Introduction
Thrombotic complications arising during the treatment of breast cancer can impact the breast reconstruction pathway. We set out to review the details of cases of thromboembolism occurring during neoadjuvant chemotherapy and peri-operatively to study the impact of the event and its management on subsequent breast reconstruction. Methods: We retrospectively reviewed the medical records of seven patients who had experienced a thrombotic event during their treatment of breast cancer between 2008 and 2012, who then proceeded to breast reconstruction. We recorded size and grade of tumour, neoadjuvant chemotherapeutic regimen, details of port insertion, planned reconstruction, thrombotic event and its management and the surgery performed and outcome. Results: All patients received chemotherapy via central venous access and went on to present with local symptomatic thrombosis. They were managed with anticoagulant regimens at the time of mastectomy and reconstruction, which were unique for each patient. The results revealed delays to surgery and modifications to planned reconstruction. Discussion: The majority of patients developing thrombotic complications go on to achieve successful reconstruction. There is significant variation in the anticoagulation management in this patient group. Identification of optimal anticoagulant regimes and the possibilities for prophylaxis may prove key in informing surgeons when planning the reconstructive process. Conclusion: An awareness of the effects of thrombotic events in this patient group is important in terms of developing an understanding of its impact on the performance of reconstruction, on the management of anticoagulation peri-operatively and on monitoring for post-operative complications.
Keywords: Neoadjuvant chemotherapy, Immediate breast reconstruction, DIEP flap, Venous thrombosis, Pulmonary embolism, Breast expander-implant
Highlights
-
•
Unknown of impact of thrombotic complications.
-
•
Majority achieve successful reconstruction.
-
•
Variation in anticoagulation.
1. Summary
Venous thrombotic complications arising from pre-operative central venous administration of chemotherapy can impact the primary breast reconstruction pathway. The records of seven such patients treated between 2008 and 2012 were retrospectively reviewed. All were managed with unique anticoagulation regimens at the time of surgery. Reconstruction was delayed in one case and the reconstructive plan significantly modified in a further case. Reconstructive breast surgeons should be aware of the vascular complications of neoadjuvant chemotherapy as they may impact on the reconstructive strategy.
2. Introduction
Line-related thromboembolic events are a recognised complication of intravenous chemotherapy administration. Neoadjuvant, primary or upfront chemotherapy is increasingly used to treat larger operable or locally advanced breast cancer, but a pre-operative thromboembolic event can significantly impact post-chemotherapy surgery. This is particularly significant when complex reconstruction is anticipated. There is limited research on the impact of this complication on breast reconstruction pathways and guidance for optimal management of these patients. Here we present our clinical experience over four years of patients with breast cancer who developed thrombotic complications of their neoadjuvant chemotherapy venous lines prior to mastectomy and immediate breast reconstruction.
A retrospective cohort study identified seven cases of pre-operative line thrombosis, who were managed under the joint care of the Breast and Plastic and Reconstructive Surgeons. We recorded patient age, tumour size and grade, receptor status, chemotherapy regime, position of catheter and flush regimen used and local treatment intent. We then analysed the details of the thromboembolic complication and the consequences for reconstruction.
All patients had tunnelled subclavian lines with implantable ports inserted by a specialist vascular access team, on the side contralateral to the breast tumour. A standard flushing regime of saline followed by a lock of 3 ml heparin at a concentration of 100u/ml was used. All patients received standard upfront chemotherapy using the FEC/T regime (fluorouracil, epirubicin, cyclophosphamide and docetaxel) [1].
Two example cases are described and the full data set presented in Table 1.
Table 1.
Summary of patient presentation and planned management.
| DoB | Tumour size | Tumour grade | Receptor status | Chemotherapy | Port | Treatment intent | Thrombotic complication | Outcome | Anticoagulation | |
|---|---|---|---|---|---|---|---|---|---|---|
| A | 6/1961 | 17 mm multifocal | III (3/7) | ER+(4)/HER2+ | FEC/T (T → AI), +RT, +herceptin | Tunnelled subclavian | Mastectomy + axillary clearance | Innominate and subclavian vein thrombosis | Temporary expandable implant; capsulectomy, expander removal + delayed salvage DIEP | Enoxaparin 0.95 ml daily omitted on day of surgery |
| B | 4/1974 | 21 mm | II (3/4) | ER+/HER2+ | FEC/T + herceptin | Right Tunnelled subclavian | LE + sentinel node → mastectomy + ALND, +DIEP flap | Occlusive R subclavian vein thrombosis | Surgery delayed 3/12 (zoladex + letrozole), pre-op RT |
|
| C | 2/1955 | Multifocal | III | ER+(8)/HER2− | FEC/T | Tunnelled subclavian | Immediate reconstruction DIEP flap | R subclavian vein thrombosis | Surgery as planned |
|
| D | 9/1965 | 28 mm multifocal | III (15/28) | ER+/HER2− | FEC/T | Tunnelled subclavian | Mastectomy + axiallary clearance + DIEP | Partially occlusive subclavian vein thrombosis | Surgery as planned |
|
| E | 2/1975 | Left | II | ER+(8)/HER2+ | FEC/T + herceptin | Tunnelled subclavian | simple mastectomy + ALNC | R axillary vein thrombosis | Surgery as planned |
|
| F | 7/1970 | 3 cm Recurrence | II | ER+(8)/HER2− | Docetaxel 6 cycles + FEC | Tunnelled subclavian | Skin sparring mastectomy + immediate SIEA | Left arm DVT | Surgery as planned |
|
| G | 12/1967 | Right 47 mm | III | ER+(8)/HER2− | ARTEMIS trial | Tunnelled subclavian | Skin sparring mastectomy, axillary dissection, lat dorsi reconstruction with McGhon 150SH expander | Subclavian and internal jugular vein thromboses | Surgery as planned |
|
Abbreviations: ER: Oestrogen Receptor; HER2: Human Epidermal Growth Factor Receptor 2; FEC/T: fluorouracil, epirubicin, cyclophosphamide & docetaxel; ARTEMIS: Chemotherapy plus bevacizumab; LE: Local Excision; ALND: Anterior Lymph Node Dissection; DIEP; Deep Inferior Epigastric Perforators flap; TRAM: Transverse Rectus Abdominis Myocutaneous flap; RT: Radiotherapy.
Case A is a 51 year old woman with a grade III, multifocal ER and HER2 positive right sided invasive ductal carcinoma. She was treated with primary chemotherapy and Herceptin through a tunnelled subclavian line. She was to proceed to mastectomy and axillary clearance with abdominal free flap reconstruction, followed by radiotherapy. An innominate and subclavian vein thrombosis was confirmed on ultrasound. She was managed with enoxaparin 1.5 mg/kg daily for three weeks, omitted on morning of surgery and recommenced 24 h following surgery, to continue for three months. The reconstructive plan was modified to an expandable implant inserted at the time of mastectomy. She received adjuvant radiotherapy, and 12 months later underwent a salvage DIEP reconstruction with a contralateral balancing LeJour mastopexy.
The patient in case B is a 38 year old lady who presented with a grade II ER and HER2 receptor positive tumour of her left breast. She was initially managed with FEC/T primary chemotherapy through a tunnelled subclavian line. The original surgical intent was local excision with sentinel node biopsy. However, it was unfortunately decided she then required a mastectomy with axillary lymph node dissection and DIEP free flap reconstruction was planned. She developed an occlusive thrombosis of her right subclavian vein (Fig. 1), which was managed therapeutically with fondaparinux. The surgery was delayed by three months. During this time the patient received zoladex and letrozole, in addition to pre-operatively radiotherapy. The therapeutic fondaparinux was omitted one day prior to surgery. Prophylactic dose enoxaparin was given 6 h post-operatively and nocte for two further days. Treatment fondaparinux was recommenced on day three. The reconstruction was achieved as planned.
Fig. 1.
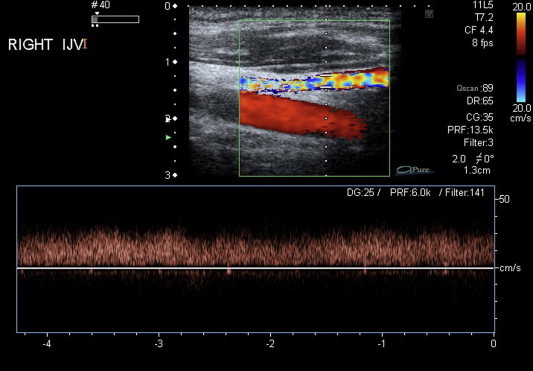
Doppler ultrasound image demonstrating subclavian vein thrombosis.
3. Discussion
Increasing use of neo-adjuvant chemotherapy will result in a greater number of line-related venous thrombotic complications. The majority of these patients eventually achieve successful post-mastectomy breast reconstruction.
Therapeutic anticoagulation necessary to treat port-related thrombosis can potentially lead to severe bleeding intra-operatively during the mastectomy and reconstruction unless it is managed appropriately. In general patients' treatment doses are omitted the day before surgery to enable safe surgery without excessive bleeding. However, lengthy surgery, especially in patients with cancer, confers a high risk of DVTs and PEs. Therefore, prophylactic anticoagulation peri-operatively has to be instituted. This does not treat the pre-existing blood clots, but does prevent their propagation and certainly prevents lower limb and iliac vein thrombosis. Once the risk of peri-operative bleeding has receded (usually day 3–5), the patients need to be recommenced on the therapeutic regime for at least three to six months or longer if the line remains in situ.
There was variation in anticoagulation management within this cohort; four patients received treatment dose enoxaparin, with peri-operative prophylactic dosing, one patient was managed on fondaparinux, one patient with tinzaparin and the remaining patient peri-operative clexane and long-term warfarin. There is limited guidance in the literature as the to most appropriate management in this patient group. Anticoagulation is continually evolving, with newer therapies available. Fondaparinux provides anticoagulation as effective as enoxaparin without the risk of heparin induced thrombocytopaenia and with a longer half-life [2]. However, reversal of the therapy is not possible. At the time of elective surgery the advantages of a shorter half-life and method of reversal may make enoxaparin a more appropriate choice.
The limitations of this study include the small patient sample size but this is not unexpected as chemotherapy line-induced thromboembolism during breast cancer treatment has hitherto been an uncommon complication. It was, however, interesting that all our patients had oestrogen-receptor positive breast cancers.
Breast cancer confers a relatively low risk for malignancy-associated venous thromboembolism; an incidence of 10 per 1000 per year compared to 110 per 1000 per year for pancreatic malignancy [3]. This is reflected in the Khorana score, which identified 5 predictive variables in a multivariate study for risk of venous thromboembolism [4]. These variables included site of cancer, raised platelet count, low haemoglobin or use of agent for erythropoiesis, raised leukocytes and BMI greater than 35. Those patients with pancreatic or stomach cancer score twice for very high risk site, whereas those with breast cancer are considered to have a low risk site and score 0. The total score confers a low, medium or high risk of thromboembolism over two and a half months. Further contributing factors for thromboembolism include cancer stage, with regional stage conferring an increased risk and distant metastases a much higher risk of thromboembolism [5].
Systemic cancer therapies contribute towards thrombotic risk (between 2 and 6 fold increase) [6]. There is currently no clear consensus on the role of anti-angiogenic therapies used in breast cancer treatment eg Bevacizumab in venous thrombosis, although an association with arterial events is recognised [7].
The mean onset for symptomatic thrombotic events has been shown to be 42.2 days [8]. The benefit of prophylaxis in reducing thromboembolic events in cancer patients with long-term use of central venous catheters has been studied with conflicting outcomes [9–11]. Current studies only consider small sample sizes and there is little evaluation of the possible bleeding risks [12]. The current overall consensus is prophylaxis is not necessary [12]. Recent evidence suggests that thromboembolic events can be safely reduced in patients with solid tumours using ultra-low molecular weight heparin (semuloparin) [13]; however, it is still unclear as to whether patients with a central venous line should specifically receive thromboprophylaxis. Concerning reconstruction, prophylaxis would prevent events occurring which may delay surgery, modify it or require management of anticoagulation peri-operatively.
The pathophysiological mechanisms in the hyper-coagulable state associated with malignancy have recently been studied in relation to the role of microparticles in breast cancer. Data shows an increased thrombogenicity of microparticles following chemotherapy administration, a possible indicator for throboprophylaxis at this time [14].
Patients with line-related thrombosis, who are scheduled to have immediate breast reconstruction with abdominal flaps, should not have their therapeutic anticoagulation administered into their abdominal tissues as this may damage the perforators on which abdominal free flaps are based. This was advised to all our patients.
No intra or post-operative bleeding complications were identified in this cohort. A concern when operating on the breast in the presence of central vein thrombosis is the effect of any collateral circulation, which may have developed. Venous flow or excessive bleeding as a result of collaterals was not encountered in any of the cases treated in the current series. Whilst this phenomenon is well established with superior vena caval obstruction, collaterals are less significant with axillary or subclavian thrombosis alone [15]. Although chest wall and breast parenchymal collaterals have also been reported, the impact of collateral circulation on the eventual operation in minimised by the routine placement of subclavian catheters on the contralateral side. Surgical technique selection may be dependent on the preservation of these vessels or a standard mastectomy technique may result in excessive bleeding.
Microsurgical breast free flap anastomoses are usually performed to the ipsilateral internal mammary or the axillary vessels (subscapular–thoracodorsal axis), but these are not usually affected as the chemotherapy ports are placed contralaterally. However, a large enough thrombosis, for example in the innominate vein, can potentially compromise venous drainage of the flap. Similarly if contralateral recipient vessels were needed, because of unusable ipsilateral vessels, microsurgical flap circulatory compromise may result.
As these cases demonstrate line-associated thrombosis will be increasingly encountered by surgeons as more patients receive neoadjuvant chemotherapy and are managed by indwelling venous access devices. With multidisciplinary cooperation between surgeons, oncologists and haematologists, the surgical management plan for these patients can remain largely unaffected. It is very important to closely liaise with the haematologists for advice about the peri-operative anticoagulation care. Further research with larger cohorts is required to establish the optimum anticoagulation regimen and to develop this with newer anticoagulants. With these developments the benefit of prophylactic anticoagulation should continue to be considered. Reconstructive surgeons should also be flexible enough to alter their surgical plan in patients who develop line-related thrombosis. We recommend a low threshold for delaying the reconstruction in order to minimise complications. In patients who refuse to accept mastectomy without reconstruction a ‘babysitter’ expander can be used as this is a much smaller operation and can serve to preserve the skin-envelope in a manner similar to the concept of ‘delayed-immediate reconstruction’, popularised by Kronowitz et al. [16].
Presentations
British Association of Plastic Reconstructive and Aesthetic Surgeons (BAPRAS) Winter Scientific Meeting 4th–7th December 2012 poster presentation. The 49th Congress of the European Society for Surgical Research (ESSR), Budapest, Hungary: May 21–24, 2014. Poster presentation.
Disclosures
-
•
The patients were fully consented for the surgery and provided both verbal and written consent for the use of the images and case histories in this article.
-
•
This article is not being considered for publication nor has it been published by any other medical journal.
-
•
The authors have no other financial interests or commercial associations to declare in relation to the contents of this article.
Conflicts of interest
None.
Funding
None.
Ethical approval
Retrospective audit project.
Service evaluation only.
Access to notes approved.
Consent
Not a case report.
Author contribution
Richards: data collection, analysis, interpretation, writing, editing.
Forouhi: data analysis & interpretation, writing up, editing.
Johnson: data analysis & interpretation, writing up, editing.
Malata: study concept + design, data collection, data analysis, writing up, editing.
Guarantor
Professor Charles Malata.
References
- 1.Azzawi K., Ismail A., Forouhi P., Earl H., Malata C.M. Influence of neoadjuvant chemotherapy on outcomes of immediate breast reconstruction. Plast Reconstr Surg. 2010 Jul;126(1):1–11. doi: 10.1097/PRS.0b013e3181da8699. [DOI] [PubMed] [Google Scholar]
- 2.Büller H.R., Davidson B.L., Decousus H., Gallus A., Gent M., Piovella F. Fondaparinux or enoxaparin for the initial treatment of symptomatic deep venous thrombosis A randomized trial. Ann Intern Med. 2004;140(11):867–873. doi: 10.7326/0003-4819-140-11-200406010-00007. [DOI] [PubMed] [Google Scholar]
- 3.Timp J.F., Braekkan S.K., Versteeg H.H., Cannegieter S.C. Epidemiology of cancer- associated venous thrombosis. Blood. 2013;122/10:1712–1723. doi: 10.1182/blood-2013-04-460121. [DOI] [PubMed] [Google Scholar]
- 4.Khorana A.A., Kuderer N.M., Culakova E., Lyman G.H., Francis C.W. Development and validation of a predictive model for chemotherapy-, associated thrombosis. Blood. 2008;111:4902–4907. doi: 10.1182/blood-2007-10-116327. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Wun T., White R.H. Epidemiology of cancer-related venous thromboembolism. Best Pract Res Clin Haematol. 2009;22(1):9–23. doi: 10.1016/j.beha.2008.12.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Sousou T., Khorana A.A. New insights into cancer-associated thrombosis. Arterioscler Thromb Vasc Biol. 2009;29(3):316–320. doi: 10.1161/ATVBAHA.108.182196. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Connolly G.C., Francis C.W. Cancer-associated thrombosis. ASH Educ Book. 2013;1:684–691. doi: 10.1182/asheducation-2013.1.684. [DOI] [PubMed] [Google Scholar]
- 8.Luciani A., Clement O., Halimi P., Goudot D., Portier F., Bassot V. Catheter-related upper extremity deep venous thrombosis in cancer patients: a prospective study based on Doppler US. Radiology. 2001;220:655–660. doi: 10.1148/radiol.2203001181. [DOI] [PubMed] [Google Scholar]
- 9.Verso M., Agnelli G. Venous thromboembolism associated with long-term use of central venous catheters in cancer patients. J Clin Oncol. 2003;21:3665–3675. doi: 10.1200/JCO.2003.08.008. [DOI] [PubMed] [Google Scholar]
- 10.Bérubé C, Zehnder JL. Catheter induced upper extremity venous thrombosis. [Uptodate.com].
- 11.Baglin T, Barrowcliffe TW, Cohen A Greaves M, British Committee for Standards in Haematology. Guidelines on the use and monitoring of heparin. Br J Haematol;133:19–34. [DOI] [PubMed]
- 12.Vescia S., Baumgärtner A.K., Jacobs V.R. Management of venous port systems in oncology: a review of the current evidence. Ann Oncol. 2008;19(1):9–15. doi: 10.1093/annonc/mdm272. [DOI] [PubMed] [Google Scholar]
- 13.Agnelli G., George D.J., Kakkar A.K., Fisher W., Lassen M.R., Mismetti P. Semuloparin for thromboprophylaxis in patients receiving chemotherapy for cancer. N Engl J Med. 2012;366(7):601–609. doi: 10.1056/NEJMoa1108898. [DOI] [PubMed] [Google Scholar]
- 14.Aharon A., Brenner B., Barsela G., Loven D. The role of breast cancer cell microparticles in thrombogenicity, angiogenesis and apoptosis following chemotherapy. Thromb Res. 2014;133(S26):0049–3848. [Google Scholar]
- 15.Richard H.M., Selby J.B., Gay S.B., Tegtmeyer C.J. Normal venous anatomy and collateral pathways in upper extremity venous thrombosis. Radiographics. 1992;12:527–534. doi: 10.1148/radiographics.12.3.1609143. [DOI] [PubMed] [Google Scholar]
- 16.Kronowitz S.J., Hunt K.K., Kuerer H.M., Babiera G., McNeese M.D., Buchholz T.A. Delayed-immediate breast reconstruction. Plast Reconstr Surg. 2004;113(6):1617–1628. doi: 10.1097/01.prs.0000117192.54945.88. [DOI] [PubMed] [Google Scholar]


