveries. The AUC for the model in our population was 0.74, which is very similar to the reported AUC of 0.75 from the model that was developed in women with one prior cesarean delivery (1). The model had good overall predictive capability as well as strong correlation with actual success rates within each decile of predicted probability of TOLAC success.
Although it may seem intuitive that the same demographic and clinical factors that predict VBAC success in women with one prior cesarean delivery would also predict VBAC success in women with two prior cesarean deliveries, it is important to demonstrate this with data, rather than assumption, prior to applying existing models to this unique population. Whenever a woman undertakes TOLAC, the risks and benefits must be weighed. In women with two prior cesarean deliveries and a reasonable likelihood of VBAC success an attempted TOLAC may minimize the morbidity associated with another cesarean delivery, and all subsequent repeat cesarean deliveries (9).
VBAC models are intended as a tool for clinicians to assist with counseling women who are considering TOLAC. Ultimately many factors will play into a woman’s decision of repeat cesarean versus TOLAC. This tool is not intended to prevent motivated patients from pursuing a TOLAC.
For the purposes of this analysis, we categorized women as having a recurring indication for cesarean (arrest of dilation or descent) if they had a recurring indication for either their first or second cesarean delivery. We considered other possibilities, including only classifying women with a recurring indication for the first cesarean delivery as having a potentially recurring indication, as well as only including women as having a recurring indication if both prior cesarean deliveries were for a recurring indication. Neither of these alternate ways of classifying women as having a recurring indication for cesarean improved the overall predictive capability of the model (data not shown). Clinically it makes the most sense to include women as having a recurring indication if either of their prior cesarean deliveries were for an indication of arrest of dilation or descent, and the model demonstrated good predictive capability with this approach.
The biggest strength of this study is the size of the cohort. We were therefore able to assess the overall predictive capability and calibration of the model. There were too few women to demonstrate the precision of the model in women with a likelihood of success less than 30%, although for women with a likelihood of VBAC that is so low it is unlikely that even relatively large deviations of the predicted from the actual chance of VBAC would alter clinical decision making. Another strength of the study is that the data for the original MFMU observational Cesarean Registry study were collected prospectively with multiple checks to ensure accurate data collection which improves the overall integrity of the data (8).
The generalizability of the study to other populations cannot be known given that the data for the original trial were collected at academic medical centers participating in the MFMU. Labor management and characteristics of these women may therefore be more similar to the initial cohort with one prior cesarean delivery in which the model was developed than the general population. However, the VBAC prediction model created with one prior cesarean delivery in this dataset has been subsequently validated in several other populations worldwide (2–4). There is therefore reason to believe that the findings of this study in women with two prior cesareans (a different subset of the same larger population) also would be generalizable to other cohorts of women.
While this model predicts success in a cohort of women who attempted TOLAC, it does not address the counseling that led to other women who were candidates for TOLAC choosing repeat cesarean delivery. We do know, however, that TOLAC was offered at all institutions participating in the initial trial which should help to reduce this potential selection bias.
We recognize that there may be other predictors of TOLAC success in women with two prior cesareans. We did not try to create a new model with this analysis as the primary purpose was to validate an existing model that is currently available for use in practice. This clinical tool may enable practitioners to more effectively counsel women with two prior cesarean deliveries regarding their likelihood of successful TOLAC.
Acknowledgments
Supported in part by the Agency for Healthcare Research and Quality grant number R24 HS022143-01, and National Institutes of Health/National Center for Research Resources Colorado CCTSI grant number UL1 RR025780.
The authors thank the National Institute of Child Health and Human Development (NICHD) and the Maternal-Fetal Medicine Units Network for making the database from the Cesarean Registry available for secondary analysis.
The contents of this report represent the views of the authors and do not represent the views of the Eunice Kennedy Shriver NICHD Maternal-Fetal Medicine Units Network or the National Institutes of Health.
Footnotes
Presented as a poster at the Society for Maternal-Fetal Medicine Annual Meeting, Feb 5, 2015 in San Diego, CA.
Financial Disclosure: The authors did not report any potential conflicts of interest.
References
- 1.Grobman WA, Lai Y, Landon MB, et al. Development of a nomogram for prediction of vaginal birth after cesarean delivery. Obstet Gynecol. 2007;109(4):806–812. doi: 10.1097/01.AOG.0000259312.36053.02. [DOI] [PubMed] [Google Scholar]
- 2.Costantine MM, Fox K, Byers BD, et al. Validation of the prediction model for success of vaginal birth after cesarean delivery. Obstet Gynecol. 2009;114(5):1029–1033. doi: 10.1097/AOG.0b013e3181bb0dde. [DOI] [PubMed] [Google Scholar]
- 3.Yokoi A, Ishikawa K, Miyazaki K, et al. Validation of the prediction model for success of vaginal birth after cesarean delivery in Japanese women. Int J Med Sciences. 2012;9:488. doi: 10.7150/ijms.4682. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Chaillet N, Bujold E, Dubé E, Grobman WA. Validation of a prediction model for vaginal birth after cesarean. J Obstet Gynaecol Can. 2013;35:119. doi: 10.1016/S1701-2163(15)31015-X. [DOI] [PubMed] [Google Scholar]
- 5.American College of Obstetricians and Gynecologists. Vaginal Birth After Previous Cesarean Delivery. Practice Bulletin Number 115. Washington, DC: ACOG; 2010. Aug, [DOI] [PubMed] [Google Scholar]
- 6.Macones GA, Cahill A, Pare E, et al. Obstetric outcomes in women with two prior cesarean deliveries: is vaginal birth after cesarean delivery a viable option? Am J Obstet Gynecol. 2005;192:1223–1228. doi: 10.1016/j.ajog.2004.12.082. [DOI] [PubMed] [Google Scholar]
- 7.Landon MB, Spong CY, Thom E, et al. Risk of uterine rupture with a trial of labor in women with multiple and single prior cesarean delivery. National Institute of Child Health and Human Development (NICHD) Maternal-Fetal Medicine Units Network (MFMU) Obstet Gynecol. 2006;108:12–20. doi: 10.1097/01.AOG.0000224694.32531.f3. [DOI] [PubMed] [Google Scholar]
- 8.Landon MB, Hauth JC, Leveno KJ, et al. Maternal and perinatal outcomes associated with a trial of labor after prior cesarean delivery. NEJM. 2004;351(25):2581–2589. doi: 10.1056/NEJMoa040405. [DOI] [PubMed] [Google Scholar]
- 9.Silver RM, Landon MB, Rouse DJ, et al. Maternal morbidity associated with multiple repeat cesarean deliveries. Obstet Gynecol. 2006;107:1226–1232. doi: 10.1097/01.AOG.0000219750.79480.84. [DOI] [PubMed] [Google Scholar]