Abstract
Background:
Treatment of end-stage ankle osteoarthritis remains challenging, especially in young patients. Initial reports have shown early benefits of joint distraction for the treatment of ankle osteoarthritis. We report the five to ten-year results of a previously described patient cohort following ankle distraction surgery.
Methods:
All thirty-six patients who had undergone ankle distraction surgery between December 2002 and October 2006 were contacted. Patients were evaluated by a clinical investigator and completed the Ankle Osteoarthritis Scale (AOS) and Short Form-36 (SF-36) surveys. Radiographs as well as computed tomography and magnetic resonance imaging scans of the ankles were obtained at the follow-up visits.
Results:
Twenty-nine patients (81%) were followed for a minimum of five years (mean and standard deviation, 8.3 ± 2.2 years). Sixteen (55%) of the twenty-nine patients still had the native ankle joint whereas thirteen patients (45%) had undergone either ankle arthrodesis or total ankle arthroplasty. Positive predictors of ankle survival included a better AOS score at two years (hazard ratio [HR] = 0.048, 95% confidence interval [CI] = 0.0028 to 0.84, p = 0.04), older age at surgery (HR = 0.91, 95% CI = 0.83 to 0.99, p = 0.04), and fixed distraction (HR = 0.094, 95% CI = 0.017 to 0.525, p < 0.01). Radiographs and advanced imaging revealed progression of ankle osteoarthritis at the time of final follow-up.
Conclusions:
Ankle function following joint distraction declines over time. Patients should be well informed of the commitment that they must make during the treatment period as well as the long-term results after surgery.
Level of Evidence:
Therapeutic Level IV. See Instructions for Authors for a complete description of levels of evidence.
Ankle osteoarthritis is a debilitating condition with an increasing prevalence in the U.S. Current estimates of the burden of ankle osteoarthritis in the U.S. suggest that there are more than 50,000 new cases annually1. The consequences of ankle osteoarthritis include not only poor ankle function but also poor general health status2. The physical disability associated with end-stage ankle osteoarthritis is equivalent to that associated with end-stage hip osteoarthritis3, end-stage kidney disease, or congestive heart failure4.
Ankle osteoarthritis is more frequently of posttraumatic origin (70% to 80%) than is osteoarthritis of the hip or knee1. Despite the best current efforts at fracture treatment, posttraumatic osteoarthritis develops in 12% of patients after lower-extremity trauma1. A study of posttraumatic ankle osteoarthritis showed the condition to be attributable to a previous rotational ankle fracture in 37.0% of cases, recurrent sprains in 14.6%, a single sprain in 13.7%, a pilon fracture in 9.0%, a tibial shaft fracture in 8.5%, and an osteochondral lesion of the talus in 4.7%5.
Ankle osteoarthritis mostly affects a younger population, which makes treatment options challenging. Ankle arthrodesis, which has been considered the gold-standard surgical treatment because of its fairly predictable results, can lead to alterations in gait, loss of function, and adjacent joint arthritis6-9. Total ankle arthroplasty is usually reserved for older, less active individuals10. Because of the notable limitations of joint-sacrificing surgical procedures, much interest has been paid recently to joint-preserving surgical options11. Short-term results in Europe and the U.S., including those at our institution, have been encouraging12-21. Ankle distraction is a way to treat symptoms while keeping arthrodesis and total ankle arthroplasty as viable options if the distraction ultimately fails. We prospectively followed a cohort of patients who had undergone ankle distraction and report here the clinical results at five to ten years postoperatively.
Materials and Methods
Thirty-six patients underwent ankle distraction surgery between December 2002 and October 2006 in a prospective clinical trial12 (Figs. 1-A and 1-B). Inclusion criteria included (1) symptomatic isolated, unilateral ankle osteoarthritis with a Kellgren-Lawrence grade of 3 or 4; (2) skeletal maturity and an age no greater than sixty years old; (3) failure of more than a year of nonsurgical treatment, including three months of continuous treatment with nonsteroidal anti-inflammatory drugs and three months of unloading treatment; and (4) an ability to maintain the extremity non-weight-bearing by using ambulatory aids. Exclusion criteria included inflammatory or crystal arthritis, diabetes, severe systemic illness, fibromyalgia, peripheral neuropathy, reflex sympathetic dystrophy, a previous infection of the ankle, a neuroarthropathic ankle, other symptomatic joints of the ipsilateral lower extremity, contralateral ankle osteoarthritis, ankle or hindfoot malalignment, living >300 mi (>483 km) from our institution, or current alcohol or drug abuse. Patients were randomized into two arms of treatment: fixed distraction and motion distraction. All patients were contacted via a letter of recruitment and telephone by one of the investigators. Verbal and written explanations of the study procedures and the potential benefits and risks were provided. Written, witnessed consent was obtained from all subjects with use of approved forms under institutional review board approval (#201204749).
Fig. 1-A.

Ankle distractor.
Fig. 1-B.
Radiographs made before and after distraction.
A history was recorded and a physical examination was performed by a physician clinical investigator. Patients were specifically asked about their overall experience with the ankle distraction, any subsequent ankle-specific treatments, and the current state of their ankle. We asked about medication requirements; the need for walking aids, special shoes, or shoe inserts; and restrictions of daily activities and/or work. Examination included evaluation of standing alignment and the range of motion of both ankles and subtalar joints. Each patient independently completed the self-assessment Ankle Osteoarthritis Scale (AOS) and the Medical Outcomes Study 36-Item Short-Form Health Survey (SF-36) (version 2). Patients with an intact native ankle underwent imaging, whenever possible, with ankle radiographs, computed tomography (CT) scans, and/or magnetic resonance imaging (MRI) scans. Patients who could not travel to the University of Iowa were given the option of receiving and returning the surveys by mail.
The surgical procedure and postoperative protocol were previously described12.
Functional Outcomes
The primary outcome was the status of the ankle joint (preserved or converted to a total ankle arthroplasty or an arthrodesis) at the time of follow-up. The functional results were evaluated with the AOS and the Physical Component Summary (PCS) of the SF-3622.
Imaging Studies
Radiographs and CT and MRI scans of the ankle were obtained at the follow-up visits. Ankle CT scans (SOMATOM Emotion 6 or Sensation 16; Siemens) to analyze joint space width were obtained at baseline and at the two-year and five to ten-year follow-up visits after treatment. A three-dimensional volumetric isotropic turbo spin-echo acquisition pulse sequence (SPACE; Siemens) was applied to acquire T2-weighted images of the entire joint. Functional assessment of cartilage was performed with quantitative T1ρ and T2 mapping.
Statistical Analysis
A significance level of α = 0.05 was used for all statistical analyses. Student t tests were used to compare the functional results between the patients with a preserved ankle joint and those who required conversion to total ankle arthroplasty or ankle arthrodesis. A Cox proportional hazards model was built to evaluate the association and strength of independent predictors of the time until ankle failure (conversion to total ankle arthroplasty or ankle arthrodesis). We included only patients with at least five years of follow-up or who had already had ankle failure. The independent predictor variables were (1) the treatment type (fixed distraction versus motion distraction), (2) the AOS score at two years following the ankle distraction, (3) the improvement in the AOS score at two years following ankle distraction, defined as the difference between the preoperative and two-year follow-up scores, and (4) the age at surgery.
Source of Funding
This project was funded by a research grant from AO North America. The original study12 was funded by Grant P50AR048939 from the National Institutes of Health, U.S. Department of Health & Human Services.
Results
Patients
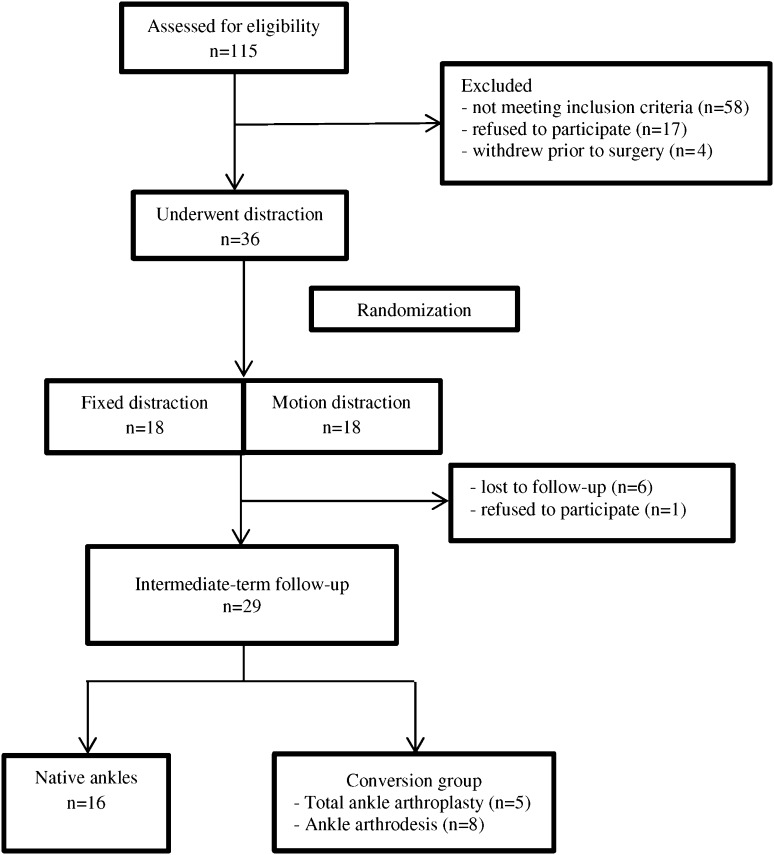
From December 2002 to October 2006, 115 patients were screened and forty entered into the study. Four patients who enrolled in the study withdrew prior to having surgery. A total of thirty-six patients underwent ankle distraction (Fig. 2). Demographic data, including patient age, sex, and body mass index, are shown in Table I.
Fig. 2.
Flowchart illustrating patient recruitment and the follow-up process.
TABLE I.
Demographic Characteristics (N = 36)
| Variable | |
| Age at surgery* (yr) | 41.5 ± 9.1 (18-59) |
| Male:female (no.) | 2:1 |
| Body mass index* (kg/m2) | 29.9 ± 4.7 (23.1-39.9) |
The values are given as the mean and standard deviation with the range in parentheses.
Intermediate-Term Survival
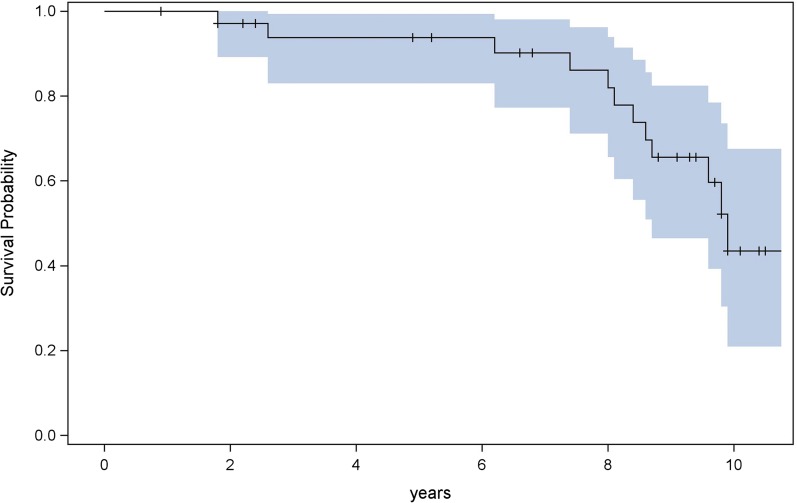
The primary outcome, defined as ankle status (preserved ankle joint or conversion to total ankle replacement or ankle arthrodesis), was available for twenty-nine patients (81%) at a minimum of five years (mean [and standard deviation], 8.3 ± 2.2 years). One patient declined to participate and six patients did not respond to our recruitment letter or telephone calls (Fig. 2). Sixteen (55%) of the twenty-nine patients still had the native ankle joint, and thirteen patients (45%) had had either ankle arthrodesis (eight patients; mean age at conversion, 42 ± 7.5 years) or total ankle arthroplasty (five patients; mean age at conversion, 58 ± 6.5 years) (Fig. 3). Of the thirteen ankle arthrodeses or total ankle arthroplasties, two were performed within one year after the ankle distraction; three, in the second year; one, in the third year; one, in the fifth year; three, in the sixth year; two, in the seventh year; and one, in the eighth year. Complete functional scores (AOS and SF-36) were available for twenty-two patients, including five who completed the surveys remotely without a return visit.
Fig. 3.
Kaplan-Meier survivorship curve with 95% confidence intervals for the end point of total ankle arthroplasty or ankle arthrodesis.
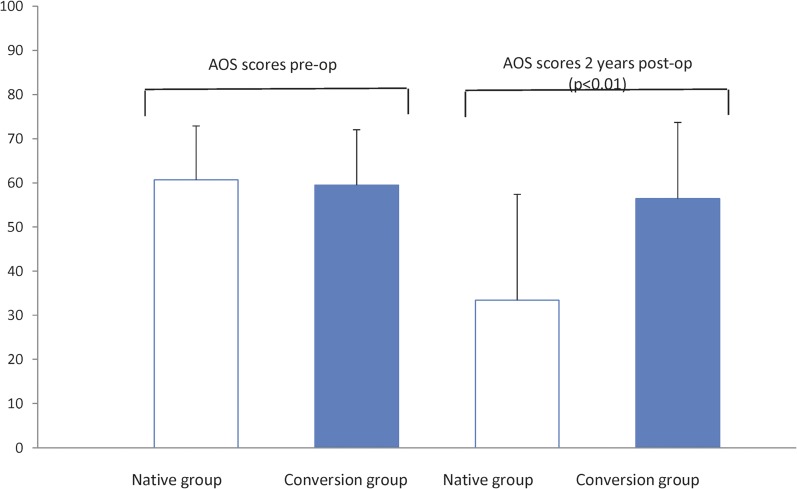
The Cox hazards model showed the treatment type (fixed distraction versus motion distraction), AOS score at two years following distraction, and age at the time of distraction to be predictive of the time until ankle failure (conversion to total ankle arthroplasty or ankle arthrodesis). Positive predictors of intermediate-term survival were fixed distraction, an AOS score of ≤42 (a lower AOS score means a better functional score) at two years following distraction, and an older age at the time of surgery (Table II). Age was a continuous variable in our analysis. Older patients had a lower failure rate compared with those who were one year younger (hazard ratio [HR] = 0.91, p = 0.04). Patients with an AOS score of ≤42 at two years were more likely to still have the native ankle at five to ten years (HR = 0.048, p = 0.04). Compared with patients who still had the native joint, patients who ultimately required ankle arthrodesis or total ankle arthroplasty showed early signs of distraction failure at two years. They demonstrated worse functional scores at two years compared with the patients whose ankle was intact at five to ten years (mean AOS score of 56.4 ± 17.2 compared with 34.4 ± 24.0, p < 0.01). There was no significant difference between the AOS scores of the two groups prior to surgery (60.7 ± 12.2 for the native-ankle group and 59.5 ± 12.5 for the conversion group, p = 0.80) (Fig. 4).
TABLE II.
Cox Proportional Hazards Model for the Time to Failure
| HR (95% CI) | P Value | |
| Fixed distraction vs. motion | 0.094 (0.017-0.525) | <0.01 |
| AOS score at 2 yr (≤42 vs. >42) | 0.048 (0.0028-0.84) | 0.04 |
| Improvement of AOS score at 2 yr | 1.75 (0.07-44.02) | 0.73 |
| Age at distraction | 0.91 (0.83-0.99) | 0.04 |
Fig. 4.
Comparison of AOS scores between the native-ankle group and the ankle-conversion group. Patients who eventually had ankle failure demonstrated an early decline in the AOS score at two years.
At the time of intermediate-term follow-up, seven of twelve patients with a native ankle reported better PCS and AOS scores compared with their preoperative scores. After conversion to total ankle arthroplasty or ankle arthrodesis, six of ten patients reported better PCS and AOS scores compared with their predistraction scores. At five to ten years, the group with a native ankle and the group that underwent conversion to ankle arthrodesis or total ankle arthroplasty reported similar patient-reported outcomes (mean PCS scores of 32.8 ± 9.5 and 37.8 ± 11.8 for the native-ankle and conversion groups, respectively, and mean AOS scores of 59.8 ± 20.7 and 42.5 ± 35.3, respectively).
Imaging Findings
At five to ten years, imaging studies were obtained for ten of the sixteen patients with a preserved ankle joint. Eight had radiographs and CTs, and eight had radiographs and MRIs. (Seven had all three studies.) All ten patients had radiographs. Ankle images consistently demonstrated subchondral sclerosis, osteophyte formation, and osseous deformity consistent with Kellgren-Lawrence grade-3 or 4 ankle osteoarthritis (see Appendix). Despite the uniformly arthritic appearance of the ankles on the radiographs, there was a spectrum of functional scores and patients’ desires to seek further treatment and surgical intervention (see Appendix).
Follow-up CT scans at the time of final follow-up revealed some loss of the benefit seen at two years, with increases in cystic formation and osseous sclerosis consistent with the natural progression of osteoarthritis (see Appendix).
Pin-Site Infection
The most common complication of ankle distraction is pin-site infection. Nineteen of the thirty-six patients in the original study12 had implant-related infections. All resolved with oral and/or intravenous antibiotics and implant removal; none resulted in amputation. All five patients who eventually underwent total ankle arthroplasty had been originally treated for a pin-site infection with no complication from the infection.
Discussion
Treatment of posttraumatic ankle osteoarthritis remains challenging given the relatively young high-demand population that tends to present with this condition. Options include arthrodesis, ankle replacement, osteotomy, allograft replacement, and distraction. Arthrodesis is associated with risks of nonunion, decreased function, progressive degeneration of other joints of the foot, and continued pain6-9. Ankle replacement is associated with risks of loosening, continued pain, and the need for a challenging revision surgery23-28. Supramalleolar osteotomies have less predictable results in patients with more than truly isolated tibiotalar or tibiofibular “gutter” arthritis and can cause secondary deformity of the hindfoot29-31. Tibiotalar allograft transplantation has been fraught with inconsistent outcomes and early failures32-34. The early results of ankle distraction have been encouraging12-21; however, there is a paucity of data on the long-term results of joint distraction.
Our study provided important sobering information for patients who seek joint-preserving surgical treatment. The most predictive factor for intermediate-term ankle survival was the AOS score at two years. If patients did not obtain improvement by two years, it was unlikely that they would eventually benefit from ankle distraction. In comparison, Marijnissen et al. reported that failure tended to occur early in some patients: 17% of the failures occurred within two years and 37%, by five years35. In their regression analysis, the only factor that was predictive of outcome was female sex.
The finding that older age was a positive predictor of intermediate-term outcome may be related to the younger patients having higher expectations and physical demands. Pain relief alone with low-demand activities may be sufficient for older patients. This seemingly paradoxical finding of older patients perceiving better outcomes suggests that, as with most reconstructive surgical procedures, there may be an optimal age window for ankle distraction that needs to be determined with further investigation. Even when the ankle distraction failed to provide long-term pain relief, it offered a joint-preserving alternative that did not preclude more definitive treatment when it was eventually necessary.
In our previous short-term study, we found that motion distraction resulted in significantly better AOS scores than fixed distraction at twenty-six, fifty-two, and 104 weeks12. In the present follow-up study, however, we found that the effect of motion may not be long-term. It is possible that, as is the case with other operations, early motion leads to decreased stiffness and better outcomes early on. Over time, however, as the fixed-distraction group regains motion, the benefit of early motion dwindles. Given the small number of patients in our study, the role of motion in predicting long-term ankle function after distraction cannot be certain without future research. Also, because of our limited number of patients, we were unable to perform analyses to identify other outcome predictors such as comorbidities, smoking, and work status.
Like other long-term studies, our study is limited by the low follow-up rate of a small cohort of patients (81% [twenty-nine] of thirty-six patients). To encourage follow-up, we excluded patients who lived >300 mi (>483 km) from our institution. Our university is a tertiary referral center and has a large catchment area. Unfortunately, several of the patients in our original study moved out of the area or were otherwise unavailable for follow-up. Although the number of patients with imaging was not high, the main results of our studies were ankle survival status (data available for twenty-nine patients) and positive predictors of ankle survival (also available for twenty-nine patients). Thus, we reported an 81% follow-up rate (twenty-nine of thirty-six patients) in the study. Because of the limited number of complete functional scores (twenty-two patients) at five to ten years, we did not perform statistical comparisons of these scores.
One rationale for ankle distraction is that, by delaying the need for joint-sacrificing surgery, distraction minimizes adjacent joint arthritis following ankle arthrodesis and increases implant longevity following total ankle arthroplasty. An interesting observation in this study was the similarity of the patient-reported outcomes at five to ten years between the native-ankle group and the ankle-conversion group. This effect needs more investigation to determine if the outcomes of primary arthrodesis or arthroplasty compare with those of the same procedures following joint distraction.
In our study, all pin-site infections were treated adequately and resulted in no long-term consequences following total ankle arthroplasty in the small subset of patients who had that procedure. Detecting pin-site infections requires high vigilance by both patients and physicians so that treatment can be initiated immediately. We recommend ankle distraction surgery only for patients who demonstrate a willingness to follow instructions and can return for treatment if infection develops. The possibility of this complication highlights the commitment required of both the surgeon and the patient if an ankle distraction is to be performed.
The exact mechanism through which distraction alleviates pain is unclear, but it may have effects on joint proteoglycans15. Analysis of ankle CT scans at two years following ankle distraction suggested that the mechanism may also be related to subchondral bone remodeling within presumably pain-generating cysts36. These effects suggest that indications for ankle distraction may be extended to severe acute fractures. Early intervention with ankle distraction in the acute or subacute setting may allow the ankle joint to remodel and prevent long-term posttraumatic osteoarthritis.
The current investigation is one of the few studies of ankle distraction with greater than five years of follow-up. A previous study in the Netherlands showed a 27% rate of failure at seven years in a cohort of twenty-seven patients, although the authors did not clearly define their inclusion criteria or the degree of preoperative osteoarthritis18. We observed a higher failure rate, with 45% of our patients having undergone a conversion procedure by a mean of 8.3 ± 2.2 years, a finding similar to those in a recent review by Marijnissen et al.35. Although the surgery provided younger patients with the use of their native ankle joint for a few more years while they were in their peak of productivity (mean age at surgery, 41.5 ± 9.1 years), patients should be well informed of the expected outcomes and the commitment of living with the distraction device for three months. Patients who are considering ankle distraction surgery should have a realistic expectation of the long-term results. In our series, approximately half of the patients underwent conversion to total ankle replacement or ankle arthrodesis in less than ten years. The remaining patients (with a preserved native ankle at the time of follow-up) generally reported moderate ankle pain and activity limitations. More research is needed to better understand how to optimize the distraction method as well as to elucidate predictive factors for long-term outcomes in order to improve the treatments of ankle osteoarthritis.
Appendix
Figures showing the spectrum of radiographic findings at the time of follow-up after ankle distraction, T2-weighted fat-saturated MRI and T1ρ mapping revealing cartilage and dense collagen fibers binding water, and progression of ankle arthritis in one patient are available with the online version of this article as a data supplement at jbjs.org.
Footnotes
Investigation performed at the University of Iowa, Iowa City, Iowa
Disclosure: One or more of the authors received payments or services, either directly or indirectly (i.e., via his or her institution), from a third party in support of an aspect of this work. In addition, one or more of the authors, or his or her institution, has had a financial relationship, in the thirty-six months prior to submission of this work, with an entity in the biomedical arena that could be perceived to influence or have the potential to influence what is written in this work. No author has had any other relationships, or has engaged in any other activities, that could be perceived to influence or have the potential to influence what is written in this work. The complete Disclosures of Potential Conflicts of Interest submitted by authors are always provided with the online version of the article.
References
- 1.Brown TD, Johnston RC, Saltzman CL, Marsh JL, Buckwalter JA. Posttraumatic osteoarthritis: a first estimate of incidence, prevalence, and burden of disease. J Orthop Trauma. 2006Nov-Dec;20(10):739-44. [DOI] [PubMed] [Google Scholar]
- 2.Marsh JL, Weigel DP, Dirschl DR. Tibial plafond fractures. How do these ankles function over time? J Bone Joint Surg Am. 2003February;85(2):287-95. [PubMed] [Google Scholar]
- 3.Glazebrook M, Daniels T, Younger A, Foote CJ, Penner M, Wing K, Lau J, Leighton R, Dunbar M. Comparison of health-related quality of life between patients with end-stage ankle and hip arthrosis. J Bone Joint Surg Am. 2008March;90(3):499-505. [DOI] [PubMed] [Google Scholar]
- 4.Saltzman CL, Zimmerman MB, O’Rourke M, Brown TD, Buckwalter JA, Johnston R. Impact of comorbidities on the measurement of health in patients with ankle osteoarthritis. J Bone Joint Surg Am. 2006November;88(11):2366-72. [DOI] [PubMed] [Google Scholar]
- 5.Saltzman CL, Salamon ML, Blanchard GM, Huff T, Hayes A, Buckwalter JA, Amendola A. Epidemiology of ankle arthritis: report of a consecutive series of 639 patients from a tertiary orthopaedic center. Iowa Orthop J. 2005;25:44-6. [PMC free article] [PubMed] [Google Scholar]
- 6.Coester LM, Saltzman CL, Leupold J, Pontarelli W. Long-term results following ankle arthrodesis for post-traumatic arthritis. J Bone Joint Surg Am. 2001February;83(2):219-28. [DOI] [PubMed] [Google Scholar]
- 7.Thomas R, Daniels TR, Parker K. Gait analysis and functional outcomes following ankle arthrodesis for isolated ankle arthritis. J Bone Joint Surg Am. 2006March;88(3):526-35. [DOI] [PubMed] [Google Scholar]
- 8.Mazur JM, Schwartz E, Simon SR. Ankle arthrodesis. Long-term follow-up with gait analysis. J Bone Joint Surg Am. 1979October;61(7):964-75. [PubMed] [Google Scholar]
- 9.Muir DC, Amendola A, Saltzman CL. Long-term outcome of ankle arthrodesis. Foot Ankle Clin. 2002December;7(4):703-8. [DOI] [PubMed] [Google Scholar]
- 10.Guyer AJ, Richardson G. Current concepts review: total ankle arthroplasty. Foot Ankle Int. 2008February;29(2):256-64. [DOI] [PubMed] [Google Scholar]
- 11.Labib SA, Raikin SM, Lau JT, Anderson JG, SooHoo NF, Carette S, Pinney SJ. Joint preservation procedures for ankle arthritis. Foot Ankle Int. 2013July;34(7):1040-7. [DOI] [PubMed] [Google Scholar]
- 12.Saltzman CL, Hillis SL, Stolley MP, Anderson DD, Amendola A. Motion versus fixed distraction of the joint in the treatment of ankle osteoarthritis: a prospective randomized controlled trial. J Bone Joint Surg Am. 2012June6;94(11):961-70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Chiodo CP, McGarvey W. Joint distraction for the treatment of ankle osteoarthritis. Foot Ankle Clin. 2004September;9(3):541-3, ix. [DOI] [PubMed] [Google Scholar]
- 14.Lamm BM, Gourdine-Shaw M. MRI evaluation of ankle distraction: a preliminary report. Clin Podiatr Med Surg. 2009April;26(2):185-91. [DOI] [PubMed] [Google Scholar]
- 15.Marijnissen AC, van Roermund PM, van Melkebeek J, Lafeber FP. Clinical benefit of joint distraction in the treatment of ankle osteoarthritis. Foot Ankle Clin. 2003June;8(2):335-46. [DOI] [PubMed] [Google Scholar]
- 16.Marijnissen AC, Van Roermund PM, Van Melkebeek J, Schenk W, Verbout AJ, Bijlsma JW, Lafeber FP. Clinical benefit of joint distraction in the treatment of severe osteoarthritis of the ankle: proof of concept in an open prospective study and in a randomized controlled study. Arthritis Rheum. 2002November;46(11):2893-902. [DOI] [PubMed] [Google Scholar]
- 17.Marijnissen AC, Vincken KL, Viergever MA, van Roy HL, Van Roermund PM, Lafeber FP, Bijlsma JW. Ankle images digital analysis (AIDA): digital measurement of joint space width and subchondral sclerosis on standard radiographs. Osteoarthritis Cartilage. 2001April;9(3):264-72. [DOI] [PubMed] [Google Scholar]
- 18.Ploegmakers JJ, van Roermund PM, van Melkebeek J, Lammens J, Bijlsma JW, Lafeber FP, Marijnissen AC. Prolonged clinical benefit from joint distraction in the treatment of ankle osteoarthritis. Osteoarthritis Cartilage. 2005July;13(7):582-8. [DOI] [PubMed] [Google Scholar]
- 19.van Roermund PM, Marijnissen AC, Lafeber FP. Joint distraction as an alternative for the treatment of osteoarthritis. Foot Ankle Clin. 2002September;7(3):515-27. [DOI] [PubMed] [Google Scholar]
- 20.van Valburg AA, van Roermund PM, Marijnissen AC, van Melkebeek J, Lammens J, Verbout AJ, Lafeber FP, Bijlsma JW. Joint distraction in treatment of osteoarthritis: a two-year follow-up of the ankle. Osteoarthritis Cartilage. 1999September;7(5):474-9. [DOI] [PubMed] [Google Scholar]
- 21.van Valburg AA, van Roermund PM, Marijnissen AC, Wenting MJ, Verbout AJ, Lafeber FP, Bijlsma JW. Joint distraction in treatment of osteoarthritis (II): effects on cartilage in a canine model. Osteoarthritis Cartilage. 2000January;8(1):1-8. [DOI] [PubMed] [Google Scholar]
- 22.Domsic RT, Saltzman CL. Ankle Osteoarthritis Scale. Foot Ankle Int. 1998July;19(7):466-71. [DOI] [PubMed] [Google Scholar]
- 23.Spirt AA, Assal M, Hansen ST Jr. Complications and failure after total ankle arthroplasty. J Bone Joint Surg Am. 2004June;86(6):1172-8. [DOI] [PubMed] [Google Scholar]
- 24.Glazebrook MA, Arsenault K, Dunbar M. Evidence-based classification of complications in total ankle arthroplasty. Foot Ankle Int. 2009October;30(10):945-9. [DOI] [PubMed] [Google Scholar]
- 25.Haddad SL, Coetzee JC, Estok R, Fahrbach K, Banel D, Nalysnyk L. Intermediate and long-term outcomes of total ankle arthroplasty and ankle arthrodesis. A systematic review of the literature. J Bone Joint Surg Am. 2007September;89(9):1899-905. [DOI] [PubMed] [Google Scholar]
- 26.Daniels TR, Younger AS, Penner M, Wing K, Dryden PJ, Wong H, Glazebrook M. Intermediate-term results of total ankle replacement and ankle arthrodesis: a COFAS multicenter study. J Bone Joint Surg Am. 2014January15;96(2):135-42. [DOI] [PubMed] [Google Scholar]
- 27.Morrey BF, Wiedeman GP Jr. Complications and long-term results of ankle arthrodeses following trauma. J Bone Joint Surg Am. 1980July;62(5):777-84. [PubMed] [Google Scholar]
- 28.Saltzman CL, Amendola A, Anderson R, Coetzee JC, Gall RJ, Haddad SL, Herbst S, Lian G, Sanders RW, Scioli M, Younger AS. Surgeon training and complications in total ankle arthroplasty. Foot Ankle Int. 2003June;24(6):514-8. [DOI] [PubMed] [Google Scholar]
- 29.Takakura Y, Tanaka Y, Kumai T, Tamai S. Low tibial osteotomy for osteoarthritis of the ankle. Results of a new operation in 18 patients. J Bone Joint Surg Br. 1995January;77(1):50-4. [PubMed] [Google Scholar]
- 30.Tanaka Y, Takakura Y, Hayashi K, Taniguchi A, Kumai T, Sugimoto K. Low tibial osteotomy for varus-type osteoarthritis of the ankle. J Bone Joint Surg Br. 2006July;88(7):909-13. [DOI] [PubMed] [Google Scholar]
- 31.Takakura Y, Takaoka T, Tanaka Y, Yajima H, Tamai S. Results of opening-wedge osteotomy for the treatment of a post-traumatic varus deformity of the ankle. J Bone Joint Surg Am. 1998February;80(2):213-8. [DOI] [PubMed] [Google Scholar]
- 32.Bugbee WD, Khanna G, Cavallo M, McCauley JC, Görtz S, Brage ME. Bipolar fresh osteochondral allografting of the tibiotalar joint. J Bone Joint Surg Am. 2013March6;95(5):426-32. [DOI] [PubMed] [Google Scholar]
- 33.Meehan R, McFarlin S, Bugbee W, Brage M. Fresh ankle osteochondral allograft transplantation for tibiotalar joint arthritis. Foot Ankle Int. 2005October;26(10):793-802. [DOI] [PubMed] [Google Scholar]
- 34.Kim CW, Jamali A, Tontz W Jr, Convery FR, Brage ME, Bugbee W. Treatment of post-traumatic ankle arthrosis with bipolar tibiotalar osteochondral shell allografts. Foot Ankle Int. 2002December;23(12):1091-102. [DOI] [PubMed] [Google Scholar]
- 35.Marijnissen ACA, Hoekstra MCL, Pré BC, van Roermund PM, van Melkebeek J, Amendola A, Maathuis P, Lafeber FP, Welsing PM. Patient characteristics as predictors of clinical outcome of distraction in treatment of severe ankle osteoarthritis. J Orthop Res. 2014January;32(1):96-101 Epub 2013 Aug 27. [DOI] [PubMed] [Google Scholar]
- 36.Intema F, Thomas TP, Anderson DD, Elkins JM, Brown TD, Amendola A, Lafeber FP, Saltzman CL. Subchondral bone remodeling is related to clinical improvement after joint distraction in the treatment of ankle osteoarthritis. Osteoarthritis Cartilage. 2011June;19(6):668-75 Epub 2011 Feb 13. [DOI] [PMC free article] [PubMed] [Google Scholar]