Abstract
Objective/Purpose
To review data for ophthalmologists published online from the Physician Payments Sunshine Act.
Design
Retrospective data review using a publicly available electronic database
Methods: Main Outcome Measures
A database was downloaded from the Centers for Medicare and Medicaid Services (CMS) Website under Identified General Payments to Physicians and a primary specialty of ophthalmology. Basic statistical analysis was performed including mean, median and range of payments for both single payments and per provider. Data were also summarized by category of payment, geographic region and compared with other surgical subspecialties.
Results
From August 1, 2013 to December 31, 2013, a total of 55,996 individual payments were reported to 9,855 ophthalmologists for a total of $10,926,447. The mean amount received in a single payment was $195.13 (range $0.04–$193,073). The mean amount received per physician ID was $1,108 (range $1–$397,849) and median amount $112.01. Consulting fees made up the largest percentage of fees. There was not a large difference in payments received by region. The mean payments for the subspecialties of dermatology, neurosurgery, orthopedic surgery and urology ranged from $954–$6,980, and median payments in each field by provider identifier ranged from $88–$173.
Conclusions
A large amount of data was released by CMS for the Physician Payment Sunshine Act. In ophthalmology, mean and median payments per physician did not vary greatly from other surgical subspecialties. Most single payments were under $100, and most physicians received less than $500 in total payments. Payments for consulting made up the largest category of spending. How this affects patient perception, patient care and medical costs warrants further study.
Introduction
As a part of the Affordable Care Act in 2010, a provision known as the Physician Payments Sunshine Act was established to provide greater transparency of physician and hospital relationships with industry.1 As many as 94% of US Physicians have relationships with industry through research, consulting, medical education and gifts.2,3 However patients tend to be unaware about their physicians’ financial ties, and generally believe they should be disclosed.2
Under the law, any payments or transfer of value, which may include cash, gifts, services, and stock to a licensed physician must be reported if the payment was made by a drug or device manufacturer who manufactures a product covered by a government-sponsored health program.1 This includes payments for consulting, gifts, food, travel, education, grants, research, ownership, licenses, royalties, speaker honoraria and charitable contributions. Small payments of less than $10 are not reported unless in aggregate the payments exceed $100 in a calendar year.1 Sample medications, educational materials for patients, trial loans of devices, discounts, rebates and dividends need not be reported.1
On September 30, 2014, the database was released publicly in several formats including a website, online database and downloadable files.4 General payments details, research payment details and physician ownership details were each released along with identified and de-identified information. The purpose of this evaluation is to review the identified general payments data to determine the characteristics of payments to providers with primary specialty identified as ophthalmology, and compare this with several other surgical subspecialties.
Methods
The study was a retrospective analysis using the Centers for Medicare and Medicaid Services (CMS) Open Payments website and data based on primary physician specialty.4 Each data point included a single payment in US dollars to a single physician by an entity. The primary taxonomy specialties of dermatology, neurosurgery, orthopedics and urology were selected for comparison to ophthalmology. If several taxonomies applied to the specialty, then these were evaluated in aggregate (for example, Dermatology included those with specialty of Dermatology, Dermatology Mohs Surgery, Procedural Dermatology). Microsoft Excel software (Microsoft Corporation, Redmond, WA) was then used to evaluate these data sets. Basic statistical calculations including average, median and range were calculated for each specialty. In ophthalmology, additional calculations were performed to calculate total payments to each provider based on Medicare provider ID, by US state and region, by type of charge, and by type of company or product.
When reviewing these data by region, states were divided into the following groups: Northeast (Connecticut, Massachusetts, Maine, New Hampshire, New Jersey, New York, Pennsylvania, Rhode Island and Vermont), Midwest (Iowa, Illinois, Kansas, Michigan, Minnesota, Missouri, North Dakota, Nebraska, Ohio, South Dakota, Indiana, Wisconsin), South (Alabama, Arkansas, Washington DC, Delaware, Florida, Georgia, Kentucky, Louisiana, Maryland, Mississippi, North Carolina, South Carolina, Oklahoma, Tennessee, Texas, Virginia, West Virginia, Puerto Rico, Virgin Islands), and West (Alaska, Arizona, California, Colorado, Hawaii, Idaho, Montana, New Mexico, Nevada, Oregon, Utah, Washington, Wyoming).
Each payment had the option to be recorded with data regarding the company and covered drug, biological or medical device. The entries were divided into the following categories: ophthalmic medication, ophthalmic surgery, ophthalmic diagnostic instrument, ophthalmic miscellaneous, systemic therapy, and category not available. If no product or device was noted then the author decided the nature of the company based on their clinical care products. In some cases the companies or organizations specialize in primarily ophthalmic medications, devices and instruments and were placed in these categories. In other cases, the companies or organizations had diverse product lines in multiple ophthalmic or medical specialties and it was not possible to derive the category. In the case of systemic medications that may be used in multiple diseases, but also in ophthalmology, the therapy was considered to fall into the category of systemic therapy.
The de-identified data were not downloaded due to file size and lack of additional demographic information. In addition, de-identified data included contested entries. Data were limited only to the general payments dataset.
Results
For physicians with primary specialty of ophthalmology, a total of 55,996 individual payments were recorded from August 1, 2013 to December 31, 2013. None of the payments reported in this database were marked as disputed. The total amount of payments reported was $10,926,447. The mean payment amount was $195.13 (range $0.04–$193,073), and a distribution of payment amounts by dollar range is noted in Table 1.
Table 1.
Distribution of single payments by dollar amount
| Dollar Range of payment (US $) | Number of payments |
|---|---|
| <$10 | 11,357 |
| $11–$50 | 29,299 |
| $51–$100 | 5,037 |
| $101–$500 | 7,179 |
| $501–$1,000 | 852 |
| $1,001–$5,000 | 2,024 |
| $5,001–$10,000 | 156 |
| $10,001–15,000 | 39 |
| $15,001–$20,000 | 27 |
| $20,001–$25,000 | 11 |
| > $25,000 | 15 |
A total of 9,855 unique physician profile identification (ID) numbers received payments, an average of 5.7 payments per physician ID. The average received per physician ID was $1,108 (range $1–$397,849) with median $112.01. Table 2 summarizes the distribution of payments by dollar range per provider ID.
Table 2.
Distribution of total payments to each provider ID
| Dollar Range of payment (US $) | Number of provider ID’s |
|---|---|
| <$50 | 3,035 |
| $51–$100 | 1,501 |
| $101–$500 | 4,141 |
| $501–$1,000 | 384 |
| $1,001–$5,000 | 453 |
| $5,001–$10,000 | 120 |
| $10,001–15,000 | 64 |
| $15,001–$20,000 | 45 |
| $20,001–$25,000 | 17 |
| $25,001–$50,000 | 60 |
| $50,001–$100,000 | 26 |
| >$100,000 | 9 |
The following categories were supplied for the “Nature of payment” classification: Charitable contribution, Compensation for services other than consulting, including serving as faculty or as a speaker at a venue other than a continuing education program, Compensation for serving as faculty or as a speaker for an accredited or certified continuing education program, Consulting Fee, Current or prospective ownership or investment interest, Education, Entertainment, Food and Beverage, Gift, Grant, Honoraria, Royalty or License, Travel and Lodging. The distributions across these categories are represented in Table 3. The greatest percentage went to Consulting Fees, followed by Compensation for services other than consulting, including serving as faculty or as a speaker at a venue other than a continuing education program, Food and Beverage and Travel and Lodging. The largest single amount received was in the category of Royalty or License, for an amount of $193,073. The greatest number of payments was in the Food and Beverage category, 9,479.
Table 3.
Distribution of Payment Categories
| Category | Total | Percent of Overall | # of payments | Min | Max | Mean |
|---|---|---|---|---|---|---|
| Charitable Contribution | $7,200 | 0.07% | 2 | $2,200 | $5,000 | $3,600 |
| Consulting Fee | $4,588,395 | 42% | 521 | $10.70 | $50,000 | $3,313 |
| Current or prospective ownership or investment interest | $2,588 | 0.02% | 3 | $500 | $1,200 | $863 |
| Education | $477,276 | 4.4% | 1237 | $0.24 | $11,076.56 | $280 |
| Entertainment | $2,463 | 0.02% | 46 | $14.57 | $150 | $48 |
| Food and Beverage | $1,610,832 | 15% | 9479 | $0.04 | $2,500 | $33 |
| Gift | $66,641 | 0.6% | 170 | $5.01 | $5,499.66 | $298 |
| Grant | $47,750 | 0.4% | 6 | $250 | $20,000 | $6,821 |
| Honoraria | $129,581 | 1.2% | 136 | $88.84 | $10,000 | $1,800 |
| Royalty or License | $964,046 | 8.8% | 13 | $20.64 | $193,072.68 | $40,169 |
| Services other than consulting, including serving as faculty/speaker at a venue other than a continuing education program | $1,686,316 | 15.43% | 439 | $5.95 | $21,800 | $1,847 |
| Faculty/speaker for an non-accredited/noncertified continuing education program | $158,805 | 1.5% | 59 | $280 | $6,500 | $2,036 |
| Faculty/speaker for an accredited/certified continuing education program | $7,000 | 0.06% | 2 | $1,000 | $6,000 | $3,500 |
| Travel and Lodging | $1,177,555 | 10.8% | 665 | $0.57 | $11,329.60 | $413 |
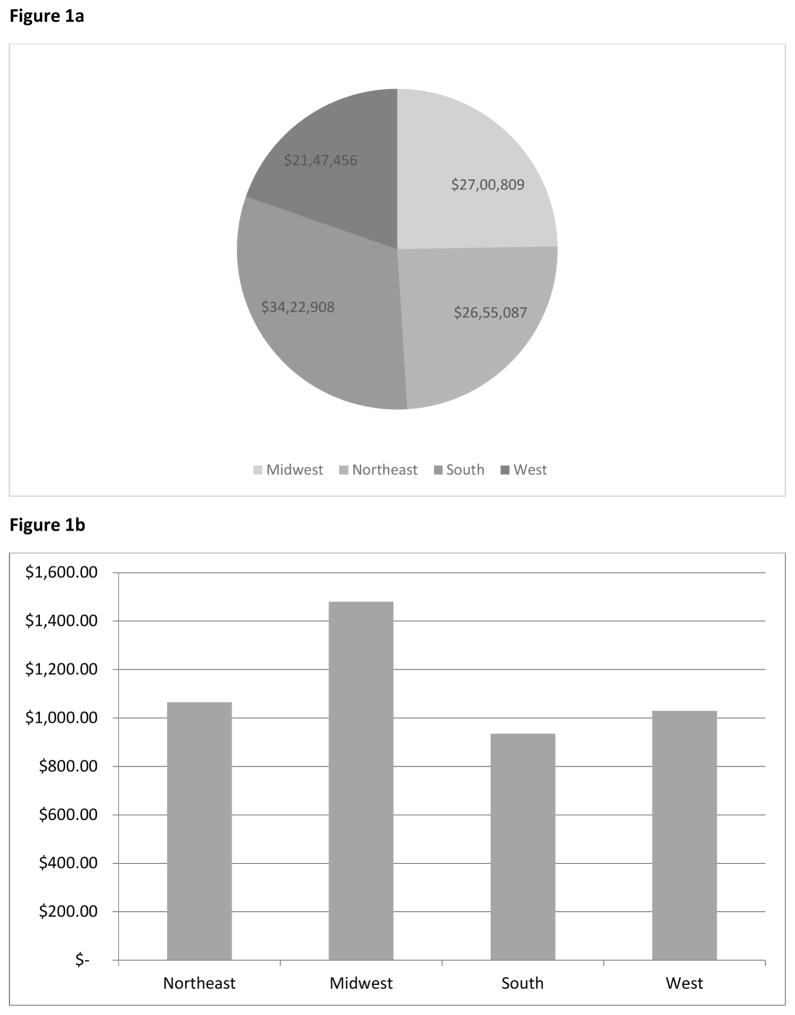
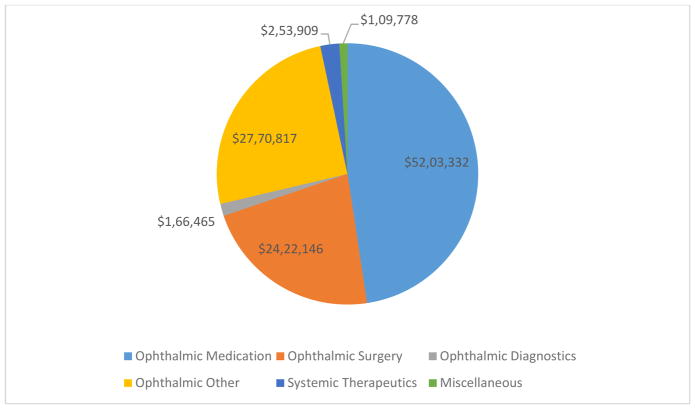
Figures 1a and 1b summarize the payments by geographic region, with the highest dollar amount going towards physicians in the South, followed by the Midwest, Northeast and West. When evaluating average payment per provider in each geographic region, the average was $1,479 in the Midwest, $1,065 in the Northeast, $1,030 in the West and $935 in the South. There was one payment assigned to a provider with no listed address of $197. A summary of payments by medication and device type is summarized in Figure 2, with the greatest dollars in the category of ophthalmic medications, followed by ophthalmic with no category and ophthalmic surgical devices. Table 4 compares the payments in ophthalmology with dermatology, neurosurgery, orthopedics and urology by total dollars, with a mean, median and range of dollars per provider ID. The mean payment per physician in these specialties ranged from $954–$6,980 and the median payment per physician ranged from $88–173.
Figure 1.
Figure 1a – Distribution of payments to providers by geographic region
All sums are reported in US Dollars. The geographic region was determined by the state in the address listed for each provider.
Figure 1b - Average payments received per physician ID by each geographic region
All sums are reported in US Dollars. The geographic region was determined by the state in the address listed for each provider. Some providers may have received payments attributed to different regions.
Figure 2.
Distribution of payments based on medication or device
All sums are reported in US Dollars. The determination of category for each payment was based on the reported device or medication. In some instances the author’s discretion was used to categorize the payments as noted in the Methods section.
Table 4.
Comparison across selected surgical subspecialties
| Specialty | Total Dollars | Mean per physician ID | Min | Max | Median |
|---|---|---|---|---|---|
| Dermatology | $6,924,255 | $954 | $1.06 | $93,927 | $102 |
| Neurosurgery | $5,848,473 | $3,459 | $1.57 | $1,252,971 | $88 |
| Ophthalmology | $10,926,447 | $1,108 | $1.04 | $397,849 | $112 |
| Orthopedics | $105,269,422 | $6,980 | $1.21 | $7,356,275 | $118 |
| Urology | $8,383,598 | $1,364 | $0 | $250,919 | $173 |
Discussion
The Physician Payments Sunshine Act has provided a large amount of data previously unavailable for the purpose of providing transparency in medical care. However this sizeable database is unmanageable for the average person as the overall data file exceeds sizes that can be downloaded simply or managed in popular commercial programs like Microsoft Excel. The easiest way to view these data was in portions at a time, as in this analysis.
Because of the enormity of the database and the configuration of the online tools, the easiest way to find information is to search for an individual provider. Retrieving individual numbers does not provide context of behavior and so a purpose of this report was to provide contextual information. The results allow for greater comparison and understanding of the details in payments to ophthalmologists, and to see if this differed greatly from other surgical subspecialties. From this analysis, 20.3% of the individual payments to ophthalmologists were listed as $10 or less, and 72.6% of the payments were $50 or less, suggesting that most of the individual payments were relatively small. Less than $500 total was received by 88% of the physician IDs reported in the field, as the largest expenditures went to a small group of physicians. Over 86% of the individual payments were categorized as “Food and beverage,” however the total spending in this category only made up 15% of the overall spending. The “Travel and lodging” category consisted of 11% of the spending. The results are consistent with the survey reported by Campbell, et al of other subspecialties, where sponsored food was the most common industry relationship reported by physicians.3 In their systematic review of patient opinions, Licurse et al, found that payments for food and trips were the most unfavorably viewed.2 Grande, et al reported that inexpensive promotional items had some effect on medical school students’ opinions of statin medications for hypercholesterolemia, and perhaps even though the vast majority of expenditures are small, they may also affect opinions of physicians.5 Another survey of pharmaceutical gifts noted that patients tend to view pharmaceutical gifts more negatively than physicians did.6
Consulting fees (42%) made up the largest category of expenditures, likely due to the average consulting fee being much higher than the average payment ($3,313 vs $195.13). While consulting payments made up the bulk of the spending, patients have a more favorable view of their physicians receiving these payments.7,8 In those studies the authors suggested that patients may believe a physician who is a consultant is most up-to-date with information, influential, or a key opinion leader (KOL).7,8 From a business standpoint, investing in physicians with a reputation for being KOLs, has greater return, likely explaining the higher fees for this segment as well as the speaker fees.
Some of the categories may overlap as it may be difficult to differentiate between a consultant physician who gives a presentation as Consulting, Education or Services other than consulting including serving as a faculty or speaker. Each category may have a different public stigmata. Since each category had a sizeable dollar allocation it is unlikely that there is misrepresentation in these categories. Only two entries were noted for the category of Faculty or speaker at an accredited/certified continuing education program. This may be due to changing regulations regarding industry sponsorship for education programs. Many education programs are run by third parties that may or may not have industry relationships and the spending for these is not disclosed in this report because they are not necessarily related to a single product.
There did not seem to be large variations by geography. While the sum of dollars was spent in the South region, on a per physician basis, it was higher in the Midwest region and lowest in the South. Higher spending in the South than in other regions is most likely because two of the largest single payments ($193,072.68 and $187,987.68 in the category of Royalty or License) was in the South. A state law restricting physicians from accepting meals in Massachusetts was in effect from 2010–2012. Only 8% percent of dollars in this state went to the Food and Beverage category as opposed to 15% nationally, suggesting there may be a lingering effect from this legislation.
As compared to other surgical subspecialties there was not a large difference in the amount the median physician in each specialty appears to have received. While the mean amounts varied somewhat, this appears to be an effect from the highest sums received. In general the range at the upper end has greater variance and this may be related to medical devices and royalty payments.
Most of the dollars came from companies associated with ophthalmic medications, and surgical and diagnostic equipment, with medications making up the largest share. This is probably due to the medications having the greatest audience within the ophthalmology group, whereas surgical equipment can vary between subspecialties. Of note, sample medications and instruments are not included and may affect physician choices9,10. By extension sample surgical instruments allow a surgeon to gain familiarity influencing future purchases. A counter argument could be presented that sample medications do benefit patients with limited insurance or pharmaceutical coverage.11,12
The impact of this information on public perception is unknown. Generally speaking, patient understanding of physician compensation is poor.13 Perhaps some might interpret receiving money from industry as beneficial, and do not mind if their physician is involved in innovation or consulting7,8 whereas others may interpret this as undue influence.2 Grady, et al demonstrated that a percentage of their patient cohort felt that the payments physicians received was a “private matter.”14 Some patients want full disclosure of financial relationships,15 although others have reported in studies that they would still participate in research regardless of the involvement of their doctors in industry.7,8,16 In a contrasting study, Kim et al, found that 64–87% of subjects in a research trial wanted to know the financial influences of the researchers.17
Other areas where industry has influence, such as direct-to-consumer marketing and advertising to non-physicians (departmental managers or staff), are not reflected in this report, and their relative impact on costs and decision making is unknown. Sponsorships of local and national meetings and drug reimbursement programs also are not included in these costs and are also likely impactful. Resident physicians are excluded from the report and this may be important as targeting younger physicians may be more effective as their practice patterns are still relatively malleable.10
Some have even suggested that this spending and influence may be beneficial and should be increased.18 Disclosure of financial relationships improved patient loyalty to physicians in one study with less than 5% of patients feeling less loyal to their physicians after financial disclosure information was provided.19
Limitations to the analysis include the short time period of August to December 2013, so it is not known if this can be extrapolated to full year data. The database is dependent on the vendors for their entry and accuracy. Physicians had the opportunity to dispute claims; however, this system encountered errors and may not have been fully utilized by each physician. Investment income or ownership in a company were not reported in this particular database. Geographic data were based on physician’s listed mailing address and it is unclear if bundled payments to a group were attributed to individuals. These data are for only one time point so no information regarding trends over time can be assessed as of yet.
As our society moves towards more open disclosures, the availability of data may prove beneficial. At this time, it remains to be seen how this information will affect the ever-present relationships between physicians, patients and industry.
Acknowledgments
Financial Support: Supported by National Institute of Health Core grant 5P30EY019007 and unrestricted funds from Research to Prevent Blindness and Columbia University, New York.
Footnotes
Disclosures: The author is among physicians reported in the data set evaluated.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Agrawal S, Brennan N, Budetti P. The Sunshine Act – Effects on Physicians. New Eng J Med. 2013;368:2054–7. doi: 10.1056/NEJMp1303523. [DOI] [PubMed] [Google Scholar]
- 2.Licurse A, Barber E, Joffe S, Cross C. The Impact of Disclosing Financial Ties in Research and Clinical Care, A Systematic Review. JAMA Int Med. 2010:675–82. doi: 10.1001/archinternmed.2010.39. [DOI] [PubMed] [Google Scholar]
- 3.Campbell EG, Gruen RL, Mountford J, et al. A National Survey of Physician-Industry Relationships. New Eng J Med. 2007;356:1742–50. doi: 10.1056/NEJMsa064508. [DOI] [PubMed] [Google Scholar]
- 4. [Accessed October 2, 2014];General Payment Data with Identifying Recipient Information – Detailed Dataset 2013 Reporting Year. Available at: https://openpaymentsdata.cms.gov/dataset/General-Payment-Data-with-Identifying-Recipient-In/hrpy-hqv8.
- 5.Grande D, Frosch DL, Perkins AW, Kahn BE. Effect of Exposure to Small Pharmaceutical Promotional Items on Treatment Preferences. Arch Intern Med. 2009;169:887–93. doi: 10.1001/archinternmed.2009.64. [DOI] [PubMed] [Google Scholar]
- 6.Gibbons RV, Landry FJ, Blouch DL, et al. A Comparison of Physicians’ and Patients’ Attitudes Toward Pharmaceutical Industry Gifts. J Gen Intern Med. 1998;13:151–4. doi: 10.1046/j.1525-1497.1998.00048.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Hampson LA, Agrawal M, Joffe S, et al. Patients’ Views on Financial Conflicts of Interest in Cancer Research Trials. New Eng J Med. 2006;355:2330–7. doi: 10.1056/NEJMsa064160. [DOI] [PubMed] [Google Scholar]
- 8.Khan MH, Lee JY, Rihn JA, et al. The Surgeon as a Consultant for Medical Device Manufacturers. What Do Our Patients Think? Spine. 2007;32:2616–8. doi: 10.1097/BRS.0b013e318158cc3a. [DOI] [PubMed] [Google Scholar]
- 9.Chew LD, O’Young TS, Hazlet TK, et al. A physician survey on the effect of drug sample availability on physicians’ behavior. J Gen Intern Med. 2000;15:478–83. doi: 10.1046/j.1525-1497.2000.08014.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Adair RF, Holmgren LR. Do drug samples influence resident prescribing behavior? A randomized trial. Am J Med. 2005;118:881–4. doi: 10.1016/j.amjmed.2005.02.031. [DOI] [PubMed] [Google Scholar]
- 11.Bastiaens L, Chowdhury S, Gitelman L. Medication samples and drug compliance. Psychiatr Serv. 2000;51:819. doi: 10.1176/appi.ps.51.6.819. [DOI] [PubMed] [Google Scholar]
- 12.Cutrona SL, Woolhandler S, Lasser KE, et al. Characteristics of recipients of free prescription drug samples: a nationally representative analysis. Am J Public Health. 2008;98:284–9. doi: 10.2105/AJPH.2007.114249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Kao AC, Zaslavsky AM, Green DC, et al. Physician incentives and disclosure of payment methods to patients. J Gen Intern Med. 2001;16:181–8. doi: 10.1111/j.1525-1497.2001.04139.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Grady C, Horstman E, Sussman JS, Hull SC. The Limits of Disclosure: What Research Subjects Want to Know about Investigator Financial Interests. J Law Med Ethics. 2006;34:592–9. doi: 10.1111/j.1748-720x.2006.00073.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Tattersall MHN, Dimoska A, Gan K. Patients expect transparency in doctors’ relationships with the pharmaceutical industry. Med J Aust. 2009;190:65–8. doi: 10.5694/j.1326-5377.2009.tb02277.x. [DOI] [PubMed] [Google Scholar]
- 16.Weinfurt KP, Hall MA, Dinan MA, et al. Effects of Disclosing Financial Interests on Attitudes Toward Clinical Research. J Gen Intern Med. 2008;23:860–6. doi: 10.1007/s11606-008-0590-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Kim SYH, Millard RW, Nisbet P, et al. Potential research participants’ views regarding researcher and institutional financial conflicts of interest. J Med Ethics. 2004;30:73–9. doi: 10.1136/jme.2002.001461. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Manchanda P, Honka E. The Effects and Role of Direct-to-Physician Marketing in the Pharmaceutical Industry: An Integrative Review. Yale J Health Pol icy Law Ethics. 2013;5:785–822. [PubMed] [Google Scholar]
- 19.Pearson SD, Kleinman K, Rusinak D, Levinson W. A trial disclosing physicians’ financial incentives to patients. Arch Intern Med. 2006;166:623–8. doi: 10.1001/archinte.166.6.623. [DOI] [PubMed] [Google Scholar]