Summary
Objectives
This study aimed to assess the research investments made to UK institutions for all infectious disease research and identify the direction of spend by institution.
Design
Systematic analysis. Databases and websites were systematically searched for information on relevant studies funded for the period 1997–2010.
Setting
UK institutions carrying out infectious disease research.
Participants
None.
Main outcome measures
Twenty academic institutions receiving greatest sum investments across infection are included here, also NHS sites, Sanger Institute, Health Protection Agency and the Medical Research Council. We measured total funding, median award size, disease areas and position of research along the R&D value chain.
Results
Included institutions accounted for £2.1 billion across 5003 studies. Imperial College and University of Oxford received the most investment. Imperial College led the most studies. The Liverpool and London Schools of Tropical Medicine had highest median award size, whereas the NHS sites combined had many smaller studies. Sum NHS funding appears to be declining over time, whilst university income is relatively stable. Several institutions concentrate almost exclusively on pre-clinical research. In some areas, there is clearly a leading institution, e.g. Aberdeen and mycology research or UCL and antimicrobial resistance.
Conclusion
UK institutions carry out research across a wide range of infectious disease areas. This analysis can identify centres of excellence and help inform future resource allocation for research priorities. Institutions can use this analysis for establishing expertise within their groups, identifying external collaborators and informing local research strategy.
Keywords: institutions, universities, NHS, infectious disease, funding, investments, UK
Introduction
Infectious diseases cause a high burden of potentially avoidable morbidity and mortality, and place substantial strain on the limited health budgets, health systems and economies of countries worldwide. Investment in research is vital to aid implementation of programmes and policy that will reduce these burdens, and to develop new tools such as vaccines, diagnostics and drugs. Given the limited funding available, allocating investments appropriately and strategically is of paramount importance.
In recent years, the UK has been considered to be the second leading investor in global health and research and development (R&D) for neglected diseases.1,2 Thus, the coverage and impact of the UK research portfolio is of great consequence, both in terms of infections within the UK, but also its global health outputs. Research takes place in university settings and clinical environments, and is also carried out by governmental or independent institutions such as Public Health England (formerly the Health Protection Agency, HPA) and the Medical Research Council.
The Research Investments in Global Health study (ResIn, www.researchinvestments.org) has tracked the investments made to UK institutions in infectious disease research over a 14-year time period from 1997 to 2010. The analysis has demonstrated that around one-third of the investments had a clear focus on global health, and that the UK appears to have strengths in pre-clinical research.3 The project has since focused on describing topic-specific areas of investment such as highlighting the investments with colonial ties,4 and assessing the investments by gender of the principal investigator.5
Here, we analyse the type of investments made by the UK institutions, and describe the funding awarded to these institutions in terms of award size and number across infectious disease, clinical specialty, type of science along the R&D pipeline, and area of microbiology.
Methods
The analysis presented here focused on research investments by public and philanthropic funding organisations awarded to the UK institutions between 1997 and 2010. The methods are based on a preliminary study mapping funding for infectious disease research and are described in further detail elsewhere.3 Further information on methods and lists of categories is openly available on the study website (http://www.researchinvestments.org).
The overarching dataset was developed following a detailed and systematic search of all the studies for infectious disease research from the major sources of public and charitable funding for infectious disease research studies, including the Wellcome Trust, Medical Research Council and other research councils, UK government departments, European Commission, the Bill and Melinda Gates Foundation, and other research charities. No private sector (commercial) funding was included in this analysis as publicly available data were limited and considered to be under-representative.
We developed the dataset by (a) downloading all data from the funder website and manually filtering the infectious disease studies; or (b) searching open access databases on the funder website for infection-related keyword terms; or (c) contacting the funder directly and requesting details of their infection studies. Funders were identified through authors’ knowledge of the R&D landscape, contributors to the National Research Register and systematic searches of the Internet. Author MGH performed the majority of data extraction, with support from author JRF. Each study was assigned to as many primary disease categories as appropriate. Within each category, topic-specific sub-sections (including specific pathogen or disease) were documented. Studies were also allocated to one of four R&D categories: pre-clinical; phase 1, 2 or 3; product development; and implementation and operational research (including surveillance, epidemiology and statistical and modelling projects; see http://researchinvestments.org/data/ for definitions and examples).
Universities receiving funding were categorised individually, and the 20 academic institutions receiving greatest sum investments across infection are included here. NHS hospitals and institutions receiving funding were grouped into an ‘NHS’ category. Other institutions classified separately and also analysed here were the Sanger Institute, Health Protection Agency (now Public Health England but referred to as Health Protection Agency in this paper) and the Medical Research Council (UK sites only, units in Gambia and Uganda were excluded as they were considered to be overseas institutions for the purposes of this study). The University of London colleges were considered separately: for example, University College London (UCL), King’s College London (KCL), and London School of Hygiene and Tropical Medicine (LSHTM); the Liverpool School of Tropical Medicine (LSTM) was considered separately to the University of Liverpool.
Major funding organisations were categorised in their own right, and smaller funding organisations were grouped into categories, such as in-house university funding, research charities and government departments. A total of 26 funder categories were used. Studies were excluded if: (i) they were not immediately relevant to infection; (ii) they were veterinary infectious disease research studies; (iii) they concerned the use of viral vectors to investigate non-communicable diseases; (iv) they were grants for symposia or meetings or (v) they included UK researchers, but with the funding awarded to and administered through a non-UK institution. Unfunded studies were excluded. Grants awarded in a currency other than pounds sterling were converted to UK pounds using the mean exchange rate in the year of the award. All awards were adjusted for inflation and reported in 2010 UK pounds. Analysis was carried out in Microsoft Excel and Access (versions 2000 and 2007) and Stata (versions 11, 12 and 13).
Results
We identified 6165 studies funded within the 14-year study period and covering all infectious disease research, representing an overall investment of £2.6 billion. In terms of total funding, the top 20 universities, plus the Sanger Institute, Health Protection Agency, Medical Research Council and NHS accounted for £2.1 billion across 5003 studies (81.9% of the total funding and 82.5% of the studies). The remainder of the projects not analysed in detail here were awarded to other academic institutions such as the universities of York, Cardiff and Sheffield, or other institutions types such as the National Blood Service, National Institute for Medical Research (NIMR) or Health Protection Scotland. There were also 34 studies, representing 0.2% (£6.4 million) of total funding, where no institution was specified.
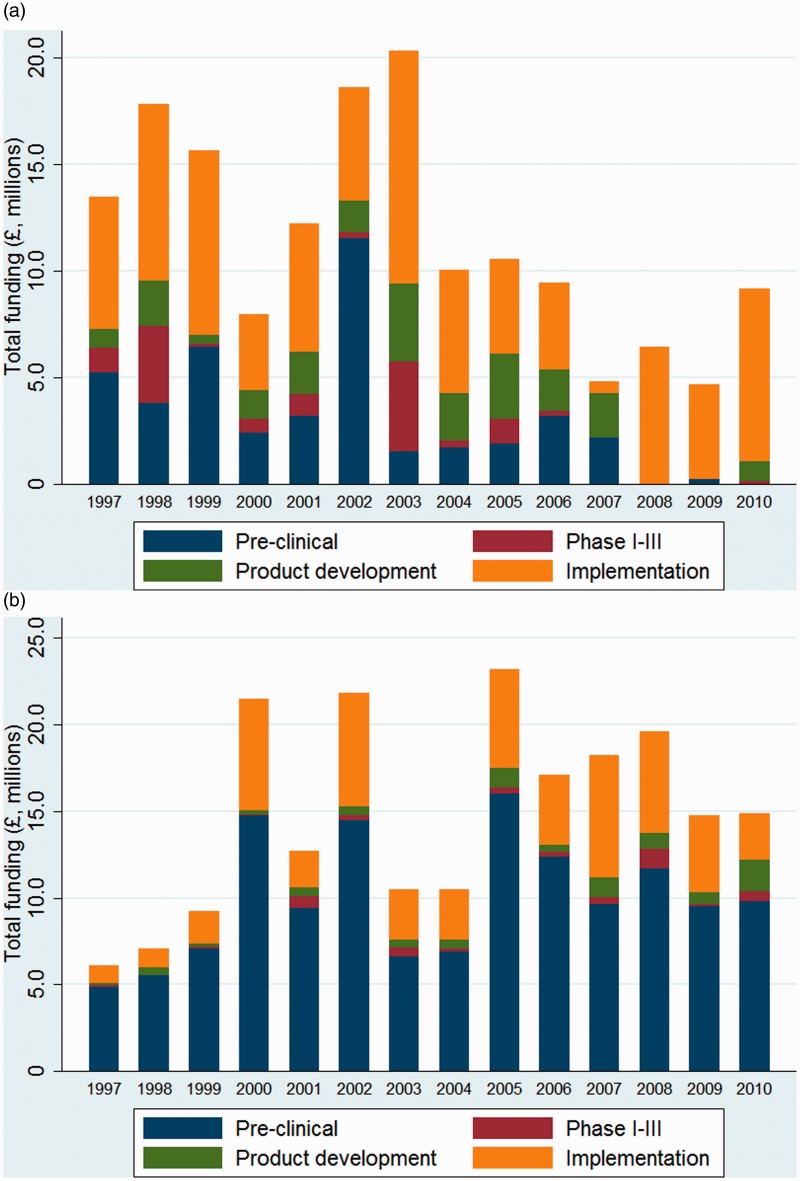
Imperial College and University of Oxford received the most investment, with Imperial College awarded the greatest number of studies to a single institution (Table 1). Other universities receiving particularly high levels of investment include LSHTM, UCL and Glasgow. The LSTM also received high levels of investment but the mean award size of £1.5 m (SD £4619005) was by far the greatest of any institution and thus the total number of studies led by LSTM were fewer than its peers. NHS institutions received the fourth highest amount of investment, and led on the most studies; the median award size for NHS research was smaller than any of the other institutions analysed (Table 1). The temporal investment awarded to the NHS for infectious disease research appears to be declining (Figure 1a), whilst university income for infection research is relatively stable and perhaps increasing over time (Figure 1b).
Table 2.
Investments awarded to named institutions by type of science.
| Institution | Number of studies | Total funding |
Pre-clinical |
Phase I–III |
Product development |
Operational |
||||
|---|---|---|---|---|---|---|---|---|---|---|
| Study numbers | Funding | Study numbers | Funding | Study numbers | Funding | Study numbers | Funding | |||
| Universities | ||||||||||
| Imperial | 539 | £269,838,681 | 428 | £171,542,393 | 8 | £9,988,349 | 20 | £17,453,311 | 83 | £70,854,629 |
| Oxford | 490 | £269,150,329 | 355 | £178,194,506 | 19 | £20,001,995 | 19 | £11,145,453 | 97 | £59,808,373 |
| LSHTM | 295 | £200,581,524 | 117 | £43,484,945 | 3 | £2,885,995 | 13 | £6,747,608 | 162 | £147,462,976 |
| UCL | 345 | £152,678,065 | 180 | £91,150,085 | 11 | £3,731,323 | 22 | £10,625,519 | 132 | £47,171,137 |
| Glasgow | 246 | £121,565,270 | 211 | £109,720,457 | 2 | £537,961 | 9 | £3,036,100 | 24 | £8,270,750 |
| LSTM | 74 | £111,128,762 | 35 | £25,252,965 | 3 | £2,061,292 | 5 | £2,235,948 | 31 | £81,578,556 |
| Edinburgh | 244 | £106,995,076 | 206 | £90,074,610 | 3 | £1,737,597 | 7 | £856,878 | 28 | £14,325,990 |
| Cambridge | 259 | £85,393,508 | 243 | £80,542,124 | 0 | – | 4 | £1,904,226 | 12 | £2,947,156 |
| Birmingham | 180 | £67,395,742 | 163 | £64,548,638 | 4 | £889,286 | 5 | £1,602,578 | 8 | £355,240 |
| KCL | 73 | £50,954,787 | 59 | £49,263,859 | 1 | £87,543 | 2 | £215,912 | 11 | £1,387,471 |
| Liverpool | 177 | £46,595,962 | 113 | £24,312,528 | 2 | £717,651 | 2 | £1,637,881 | 60 | £19,927,900 |
| SGUL | 85 | £43,101,362 | 57 | £34,345,483 | 4 | £808,653 | 6 | £4,824,789 | 18 | £3,122,435 |
| Nottingham | 94 | £41,169,001 | 80 | £35,685,679 | 0 | – | 3 | £504,948 | 11 | £4,978,372 |
| Dundee | 77 | £35,636,801 | 54 | £33,634,696 | 0 | – | 4 | £325,474 | 19 | £1,676,630 |
| Manchester | 83 | £34,955,998 | 67 | £26,723,112 | 2 | £124,091 | 1 | £1,280,752 | 13 | £6,828,041 |
| QMUL | 70 | £31,724,564 | 45 | £16,582,238 | 0 | – | 6 | £759,114 | 19 | £14,383,211 |
| Bristol | 87 | £29,414,376 | 62 | £19,100,902 | 3 | £83,443 | 3 | £1,801,664 | 19 | £8,428,366 |
| Institute of Food Research | 56 | £27,370,465 | 52 | £26,971,820 | 0 | – | 0 | – | 4 | £398,644 |
| Aberdeen | 76 | £25,877,695 | 62 | £22,493,254 | 0 | – | 1 | £354,007 | 13 | £3,030,433 |
| Leicester | 60 | £25,775,965 | 54 | £18,696,028 | 1 | £1,036,952 | 3 | £5,880,128 | 2 | £162,856 |
| Other institutions | ||||||||||
| Sanger | 17 | £10,903,772 | 17 | £10,903,772 | 0 | – | 0 | – | 0 | – |
| Health Protection Agency | 95 | £35,073,098 | 39 | £15,815,456 | 2 | £2,330,291 | 3 | £812,556 | 51 | £16,114,795 |
| Medical Research Council | 89 | £144,638,719 | 29 | £18,289,447 | 22 | £80,931,298 | 11 | £10,193,582 | 27 | £35,224,392 |
| All NHS | 1192 | £161,254,059 | 441 | £43,529,363 | 43 | £12,931,700 | 129 | £22,071,579 | 579 | £82,721,415 |
Table 1.
Investments awarded to named institutions by sum, number of studies and mean and median award size.
| Institution | Number of studies | Percentage of total studies | Total funding | Percentage of total funding | Mean award, £(SD) | Median award, £(IQR) | Top funder, millions (%) |
|---|---|---|---|---|---|---|---|
| Universities | |||||||
| Imperial | 539 | 8.9% | £269,838,681 | 10.4% | 500628 (1435781) | 187606 (84573-381328) | Wellcome Trust, 112.3 (41.6) |
| Oxford | 490 | 8.1% | £269,150,329 | 10.4% | 549286 (1055327) | 191461 (84531-515075) | Wellcome Trust, 137.0 (50.7) |
| LSHTM | 295 | 4.9% | £200,581,524 | 7.7% | 679937 (2468993) | 215530 (74747-477897) | Bill and Melinda Gates Foundation, 69.6 (34.7) |
| UCL | 345 | 5.7% | £152,678,065 | 5.9% | 442545 (1157936) | 170038 (54019-355657) | Medical Research Council, 55.3 (36.2) |
| Glasgow | 246 | 4.1% | £121,565,270 | 4.7% | 494167 (978230) | 229575 (95110-434677) | Medical Research Council, 54.6 (44.9) |
| LSTM | 74 | 1.2% | £111,128,762 | 4.3% | 1501740 (4619005) | 284024 (100343-691362) | Bill and Melinda Gates Foundation, 65.7 (59.2) |
| Edinburgh | 244 | 4.0% | £106,995,076 | 4.1% | 438504 (688180) | 223431 (100026-460111) | Wellcome Trust, 40.6 (37.9) |
| Cambridge | 259 | 4.3% | £85,393,508 | 3.3% | 329705 (400597) | 200689 (111115-364834) | Wellcome Trust, 41.6 (48.7) |
| Birmingham | 180 | 3.0% | £67,395,742 | 2.6% | 374420 (472408) | 222353 (113560-417474) | Charity, 34.4 (51.0) |
| KCL | 73 | 1.2% | £50,954,787 | 2.0% | 698010 (1714738) | 189677 (98317-454802) | European Commission, 23.8 (46.8) |
| Liverpool | 177 | 2.9% | £46,595,962 | 1.8% | 263254 (468016) | 148383 (47251-332938) | Wellcome Trust, 28.2 (60.5) |
| SGUL | 85 | 1.4% | £43,101,362 | 1.7% | 507075 (1766104) | 178375 (91602-323528) | European Commission, 15.2 (35.2) |
| Nottingham | 94 | 1.5% | £41,169,001 | 1.6% | 437968 (645475) | 221452 (116325-463543) | Medical Research Council, 17.8 (43.3) |
| Dundee | 77 | 1.3% | £35,636,801 | 1.4% | 462815 (1239808) | 131918 (16881-227408) | Wellcome Trust, 20.7 (58.0) |
| Manchester | 83 | 1.4% | £34,955,998 | 1.3% | 421156 (661739) | 221736 (96555-379346) | Wellcome Trust, 11.9 (34.1) |
| QMUL | 70 | 1.2% | £31,724,564 | 1.2% | 453208 (803551) | 222162 (75228-448641) | Charity, 14.7 (46.4) |
| Bristol | 87 | 1.4% | £29,414,376 | 1.1% | 338096 (431246) | 217039 (126966-379060) | Wellcome Trust, 12.1 (41.1) |
| Institute of Food Research | 56 | 0.9% | £27,370,465 | 1.1% | 488758 (840838) | 154359 (50886-371885) | BBSRC, 25.8 (94.1) |
| Aberdeen | 76 | 1.3% | £25,877,695 | 1.0% | 340496 (435944) | 211764 (94611-377555) | BBSRC, 8.7 (33.8) |
| Leicester | 60 | 1.0% | £25,775,965 | 1.0% | 429599 (599044) | 272284 (132613-434953) | Wellcome, 8.5 (32.9) |
| Other institutions | |||||||
| Sanger | 17 | 0.3% | £10,903,772 | 0.4% | 641398 (508844) | 489536 (226970-944867) | Wellcome, 9.2 (84.8) |
| Health Protection Agency | 95 | 1.6% | £35,073,098 | 1.3% | 369190 (580383) | 190189 (80922-390620) | Department of Health, 16.6 (47.2) |
| Medical Research Council | 89 | 1.5% | £144,638,719 | 5.6% | 1625154 (5403942) | 553045 (133975-1550288) | Medical Research Council, 71.1 (49.1) |
| All NHS | 1192 | 19.7% | £161,254,059 | 6.2% | 135280 (399808) | 36661 (7405-115220) | Department of Health, 55.3 (34.3) |
Figure 1.
Investments for research awarded to the UK institutions over time and by type of science, showing research led by (a) NHS institutions and (b) universities.
In terms of the funding organisation (Table 1), LSHTM and LSTM both received the greatest investment from the Bill and Melinda Gates Foundation, who have made relatively few awards but have the highest mean and median award size of all the funders.3 The Wellcome Trust was the leading investor for 10 of the 24 institutions included here. The Department of Health has been the main funder of NHS-led research.
According to the type of science along the R&D pipeline (Table 2), many of the institutions focused heavily on pre-clinical science, with Glasgow, Cambridge, King’s College London (KCL), Birmingham, Dundee and the Institute of Food Research all receiving greater than 90% of their funding for basic science (Table 2). The entirety of the investments made to the Sanger Institute was funding for pre-clinical research. The London and Liverpool schools of tropical medicine and the NHS had a higher proportion of implementation and operational research in their portfolios than most institutions. The only institution with greater than 10% of their portfolio related to phase I–III clinical trials was the Medical Research Council (56.0% of funding, 24.7% of studies); most institutions received little or no funding for phase I–III clinical trials from public and philanthropic funders.
In the area of microbiology (Table 3), Imperial College received the greatest number of awards and the highest total funding for bacteriology studies, although Nottingham (67.9%) and Leicester (75.5%) universities received the greatest proportion of their total funding for bacteriology research. Imperial and UCL received the greatest investments for virology research, with UCL’s virology portfolio totalling 61.2% of their investment received. The Medical Research Council (84.7%) and KCL (76.9%) also had a clear focus on virology research. In terms of total investment, LSHTM and LSTM focused primarily on parasitology research, whilst Dundee (64.5%) also had a significant investment in this area. Aberdeen (64.8% of total funding) was the sole university to have a dominant focus on mycology research. The NHS focused on virology (47.1%) and bacteriology (30.7%) studies, with smaller amounts on mycology, parasitology and also prion research (not reported here).
Table 3.
Investments awarded to named institutions by area of microbiology.
| Institution | Number of studies | Total funding |
Bacteriology |
Virology |
Parasitology |
Mycology |
||||
|---|---|---|---|---|---|---|---|---|---|---|
| Study numbers | Funding | Study numbers | Funding | Study numbers | Funding | Study numbers | Funding | |||
| Universities | ||||||||||
| Imperial | 539 | £269,838,681 | 187 | £67,204,051 | 163 | £104,750,878 | 86 | £63,287,217 | 14 | £4,531,594 |
| Oxford | 490 | £269,150,329 | 134 | £51,127,725 | 133 | £72,449,091 | 196 | £91,882,714 | 6 | £554,182 |
| LSHTM | 295 | £200,581,524 | 80 | £35,184,629 | 101 | £44,445,476 | 111 | £116,485,189 | 0 | – |
| UCL | 345 | £152,678,065 | 80 | £22,034,834 | 180 | £93,377,095 | 13 | £4,946,432 | 1 | £268,281 |
| Glasgow | 246 | £121,565,270 | 36 | £7,271,257 | 104 | £59,093,715 | 97 | £51,802,643 | 2 | £215,101 |
| LSTM | 74 | £111,128,762 | 15 | £6,298,198 | 15 | £41,327,407 | 49 | £96,766,718 | 1 | £1,234,683 |
| Edinburgh | 244 | £106,995,076 | 48 | £10,216,035 | 67 | £18,821,712 | 91 | £47,309,875 | 4 | £928,114 |
| Cambridge | 259 | £85,393,508 | 55 | £24,822,977 | 101 | £37,067,560 | 36 | £14,256,328 | 0 | – |
| Birmingham | 180 | £67,395,742 | 56 | £17,491,915 | 113 | £47,980,322 | 0 | – | 1 | £404,882 |
| KCL | 73 | £50,954,787 | 12 | £2,356,336 | 38 | £39,200,644 | 8 | £1,588,650 | 5 | £3,592,317 |
| Liverpool | 177 | £46,595,962 | 42 | £10,495,113 | 61 | £13,069,491 | 75 | £22,935,414 | 0 | – |
| SGUL | 85 | £43,101,362 | 39 | £11,930,626 | 24 | £26,625,316 | 16 | £3,999,993 | 6 | £1,889,998 |
| Nottingham | 94 | £41,169,001 | 55 | £27,956,234 | 20 | £6,892,417 | 13 | £4,609,721 | 1 | £221,162 |
| Dundee | 77 | £35,636,801 | 22 | £2,503,709 | 13 | £6,661,426 | 26 | £22,982,162 | 5 | £2,704,113 |
| Manchester | 83 | £34,955,998 | 24 | £5,369,298 | 13 | £8,565,852 | 29 | £11,140,970 | 6 | £2,812,549 |
| QMUL | 70 | £31,724,564 | 33 | £10,734,514 | 14 | £15,278,273 | 3 | £1,056,117 | 0 | – |
| Bristol | 87 | £29,414,376 | 48 | £16,750,076 | 19 | £5,772,863 | 10 | £2,595,573 | 1 | £379,059 |
| Institute of Food Research | 56 | £27,370,465 | 54 | £27,366,739 | 0 | – | 0 | – | 0 | – |
| Aberdeen | 76 | £25,877,695 | 18 | £4,901,485 | 5 | £578,495 | 10 | £1,900,502 | 33 | £16,777,091 |
| Leicester | 60 | £25,775,965 | 49 | £19,469,292 | 4 | £2,114,790 | 2 | £955,554 | 0 | – |
| Other institutions | ||||||||||
| Sanger | 17 | £10,903,772 | 10 | £4,982,812 | 0 | – | 6 | £5,129,834 | 1 | £791,125 |
| Health Protection Agency | 95 | £35,073,098 | 45 | £11,998,736 | 27 | £6,693,295 | 2 | £587,599 | 0 | – |
| Medical Research Council | 89 | £144,638,719 | 4 | £1,283,801 | 68 | £122,522,567 | 6 | £3,958,172 | 0 | – |
| All NHS | 1192 | £161,254,059 | 404 | £49,499,942 | 481 | £75,913,812 | 5 | £447,869 | 55 | £3,106,758 |
In consideration of the analysis by ‘the big three’ diseases of HIV, TB and malaria (Table 4), UCL received greatest investments for HIV research, though the NHS carried out more studies. HIV was the focus of 20.1% of NHS funding. St Georges, University of London (SGUL) had a proportionately large HIV portfolio at their institution (56.1% of total funding), as did KCL (68.2%). There was proportionately less of a focus for tuberculosis research across all institutions, with only Imperial College, QMUL and Leicester receiving greater than 10% of their total funding for tuberculosis studies (QMUL the greatest proportion at 10.6%). The London and Liverpool schools of tropical medicine and Oxford carried out the most malaria-related research.
Table 4.
Investments awarded to named institutions by tuberculosis, HIV and malaria.
| Institution | Number of studies | Total funding |
HIV |
Tuberculosis |
Malaria |
|||
|---|---|---|---|---|---|---|---|---|
| Study numbers | Funding | Study numbers | Funding | Study numbers | Funding | |||
| Universities | ||||||||
| Imperial | 539 | £269,838,681 | 58 | £54,693,397 | 46 | £27,852,882 | 40 | £16,451,059 |
| Oxford | 490 | £269,150,329 | 61 | £37,919,448 | 26 | £18,629,860 | 149 | £68,387,189 |
| LSHTM | 295 | £200,581,524 | 86 | £40,231,700 | 49 | £20,727,491 | 63 | £89,523,014 |
| UCL | 345 | £152,678,065 | 89 | £57,627,575 | 24 | £11,208,188 | 4 | £2,039,379 |
| Glasgow | 246 | £121,565,270 | 7 | £5,097,820 | 1 | £156,847 | 15 | £19,425,400 |
| LSTM | 74 | £111,128,762 | 10 | £7,635,758 | 4 | £3,928,211 | 38 | £47,920,662 |
| Edinburgh | 244 | £106,995,076 | 20 | £6,763,308 | 3 | £633,038 | 43 | £16,992,519 |
| Cambridge | 259 | £85,393,508 | 12 | £6,253,539 | 7 | £2,700,714 | 9 | £2,476,708 |
| Birmingham | 180 | £67,395,742 | 2 | £115,736 | 18 | £6,551,225 | 1 | £177,758 |
| KCL | 73 | £50,954,787 | 26 | £34,735,521 | 2 | £560,781 | 3 | £671,042 |
| Liverpool | 177 | £46,595,962 | 29 | £5,344,190 | 11 | £2,007,228 | 52 | £10,949,348 |
| SGUL | 85 | £43,101,362 | 12 | £24,162,004 | 11 | £2,035,981 | 7 | £2,518,445 |
| Nottingham | 94 | £41,169,001 | 2 | £110,476 | 1 | £127,418 | 4 | £2,367,693 |
| Dundee | 77 | £35,636,801 | 2 | £346,340 | 2 | £480,613 | 1 | £1,584,413 |
| Manchester | 83 | £34,955,998 | 2 | £75,454 | 4 | £883,147 | 5 | £2,383,457 |
| QMUL | 70 | £31,724,564 | 1 | £285,091 | 6 | £3,357,363 | 0 | – |
| Bristol | 87 | £29,414,376 | 4 | £2,407,688 | 0 | – | 0 | – |
| Institute of Food Research | 56 | £27,370,465 | 0 | – | 2 | £242,765 | 0 | – |
| Aberdeen | 76 | £25,877,695 | 0 | – | 1 | £197,413 | 1 | £273,015 |
| Leicester | 60 | £25,775,965 | 0 | – | 12 | £2,698,015 | 1 | £500,000 |
| Other institutions | ||||||||
| Sanger | 17 | £10,903,772 | 0 | – | 1 | £226,970 | 3 | £3,397,382 |
| Health Protection Agency | 95 | £35,073,098 | 9 | £1,684,463 | 4 | £1,432,104 | 0 | – |
| Medical Research Council | 89 | £144,638,719 | 51 | £115,646,608 | 4 | £1,132,220 | 5 | £3,859,883 |
| All NHS | 1192 | £161,254,059 | 193 | £32,389,815 | 29 | £4,855,298 | 0 | – |
By cross-cutting theme (Table 5), the London (85.6%) and Liverpool (96.5%) Schools of Tropical Medicine had the greatest focus on global health. University of Liverpool, Dundee and the Medical Research Council also received greater than half of their total investments for research related to global health. Antimicrobial resistance has historically been a neglected area of research,6 and only UCL (11.9% of total funding across 24 studies) appears to have a portfolio of any size at all in this area; the NHS carried out 90 studies, but the total funding was only £6.6 million. The NHS also carried out 208 studies in the area of diagnostics, but the total funding was only £27.9 million; the other key institution in this area was QMUL (£13.9 million, 43.9% of total funding received). Oxford (£65.0 million, 24.2%) carried out the most research related to vaccinology, with SGUL (39.1% of total funding) also having a proportionately greater focus in this area. The Liverpool School of Tropical Medicine and the Medical Research Council carried out the most research into therapeutics.
Table 5.
Investments awarded to named institutions by selected cross-cutting themes.
| Institution | Number of studies | Total funding |
Global health |
Antimicrobial resistance |
Diagnostics |
Vaccinology |
Therapeutics |
|||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Study numbers | Funding | Study numbers | Funding | Study numbers | Funding | Study numbers | Funding | Study numbers | Funding | |||
| Universities | ||||||||||||
| Imperial | 539 | £269,838,681 | 117 | £106,105,928 | 18 | £3,023,898 | 21 | £5,291,472 | 24 | £27,433,268 | 29 | £34,897,673 |
| Oxford | 490 | £269,150,329 | 221 | £101,653,787 | 22 | £11,084,567 | 5 | £3,482,124 | 70 | £65,012,775 | 30 | £21,438,291 |
| LSHTM | 295 | £200,581,524 | 219 | £171,616,293 | 9 | £6,653,741 | 8 | £4,834,436 | 17 | £12,602,957 | 21 | £30,462,381 |
| UCL | 345 | £152,678,065 | 40 | £34,868,163 | 24 | £18,107,558 | 28 | £7,541,347 | 23 | £20,079,552 | 30 | £19,166,266 |
| Glasgow | 246 | £121,565,270 | 99 | £52,188,126 | 7 | £2,528,858 | 10 | £1,348,319 | 9 | £3,162,344 | 13 | £7,455,825 |
| LSTM | 74 | £111,128,762 | 61 | £107,245,162 | 6 | £1,524,841 | 1 | £492,391 | 5 | £1,284,910 | 16 | £51,157,346 |
| Edinburgh | 244 | £106,995,076 | 67 | £46,391,841 | 13 | £4,903,081 | 7 | £2,208,129 | 7 | £9,657,389 | 17 | £6,417,473 |
| Cambridge | 259 | £85,393,508 | 42 | £15,327,956 | 5 | £4,199,895 | 3 | £1,501,730 | 6 | £2,953,253 | 6 | £1,308,002 |
| Birmingham | 180 | £67,395,742 | 3 | £234,270 | 11 | £4,001,974 | 2 | £920,830 | 6 | £544,074 | 14 | £3,356,737 |
| KCL | 73 | £50,954,787 | 11 | £14,880,749 | 3 | £375,445 | 2 | £196,181 | 7 | £5,317,059 | 9 | £21,820,332 |
| Liverpool | 177 | £46,595,962 | 97 | £28,900,463 | 8 | £2,174,823 | 1 | £100,000 | 3 | £2,205,002 | 21 | £4,370,628 |
| SGUL | 85 | £43,101,362 | 19 | £4,844,079 | 7 | £889,471 | 6 | £4,497,127 | 6 | £16,831,083 | 14 | £17,708,908 |
| Nottingham | 94 | £41,169,001 | 14 | £4,662,018 | 4 | £501,563 | 3 | £940,890 | 3 | £445,810 | 11 | £7,916,189 |
| Dundee | 77 | £35,636,801 | 26 | £22,982,162 | 6 | £292,353 | 2 | £6,945 | 0 | £0 | 6 | £12,416,514 |
| Manchester | 83 | £34,955,998 | 31 | £11,216,424 | 4 | £994,307 | 5 | £3,306,533 | 4 | £1,012,670 | 8 | £3,142,894 |
| QMUL | 70 | £31,724,564 | 7 | £2,686,083 | 3 | £673,299 | 22 | £13,913,807 | 5 | £1,550,890 | 3 | £770,114 |
| Bristol | 87 | £29,414,376 | 14 | £3,531,986 | 6 | £867,332 | 4 | £2,315,730 | 8 | £1,084,746 | 6 | £1,353,942 |
| Institute of Food Research | 56 | £27,370,465 | 0 | – | 0 | – | 1 | £813 | 1 | £177,984 | 2 | £1,091,589 |
| Aberdeen | 76 | £25,877,695 | 10 | £1,900,502 | 7 | £1,457,249 | 3 | £357,723 | 0 | £0 | 4 | £299,573 |
| Leicester | 60 | £25,775,965 | 4 | £1,885,103 | 2 | £1,230,458 | 2 | £1,135,490 | 3 | £1,811,794 | 1 | £3,480,608 |
| Other institutions | ||||||||||||
| Sanger | 17 | £10,903,772 | 6 | £5,129,834 | 1 | £74,307 | 0 | – | 0 | £0 | 0 | £0 |
| Health Protection Agency | 95 | £35,073,098 | 3 | £658,608 | 8 | £1,495,256 | 13 | £1,235,662 | 15 | £9,701,862 | 5 | £663,071 |
| Medical Research Council | 89 | £144,638,719 | 18 | £68,804,202 | 4 | £2,267,503 | 0 | – | 6 | £2,423,560 | 28 | £81,517,047 |
| All NHS | 1192 | £161,254,059 | 13 | £4,497,875 | 90 | £6,552,161 | 208 | £27,902,503 | 68 | £16,645,455 | 133 | £22,201,178 |
Discussion
The top 20 universities plus selected other institutions account for £2.1 billion of investment related to infectious disease research across 5003 studies that were awarded between 1997 and 2010. Imperial College and Oxford received the most funding, and LSTM received the highest mean and median awards (owing primarily to being awarded several large grants from the Bill and Melinda Gates Foundation for neglected tropical disease research). Many universities had a clear focus on pre-clinical research, whilst the Medical Research Council focused on clinical trials, and the London and the Liverpool Schools of Tropical Medicine focused on implementation and operational research. Several universities carried out numerous studies on HIV, but few had a sizeable portfolio relating to tuberculosis research, or for antimicrobial resistance. The NHS has carried out numerous studies across the R&D value chain, but the amount of investment received by the NHS for infection research appears to be declining.
This analysis is the most comprehensive description available of UK infectious disease research, providing a rigorous inspection of awards across many institutions, many funders and many disease areas; however, our study has several limitations.3 There were little publicly available data from the pharmaceutical industry. Hence, there is a data gap in relation to funding of clinical trials and development of vaccines and diagnostics, which the pharmaceutical and biotechnology industries are typically financing. We rely on the original data being complete and accurate, and are unable to take into account distribution of funds from the lead institution to collaborating partners, nor can we assess quantity of each award given to overheads or the impact of the introduction of full-economic costing. Institutions such as the Sanger may also receive significant capital investments which may be used to fund research and this would not be captured here. Also, assigning studies to categories is a subjective process – although we used at least two researchers to do this to reduce inter-observer error. Our study focuses on UK-led investments – we do not know if similar patterns (e.g. a dominance of pre-clinical research and lack of public or charitably-funded clinical trials) would also emerge if the analysis is repeated for other high-income countries. We have not here measured either the outputs or impact of funded research, nor assessed the value of this research to the hosting institution.
UK investments for infectious disease research overall show a broadly varied portfolio across disease areas and type of science. Investments will often reflect the research track record and local expertise; for example, the UK schools of tropical medicine have clear expertise in parasitology, and also within implementation research where skills such as executing operational and epidemiological activity are important for carrying out the studies. Within the other leading (in terms of total investment) universities, they generally have several leading research groups or disciplines; for example, Imperial has received funding for many HIV studies, and with some overlap, they have also conducted a portfolio of research into therapeutics relating to infectious disease. UCL received less in the way of global health funding, though subsequent to the time period of this analysis they have made concerted efforts to bolster their standing globally in both research and education.7 UCL also has a large portfolio of HIV studies. Where universities had a smaller total portfolio and possibly less capacity to expand or compete in other topics, they often concentrated their efforts in specific areas, such as mycology research at Aberdeen, or Birmingham carrying out almost entirely pre-clinical research (much of which was related to infection-associated cancers).
There is a clear lack of public and philanthropic funding being directed towards clinical trials (with the exception of the Medical Research Council, where much of the investment was directed through its Clinical Trials Unit). Whilst the majority of investment will be sourced from the private sector in this area, it may also be down to a cautious approach from funders in that they will want a return on their investment, and trials are often expensive and methodologically difficult to perform; if the trial is in a low-income setting, then the difficulties may become even greater. Thus, it may be that investments are typically awarded to institutions that have a track record in relation to the proposed piece of research, and where the funder assumes a likelihood of ‘success’ (however that may be defined). UK investments in global health and infectious disease have been shown to follow previous colonial ties,4 and this may in part be explained by adoption of the English language and the presence of existing infrastructure in these countries that UK institutions have accessed previously (e.g. the Medical Research Council units in Gambia and Uganda). There are questions to be raised on whether a more ambitious approach from funders might lead to further high-impact research findings, and further help to improve health outcomes and reduce inequalities in other geographical areas.
Beyond the universities and the NHS, there is comparatively little in the way of research being led by institutions such as the Sanger and the Health Protection Agency. They collaborate on numerous studies, but given the expertise, equipment and facilities at the disposal of the Health Protection Agency as a whole, it is perhaps disappointing that the Health Protection Agency has not been able to initiate and lead more research than is shown here.
There is a decrease in the temporal trend of total investment by annum,3 although the figures here show that universities' income for infection research is broadly stable and it is research investments in the NHS that are particularly in decline. The NHS has carried out research across the R&D value chain, and again, given the expertise within the hospitals and other healthcare facilities, government and policy groups should consider how best to enable greater quantities of research within these settings as the NHS moves forward from its most recent and continuing reforms.
The UK has received significant quantities of investment to research a broad range of infectious diseases along the R&D value chain from pre-clinical to translational research. In order to better assess the distribution of investments and research output globally, there is a need for funders and institutions in other countries to provide similar and detailed information on funded studies, and so build a global research funding database; the World Health Organisation is creating a global R&D observatory to combine worldwide efforts in this area.8 Our analysis could be used for analytical work to identify gaps in research funding, reduce unnecessary duplication of research investments, prioritise health and social policy decisions and help inform future resource allocation for global research priorities. Institutions can similarly use this analysis for establishing expertise within their groups, identifying external collaborators and informing local research strategy. Future research can describe updated award data across greater numbers of institutions and include multi-country analyses to identify how research-active institutions in the UK compare with international universities.
Declarations
Competing interests
None declared
Funding
MGH works for the Infectious Disease Research Network, which has supported this work and is funded by the UK Department of Health. JRF has received funds from the Wellcome Trust and is a steering group member for the Infectious Disease Research Network. RA has received research funding from the Medical Research Council, the National Institute for Health Research and the UK Department for International Development. RA is a member of the Medical Research Council Global Health Group. DAJM has received funding from the Wellcome Trust, Medical Research Council and Department for International Development.
Ethical approval
Not required because no patient data is incorporated into this study.
Guarantor
MGH
Contributorship
MGH designed the study and collated the dataset. JRF checked and refined the dataset. MGH and JRF undertook data analysis and created the graphs and figures with input from DAJM and RA. MGH interpreted the data and wrote the draft and final versions. DAJM, JRF and RA commented on the dataset, draft paper and the final version. All authors reviewed and approved the final version.
Acknowledgements
We thank the Infectious Disease Research Network for their contribution to this work, and acknowledge the assistance of the research and development funding agencies for provision of data.
Provenance
Not commissioned; peer-reviewed by Tom Parks.
References
- 1.Moran M, Guzman J, Henderson K, Abela-Oversteegen L, Wu L, Omune B, et al. Neglected disease research and development: Is the global financial crisis changing R&D? Report, Policy Cures, Sydney, 2010. . [Google Scholar]
- 2.Moran M, Guzman J, Abela-Oversteegen L, Liyanage R, Omune B, Wu L, et al. Neglected disease research and development: Is innovation under threat? Report, Policy Cures, Sydney, 2011. [Google Scholar]
- 3.Head MG, Fitchett JR, Cooke MK, Wurie FB, Hayward AC, Atun R. UK investments in global infectious disease research 1997–2010: a case study. Lancet Infect Dis 2013; 13: 55–64. [DOI] [PubMed] [Google Scholar]
- 4.Fitchett JR, Head MG, Atun R. Infectious disease research investments follow colonial ties: questionable ethics. Int Health 2014; 6: 74–6. [DOI] [PubMed] [Google Scholar]
- 5.Head MG, Fitchett JR, Cooke MK, Wurie FB, Atun R. Differences in research funding for women scientists: a systematic comparison of UK investments in global infectious disease research during 1997–2010. BMJ Open 2013; 3: e003362–e003362. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Head MG, Fitchett JR, Cook MK, Wurie FB, Atun R, Hayward AC, et al. Systematic analysis of funding awarded for antimicrobial resistance research to institutions in the UK, 1997–2010. J Antimicrob Chemother 2014; 69: 548–554. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.University College London. Global Vision – UCL international strategy 2012–2017 A summary, 2011; http://www.ucl.ac.uk/global/about-us/International_Strategy_2012-2017_summary (accessed 14 March 2014). [Google Scholar]
- 8.Røttingen J-A, Regmi S, Eide M, et al. Mapping of available health research and development data: what’s there, what's missing, and what role is there for a global observatory? Lancet 2013. http://www.thelancet.com/journals/a/article/PIIS0140-6736(13)61046-6/fulltext (accessed 23 May 2013). [DOI] [PubMed] [Google Scholar]