Abstract
Mycosis fungoides is the most common type of cutaneous T-cell lymphoma (CTCL) and a rare disorder that typically affects older adults with erythematous scaling patches and plaques. Hypopigmented patches are a rare clinical variant of the disease. Granulomatous mycosis fungoides (GMF) is also a rare type of CTCL. No particular clinical criteria are available for the diagnosis of GMF, because of its variable presentations, and so the detection of GMF is primarily considered as a histopathological diagnosis. Rarely, a co-existence of more than one clinical or histopathological feature of mycosis fungoides may be present. To the best of our knowledge this is the first report of MF that shows the simultaneous co-existence of more than one clinical and histopathological variant of MF. We present a 29-year-old female with clinical presentations of both classic and hypopigmented mycosis fungoides (MF), and also the histopathological features of the classic and granulomatous types of the disease.
Keywords: Co-existence, granulomatous mycosis fungoides, hypopigmented mycosis fungoides, mycosis fungoides
What was known?
Mycosis fungoides is the most common type of cutaneous T-cell lymphoma (CTCL) and a rare disorder that typically affects older adults with erythematous scaling patches and plaques.
Introduction
Mycosis fungoides (MF) is the most common type of cutaneous T-cell lymphoma (CTCL) which typically affects older adults.[1,2] Early typical lesions in MF are variably sized erythematous finely scaling lesions, which may be mildly pruritic; as the lesions progress, they become infiltrated, reddish-brown scaling plaques. Some patients may develop nodules or tumors.[1] Patients also present with atypical presentations such as hypopigmented lesions.[1] Granulomatous mycosis fungoides (GMF) is a rare type of cutaneous T cell lymphoma.[3] No particular clinical criteria are available for the diagnosis of GMF because of its variable presentations; therefore, detecting GMF is primarily considered as a histopathological diagnosis.[3,4,5] Rarely, the co-existence of more than one clinical or histopathological feature of mycosis fungoides may be present. To the best of our knowledge this is the first report of MF that shows the simultaneous co-existence of more than one clinical and histopathological variant of MF. We describe a 29-year-old female with various clinical lesions of MF, i.e., the erythematous scaly and hypopigmented patch lesions, and also the different histopathological features of the disease such as the granulomatous and classic variants.
Case Report
A 29-year-old Iranian woman was referred to the Al-Zahra Hospital MF clinic which is an academic referral center for cutaneous lymphoma of Isfahan University of Medical Sciences, Iran. She had had a history of developing bilaterally nonpruritic erythematous and hypopigmented patches on both the arms and axillary areas for 3 years. At the time of referral, she had hypopigmented and depigmented macules and patches (pityriasis versicolor-like lesions) [Figure 1], erythematous scaly plaques, and a few small nodules (<1 cm) on the upper and lower extremities, flanks, buttocks, abdomen, and both axillary areas [Figures 1 and 2]. Body surface area involvement was about 30%. On physical examination, no lymphadenopathy or organomegaly was detected. Her family history was negative in this respect. Four skin biopsies were obtained from four different anatomic sites with different clinical pictures (1 - left flank: Erythematous patch, 2 - left buttock: Erythematous plaque, 3 - left inner aspect of thigh: Erythematous patch and 4 - left arm: Hypopigmented patch) and immunohistochemical (IHC) studies were performed on paraffin sections too. Histopathological examination confirmed the diagnosis of MF in all of the specimens and, in addition, IHC staining supported this diagnosis [Figures 3 and 4]. Interestingly, the specimen, which had been obtained from the erythematous patch of the inner thigh, showed granuloma formation in some areas and these findings were consistent with the MF granulomatous variant [Figures 5]. So our clinical suspicion of MF was confirmed by the results of pathology and IHC staining. The complete blood count, peripheral blood smear, blood chemistry panel, and liver function tests were normal. The LDH level was 241 IU/L (normal range: 225-450). Chest X-ray revealed no abnormality. The initial stage of the patient was on Ib. She was treated with phototherapy and advised to pursue regular follow-up sessions for the monitoring of her condition.
Figure 1.

Mycosis fungoides. Hypopigmented patches seen on left forearm, abdomen, and flank. Erythematous patches on the inner aspect of left thigh
Figure 2.

Mycosis fungoides. Co-existence of various clinical features of mycosis fungoides in a young female. Erythematous patches and plaques on left flank and buttock, and hypopigmented patches on the left arm
Figure 3.
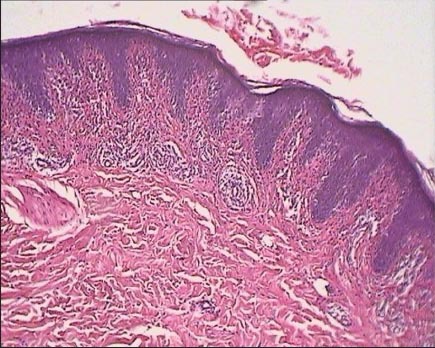
Histopathological feature of the patch stage of mycosis fungoides. Sections from the left arm (hypopigmented) patch show epidermotropism of atypical lymphocytes, mostly in basal layer and dermis, mild interstitial infiltrate of small lymphocytes seen (H and E×100)
Figure 4.
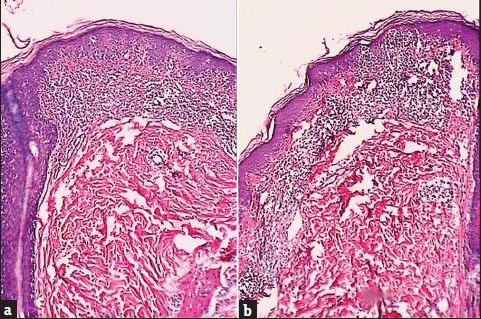
Histopathological feature of mycosis fungoides. (a: Patch, b: Plaque.) Sections show epidermotropism of atypical lymphocytes in epidermis with focal Pautrieræs microabscesses. Upper dermis reveals prominent fibrosis with thick and wiry collagen bundles in haphazard directions intermingled with a moderately dense and band-like infiltration of atypical lymphoid cells (H and E×100)
Figure 5.
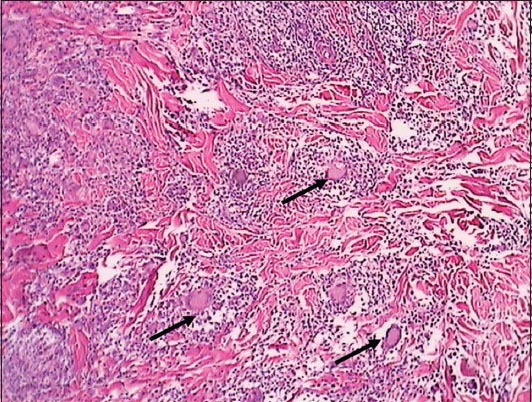
Granulomatous mycosis fungoides. Moderately dense infiltration of small-to medium-sized atypical lymphocytes in dermis with irregular and convoluted hyperchromatic nuclei admixed with some histiocytes and multiple multinucleated giant cells (arrows show the granulomas and multinucleated giant cells) producing ill-defined nonnecrotizing granulomatous aggregates and extending form superficial dermis down to deep reticular dermis. Also phagocytosis of atypical lymphocytes by multinucleated giant cells (H and E×100)
Discussion
About 75% of cutaneous lymphomas are in the category of T-cell lymphomas.[6] MF is the most common type of CTCL which is responsible for nearly 50% of all primary cutaneous lymphomas.[1] Although MF is a rare disorder of older adults (55-60 years) with a 2:1 male:female ratio, our patient was young and female.[1,2] In an epidemiologic study that we performed in Isfahan, Iran, the mean age of patients with MF was 43.14 years and the male:female ratio was 3:4.[7] Thus it seems that, on average, Iranian patients are younger than patients in the West and the number of female cases is higher.[7] Classic clinical presentations of MF are erythematous scaling patches and plaques which may progress to nodules and tumors.[1] Typical histopathology of early lesions shows superficial band-like or lichenoid infiltrates, mainly composed of lymphocytes. Atypical lymphocytes with small to medium-sized, highly convoluted (cerebriform), and sometimes hyperchromatic nuclei are few, and are mostly confined to the epidermis (epidermotropism).[1] The presence of intraepidermal nests of atypical cells (Pautrier's microabscesses) is highly characteristic but is only seen in a minority of patients.[1] Clinical variants of MF such as bullous, hyper, or hypopigmented MF are histopathologicaly similar to classic MF and are not considered separately.[1] Purely hypopigmented MF is rare. Primary lesions may present in the ages ranging between 2 and 19 years, but histologic diagnosis may be delayed until 2-10 years later.[8] Its usual presentation is scattered hypopigmented macules or large patches on the trunk and the extremities.[8] Hypopigmented lesions are generally asymptomatic, nonatrophic, and nonscaly and nonpruritic, but itching may occur in some cases such as that in work by Topar et al.[6] Das et al. describe a case of a 24-year-old male, with asymptomatic vitiligo-like skin lesions harboring the characteristics of mycosis fungoides and lesions with the characteristics of large plaque Parapsoriasis, developing over preexisting hypopigmented lesions, as the presentation of unusual clinical features and conspicuous histopathological findings.[9] In our case, hypopigmented lesions also were seen coexisting with instances of early patch and plaque. The typical histologic feature of MF usually shows epidermotropism by abnormal lymphocytes and sometimes Pautrier microabscesses.[1,8] Granulomatous mycosis fungoides (GMF) is a rare histological variant of CTCL without clinical distinction from classic MF. Due to the variable presentations of GMF, no particular clinical criteria are available for the diagnosis of GMF; therefore, detecting GMF is primarily considered as a histopathological diagnosis.[3,4,5] In our case the erythematous patch of the inner thigh showed granuloma formation in some areas and these findings were consistent with the MF granulomatous variant. So in this report, we described a patient with the clinical features of both classic and hypopigmented MF and the histological features of classic MF and also the granulomatous variant of the disease. To the best of our knowledge, in the literature, there is no other case with various clinical and histopathological presentations of MF present simultaneously in one patient.
What is new?
To the best of our knowledge, there is no other case with various clinical (classic and hypopigmented) and histopathological (classic and granulomatous types) presentation simultaneously in one patient.
Footnotes
Source of support: Skin disease and leishmaniasis research center, Isfahan University of Medical Sciences, Isfahan, Iran.
Conflict of Interest: Nil.
References
- 1.Bolognia JL, Jorizzo JL, Schaffer JV. Dermatology. In: Willemze R, editor. Cutaneous T-cell Lymphoma. 3nd ed. Madrid: Mosby (Elsevier); 2012. pp. 2017–27. [Google Scholar]
- 2.Koga M, Imafuku S, Nakayama J. Various skin manifestations of mycosis fungoides: Histopathological features and prognosis. Fukuoka Igaku Zasshi. 2011;102:229–36. [PubMed] [Google Scholar]
- 3.Gutte R, Kharkar V, Mahajan S, Chikhalkar S, Khopkar U. Granulomatous mycosis fungoides with hypohidrosis mimicking lepromatous leprosy. Indian J Dermatol Venereol Leprol. 2010;76:686–90. doi: 10.4103/0378-6323.72470. [DOI] [PubMed] [Google Scholar]
- 4.Fischer M, Wohlrab J, Audring TH, Sterry W, Marsch WC. Granulomatous mycosis fungoides. Report of two cases and review of the literature. J Eur Acad Dermatol Venereol. 2000;14:196–202. doi: 10.1046/j.1468-3083.2000.00047.x. [DOI] [PubMed] [Google Scholar]
- 5.Von Nida J, Randell P, Heenan P. Granulomatous mycosis fungoides with extensive chest wall involvement. Australas J Dematol. 2004;45:42–6. doi: 10.1111/j.1440-0960.2004.00029.x. [DOI] [PubMed] [Google Scholar]
- 6.Topar G, Zelger B, Schmuth M, Romani N, Thaler J, Sepp N. Granulomatous slack skin: A distinct disorder or a variant of mycosis fungoides? Acta Derm Venereol. 2001;81:42–4. doi: 10.1080/00015550119980. [DOI] [PubMed] [Google Scholar]
- 7.Salehi M, Azimi Z, Fatemi F, Rajabi P, Kazemi M, Amini G. Incidence rate of mycosis fungoides in Isfahan (Iran) J Dermatol. 2010;37:703–7. doi: 10.1111/j.1346-8138.2010.00899.x. [DOI] [PubMed] [Google Scholar]
- 8.Neuhaus IM, Ramos-Caro FA, Hassanein AM. Hypopigmented mycosis fungoides in childhood and adolescence. Pediatr Dermatol. 2000;17:403–6. doi: 10.1046/j.1525-1470.2000.017005403.x. [DOI] [PubMed] [Google Scholar]
- 9.Das JK, Sengupta S, Gangopadhyay AK. Vitiligo-like lesions of mycosis fungoides coexisting with large plaque parapsoriasis: An association or a spectrum? Indian J Dermatol. 2006;51:120–2. [Google Scholar]


