Abstract
Familial atypical multiple mole melanoma syndrome (FAMMMS) is an autosomal dominant genodermatosis characterized by multiple melanocytic nevi, usually more than 50, and a family history of melanoma. It is known to be associated with carcinoma of pancreas and other malignancies involving gastrointestinal tract, breast, lung, larynx, and skin in the kindred. There is no published report of FAMMMS in dark-skinned individuals. We report a case of FAMMMS in a dark-skinned adult Indian male, who had multiple extensive nevi all over the body and oral mucosa; associated with malignant melanoma, squamous cell carcinoma (Marjolin's ulcer), and carcinoma of pancreas. His father had died of carcinoma of lung and his sister had a partial phenotypic expression. The clinical presentation of the case is discussed with review of literature.
Keywords: Atypical nevi, familial atypical multiple mole melanoma syndrome, familial atypical multiple mole melanoma-pancreatic cancer, multiple skin malignancies
What was known?
Familial Atypical Multiple Mole Melanoma syndrome (FAMMM syndrome) is an autosomal dominant disorder characterized by the presence of multiple large moles of variable size and color with pigmentary leakage, associated with an increased incidence of malignant melanoma, pancreatic carcinoma, and other visceral malignancies.
Introduction
Norris in 1820 reported the first case of what is now recognized as Familial atypical multiple mole melanoma syndrome (FAMMMS). He described a case of 59-year-old man with melanoma, a high total body mole count, and family history of the same.[1] Lynch and Krush reported an association between multiple nevi, melanoma, and pancreatic cancer. Lynch et al.,[2] proposed the term FAMMMS to the syndrome of “malignant melanoma in association with a distinguishing cutaneous phenotype characterized by multiple large moles, irregular in shape, colored reddish-brown to pink, with evidence of pigmentary leakage, and an apparent autosomal dominant mode of inheritance.” Several studies[3,4,5,6,7,8,9] subsequently reported the autosomal dominant mode of inheritance with variable expressivity and reduced penetrance. Lynch later proposed the term FAMMM-pancreatic cancer (PC) for those cases associated with pancreatic cancer. Whereas atypical moles are more common in people of northern European Celtic background, they are rare in black, Asian, or Middle Eastern populations.[10] Hence, there is no published report of FAMMMS in dark-skinned individuals. We report here a case of FAMMMS in an adult Indian male, with extensive nevi affecting the body and oral mucosa with established skin malignancies and carcinoma of pancreas.
Case Report
A 42-year-old man presented with a rapidly proliferating painless growth on the lateral aspect of right thigh over 4 months duration [Figure 1]. He had a 4 × 5 cm irregular, brownish, proliferative growth arising from the skin, free of underlying muscles. There were two right inguinal lymph nodes less than 1cm size. Another ulcerative growth was found over the medial malleolus on the left leg with raised edges at the site of old burns scar.[Figure 2] Patient had more than 100 nevi all over the body and oral cavity brown-black in color, with irregular borders and variegated appearance [Figures 3 and 4]. There was extensive actinic damage of the scalp and facial skin. FAMMMS was clinically suspected as the patient had multiple atypical moles on the skin and mucosa along with two distinct proliferative skin malignancies.
Figure 1.

Amelanotic melanoma on lateral aspect of thigh
Figure 2.

Marjolin's ulcer above medial malleolus
Figure 3.

Front of torso showing multiple moles
Figure 4.

Lateral view of head and neck showing multiple moles
Otorhinolaryngological examination showed a pigmented naevus of right vocal cord. The punch biopsy of the first growth showed amelanotic melanoma (AM) [Figure 5] and the four-quadrant biopsy of the left leg ulcer showed squamous cell carcinoma (SCC). Multiple skin biopsies showed features of atypical nevi. Ophthalmic examination, abdominal ultrasonography, and chest X-ray were normal. Contrast-enhanced computed tomography (CT) scan of the abdomen during this admission did not show any pancreatic mass. Magnetic resonance imaging scan of the brain was normal.
Figure 5.
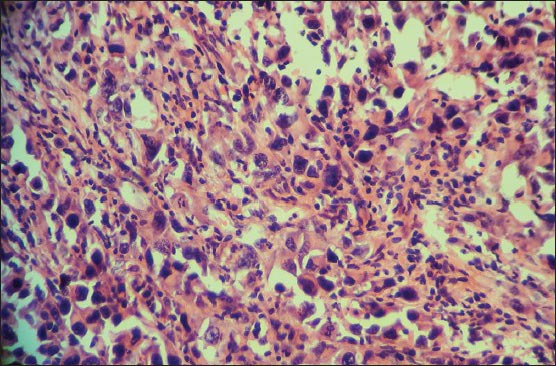
Microphotograph of hematoxylin and eosin-stained section showing tumor cells with epithelioid morphology having plenty, pink cytoplasm, hyperchromatic nuclei, and prominent nucleoli with increased mitotic activity. Cells lacked melanin pigment. Original magnification: ×400
Patient's father had died of carcinoma of lung at the age of 40 years. Patient's sister was examined and found to have actinic damage to the scalp resulting in significant alopecia, but did not have any atypical nevi. Patient was unmarried and had no children.
The patient was advised wide local excision of both the AM and SCC with right inguinal block dissection. He refused all treatment and returned 5 months later with a secondarily infected fungating AM of size 10 × 8 cm, enlarged inguinal lymph nodes, pleural effusion, and lung metastases. The SCC on the left leg had become adherent to the bone. Wide local excision of the infected AM was done for palliation as he did not want any further treatment. He developed obstructive jaundice 2 months later and a contrast-enhanced CT scan of the abdomen showed locally advanced carcinoma of pancreas of the head and body. He underwent stenting of the common bile duct for relief of obstructive jaundice.
Discussion
Atypical moles are more common in people of northern European Celtic background. All published studies about FAMMMS involved white-skinned population. FAMMMS has not been reported in dark-skinned individuals. A PubMed search using the terms “FAMMMS” and “blacks”/“Asian” did not yield any published report. This may be the first reported case of FAMMMS from India.
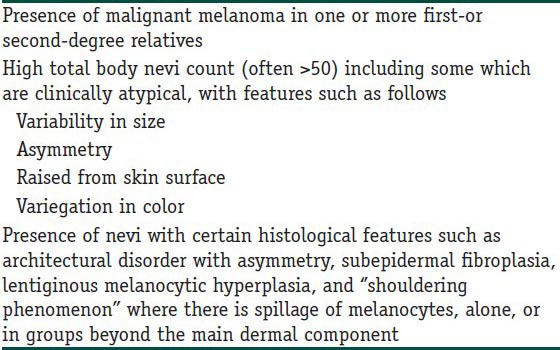
Presently, the accepted diagnostic criteria[8,11] for FAMMMS are listed in Table 1. Identification of FAMMMS is difficult due to the heterogeneity in the cutaneous phenotypes and the spectrum of cancer presentation.[1,3,4,5] Some members of the FAMMMS kindred may only have atypical nevi, whereas others may harbor the mutation with no cutaneous manifestations but later on develop a malignancy associated with FAMMMS. Our patient had more than 100 nevi all over the body and mucosa, of which many were atypical nevi with histological confirmation after biopsy. He had multiple skin malignancies such as melanoma, SCC, and carcinoma of pancreas. There was a significant family history as his father had died of carcinoma of lung at the age of 40 years. The extensive actinic damage to the scalp and face along with alopecia, suggested an incomplete phenotypic expression of the trait in the patient's sister, consequent to increased susceptibility to ultraviolet (UV) radiation in this familial disorder.[12] Fibroblasts in FAMMMS afflicted have an unknown mechanism which enhances tyrosinase expression by UVB irradiation. The resulting increase in melanin synthesis affects the cytotoxicity of UVB to fibroblasts in FAMMMS.[13]
Table 1.
Diagnostic criteria for familial atypical multiple mole melanoma syndrome (Adapted from Eckerle Mize et al.)
Various studies have established the autosomal dominant mode of inheritance of FAMMMS. Two high-risk melanoma susceptibility genes, CDKN2A (cyclin-dependent kinase inhibitor 2A) and CDK4 (cyclin-dependent kinase 4) have been identified in 20-40% of familial melanomas.[6,7,8] CDKN2A is a tumorsuppressor gene located on Ch9p21, involved in cell cycle control maintenance. Germ line mutation in CDKN2A is transmitted by autosomal-dominant inheritance with variable penetrance and expression. Germ-line mutations of CDK4 are rare.
The significance of atypical moles in the pathogenesis of melanoma has not been fully investigated. The opinions of dermatologists and oncologists on the subject are divided. One group supports the theory of treating atypical moles as “premalignant states,” and the other defends the hypothesis of atypical moles as markers of increased risk of melanoma development de novo.[11] Persons with FAMMMS have a markedly increased risk of developing melanoma with a lifetime risk as high as 100%.[14] FAMMMS is also associated with five fold increased incidence of other malignancies of the lung, skin, larynx, breast, gastrointestinal tract, and eyes.[7,9] Pancreatic cancer is seen in 11-60% of the afflicted family members depending on the type of mutation.[1]
As melanoma and other malignancies can occur in the families affected by FAMMMS, surveillance is necessary for early diagnosis.[11] Recognition of families afflicted by this syndrome will help in early diagnosis of malignancies and their effective treatment in the family members. Hence, it is necessary to look out for atypical moles in patients diagnosed with pancreatic cancer and for solid tumor cancers, including pancreatic cancer when a patient presents with multiple atypical moles.
Conclusion
FAMMMS is a rare autosomal dominant disorder and is being reported for the first time in India. It poses life-time risk of melanomas, pancreatic carcinoma, and other malignancies in the affected individual and kindred. Surveillance is the key for early diagnosis and management of these malignancies. Patients presenting with multiple atypical moles should be kept under surveillance for the development of pancreatic cancer and other solid tumors. Similarly, presence of any atypical moles should be looked for in patients with pancreatic cancer to recognize FAMMMS.
What is new?
Familial Atypical Multiple Mole Melanoma syndrome (FAMMM syndrome) is being reported for the first time in India. Surveillance is the key for its management as it poses life-time risk of melanomas and other malignancies in the affected person.
Footnotes
Source of support: Nil
Conflict of Interest: Nil.
References
- 1.Lynch HT, Krush AJ. Hereditary and malignant melanoma: Implications for early cancer detection. Can Med Assoc J. 1968;99:17–21. [PMC free article] [PubMed] [Google Scholar]
- 2.Lynch HT, Frichot BC, 3rd, Lynch JF. Familial atypical multiple mole-melanoma syndrome. J Med Genet. 1978;15:352–356. doi: 10.1136/jmg.15.5.352. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Lynch HT, Brand RE, Hogg D, Deters CA, Fusaro RM, Lynch JF, et al. Phenotypic variation in eight extended CDKN2A germline mutation familial atypical multiple mole melanoma-pancreatic carcinoma-prone families: The familial atypical mole melanoma-pancreatic carcinoma syndrome. Cancer. 2002;94:84–96. doi: 10.1002/cncr.10159. [DOI] [PubMed] [Google Scholar]
- 4.Rulyak SJ, Brentnall TA, Lynch HT, Austin MA. Characterization of the neoplastic phenotype in the familial atypical multiple-mole melanoma-pancreatic carcinoma syndrome. Cancer. 2003;98:798–804. doi: 10.1002/cncr.11562. [DOI] [PubMed] [Google Scholar]
- 5.Czajkowski R, Placek W, Drewa G, Czajkowska A, Uchańska G. FAMMM syndrome: Pathogenesis and management. Dermatol Surg. 2004;30:291–6. doi: 10.1111/j.1524-4725.2004.30088.x. [DOI] [PubMed] [Google Scholar]
- 6.NIH Consensus Conference. Diagnosis and treatment of early melanoma. JAMA. 1992;268:1314–9. doi: 10.1001/jama.1992.03490100112037. [DOI] [PubMed] [Google Scholar]
- 7.Måsbäck A, Olsson H, Westerdahl J, Sandberg T, Borg A, Jonsson N, et al. Clinical and histopathological features of malignant melanoma in germline CDKN2A mutation families. Melanoma Res. 2002;12:549–57. doi: 10.1097/00008390-200212000-00004. [DOI] [PubMed] [Google Scholar]
- 8.Eckerle Mize D, Bishop M, Resse E, Sluzevich J. Riegert-Johnson DL, Boardman LA, Hefferon T, Roberts M, et al., editors. Familial atypical multiple mole melanoma syndrome. Cancer Syndromes. Bethesda: National Center for Biotechnology Information (US) 2009. [Last accessed date on 2012 April 2]. Available from: http://www.ncbi.nlm.nih.gov/books/NBK7030/ [PubMed]
- 9.Kefford RF, Newton Bishop JA, Bergman W, Tucker MA. Counseling and DNA testing for individuals perceived to be genetically predisposed to melanoma: A consensus statement of the Melanoma Genetics Consortium. J ClinOncol. 1999;17:3245–51. doi: 10.1200/JCO.1999.17.10.3245. [DOI] [PubMed] [Google Scholar]
- 10.Goldstein AM, Struewing JP, Chidambaram A, Fraser MC, Tucker MA. Genotype-phenotype relationships in U.S. Melanoma-prone families with CDKN2A and CDK4 mutations. J Natl Cancer Inst. 2000;92:1006–10. doi: 10.1093/jnci/92.12.1006. [DOI] [PubMed] [Google Scholar]
- 11.Greene MH, Tucker MA, Clark WH, Jr, Kraemer KH, Elder DE, Fraser MC. Hereditary melanoma and the dysplastic nevus syndrome: The risk of cancers other than melanoma. J Am Acad Dermatol. 1987;16:792–7. doi: 10.1016/s0190-9622(87)70103-0. [DOI] [PubMed] [Google Scholar]
- 12.Wenner KA, Acker SM, Shidham VB, Sloan SB, Travers R, Vinson R, et al. Elston DM, editor. Atypical Mole (Dysplastic Nevus) Emedicine Medscape Reference. 2012. [Last accessed date on 2012 April 2]. Available from: http://www.emedicine.medscape.com/article/1056283-overview .
- 13.Yoneta A, Yamashita T, Jin HY, Kondo S, Jimbow K. Ectopic expression of tyrosinase increases melanin synthesis and cell death following UVB irradiation in fibroblasts from familial atypical multiple mole and melanoma (FAMMM) patients. Melanoma Res. 2004;14:387–94. doi: 10.1097/00008390-200410000-00009. [DOI] [PubMed] [Google Scholar]
- 14.Kanzler MH, Swetter SM. Malignant melanoma. J Am Acad Dermatol. 2003;48:780–3. doi: 10.1067/mjd.2003.284. [DOI] [PubMed] [Google Scholar]


