Abstract
Supplemental melatonin has been used to treat sleep onset insomnia in children with autism spectrum disorders (ASD), although the mechanism of action is uncertain. We assessed endogenous and supplemental melatonin profiles in relation to sleep in nine children with ASD. In endogenous samples, maximal melatonin concentration (Cmax) and time to peak concentration (Tmax) were comparable to those previously published in the literature for typically developing children, and dim light melatonin onsets were captured in the majority of children. In treatment samples (supplemental melatonin), melatonin parameters were also comparable to those previously published for typically developing children. Our findings support that children with ASD and insomnia responsive to low dose melatonin treatment have relatively normal profiles of endogenous and supplemental melatonin.
Keywords: Insomnia, N-acetylserotonin, Dim light melatonin onset
Introduction
Autism spectrum disorders (ASD) are one of the most common neurodevelopmental disorders with a prevalence rate currently estimated in 1:88 children (Centers for Disease Control and Prevention 2012). Sleep difficulties occur in 50–80 % of the children, with insomnia (difficulty initiating or maintaining sleep) a major concern (Couturier et al. 2005; Goldman et al. 2012; Krakowiak et al. 2008; Souders et al. 2009). Disordered sleep may exacerbate social interactions, repetitive behaviors, affective problems, and inattention/hyperactivity (Gabriels et al. 2005; Goldman et al. 2012, 2009; Malow et al. 2006; Schreck et al. 2004).
Circadian abnormalities have been postulated as underlying contributors to these sleep disturbances (Glickman 2010). Melatonin, produced in the pineal gland, is a key regulator of the circadian system. Melatonin, taken as a dietary supplement, has shown promise in reducing sleep latency in children with ASD in our work (Andersen et al. 2008; Malow et al. 2012) and in a recent review (Rossignol and Frye 2011). One hypothesis why melatonin may be effective in treating the insomnia associated with ASD is that it is treating a deficiency state. Relatively low levels of blood melatonin or the urinary metabolite 6-sul-foxymelatonin, sampled overnight (Kulman et al. 2000; Nir et al. 1995; Tordjman et al. 2005) or during the day (Melke et al. 2008) have been reported. However, with the exception of one study relating low levels of 6-sul-foxymelatonin to reduced proportion of delta sleep (Leu et al. 2011), our understanding of endogenous and supplemental melatonin pharmacokinetics (PKs) in relation to sleep patterns in children with ASD is limited.
Therefore, the aim of our study was to describe overnight endogenous and PK melatonin profiles in children with ASD participating in an open-label trial of melatonin for sleep onset insomnia. To accomplish this aim, we analyzed key parameters in relation to sleep recordings, as well as in relation to data published previously in children with ASD and of typical development. These parameters included: (1) The dim light melatonin onset (DLMO) of endogenous melatonin. The DLMO is a reliable marker of circadian phase, occurring approximately 2 h before sleep onset (Burgess and Fogg 2008); (2) The concentration and timing of peak endogenous melatonin; (3) PK parameters [maximal concentration of melatonin (Cmax), time to maximal concentration (Tmax), area under the curve (AUC), half-life (t1/2), clearance (CI), and volume of distribution (Vz)]. We hypothesized that melatonin profiles in children with ASD would be abnormal, showing delays in the timing or peak levels of melatonin compared to those described in the literature for children of typical development.
The relationship of the melatonin precursor, N-ace-tylserotonin, to melatonin was also determined. We hypothesized that endogenous N-acetylserotonin concentrations would be inversely related to endogenous melatonin concentrations due to abnormalities in acetylserotonin-O-methyltransferase (ASMT), the enzyme which converts NAS to melatonin in the pineal gland.
Methods
Study Sample
Details of the recruitment and study design are described in prior work (Malow et al. 2012). Briefly, children who met the clinical diagnosis of either autistic disorder, pervasive developmental disorder—not otherwise specified, or Asperger’s disorder by DSM-IV-TR criteria (American Psychiatric Association 2000) and confirmed with the autism diagnostic observation schedule (ADOS) (Lord et al. 2000), were recruited from subspecialty clinics and neighboring regions. For the purposes of this report, these clinical diagnoses are referred to collectively as autism spectrum disorder (ASD). Children were between the ages of 3 and 10 years and took at least 30 min or longer at baseline to fall asleep on three or more nights (by parent report and actigraphy), and were free of psychotropic medications. They were all prepubertal (as documented by physical examination). This study was approved by our Institutional Review Board and all parents of children provided informed consent. All children underwent a comprehensive medical evaluation to exclude medical comorbidities and had a comprehensive sleep interview. Parents then received structured education to address sleep habits, emphasize the importance of a regular bedtime and wake time, implement a calming bedtime routine, and provide guidance in managing night wakings. Children were initially started on an inert (placebo) liquid for 2 weeks, to obtain baseline data. They then began on 1 mg of melatonin for 3 weeks taken 30 min before bedtime. If sleep latency, as measured by actigraphy, remained above 30 min on two or more nights in at least one of the weeks, the dose was escalated to 3 mg for 3 weeks. If sleep latency, as measured by actigraphy, remained above 30 min on two or more nights in at least one of the weeks, the dose was escalated to 6 mg for 3 weeks. While an escalation as high as 9 mg was allowed, no children required this level of dose escalation. The entire trial lasted 17 weeks, with children wearing actigraphy monitors continuously throughout the trial.
The nine children described in this paper represent a subset of the 24 children included in a larger study (Malow et al. 2012). Parents of these nine children gave informed consent (with children 7 years of age or older providing assent), to participate in overnight polysomnography and serial blood draws at baseline and at each dose of supplemental melatonin. A previous study from our group related urinary melatonin metabolite levels to polysomnography (Leu et al. 2011)—none of the children in the current report participated in that study.
Melatonin Administration and Sampling
Children received an inert (placebo) liquid for 2 weeks during which time baseline actigraphy was collected throughout each night, and two nights of consecutive overnight PSG were performed in our institution’s sleep research core located in our clinical research center. The first night of PSG was included to allow the child to desensitize to a new and unfamiliar setting. On the second night of PSG, children underwent intravenous (IV) catheter placement for serial blood draws by pediatric emergency department nurses with specialized training in IV placement. The study team reviewed desensitization methods with each parent to prepare the child for IV placement. An individualized plan was created for each child and all team members who participated in the child’s care were trained on this plan. All endogenous samples were collected in a darkened room (<30 lux) with only brief exposure to light from a small pen light flashlight (as light exposure suppresses melatonin secretion). Catheter placement occurred early in the child’s overnight stay to avoid disruption of the child’s bedtime routine. The endogenous sampling began 10 min after the child received the inert dose (30 min before their established bedtime), determined by 3 weeks of wrist actigraphy in the home, and continued at 20, 30, 45, 60, 75, 90, 120, 150, 180, 240, 300, 360 and 480 min to define the child’s endogenous melatonin profile. We chose this sampling protocol to be consistent with the PK sampling protocol outlined below.
After endogenous sampling was completed, children began taking supplemental melatonin (liquid, immediate release, Natrol brand, Chatsworth, CA, USA) at home beginning at 1 mg, 30 min before bedtime, for 3 weeks and with continued collection of actigraphy throughout each night. Children returned for a one-night PSG during this 3 week period. On the PSG night, the child continued with their dose schedule of melatonin at 30 min prior to bedtime. The PK sampling began 10 min after melatonin administration continuing at 20, 30, 45, 60, 75, 90, 120, 150, 180, 240, 300, 360, and 480 min after melatonin to establish the child’s supplemental melatonin profile for the 1 mg dose. As mentioned above, if sleep latency, as measured by actigraphy, remained above 30 min on two or more nights in at least one of the weeks, the dose was escalated to 3 mg, with an additional night of overnight PSG with repeated sampling obtained using the same blood sampling protocol as for the 1 mg dose. Eight children had blood sampling at 1 mg and five participants had blood sampling at 3 mg. One participant was unable to have blood sampled at 1 mg as the parent was not able to get time off of work. This patient did require an escalation to 3 mg, however, and did have sampling at this dose.
Sleep Measurements
Sleep parameters (sleep onset latency, wake-after-sleep-onset (WASO), sleep efficiency, sleep duration) were computed for each participant for the 2-week baseline (inert) phase and each 3-week dosing phase using Actiware V 5 software (Philips Respironics). The sleep parameters from the night of PSG were also computed. As WASO does not provide a measure of discrete night wakings, parent-reported assessments of discrete night wakings were included using several sources, including the Children’s Sleep Habits Questionnaire (CSHQ) obtained at baseline and after treatment, sleep histories collected at baseline and at each dosing phase, and sleep diaries collected throughout the study on the CSHQ, night wakings (single and multiple) were classified as rarely (0–1 times a week), sometimes (2–4 times a week) or usually (5–7 times a week) as well as whether they were considered a problem.
Video-EEG-polysomnography was performed on digital systems (Neurofax EEG-1100, Polysmith 6.0, Nihon-Kohden Corporation, Tokyo, Japan). These included digital video recordings-time locked to the PSG recording, 21 channels of electroencephalography, two channels of electrooculography, three channels of electromyography, thermistor and nasal pressure transducer monitoring to measure airflow, thoracic and abdominal wall motion to measure respiratory effort, oximetry to measure oxygen saturation, electrocardiography, and leg electromyography. Bedtime in the laboratory was as close as possible to the child’s bedtime at home. The actiwatch and PSG were time-synchronized. Laboratory PSGs were scored by a registered PSG technologist using American Academy of Sleep Medicine (Iber et al. 2007) and reviewed by a sleep physician to ensure accuracy in scoring.
DLMO Calculations
For each endogenous melatonin profile, a 10 pg/ml threshold was used to calculate the DLMO (Benloucif et al. 2008). Each DLMO was calculated as the point in time (determined with linear interpolation) when the melatonin concentration exceeded 10 pg/ml. In participant 9, whose endogenous melatonin levels were ≥50 % lower than the other children, a threshold of 5 pg/ml was used (Lewy 1999). We reported sleep onset in relation to DLMO based on PSG (the night of the endogenous melatonin collection). We also reported sleep onset in relation to DLMO based on 2 weeks of actigraphy in the home during the 0 mg (inert) dosing period.
Analytical Method and Pharmacokinetics
Details of the analytical method used in the study are reported in (Carter et al. 2012). Briefly, blood was collected over an 8-h period and immediately placed on ice. Plasma was isolated within 45 min of blood collection. Baseline and PK plasma samples were analyzed in the Vanderbilt Bioanalytical Mass Spectrometry Core Facility by nanoflow LC–MS/MS and HPLC–MS/MS repectively (Carter et al. 2012). Nanoflow LC was necessary to reliably quantitate the low (pg/ml) endogenous levels of melatonin and N-acetylserotonin (NAS). PK parameters [maximal concentration of melatonin (Cmax), time to maximal concentration (Tmax), AUC, half-life (t1/2), clearance (CI), and volume of distribution (Vz)] were derived from plasma concentration versus time curves using the program Win-Nonlin v. 5.2 (Pharsight, Palo Alto, CA, USA). The data were analyzed using a noncompartment model as described in Carter et al. 2012. The LC–MS/MS analytical method was validated on a small group of adult volunteers (two male, two female, weight 72–109 kg, age 28–64 years, height 1.65–1.83 m). For the adult population, calculated PK parameters were consistent with literature values (Table SI and S2). The AUC and Cmax showed evidence of linear kinetics. The half-life (t1/2) and Tmax were not a function of dose.
Statistical Analysis
Data were analyzed using SAS software (version 9.1, SAS institute Inc., Cary, NC, USA), SPSS software (version 20, SPSS Inc., Chicago, IL, USA) and R (www.r-project.org). For sleep onset as measured by actigraphy, the median and interval for interquartile range (IQR) were calculated for each participant. Spearman correlations were performed to access the association between maximal endogenous melatonin concentration with participant age and weight. Related samples Wilcoxon Signed Rank Test was performed to test the hypothesis that sleep parameters improved from baseline to treatment. McNemar test was performed to test the hypothesis that single and multiple night wakings were equally likely to be a problem before and after treatment.
Results
Participants
Nine children (seven male, two female) participated in the serial blood sampling and overnight polysomnography for the PK portion of the study (Table 1). Children ranged in age from 3 to 8 years, mean (SD) 4.7 (1.5) years. Average weight was 21.1 (7.1) kg. All children were able to tolerate wearing the wrist actigraph for the entire study. Three children were not able to tolerate PSG at the time of the endogenous sampling. In these children, we used video to determine sleep onset. One of the children unable to tolerate PSG during endogenous sampling was also not able to tolerate PSG during PK sampling (treatment studies). All of the other children were able to tolerate PSG during the PK treatment studies. All children tolerated the melatonin administration and serial blood draws for the melatonin PK portion of the study. Review of PSG data documented that children remained asleep during the serial blood draws.
Table 1.
Participant characteristics and endogenous melatonin parameters
| Subject | Age, sex |
Weight (kg) |
DLMO (clock time) |
Sleep onset (PSG) |
Sleep onset (actigraphy) a median, IQR |
Maximum MEL concentration |
Clock time at peak MEL level |
Clock time at peak NAS |
Peak NAS level |
|---|---|---|---|---|---|---|---|---|---|
| 1 | 4, M | 15.50 | n/a | 21:00 | 21:08 (20:46, 21:37) |
126.1 | 22:05 | 21:30 | 8.5 |
| 2 | 8, M | 36.90 | n/a | 20:52 | 21:44 (21:28, 22:13) |
79.4 | 1:05 | 1:05 | 44.1 |
| 3 | 5, M | 17.40 | 22:14 | 21:43 | 23:00 (22:26, 23:51) |
156.3 | 1:40 | 0:10 | 15.1 |
| 4 | 4, M | 17.50 | 21:30 | 22:01 | 22:50 (22:24, 23:27) |
310.3 | 3:03 | 0:03 | 24.1 |
| 5 | 4, M | 21.36 | 21:29 | 20:52 | 22:53 (22:22, 23:21) |
100.0 | 2:40 | 1:38 | 26.8 |
| 6 | 4, M | 21.72 | n/a | 22:53 | 22:15 (21:59, 22:45) |
97.2 | 1:00 | 1:00 | 7.2 |
| 7 | 4, M | 17.10 | 21:44 | 21:53 | 22:18 (21:54, 23:04) |
217.8 | 2:30 | 22:00 | 38.9 |
| 8 | 3, F | 15.00 | 20:47 | 21:09 | 22:01 (21:17, 22:25) |
129.0 | 0:30 | 0:30 | 10.9 |
| 9 | 6, F | 27.70 | 20:51 | 20:13 | 20:45 (20:25, 21:15) |
42.4 | 1:50 | 21:50 | 13.4 |
Based on 2 weeks of actigraphy, excluding PSG nights
DLMO dim light melatonin onset, PSG polysomnography, IQR interquartile range, MEL melatonin, NAS N-acetylserotonin
Melatonin Blood Sampling
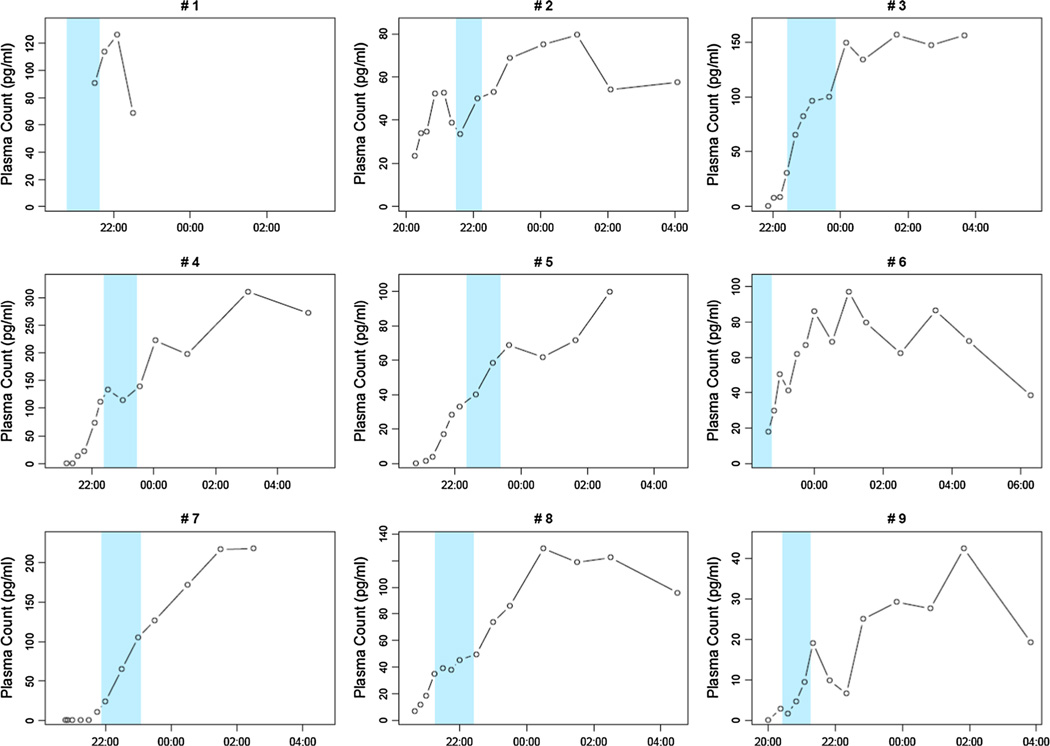
Endogenous melatonin profiles varied considerably by participant (Table 1; Fig. 1). In one participant (participant 1) complications with the IV precluded an entire night’s sampling, as well as determination of the DLMO. In two participants (participants 2 and 6) the DLMO was missed likely due to sampling starting after the DLMO occurred.
Fig. 1.
Endogenous melatonin levels in relation to time of night. The inter-quartile range for sleep onset latency corresponding with the 2 weeks of baseline actigraphy occurred as melatonin levels were rising (shaded area). Maximum melatonin concentration varied from 42.4 to 310.3 pg/ml. An IV malfunction in participant 1 limited sampling. In participants 2 and 6 no DLMO was obtained due to delay in sampling
DLMOs occurred between 20:47 and 22:14. The timing of the DLMO was closer to PSG sleep onset than sleep onset as measured by actigraphy (based on 2 weeks of data collected at home during the inert dosing period). The DLMOs in all children except one occurred before the median sleep onset, as determined from actigraphy. This child had the lowest maximum concentration of melatonin on the sampling night.
Peak plasma concentrations of endogenous melatonin occurred between 10:05 p.m. and 3:03 a.m. (Table 1). The inter-quartile range for SOL corresponding with the 2 weeks of baseline actigraphy (Table 1; Fig. 1) occurred as melatonin levels were rising. Maximum melatonin concentration varied from 42.4 to 310.3 pg/ml. Of note, the two lowest concentrations occurred in the children who had the highest weights. These children were also the oldest, although the maximum concentration of endogenous melatonin was inversely associated with participant weight (rs = −0.683, p = 0.04) but not age (r = −0.511; p = 0.16).
Endogenous N-Acetylserotonin (NAS) Findings in Relation to Endogenous Melatonin Profiles
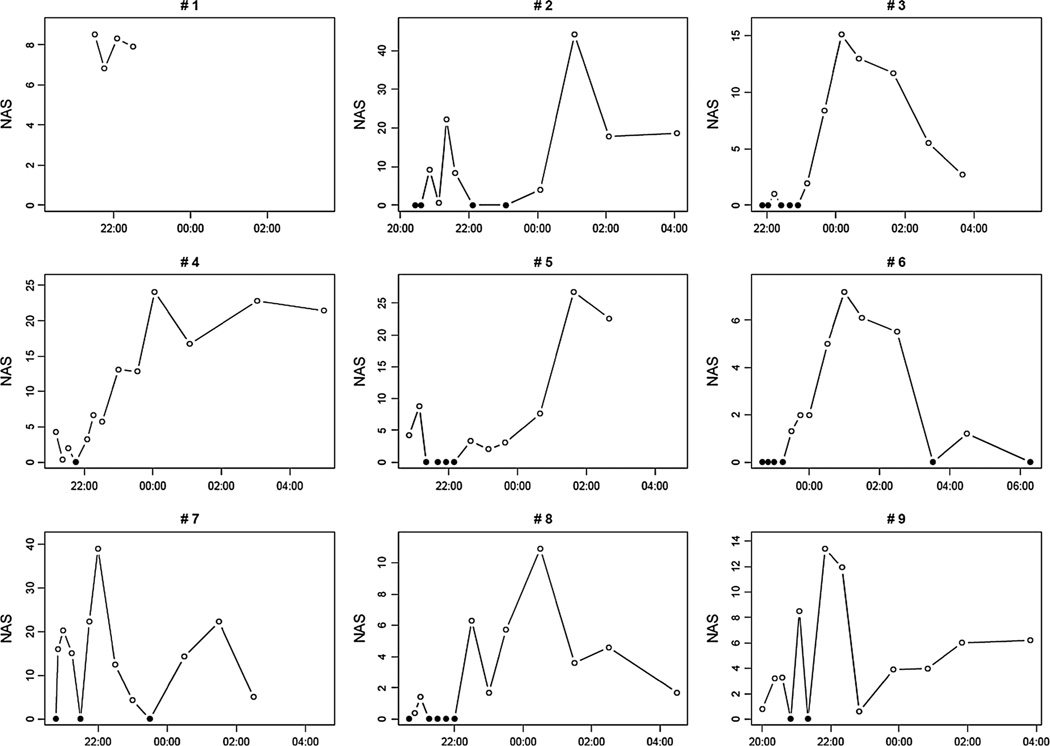
Peak NAS levels ranged from 7.2 to 44.1 (Table 1). The peak NAS level occurred within 90 min of the peak melatonin concentration in six participants, and at the same time as the peak melatonin concentration in three participants. The NAS profiles were not inversely related to melatonin profiles, with NAS concentration either paralleling the melatonin concentration or else randomly distributed (NAS; Fig. 2).
Fig. 2.
Endogenous N-acetylserotonin levels in relation to time of night. The zero values are represented as solid black circles to differentiate them from non-zero values. An IV malfunction in participant 1 limited sampling
Pharmacokinetic Parameters for Supplemental Melatonin
The PK parameters for supplemental melatonin at 1 and 3 mg doses are presented in Table 2. Published values of PK parameters for exogenous melatonin in plasmafrom young healthy human subjects are presented for comparison in Table S2.
Table 2.
Summary of PK data for exogenous oral melatonin at 1 and 3 mg doses
| Subject | Dose (mg) |
t1/2 (h) |
Tmax (h) |
Cmax (pg/ml) |
AUC0-tlast (pg/ml h) |
V/F (ml/kg) |
Cl/F (ml/h/kg) |
|---|---|---|---|---|---|---|---|
| 1 | 1 | 2.0 | 1.0 | 1,480 | 4,129 | 41,807 | 14,724 |
| – | |||||||
| 2 | 1 | 1.6 | 2.2 | 376 | 1,377 | 43,384 | 19,261 |
| – | |||||||
| 3 | 1 | 1.1 | 0.50 | 1,412 | 2,146 | 39,411 | 25,157 |
| 3 | 1.0 | 0.50 | 3,352 | 7,055 | 33,668 | 24,113 | |
| 4 | 1 | 0.68 | 1.0 | 4,180 | 8,329 | 6,457 | 6,586 |
| 3 | 1.1 | 1.0 | 8,709 | 22,679 | 11,940 | 7,444 | |
| 5 | 1 | 1.6 | 0.50 | 729 | 2,531 | 41,525 | 17,726 |
| 3 | 0.77 | 0.75 | 5,295 | 8,238 | 18,518 | 16,746 | |
| 6 | – | ||||||
| 3 | 0.88 | 0.37 | 17,324 | 18,385 | 9,497 | 7,480 | |
| 7 | 1 | 1.6 | 0.33 | 2,434 | 4,490 | 27,394 | 11,984 |
| – | |||||||
| 8 | 1 | 0.93 | 0.17 | 7,591 | 10,137 | 8,671 | 6,494 |
| 3 | 1.1 | 0.17 | 23,151 | 28,282 | 11,236 | 7,004 | |
| 9 | 1 | 1.3 | 0.18 | 1,841 | 2,963 | 21,575 | 11,710 |
| – | |||||||
| Mean (SD) | 1 (n = 8) | 1.3 (0.42) | 0.73 (0.67) | 2,505 (2,362) | 4,513 (3,119) | 28,778 (15,189) | 14,205 (6,401) |
| 3 (n = 5) | 0.97 (0.15) | 0.56 (0.33) | 11,566(8,401) | 16,928 (9,180) | 16,972 (9,940) | 12,557 (7,646) |
t1/2 = oral half-life; Cmax = maximum concentration of melatonin; Tmax = time to maximum concentration; AUC0-tlast = area under the concentration versus time curve determined to the last PK sampling time point; V/F = ratio of volume of distribution to bioavailability; Cl/F = ratio of clearance to bioavailability. For oral dosing, WinNonLin does not assume F = 100 %. The bioavailability of orally dosed melatonin is highly variable between subjects; literature values for F ranging from 0.01 to 0.3 have been reported in adult studies
Sleep Measurements
Sleep parameters are presented in Table 3. Sleep onset latency, measured by actigraphy, improved with supplemental melatonin treatment (comparing baseline and final treatment dose for each participant; p = 0.01). Other sleep parameters measured by PSG and actigraphy did not change. No children had sleep apnea, parasomnias (sleep walking, sleep terrors, confusional arousals, or REM behavior disorder) or seizures recorded on PSG.
Table 3.
Sleep parameters mean (SD) measured by actigraphy and polysomnography at each dose of melatonin
| Parameter | 0 mg | 1 mg | 3 mg | p valuea |
|---|---|---|---|---|
| Sleep latency (ACT) | 43.7 (19.6) | 30.8 (15.7) | 26.6 (10.2) | 0.01 |
| Sleep latency (PSG) | 13.4 (13.3) | 43.6 (67.0) | 10.8 (14.8) | 0.35 |
| Sleep duration (ACT) | 421.9 (48.4) | 439.1 (61.3) | 442.8 (48.0) | 0.67 |
| Sleep duration (PSG) | 476 (72.2) | 468.0 (153.8) | 380.4 (187.8) | 0.35 |
| Sleep efficiency (ACT) | 73.3 (5.4) | 74.8 (7.6) | 75.1 (5.0) | 0.09 |
| Sleep efficiency (PSG) | 86.4 (8.4) | 80.6 (22.8) | 72.2 (25.4) | 0.23 |
| WASO (ACT) | 79.8 (27.0) | 83.3 (26.1) | 88.9 (27.0) | 0.21 |
| WASO (PSG) | 44.4 (54.0) | 32.9 (58.0) | 18.6 (20.0) | 0.89 |
Actigraphy parameters were measured based on 2 weeks at 0 mg and 3 weeks at 1 and 3 mg excluding PSG nights; PSG parameters were measured on the night of the serial blood draws
Related samples Wilcoxon signed rank test
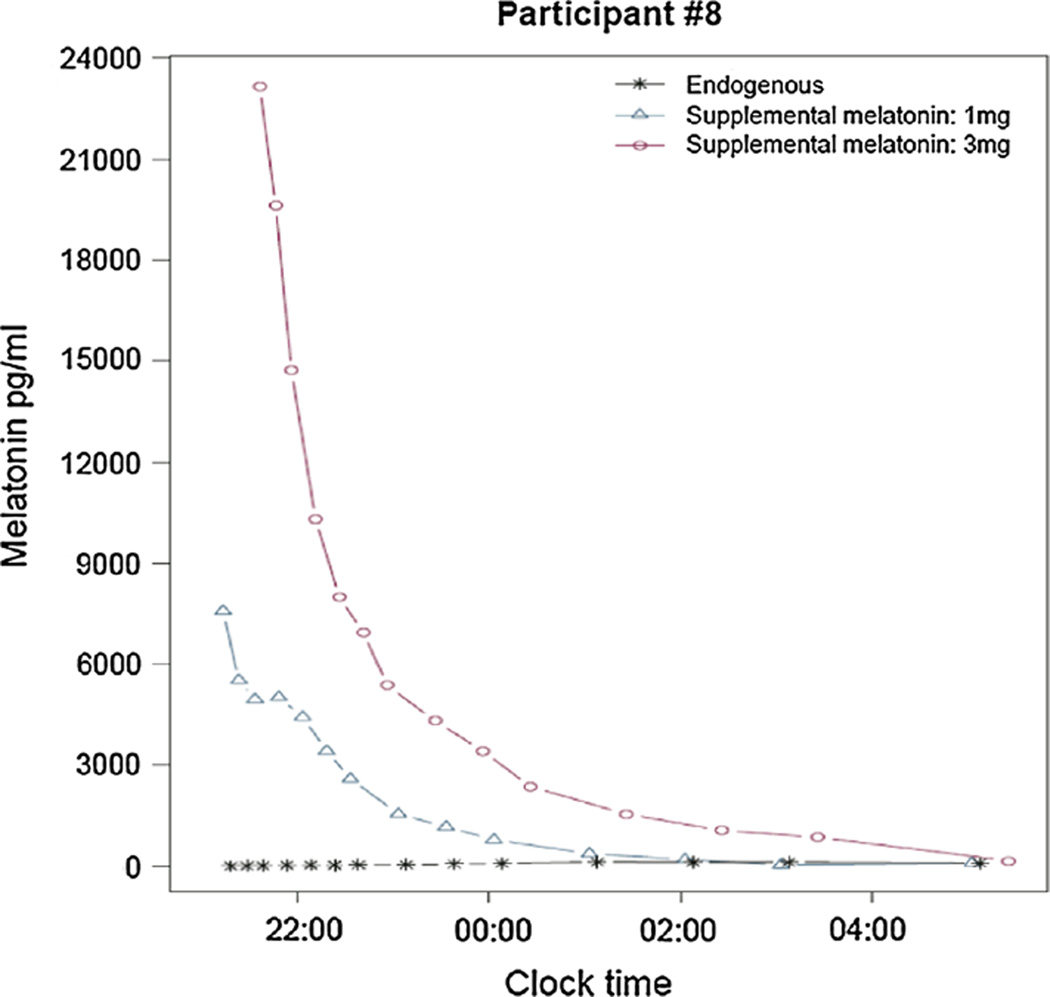
Night wakings data obtained from the CSHQ are presented in Table 4. Single night wakings were no longer considered a problem during treatment with supplemental melatonin (p = 0.008) although multiple night wakings were still considered a problem (p = 0.125). During treatment with supplemental melatonin, night wakings did not increase toward morning as might be expected after melatonin levels returned to endogenous levels. As an example, Participant #8 was reported by her parent to awaken around 2 a.m. at baseline. Figure 3 shows that by 2 a.m., the 1 mg PK curve had fallen to endogenous levels. However, her parents reported an improvement in night wakings on the 1 mg dose. This improvement was sustained on the 3 mg dose.
Table 4.
Night wakings in relation to melatonin treatment
| Study ID | Single wakings |
Problem?* | Multiple wakings |
Problem?** | Additional notes from sleep histories and diaries | |
|---|---|---|---|---|---|---|
| 1 | Baseline | U | Yes | R | No | Awakened most nights screaming |
| Treatment | S | No | R | No | Rare wakings, usually after 3 a.m., with only some wakings involving screaming (1 mg) | |
| 2 | Baseline | U | Yes | U | Yes | Frequent night wakings |
| Treatment | S | No | R | No | Awakened occasionally (12:45–1:20 a.m.) but only once during the night (1 mg) | |
| 3 | Baseline | S | Yes | S | Yes | Difficulty returning to sleep after night wakings |
| Treatment | R | No | R | No | Easily returns to sleep after night wakings (on 1 mg and sustained on 3 mg) | |
| 4 | Baseline | S | Yes | R | No | Single night wakings |
| Treatment | R | No | R | No | Night wakings improved on 1 mg and were sustained on 3 mg | |
| 5 | Baseline | R | No | R | No | Rare night wakings, not considered a problem |
| Treatment | R | No | R | No | Rare night wakings, not considered a problem | |
| 6 | Baseline | U | Yes | U | Yes | Night wakings 3 or more times most nights, throughout night |
| Treatment | U | No | S | Yes | Night wakings 1–2 times most nights, throughout night (on 3 mg) | |
| 7 | Baseline | S | Yes | S | Yes | Waking after several hours “happy and ready to go” |
| Treatment | S | No | R | No | Improved night wakings | |
| 8 | Baseline | u | Yes | S | Yes | Night wakings occurring around 2 a.m.; chattering in room |
| Treatment | S | No | R | No | Night wakings improved on 1 mg and sustained on 3 mg | |
| 9 | Baseline | S | Yes | R | No | Awakens at 1:30–2 a.m. happy and making noises |
| Treatment | S | No | R | No | Improved night wakings |
Classified as R rarely (0–1 times a week), S sometimes (2–4 times a week) or U usually (5–7) times a week and problem/no problem based on the CSHQ (Owens et al. 2000). Sleep histories and diaries were also referenced
p = 0.008;
p = 0.125 Related-samples McNemar test comparing whether night wakings were a problem before and after treatment
Fig. 3.
Comparison of melatonin profiles at 0, 1, and 3 mg. Endogenous and supplemental melatonin curves are superimposed for participant #8. Note that by 2 a.m., the melatonin profile after administration of 1 mg supplemental melatonin has returned to endogenous values. By 5 a.m., the melatonin profile after administration of 3 mg supplemental melatonin has returned to endogenous values
Discussion
This work describes plasma melatonin levels in children with ASD and also describes the relationship of these blood levels to sleep parameters. To our knowledge, this is the first study to report on both overnight endogenous and PK melatonin profiles in relation to sleep parameters in prepubertal, medication-free children with well-characterized ASD. This report extends earlier work showing the effectiveness of melatonin on sleep latency (Malow et al. 2012) and presents evidence for melatonin’s role in night wakings. Our study was unique in that we were able to obtain serial overnight blood samples with simultaneous PSGs in children with ASD. Further, through the use of continuous in-home wrist actigraphy, and parent-completed sleep measures, we were able to fully characterize the change in nightly sleep metrics with administration of exogenous melatonin.
Endogenous Melatonin Profiles, Including DLMO, and Relationship to Sleep Parameters
A melatonin profile, with a quantifiable DLMO occurring prior to habitual sleep onset (by home actigraphy), was obtained in the majority of the children. The DLMOs, peak melatonin concentration and clock time at peak level exhibited large variability among subjects. Variability in endogenous melatonin has been reported in children (Ardura et al. 2003; Novakova et al. 2011; Salti et al. 2000) as well as in adults (Burgess and Fogg 2008; Fourtillan et al. 2000; Kennaway 2000). The variability in our population may be associated with multiple factors, either related to the child’s environment (e.g. variability in bedtimes in the home environment) or intrinsic to the child. For instance, the heavier children in our study had lower endogenous melatonin concentrations. This extends findings of an association between weight and amplitude of melatonin secretion previously reported in adults (Burgess and Fogg 2008) to a younger aged cohort. Variable rates of hepatic metabolism of melatonin to 6-sulfatoxymelatonin contribute to high inter-individual differences in the bioavailability (F) of orally dosed melatonin; the same metabolic differences may contribute to the high variability observed in endogenous melatonin levels.
In our study, the amplitude and timing of endogenous melatonin was comparable to that described in the literature for typically developing children (Salti et al. 2000). In contrast to the one study that measured overnight endogenous melatonin levels in children with ASD (Kulman et al. 2000), our study did not document endogenous levels of melatonin to be low or delayed in the majority of our sample, all of whom were melatonin responders. This study design was different than ours in that their subjects were generally older (5–10 years), there was less frequent sampling (samples collected every 4 h), and a nonspecific radioimmunoassay was used in the quantitation of venous melatonin. Similar to our study, children were free of psychotropic medication. Other studies that documented low melatonin levels either measured daytime levels in platelets (Melke et al. 2008) or overnight levels of the melatonin metabolite in urine (Tordjman et al. 2005). These methodological differences may explain the discrepancies in our findings.
Sleep onset times by PSG were closer to DLMOs than the sleep onset times measured by actigraphy. This may reflect differences in light exposure in the home and sleep laboratory settings, with dim light strictly enforced in the laboratory setting. In addition, the night of the blood sampling on the PSG followed a habituation night followed by an active day (parents were encouraged to take their children out of the clinical research center and engage them in activities), so that children may have been relatively sleep deprived and more likely to fall asleep more quickly on the PSG night. Our data support the complementary use of PSG and actigraphy in treatment studies in the ASD population. While PSG is needed to stage sleep and evaluate for sleep apnea, seizures, and other sleep disorders, actigraphy has major advantages in that it can be performed over multiple weeks in the home setting and is more easily tolerated by children with ASD. In our trial, actigraphy showed improvement in sleep latency during treatment with supplemental melatonin.
Pharmacokinetic Parameters for Supplemental Melatonin, and Relationship to Sleep Parameters
Our finding of relatively normal melatonin profiles in our participants is consistent with some children requiring more than 1 mg to achieve a satisfactory response (falling asleep within 30 min on five or more nights). The super-therapeutic levels of Cmax documented at the 1 mg dose, coupled with this finding of normal melatonin profiles, suggest that supplemental melatonin is not replacing a deficiency state but has other mechanisms of action. These include hypnotic effects, circadian phase-shifting effects, and antianxiolytic effects (Pandi-Perumal et al. 2006).
Nine children completed an overnight PKs study for at least one dose level of supplemental melatonin, given orally 30 min before bedtime. To our knowledge, this is the first plasma PK study of orally dosed melatonin reported in children (Table S2). The PK parameters we calculated from plasma concentration versus time curves are consistent with published values from adult populations and with IV dosed melatonin in healthy children (Table S2). Complete PK profiles were obtained from eight children at the 1 mg dose (Table 2). In the four children who completed the melatonin PKs study at both dose levels (1 and 3 mg), there was no evidence of saturation kinetics. We saw similar dose linearity in the preliminary adult study. The bioavailability of orally dosed melatonin is highly variable between subjects; literature values for F ranging from 0.01 to 0.3 have been reported in adult studies (Table S1).
The inter-subject variability in our PK study was high in children and adults, presumably due to differences in rates of first pass hepatic metabolism of melatonin (Aldhous et al. 1985; DeMuro et al. 2000; Di et al. 1997; Fourtillan et al. 2000; Waldhauser et al. 1984). In an elegant PK study employing stable isotope-labeled melatonin and GC–MS detection, Fourtillan et al. (2000) reported bioavailability values (the fraction of oral dose that reaches systemic circulation) ranging from 0.011 to 0.316 in a group of twelve healthy adult subjects. In addition to hepatic metabolism there are other variables inherent to the PK of orally dosed drugs, including intestinal absorption rates, body mass index, diet and nutritional state of subjects, as well as lipophilicity and formulation (e.g. immediate release vs. extended release) of the drug.
We saw improvement in parent-reported night wakings with administration of supplemental melatonin. This occurred despite melatonin levels falling back to baseline at the 1 and 3 mg doses after several hours. Parents did not report that their children awakened several hours after taking melatonin, as might be expected based on the melatonin PK profiles. Our findings are in contrast to prior work reporting improved sleep latency, but not night wakings with melatonin treatment (Rossignol and Frye 2011). One hypothesis for the improvement in parent-reported night wakings may be that supplemental melatonin, in combination with the behavioral interventions we provided, improved children’s ability to fall asleep on their own, and thereby return to sleep during night wakings without alerting their parents. This hypothesis would also explain the discrepancy noted between parent report and objective measures of sleep continuity by actigraphy or PSG (which did not show treatment improvements, although our low sample size may also have been a factor). Actigraphy-measured WASO may also be measuring aspects of sleep that differ from discrete night wakings, such as overall movement or restlessness of sleep.
N-acetylserotonin (NAS) is a precursor of melatonin synthesis. Melke et al. (2008) hypothesized that NAS levels in children with ASD would be elevated in relation to low endogenous melatonin levels, due to abnormalities in ASMT, the enzyme which converts NAS to melatonin in the pineal gland. These investigators found lower levels of ASMT activity in children with ASD as well as genetic variation in the promoter of ASMT. Although other studies have failed to replicate the direct associations of the common promoter variants in ASMT with ASD risk (Toma et al. 2007; Wang et al. 2013), genetic variation elsewhere in ASMT has been observed to be more frequent in ASD compared to controls by another group (Cai et al. 2008), and several rare mutations have been identified in individuals with ASD (Jonsson et al. 2010; Wang et al. 2013). We did not find NAS levels to be inversely related to endogenous melatonin. However, our findings in peripheral blood may not reflect the relationship of NAS to melatonin in the pineal gland.
Our study has several strengths and limitations. We were able to obtain serial blood samples on three separate nights, as well as PSGs, in children with ASD free of psychotropic medications, a population with a high prevalence of anxiety and tactile sensitivities. We achieved this with the assistance of highly skilled nursing staff, although it is likely that our sample represents children whose parents felt their children could tolerate the study procedures. Additionally we were able to obtain multiple weeks of in-home sleep measurements, which along with nightly sleep diaries, allowed us to characterize the sleep of this population, and response to treatment, in a naturalistic setting. Further strengths of our sample include children were well characterized in terms of autism diagnosis, who had been screened for medical comorbidities, and who received parent sleep education. This study was limited by a small sample size, lack of a control group, and variability in the specific start time of the serial blood sampling. These limitations are inherent to our population. We were concerned that requiring parents to have their children participate in overnight studies involving IV catheterization and repeated blood sampling would bias our enrollment in the larger melatonin study. While we recognize that having a control group of children without ASD and sleep disturbance would have strengthened our study, we were concerned about the limited benefit of the study to children of typical development, as well as giving melatonin to children without sleep disturbance. Finally, it was challenging to control the times of blood sampling, which were affected by several factors, including the child’s habitual bedtime and how well they tolerated the IV catheter placement.
In conclusion, our findings document that in children with ASD and insomnia responsive to treatment with supplemental melatonin, evidence exists for normal endogenous melatonin profiles. Furthermore, despite a relatively short duration of action of supplemental melatonin, night wakings improved in most children with treatment. This raises the possibility that supplemental melatonin may be influencing sleep onset delay and night wakings by mechanisms other than simply replacing melatonin. The mechanism of action whereby supplemental melatonin affects sleep will require further study. Given the challenges associated with blood sampling in this population, future studies examining melatonin profiles using home saliva sampling may be useful. Our results further support the need for controlled trials of melatonin, coupled with mechanistic studies, to improve insomnia in this population.
Supplementary Material
Acknowledgments
This work was supported by NICHD (RO1 HD59253), Vanderbilt General Clinical Research Center (M01 RR-00095 from the National Center for Research Resources, National Institutes of Health), and by the Vanderbilt University Kennedy Center (NICHD HD15052). Natrol® (Chatsworth, CA, USA), provided study drug but no other support. We acknowledge Ms. Kyla Surdyka and Ms. Meg Touvelle for their assistance with data entry and Dr. Susan McGrew for her assistance with medical evaluations. We are appreciative to the families who participated in this project.
Footnotes
Electronic supplementary material The online version of this article (doi: 10.1007/s10803-014-2123-9) contains supplementary material, which is available to authorized users.
Conflict of interest The authors declare that they have no conflict of interest.
Contributor Information
Suzanne E. Goldman, Departments of Neurology and Pediatrics Burry Chair in, Cognitive Childhood Development, Sleep Disorders Division, Vanderbilt University Medical Center, 1161 21st Avenue South, Room A-0116, Nashville, TN 37232-2551, USA
Karen W. Adkins, Departments of Neurology and Pediatrics Burry Chair in, Cognitive Childhood Development, Sleep Disorders Division, Vanderbilt University Medical Center, 1161 21st Avenue South, Room A-0116, Nashville, TN 37232-2551, USA
M. Wade Calcutt, Department of Biochemistry, Vanderbilt University Medical, Center, Nashville, TN, USA; Mass Spectrometry Research Center, Vanderbilt University, Medical Center, Nashville, TN, USA.
Melissa D. Carter, Department of Biochemistry, Vanderbilt University Medical, Center, Nashville, TN, USA Mass Spectrometry Research Center, Vanderbilt University, Medical Center, Nashville, TN, USA.
Robert L. Goodpaster, Departments of Neurology and Pediatrics Burry Chair in, Cognitive Childhood Development, Sleep Disorders Division, Vanderbilt University Medical Center, 1161 21st Avenue South, Room A-0116, Nashville, TN 37232-2551, USA
Lily Wang, Department of Bio statistics, Vanderbilt University Medical, Center, Nashville, TN, USA.
Yaping Shi, Department of Bio statistics, Vanderbilt University Medical, Center, Nashville, TN, USA.
Helen J. Burgess, Department of Behavioral Sciences, Rush University Medical, Center, Chicago, IL, USA
David L. Hachey, Mass Spectrometry Research Center, Vanderbilt University, Medical Center, Nashville, TN, USA Department of Pharmacology, Vanderbilt University Medical, Center, Nashville, TN, USA.
Beth A. Malow, Email: beth.malow@vanderbilt.edu, Departments of Neurology and Pediatrics Burry Chair in, Cognitive Childhood Development, Sleep Disorders Division, Vanderbilt University Medical Center, 1161 21st Avenue South, Room A-0116, Nashville, TN 37232-2551, USA.
References
- Aldhous M, Franey C, Wright J, Arendt J. Plasma concentrations of melatonin in man following oral absorption of different preparations. British Journal of Clinical Pharmacology. 1985;19:517–521. doi: 10.1111/j.1365-2125.1985.tb02679.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- American Psychiatric Association. Diagnostic and statistical manual of mental disorders. 4th ed. Washington, DC: American Psychiatric Association; 2000. [Google Scholar]
- Andersen IM, Kaczmarska J, McGrew SG, Malow BA. Melatonin for insomnia in children with autism spectrum disorders. Journal of Child Neurology. 2008;23:482–485. doi: 10.1177/0883073807309783. [DOI] [PubMed] [Google Scholar]
- Ardura J, Gutierrez R, Andres J, Agapito T. Emergence and evolution of the circadian rhythm of melatonin in children. Hormone Research. 2003;59:66–72. doi: 10.1159/000068571. [DOI] [PubMed] [Google Scholar]
- Benloucif S, Burgess HJ, Klerman EB, Lewy AJ, Middleton B, Murphy PJ, et al. Measuring melatonin in humans. Journal of Clinical Sleep Medicine. 2008;4:66–69. [PMC free article] [PubMed] [Google Scholar]
- Burgess HJ, Fogg LF. Individual differences in the amount and timing of salivary melatonin secretion. PLoS ONE. 2008;3:e3055. doi: 10.1371/journal.pone.0003055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cai G, Edelmann L, Goldsmith JE, Cohen N, Nakamine A, Reichert JG, et al. Multiplex ligation-dependent probe amplification for genetic screening in autism spectrum disorders: Efficient identification of known microduplications and identification of a novel microduplication in ASMT. BMC Medical Genomics. 2008;1:50. doi: 10.1186/1755-8794-1-50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carter MD, Calcutt MW, Malow BA, Rose KL, Hachey DL. Quantitation of melatonin and n-acetylserotonin in human plasma by nanoflow LC-MS/MS and electrospray LC-MS/MS. Journal of Mass Spectrometry. 2012;47:277–285. doi: 10.1002/jms.2051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention. Prevalence of autism spectrum disorders—autism and developmental disabilities Monitoring Network, 14 sites, United States, 2008. MMWR Surveillance Summaries. 2012;61:1–19. [PubMed] [Google Scholar]
- Couturier JL, Speechley KN, Steele M, Norman R, Stringer B, Nicolson R. Parental perception of sleep problems in children of normal intelligence with pervasive developmental disorders: Prevalence, severity, and pattern. Journal of the American Academy of Child and Adolescent Psychiatry. 2005;44:815–822. doi: 10.1097/01.chi.0000166377.22651.87. [DOI] [PubMed] [Google Scholar]
- DeMuro RL, Nafziger AN, Blask DE, Menhinick AM, Bertino JS., Jr The absolute bioavailability of oral melatonin. Journal of Clinical Pharmacology. 2000;40:781–784. doi: 10.1177/00912700022009422. [DOI] [PubMed] [Google Scholar]
- Di WL, Kadva A, Johnston A, Silman R. Variable bioavailability of oral melatonin. New England Journal of Medicine. 1997;336:1028–1029. doi: 10.1056/NEJM199704033361418. [DOI] [PubMed] [Google Scholar]
- Fourtillan JB, Brisson AM, Gobin P, Ingrand I, Decourt JP, Girault J. Bioavailability of melatonin in humans after day-time administration of D(7) melatonin. Biopharmaceutics and Drug Disposition. 2000;21:15–22. doi: 10.1002/1099-081x(200001)21:1<15::aid-bdd215>3.0.co;2-h. [DOI] [PubMed] [Google Scholar]
- Gabriels RL, Cuccaro ML, Hill DE, Ivers BJ, Goldson E. Repetitive behaviors in autism: Relationships with associated clinical features. Research in Developmental Disabilities. 2005;26:169–181. doi: 10.1016/j.ridd.2004.05.003. [DOI] [PubMed] [Google Scholar]
- Glickman G. Orcadian rhythms and sleep in children with autism. Neuroscience and Biobehavioral Reviews. 2010;34:755–768. doi: 10.1016/j.neubiorev.2009.11.017. [DOI] [PubMed] [Google Scholar]
- Goldman SE, Richdale AL, Clemons T, Malow BA. Parental sleep concerns in autism spectrum disorders: Variations from childhood to adolescence. Journal of Autism and Developmental Disorders. 2012;42:531–538. doi: 10.1007/s10803-011-1270-5. [DOI] [PubMed] [Google Scholar]
- Goldman SE, Surdyka K, Cuevas R, Adkins K, Wang L, Malow BA. Defining the sleep phenotype in children with autism. Developmental Neuropsychology. 2009;34:560–573. doi: 10.1080/87565640903133509. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Iber C, Ancoli-Israel S, Jr, Chesson AL, Quan SF. The AASM manual for the scoring of sleep and associated events: Rules, terminology and technical specifications. Westchester: American Academy of Sleep Medicine; 2007. [Google Scholar]
- Jonsson L, Ljunggren E, Bremer A, Pedersen C, Landen M, Thuresson K, et al. Mutation screening of melatonin-related genes in patients with autism spectrum disorders. BMC Medical Genomics. 2010;8(3):10. doi: 10.1186/1755-8794-3-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kennaway DJ. Melatonin and development: Physiology and pharmacology. Seminars in Perinatology. 2000;24:258–266. doi: 10.1053/sper.2000.8594. [DOI] [PubMed] [Google Scholar]
- Krakowiak P, Goodlin-Jones B, Hertz-Picciotto I, Croen LA, Hansen RL. Sleep problems in children with autism spectrum disorders, developmental delays, and typical development: A population-based study. Journal of Sleep Research. 2008;17:197–206. doi: 10.1111/j.1365-2869.2008.00650.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kulman G, Lissoni P, Rovelli F, Roselli MG, Brivio F, Sequeri P. Evidence of pineal endocrine hypofunction in autistic children. Neuroendocrinology Letters. 2000;21:31–34. [PubMed] [Google Scholar]
- Leu RM, Beyderman L, Botzolakis EJ, Surdyka K, Wang L, Malow BA. Relation of melatonin to sleep architecture in children with autism. Journal of Autism and Developmental Disorders. 2011;41:427–433. doi: 10.1007/s10803-010-1072-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lewy AJ. The dim light melatonin onset, melatonin assays and biological rhythm research in humans. Biological Signals and Receptors. 1999;8:79–83. doi: 10.1159/000014573. [DOI] [PubMed] [Google Scholar]
- Lord C, Risi S, Lambrecht L, Cook EH, Jr, Leventhal BL, DiLavore PC, et al. The autism diagnostic observation schedule-generic: A standard measure of social and communication deficits associated with the spectrum of autism. Journal of Autism and Developmental Disorders. 2000;30:205–223. [PubMed] [Google Scholar]
- Malow B, Adkins KW, McGrew SG, Wang L, Goldman SE, Fawkes D, et al. Melatonin for sleep in children with autism: A controlled trial examining dose, tolerability, and outcomes. Journal of Autism and Developmental Disorders. 2012;42:1729–1737. doi: 10.1007/s10803-011-1418-3. (author reply 1738) [DOI] [PMC free article] [PubMed] [Google Scholar]
- Malow BA, Marzec ML, McGrew SG, Wang L, Henderson LM, Stone WL. Characterizing sleep in children with autism spectrum disorders: A multidimensional approach. Sleep. 2006;29:1563–1571. doi: 10.1093/sleep/29.12.1563. [DOI] [PubMed] [Google Scholar]
- Melke J, Goubran Botros H, Chaste P, Betancur C, Nygren G, Anckarsater H, et al. Abnormal melatonin synthesis in autism spectrum disorders. Molecular Psychiatry. 2008;13:90–98. doi: 10.1038/sj.mp.4002016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nir I, Meir D, Zilber N, Knobler H, Hadjez J, Lerner Y. Brief report: Orcadian melatonin, thyroid-stimulating hormone, prolactin, and Cortisol levels in serum of young adults with autism. Journal of Autism and Developmental Disorders. 1995;25:641–654. doi: 10.1007/BF02178193. [DOI] [PubMed] [Google Scholar]
- Novakova M, Paclt I, Ptacek R, Kuzelova H, Hajek I, Sumova A. Salivary melatonin rhythm as a marker of the circadian system in healthy children and those with attention-deficit/hyperactivity disorder. Chronobiology International. 2011;28:630–637. doi: 10.3109/07420528.2011.596983. [DOI] [PubMed] [Google Scholar]
- Owens JA, Spirito A, McGuinn M. The Children’s Sleep Habits Questionnaire (CSHQ): Psychometric properties of a survey instrument for school-aged children. Sleep. 2000;23:1043–1051. [PubMed] [Google Scholar]
- Pandi-Perumal SR, Srinivasan V, Maestroni GJ, Cardinali DP, Poeggeler B, Hardeland R. Melatonin: Nature’s most versatile biological signal? FEBS Journal. 2006;273:2813–2838. doi: 10.1111/j.1742-4658.2006.05322.x. [DOI] [PubMed] [Google Scholar]
- Rossignol DA, Frye RE. Melatonin in autism spectrum disorders: A systematic review and meta-analysis. Developmental Medicine and Child Neurology. 2011;53:783–792. doi: 10.1111/j.1469-8749.2011.03980.x. [DOI] [PubMed] [Google Scholar]
- Salti R, Galluzzi F, Bindi G, Perfetto F, Tarquini R, Halberg F, et al. Nocturnal melatonin patterns in children. Journal of Clinical Endocrinology and Metabolism. 2000;85:2137–2144. doi: 10.1210/jcem.85.6.6656. [DOI] [PubMed] [Google Scholar]
- Schreck KA, Mulick JA, Smith AF. Sleep problems as possible predictors of intensified symptoms of autism. Research in Developmental Disabilities. 2004;25:57–66. doi: 10.1016/j.ridd.2003.04.007. [DOI] [PubMed] [Google Scholar]
- Souders MC, Mason TB, Valladares O, Bucan M, Levy SE, Mandell DS, et al. Sleep behaviors and sleep quality in children with autism spectrum disorders. Sleep. 2009;32:1566–1578. doi: 10.1093/sleep/32.12.1566. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Toma C, Rossi M, Sousa I, Blasi F, Bacchelli E, Alen R, et al. Is ASMT a susceptibility gene for autism spectrum disorders? A replication study in European populations. Molecular Psychiatry. 2007;12:977–979. doi: 10.1038/sj.mp.4002069. [DOI] [PubMed] [Google Scholar]
- Tordjman S, Anderson GM, Pichard N, Charbuy H, Touitou Y. Nocturnal excretion of 6-sulphatoxymelatonin in children and adolescents with autistic disorder. Biological Psychiatry. 2005;57:134–138. doi: 10.1016/j.biopsych.2004.11.003. [DOI] [PubMed] [Google Scholar]
- Waldhauser F, Waldhauser M, Lieberman HR, Deng MH, Lynch HJ, Wurtman RJ. Bioavailability of oral melatonin in humans. Neuroendocrinology. 1984;39:307–313. doi: 10.1159/000123997. [DOI] [PubMed] [Google Scholar]
- Wang L, Li J, Ruan Y, Lu T, Liu C, Jia M, et al. Sequencing ASMT identifies rare mutations in Chinese Han patients with autism. PLoS ONE. 2013;8:e53727. doi: 10.1371/journal.pone.0053727. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.