Abstract
A 40-year-old male human immunodeficiency virus (HIV) -positive patient on highly active antiretroviral therapy (HAART) developed bilateral cervical lymphadenopathy with fine needle aspiration cytology (FNAC) showing yeast cells of Penicillium marneffei. The adenopathy disappeared after 9 months of itraconazole therapy at a dose of 200 mg/day. Seven years later and 2 days following second-line HAART, the patient presented with generalized papulonodules and ulceronecrotic lesions. Biopsy of the skin lesion revealed plenty of yeast forms dividing by binary fission morphologically resembling Penicillium marneffei. Significant improvement was observed at 2 weeks of starting itraconazole 400 mg/day. After 3 months, the dose was reduced to 200 mg/day and advised to continue for 6 months. Penicillosis presenting initially in the form of cervical adenopathy and later, developing typical skin lesions rapidly progressing to ulcerative and necrotic erosions may be due to continued immunosuppression followed by immune reconstitution inflammatory syndrome (IRIS).
Keywords: Highly active antiretroviral therapy, immune reconstitution inflammatory syndrome penicillium marneffei, relapse, ulceronecrotic
What was known?
Umbilicated papulonodular lesions of penicillosis.
Introduction
Penicillium marneffei is a fungal pathogen that causes penicillosis in both healthy and immunocompromised patients. Though earlier confined to Southeast Asia, particularly Thailand, South China, and Vietnam, P. marneffei infections have also been reported in Europe, the United States, and in other Asian countries.[1] Most patients of penicillosis present with a chronic course of fever, lymphadenopathy, hepatosplenomegaly, and cutaneous lesions. The only known nonhuman host of P. marneffei is the bamboo rat.[2] In humans, individuals with deficient T-helper cells, namely, patients with human immunodeficiency virus (HIV) infection or acquired immunodeficiency syndrome (AIDS), are prone to the infection. Most of these patients have a cluster of differentiation (CD) 4+ count less than 100 cells/cu mm and yet have to be treated with highly active antiretroviral therapy (HAART). The relapse rate of penicillosis after successful treatment was reported to be between 4% and 50%.[3]
Case Report
A 40-year-old male HIV-positive patient on second-line HAART was admitted in the male Dermatology ward, Regional Institute of Medical Sciences, Imphal in April 2010 with multiple skin lesions over the body of 45-day duration. He developed 2-3 skin-colored asymptomatic papules over the tip of the nose, which rapidly progressed in 2 days following second-line HAART and became generalized in about 10 days. The lesions became eroded, crusted, and turned brown–black in color. There was a history of generalized weakness, loss of appetite, weight loss, and mild productive cough off and on. There was no history of fever. He gave a history of taking itraconazole 200 mg daily for 9 months for a swelling in his neck, which was diagnosed as penicillosis by fine needle aspiration cytology (FNAC) in January 2003. Reportedly, there were no skin eruptions or any other complaints besides his neck swelling at that time. He was an intravenous drug abuser for 9 years and his HIV-positive status was known in 2001, for which first-line HAART was started with zidovudine, lamivudine, and nevirapine; later, efavirenz was substituted for nevirapine as he was on antitubercular therapy (ATT) for tubercular lymphadenitis. Second-line HAART was started since February 4, 2010, with ritonavir, tenofovir, lamivudine, and atazanavir. On examination, the patient was emaciated with mild pallor. The liver was palpable 6 cm below the right costal margin and was firm and tender. Cutaneous examination revealed papulonodular lesions, most with crusted central umbilication, and ulceronecrotic lesions, some hemorrhagic, 2-3 cm in size, over the face, back, and upper extremities [Figures 1a and b]. Two erosions 2-3 cm were also present in the soft palate. The palms, soles, and the genitals were also involved. The genital lesions consisted of a punched-out ulcer 1.5-2 cm over the prepuce and an umbilicated nodule with central necrosis over the scrotum. There was no lymphadenopathy. The patient was diagnosed as a case of ulceronecrotic penicillosis. Investigations showed hemoglobin 8 g%, total leucocyte count 8570 cells/cu mm, differential count with neutrophls 89%, lymphocytes 8%, monocytes 2%, eosinophils 1%, platelet count of 2.06 lac/cu mm, erythrocyte sedimentation rate of 55 mm/1st hour. Peripheral blood smear showed normocytic normochromic with a few polychromatic forms, absolute neutrophilia, and adequate platelets. Other routine investigations including chest X-ray were normal; Venereal Disease Research Laboratory (VDRL) test was nonreactive. CD4+ count was 10 cells/cu mm on June 21, 2002, 284 cells/cu mm on March 28, 2003, and 57 cells/cu mm on December 5, 2009. Viral load was 130,000 cells/mL on October 30, 2009, and 389,000 cells/mL 2 months later. Skin biopsy from a papulonodular lesion showed the dermis displaying well-formed epithelioid granulomas with areas of suppuration and dense lymphohistiocytic infiltration with many yeast forms dividing by binary fission, morphologically resembling Penicillium marneffei [Figure 2]. The patient was started on itraconazole 400 mg/day in two divided doses. HAART was continued. Significant clinical improvement was noted at 2 weeks of therapy, and complete resolution of the skin lesions with scarring at a few sites was observed at a 3-month follow-up [Figure 3]. Itraconazole was tapered to 200 mg/day and given for another 6 months. His CD4 count of 140 cells/cu mm on admission had increased to 300 cells/cu mm after 6 months, and 365 cells/cu mm and viral load 1090 1 year later. There was no relapse at 34 months [Figure 4].
Figure 1.

(a) Generalized papulonodular lesions with central umbilication, (b) Ulceronecrotic lesions on the face
Figure 2.
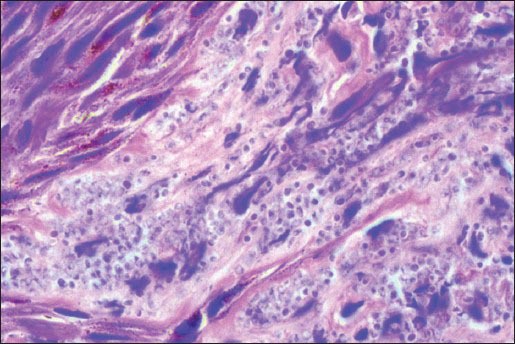
Microphotograph of skin biopsy showing plenty of yeast cells dividing by binary fission resembling Penicillium marneffei (H and E, ×100)
Figure 3.

At 3-month follow-up showing complete clearance of lesions leaving atrophic scars
Figure 4.

At 34-month follow-up
Discussion
Penicillosis has been associated with living in rural areas and with predisposing factors in human hosts, such as cell-mediated immunodeficiency caused by lymphoproliferative disorders, corticosteroid treatment, and, most importantly, HIV infection.[4] It may be confused with histoplasmosis, leishmaniasis, molluscum contagiosum, and other diseases. Diagnosis is confirmed by fungal culture or histopathology.[5] It usually causes an invasive disseminated disease, characterized in AIDS patients by a more rapid onset and more severe symptoms.[4] Penicillosis is mostly seen in late HIV infection with CD4+ count less than 100/uL.[6] The mortality rate of untreated penicillosis is 100% in AIDS patients.[4] In patients not already on HAART, immune reconstitution inflammatory syndrome (IRIS) may develop after starting HAART.[6] In our case, the lesions rapidly became generalized and worsened just after starting second-line HAART. This may be due to continued immune suppression followed by IRIS. Itraconazole remains the drug of choice as shown by its effectiveness in our case. The present case highlights another facet of penicillosis that can occur in immunocompromised patients.
What is new?
Generalized ulceronecrotic and hemorrhagic lesions not described before. Itraconazole may be used as the first drug of choice as documented by our case.
Footnotes
Source of support: Nil
Conflict of Interest: Nil.
References
- 1.Burns T, Breathnach S, Cox N, Griffiths C. Penicillosis. In: Burns T, Breathnach S, Cox N, Griffiths C, editors. Rook's Textbook of Dermatology. 8th ed. Vol. 2. UK: Wiley Blackwell; 2010. pp. 36.88–9. [Google Scholar]
- 2.Plongla R, Leethong P, Asavametha K, Chaindamporn A, Saunkratay CH. Penicillosis marneffei infection in Non-HIV-infected patients. J Infect Dis Antimicrob Agents. 2011;28:71–6. [Google Scholar]
- 3.Yap FB, Thevarajah S, Asmah J. Penicillium marneffei infection in an African man. Dermatol Online J. 2010;16:2. [PubMed] [Google Scholar]
- 4.Viviani MA, Tortorani AM. Penicillium Marneffei. In: Collier L, Balows A, Sussman M, Ajello L, Hay RJ, editors. Topley and Wilson's Microbiology and Microbial Infection. 9th ed. Vol. 4. New York: Arnold Publishing; 1998. pp. 409–19. Medical Mycology. [Google Scholar]
- 5.Hien TV, Loc PP, Hoa NT, Duong NM, Quang VM, McNeil MM, et al. First Cases of Disseminated Penicilliosis Marneffei Infection among Patients with Acquired Immunodeficiency Syndrome in Vietnam. Clin Infect Dis. 2001;32:e78–80. doi: 10.1086/318703. [DOI] [PubMed] [Google Scholar]
- 6.Wong SY, Wong KF. Penicillium marneffei infection in AIDS. Patholog Res Int 2011. 2011 doi: 10.4061/2011/764293. 764293. [DOI] [PMC free article] [PubMed] [Google Scholar]


