Abstract
Background:
Uremic pruritus (UP) is a very distressing symptom and remains one of the most frustrating and potentially disabling symptoms in patients with end-stage renal disease (ESRD). Its etiopathogenesis remains unclear and complex. The aim of this study was to investigate the possible role of interleukin-2 (IL-2) in UP, and correlate its level with the severity of itching in ESRD patients.
Patients and Methods:
This study was carried out on 60 patients on maintenance hemodialysis (HD), 30 patients with UP and 30 patients without UP, and 30 apparently healthy age- and sex-matched subjects as controls. Itch intensity was scored as mild, moderate, and severe using five-dimensional itch scale. Some relevant clinical parameters (age, sex, xerosis, presence of neuropathy, duration of dialysis, complete medical history, and history of pruritic skin diseases) and laboratory findings including creatinine, urea, calcium, phosphorus, parathyroid hormone, and serum levels of IL-2 were evaluated.
Results:
In our study, we found a statistically significant difference in IL-2 level between patients and controls. However, there was no statistically significant difference in IL-2 levels between cases with pruritus and cases without pruritus. Also, there was a statistically significant relation between IL-2 level and duration of the disease.
Conclusion:
Further studies are needed to understand the contribution of IL-2 and possibly other cytokines in the pathogenesis of this distressing symptom in ESRD.
Keywords: End-stage renal disease, hemodialysis, interleukin-2, uremic pruritus
What was known?
Uremic pruritus still remains a distressing symptom that affects large number of patients undergoing HD.
ESRD itch is associated with a proinflammatory state and an imbalance in the Th1 cytokines. HD patients with pruritus have significantly enhanced Th1 cytokines. In line with this theory, ultraviolet B attenuates Th1 cell differentiation and decreases IL-2 production.
Pruritus in patients with ESRD on HD is a complex multifactorial problem that necessitates further investigation.
Introduction
Uremic pruritus (UP) remains one of the most distressing and disabling symptoms in patients undergoing hemodialysis (HD).[1] Interleukin-2 (IL-2) has a well-documented role in induction of pruritus.[2] However, conflicting data have been found as regards its role in UP. In this work, we tried to investigate the possible role of IL-2 in UP, and correlate its level with the severity of itching in HD patients.
Patients and Methods
This study was carried out on 60 patients on maintenance HD, 30 patients with UP and 30 patients without UP, and 30 apparently healthy age- and sex-matched subjects as controls. Subjects with mean age ± standard deviation (SD) of 52.8 ± 10.26 years were selected in a hospital-based case–control study conducted over a period of 3 months (July 2011-September 2011).
Patients were recruited from the HD unit of Al-Zahraa University Hospital in Cairo. All patients were on regular HD three times weekly.
Exclusion criteria for patients
Systemic pruritic diseases such as hepatic disease and allergic diseases
Pruritic dermatological diseases such as eczema, lichen simplex, urticaria, and infections
Immunosuppressive disease such as HIV infection and neoplastic diseases
Immunosuppressive therapy in the past 3 months.
All eligible patients were submitted to the following:
Detailed history with special reference to age, sex, duration, and intensity of pruritus
General and dermatological examination for exclusion of other causes of pruritus
-
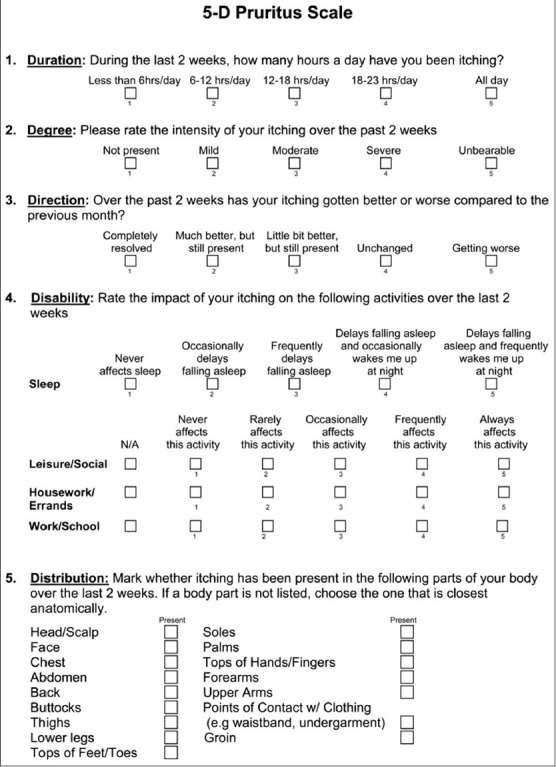
Assessment of itching severity by five-dimensional (5-D) itch scale which is multidimensional questionnaire containing five dimensions (degree, duration, direction, disability, and distribution) designed to be useful as an outcome measure for itching severity in clinical studies as follows:[3]
The scores of each of the five domains are achieved separately and then summed together to obtain a total 5-D score. 5-D scores can potentially range between 5 (no pruritus) and 25 (most severe pruritus).
-
Laboratory tests:
- Serum glutamic oxaloacetic transaminase (SGOT), serum glutamic pyruvate transaminase (SGPT), urea, creatinine, uric acid (UA), calcium (Ca+), phosphorus (P), and parathyroid hormone (PTH) levels
- Serum (IL-2) by ELISA technique using Quantikine Human IL-2 Immunoassay.
Apparently, healthy, age- and sex-matched control subjects were recruited from relatives of patients who had not received any systemic treatment that may cause pruritus during the last 4 weeks prior to sample.
After explaining the purpose of the study which was approved by the faculty ethics committee and taking the consents of both cases and controls, data were collected through personal interview and they were asked to fulfill a specially designed structured questionnaire.
Sampling
Three milliliters of venous blood were aseptically collected from each patient and control. Samples were dispensed in tubes and left to clot for 30 min at 37°C, then they were centrifuged at 2000-3000 rpm for 20 min. The collected sera were finally stored at −20°C until analysis.[4]
ELISA: Principle of the assay
The kit assay Human IL-2 level, in the sample, used purified Human IL-2 antibody to coat microtiter plate wells and made solid-phase antibody. Then IL-2 was added to wells; IL-2 antibody combined with horse raddish peroxidase (HRP)-labeled goat anti-human to became antibody-antigen-enzyme-antibody complex; after washing completely, TMB substrate solution was added; now tetramethylbenzidine (TMB) substrate became blue color at HRP enzyme catalyzed; reaction was terminated by the addition of a sulfuric acid solution; and finally the color change was measured spectrophotometrically at a wave length of 450 nm. The concentration of Human IL-2 in the samples was then determined by comparing the optical density of the samples to the standard curve.[4]
Statistical analysis
Statistical analysis was done using SPSS 15.0 (SPSS Inc., Chicago, USA) as following:
Mean and SD were calculated to measure central tendency and dispersion of quantitative data.
Frequency of occurrence was calculated to measure qualitative data.
Comparing groups was done using the following:
Chi-square test (χ2) for comparison of qualitative data
Student's “t”-test for quantitative data of two independent samples and ANOVA test was also done to determine the significance in the difference between means.
The level of significance was taken at P ≤ 0.05.[5]
Results
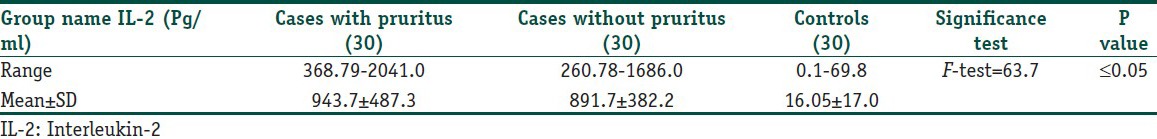
The duration of maintenance HD in all patients ranged from 1.5 to 12 years. In this study, there was a statistically significant difference between IL-2 level between patients and controls (P ≤ 0.05), but there was no statistically significant difference between IL-2 levels in cases with pruritus and in cases without pruritus (P > 0.05; Table 1).
Table 1.
Levels of interleukin-2 among the studied groups
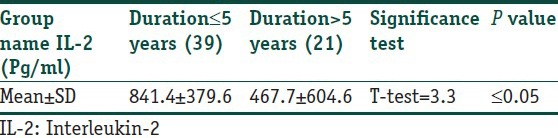
As shown in Table 2, there was no statistically significant difference between IL-2 level and severity of pruritus (P > 0.05) Table 3 reveals statistically significant relation between IL-2 level and duration of disease. The level of IL-2 was significantly high in patients with disease duration of ≤5 years more than among patients with disease duration of ≥5 years.
Table 2.
Relation of interleukin-2 with pruritus score
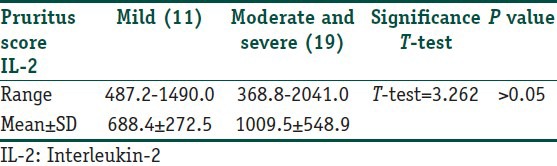
Table 3.
Comparison between serum interleukin-2 levels as regard duration of disease
It is shown in Table 4, there was a statistically significant difference in PTH and P levels between patients and controls (P ≤ 0.05), but there was no statistically significant difference between Ca+level among patients and control.
Table 4.
Serum parathyroid hormone, phosphorus, and calcium Ca+ levels among cases with pruritus, cases without pruritus, and controls
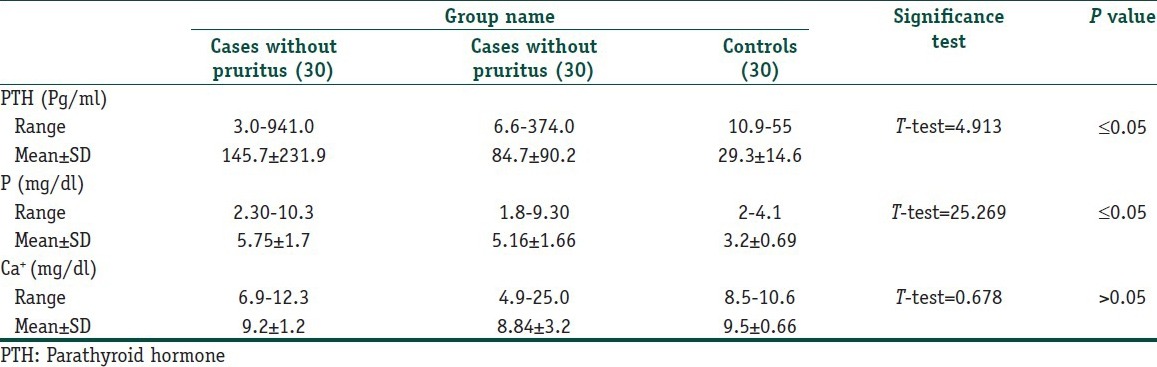
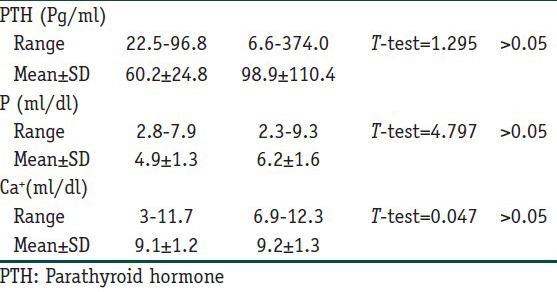
Also, there was no statistically significant difference among PTH, P, Ca+ levels, and severity of pruritus (P > 0.05; Table 5).
Table 5.
Relation of serum parathyroid hormone, phosphorus, and calcium (Ca+) levels with pruritus score
There was a statistically significant difference among urea, creatinine, and UA levels between patients and control group, but there were no statistically significant differences between their levels between patients with pruritus and patients without pruritus [Figure 1]. No statistically significant difference was found among urea, creatinine, UA levels, and severity of pruritus (P > 0.05; Figure 2).
Figure 1.
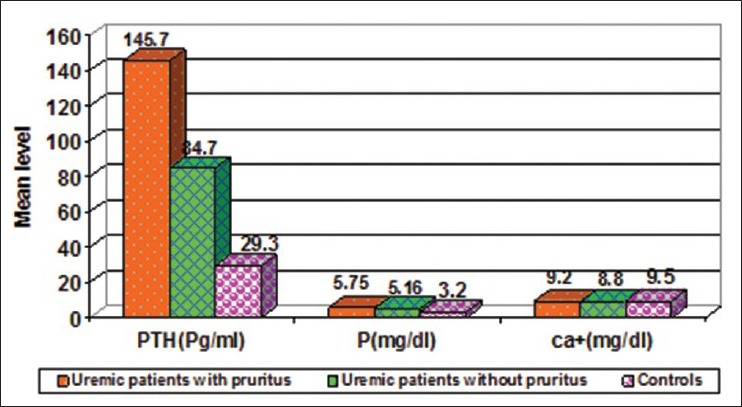
There was a statistically significant difference among urea, creatinine, and uric acid levels between patients and control group, but there were no statistically significant differences between their levels between patients with pruritus and patients without pruritus
Figure 2.
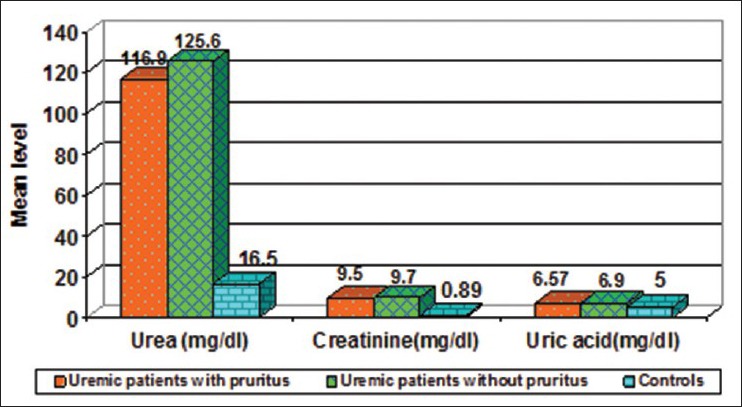
No statistically significant difference was found among urea, creatinine, uric acid levels, and severity of pruritus (P > 0.05)
Discussion
UP is a common and sometimes severe complication of chronic renal failure. The pathogenesis underlying UP is poorly understood and most likely multifactorial. Possible pathogenic mechanisms may include elevated levels of toxins, proteases, IL2, tumor necrosis factor and or other inflammatory mediators.[6]
In this study, no significant elevation in serum level of IL-2 was found in patients with UP as compared to patients without pruritus.
These results are not in accordance with Jamshid et al.[7] who demonstrated a significant increase in the serum IL-2 in HD patients with UP compared to those without UP.
The discrepancy between the above-mentioned studies may be explained by the fact that Jamshid et al.[7] scored pruritus by visual analog scale >4 (moderate) for all patients, for more than 3 months. In our study, pruritus was scored by 5-D pruritus scale as mild, moderate and severe, for the preceding 2 weeks.
Oppenhein et al.[8] explained that in normal human lymphocytes stimulated with para-hippuric acid, IL-2 messenger ribonucleic acid (mRNA) expression becomes detectable after 4 h, reaches peak concentration at 12 h, and thereafter declines rapidly. So, IL-2 production is very transient and could not be easily detected in the serum.
Also Duque et al.[9] found that tacrolimus, which blocks IL-2 production, was not found to be superior to placebo in relieving UP in a double-blind randomized clinical trial.
Moreover, Lin et al.[10] found that dialyzing patients with polymethylmethacrylate artificial kidney for 4 weeks resulted in significant reduction in UP severity, this type of membrane was supposed to remove more inflammatory cytokines than other high-flux membranes; but in our study, dialyzing membrane was high purity salt-free membrane 7, this difference in the type of membrane may indicate why IL-2 was not significantly elevated in UP in our study.
All the above findings may indicate why IL-2 was not significantly elevated in patients with UP in our study.
In our study, we found an inversely proportional relationship between IL-2 level and duration of ESRD; this may be interpreted by the findings of Jiangzhong et al.,[11] who stated that there is deprivation of the immune function in patients with chronic HD more than 7 years.
Schollmeyer et al.[12] concluded that the absolute numbers of circulating T-cells in uremic patients are reduced. With increasing time of dialysis, the alterations become more pronounced and this may interpret the finding in our study in which IL-2 levels decreased in patients on HD more than 5 years.
We detected an elevation in the serum level of PTH in patients with UP but without significant differences between pruritic and non-pruritic patients. This finding is in agreement with Cho,[13] who observed no statistical significant difference in the level of PTH among his cases.
These results are not in agreement with Chou et al.,[14] who found rapid relief of UP after parathyroidectomy.
In our study, we did not find a relationship between the itching scale and the serum levels of calcium and P. These were also observed by Ji-Chen et al.,[15] who stated that no relation exists between Ca+ and P serum levels among pruritic and non-pruritic patients.
Conclusion
The pathogenesis of pruritus is complex and multifactorial; it is even more so in cases of ESRD patients on HD. The immune dysregulation associated with ESRD may be one of the main causes for this distressing symptom. There is a substantial body of evidence in favor of the concept that ESRD is an inflammatory state, UP is considered as a skin counterpart of chronic ongoing inflammation; however, the direct contribution of IL-2 in the pathogenesis of pruritus is yet to be confirmed.
Recommendation
Further researches on larger scale of patients with assessment of all limbs of the immune system are recommended.
What is new?
IL-2 is probably not a key player in pruritus associated with ESRD patients on HD but it is one of many markers for the proinflammatory dysregulation present in ESRD and the longer the duration of the disease the lower the level of this cytokines indicating deprivation of the immune system.
Footnotes
Source of support: Researchers personal financial
Conflict of Interest: There is no conflict of interest of any of the authors with the results of this study.
References
- 1.Kuypers DR. Skin problems in chronic kidney disease. Nat Clin Pract Nephrol. 2009;5:157–70. doi: 10.1038/ncpneph1040. [DOI] [PubMed] [Google Scholar]
- 2.Sonkoly E, Muller A, Lauerma AI, Pivarcsi A, Soto H, Kemeny L, et al. IL-31: A new link between T cells and pruritus in atopic skin inflammation. J Allergy Clin Immunol. 2006;117:411–7. doi: 10.1016/j.jaci.2005.10.033. [DOI] [PubMed] [Google Scholar]
- 3.Thornton AM, Donovan EE, Piccirillo CA, Shevach EM. Cutting edge: IL-2 is critically required for the in vitro activation of CD4+CD25+T cell suppressor function. J Immunol. 2004;172:6519–23. doi: 10.4049/jimmunol.172.11.6519. [DOI] [PubMed] [Google Scholar]
- 4.Elman S, Hynan LS, Gabriel V, Mayo MJ. The 5-D itch scale: A new measure of pruritus. Br J Dermatol. 2010;162:587–93. doi: 10.1111/j.1365-2133.2009.09586.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Malek TR, Castro I. Interleukin-2 receptor signaling: At the interface between tolerance and immunity. Immunity. 2010;33:153–65. doi: 10.1016/j.immuni.2010.08.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Sokal RR. The principles and practice of statistics in biological research. In: Robert RS, Rolf JF, editors. Text Book of Biometry. 3rd ed. New York: Freeman WH; 1995. pp. 313–4. [Google Scholar]
- 7.Corić-Martinović V, Basić-Jukić N. Uremic pruritus. Acta Med Croatica. 2008;62:32–6. [PubMed] [Google Scholar]
- 8.Fallahzadeh MK, Roozbeh J, Geramizadeh B, Namazi MR. Interleukin-2 serum levels are elevated in patients with uremic pruritus: A novel finding with practical implications. Nephrol Dial Transplant. 2011;26:3338–44. doi: 10.1093/ndt/gfr053. [DOI] [PubMed] [Google Scholar]
- 9.Oppenheim JJ, Faltynek CR, Ruscetti FW. Cytokines. In: Stites P, Terr AI, Parslow G, editors. Text Book of Medical Immunology. 9th ed. Norwalk, San Mateo, California: Appelton and Lange; 1997. pp. 146–69. [Google Scholar]
- 10.Duque MI, Yosipovitch G, Fleischer AB, Jr, Willard J, Freedman BI. Lack of efficacy of tacrolimus ointment 0.1% for treatment of hemodialysis-related pruritus: A randomized, double-blind, vehicle-controlled study. J Am Acad Dermatol. 2005;52:519–21. doi: 10.1016/j.jaad.2004.08.050. [DOI] [PubMed] [Google Scholar]
- 11.Lin HH, Liu YL, Liu JH, Chou CY, Yang YF, Kuo HL, et al. Uremic pruritus, cytokines, and polymethylmethacrylate artificial kidney. Artif Organs. 2008;32:468–72. doi: 10.1111/j.1525-1594.2008.00568.x. [DOI] [PubMed] [Google Scholar]
- 12.Jiangzhong M, Dandan LI, Peng K. Influence of hemodialysis on peripheral mood prostaglandin E2 (PGE2), NK cell and T cell subsets in uremic patients. Chin J Blood Purif. 2003;6:459–60. [Google Scholar]
- 13.Schollmeyer P, Bozkurt F. The immune status of the uremic patient: Hemodialysis vs CAPD. Clin Nephrol. 1988;30:S37–40. [PubMed] [Google Scholar]
- 14.Cho YL, Liu HN, Huang TP, Tarng DC. Uremic pruritus: Roles of parathyroid hormone and substance P. J Am Acad Dermatol. 1997;36:538–43. doi: 10.1016/s0190-9622(97)70240-8. [DOI] [PubMed] [Google Scholar]
- 15.Chou FF, Ho JC, Huang SC, Sheen-Chen SM. A study on pruritus after parathyroidectomy for secondary hyperparathyroidism. J Am Coll Surg. 2000;190:65–70. doi: 10.1016/s1072-7515(99)00212-4. [DOI] [PubMed] [Google Scholar]


