Abstract
Objective
Posterior vertebral translation as a type of spondylolisthesis, retrolisthesis is observed commonly in patients with degenerative spinal problems. Nevertheless, there is insufficient literature on retrolisthesis compared to anterolisthesis. The purpose of this study is to clarify the clinical features of retrolisthesis, and its developmental mechanism associated with a compensatory role in sagittal imbalance of the lumbar spine.
Methods
From 2003 to 2012, 230 Korean patients who underwent spinal surgery in our department under the impression of degenerative lumbar spinal disease were enrolled. All participants were divided into four groups : 35 patients with retrolisthesis (group R), 32 patients with simultaneous retrolisthesis and anterolisthesis (group R+A), 76 patients with anterolisthesis (group A), and 87 patients with non-translation (group N). The clinical features and the sagittal parameters related to retrolisthesis were retrospectively analyzed based on the patients' medical records.
Results
There were different clinical features and developmental mechanisms between retrolisthesis and anterolisthesis. The location of retrolisthesis was affected by the presence of simultaneous anterolisthesis, even though it predominantly manifest in L3. The relative lower pelvic incidence, pelvic tilt, and lumbar lordosis compared to anterolisthesis were related to the generation of retrolisthesis, with the opposite observations of patients with anterolisthesis.
Conclusion
Retrolisthesis acts as a compensatory mechanism for moving the gravity axis posteriorly for sagittal imbalance in the lumbar spine under low pelvic incidence and insufficient intra-spinal compensation.
Keywords: Spondylolisthesis, Retrolisthesis, Sagittal imbalance, Lumbar spine
INTRODUCTION
Spondylolisthesis usually implies an anterior translation of a superior vertebra relative to a neighboring inferior vertebra in the sagittal plane. Posterior vertebral translation, a type of spondylolisthesis, has been called retro-spondylolisthesis, or retrolisthesis4,16,18,28,33). Lumbar degenerative spondylolisthesis is a major cause of spinal canal stenosis, and is often related to lower back and leg pain17). The clinical features17), natural course22), and pathogenesis5,14,22,27,31) of degenerative anterolisthesis have been extensively described, because of its importance to the diagnosis of and treatment for spinal canal stenosis1). In contrast to anterolisthesis, there is insufficient literature on retrolisthesis, even though it is common at the end vertebra of a fused spine, particularly in the case of long fusion16), and has also been observed in patients with typical degenerative spinal diseases4,27). Most previous reports of retrolisthesis have had some limitations, because of the small sample size, limited examinations confined to distal lumbar segments4,9,14,16), or the lack of observations of the vertebral relationships to sagittal balance and alignment1).
The purpose of this study is to clarify the clinical features of retrolisthesis, and its developmental mechanism associated with a compensatory role in sagittal imbalance of the lumbar spine.
MATERIALS AND METHODS
Patients
From 2003 to 2012, 230 Korean patients who underwent spinal surgery in our department under the impression of degenerative spinal disorders in the lumbar spine were enrolled. The patients with previous traumatic lesions such as osteoporotic compression fracture; isthmic lysis; degenerative scoliosis of ≥10 degrees; stooping gait implying lumbar degenerative kyphosis; or a history of previous spinal operations were excluded from this study. In total, 67 patients [39 men and 28 women, ranging in age from 38-82 years (mean 65.66±9.75)] with posterior vertebral translation on radiological examination were selected as the patients with retrolisthesis among the participants, and they were divided into two groups. One was the group with only retrolisthesis (group R), and the other group had simultaneous retrolisthesis and anterolisthesis (group R+A). There were 35 patients in group R [total 47 levels, 21 men and 14 women, ranging in age from 45-82 years (mean 66.83±10.51)] and 32 patients in group R+A [total 40 retrolisthesis and 38 anterolisthesis levels, 18 men and 14 women, ranging in age from 38-78 years (mean 64.38±8.84)]. Additionally, 76 patients with only anterolisthesis [group A, 18 men and 58 women, ranging in age from 40-81 years (mean 64.66±9.32)] and 87 patients with non-translation [group N, 40 men and 47 women, ranging in age from 30-88 years (mean 64.17±11.18)], except the 67 patients with retrolisthesis, comprised Groups A and N in order to retrospectively analyze the differences in sagittal profile with the other groups. Before the operation, lateral lumbar radiographs were obtained while patients were lying down with knees and hips fully extended and covering the thoracolumbar area through the sacrum and femoral heads (The supine extended position is a functionally relevant position, and it is suggested that it can replace the upright extended position3). Two observers identified the existence of retrolisthesis, anterolisthesis, and its instability, and measured the degree of degeneration for disc and facet joint, the facet joint angulation, the sagittal parameters including pelvic incidence (PI), sacral slope (SS), pelvic tilt (PT), and lumbar lordosis (LL). All measurements were performed using the stored data of a digitalized radiogram on a computer software system (PACS, INFINITT, Seoul, Korea) in our hospital. All data related to this study were based on retrospective medical records.
Measurement of slippage
The amount of slippage in retrolisthesis or anterolisthesis was measured as the distance between two posterior perpendicular lines over the transverse line of the upper or lower endplate of each vertebra on a lateral neutral film. Retrolisthesis and anterolisthesis were respectively defined as a backward slippage of ≥2 mm and a forward slippage of ≥3 mm on a static lateral lumbar radiograph.
Evaluation of clinical features related to spondylolisthesis
All radiological evaluation was done by two observers, and inter-observer reliability was analyzed for every measurement. Each group was investigated with respect to age; sex; level of spondylolisthesis; direction of slip (anterior or posterior); LL (the angle between the superior endplates of L1 and S1); PI (defined as the angle between the line connecting the center of rotation of the hip joint to the midpoint of the endplate of S1 and perpendicular to the endplate of S1 at its midpoint); PT (defined as the angle between the superior endplate of S1 and the horizontal plane); SS (defined as the angle between a line joining the midpoint of the superior endplate of S1 and the center of rotation of the hip with the vertical plane); amount of disc (Pfirrmann classification, I-V, based on the T2-weighted mid-sagittal MRI scan of the lumbar spine) and facet joint (Weishaupt grade, 0-3, measured as the angle subtended by a line along the long axis of the facet articulation within the midline on T2-weighted axial scan of MRI of the lumbar spine) degeneration; facet joint angulation in the horizontal plane (defined as the angle between a line along the two points at the anteromedial and posterolateral margins of each facet with respect to a coronal reference plane on the posterior wall of the vertebral body); and the existence of instability (difference of slippage of ≥3 mm or angulation ≥10 degrees on a dynamic lateral lumbar radiograph).
Statistical analysis
Student's t-test and one-way analysis of variance for each parametric continuous variable, as well as Mann-Whitney U test and Kruskal-Wallis test for each non-parametric continuous variable, were used for comparing statistical differences. Each categorical variable between each study group was compared using chi-square test, Fisher's exact test, and linear-by-linear association method.
Inter-observer reliability between the measurements of two observers was analyzed using kappa coefficient for categorical variables and Pearson's correlation coefficient and intra-class correlations (ICC; two-way mixed model with consistency agreement; 95% confidence interval) for continuous variables. ICC and Cohen's kappa coefficient values determine their classifications : poor (0.00-0.40), fair (0.40-0.59), good (0.60-0.79), and excellent (0.80-1.00). Statistical analysis was carried out using SPSS version 20.0 software (SPSS Inc., Chicago, IL, USA), and probability values of <0.05 were considered statistically significant.
RESULTS
Clinical characteristics of retrolisthesis and anterolisthesis
Disc degeneration
There was no significant statistical difference between the mean Pfirmann's scores at the level of either retrolisthesis and anterolisthesis in group R+A (p=0.797 in observer 1, p=0.587 in observer 2) (Table 1).
Table 1. Clinical characteristics of retrolisthesis and anterolisthesis in group R+A.
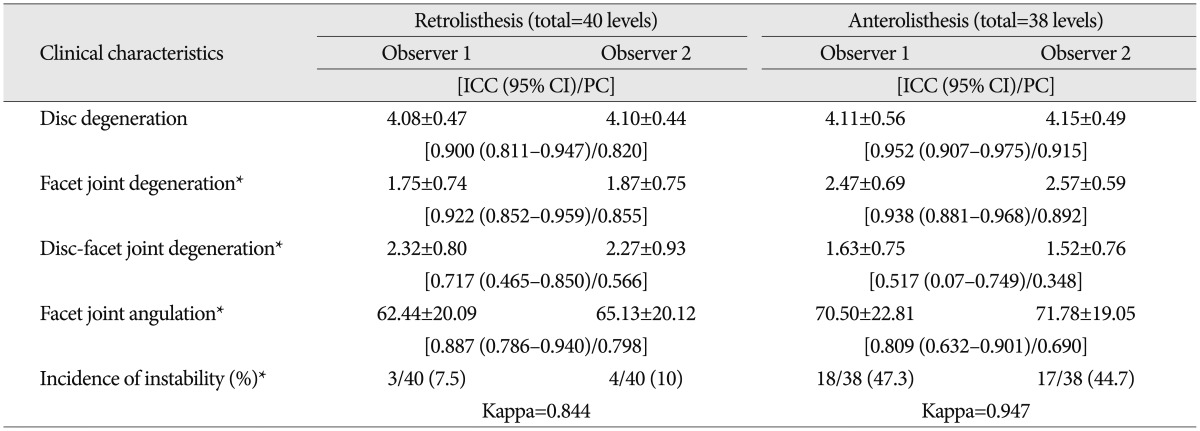
Group R+A : simultaneous retrolisthesis and anterolisthesis (32 patients). Student's t-test, Mann-Whitney U test, and chi-square test were used for statistical analysis. *p<0.05; interclass correlation (ICC), Cohen's kappa coefficient, and Pearson's coefficient (PC) were used for the reliability of sagittal parameter between two observers. CI : confidence interval
Facet joint degeneration
There was a significant statistical difference between the mean Weishaupt grades at the level of either retrolisthesis and anterolisthesis in group R+A (p=0.000 in observers 1 and 2) (Table 1).
The degeneration gap among disc and facet joint (Pfirmann's score minus Weishaupt grade) at the level of either retrolisthesis or anterolisthesis
There was a significant statistical difference between the degeneration gap among disc and facet joint at the level of either retrolisthesis or anterolisthesis in group R+A (p=0.000 in observers 1 and 2) (Table 1).
Facet joint angulation in the horizontal plane
There was no significant statistical difference between the mean facet joint angles at the level of retrolisthesis and anterolisthesis in group R+A (p=0.108 in observer 1, p=0.136 in observer 2) (Table 1).
Incidence of instability
There was a significant statistical difference in the incidence of instability between retrolisthesis (3/40 in observer 1, 4/40 in observer 2) and anterolisthesis (18/38 in observer 1, 17/38 in observer 2) in group R+A (p=0.000 in observer 1, p=0.001 in observer 2) (Table 1).
Prevalence level of retrolisthesis
L3 was the level with the most frequently developing retrolisthesis in groups (group R and R+A), and there was a significant statistical difference of prevalence level between two groups (p=0.022 in observers 1 and 2). The retrolisthesis has a tendency to dominate on L3 and below level in group R, and L3 and above level in group R+A (Table 2).
Table 2. Prevalence level of developing retrolisthesis depends on the presence of anterolisthesis.
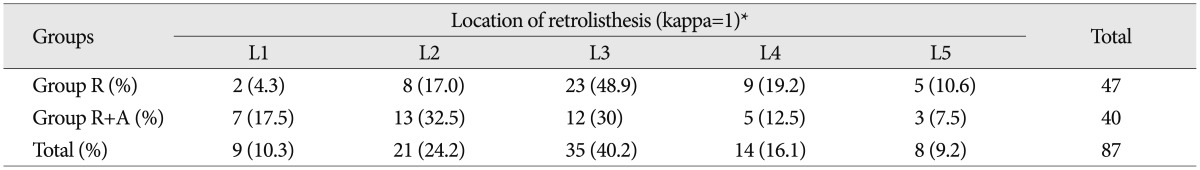
Group R : only retrolisthesis (35 patients), Group R+A : simultaneous retrolisthesis and anterolisthesis (32 patients). Linear by linear association test was used for statistical analysis. *p<0.05; Cohen's kappa coefficient was used for the reliability of location of retrolisthesis between two observers
Sagittal parameters related to spondylolisthesis
Age
There was no significant statistical difference in age between four groups (p=0.633) (Table 3).
Table 3. Sagittal parameters related with spondylolisthesis.
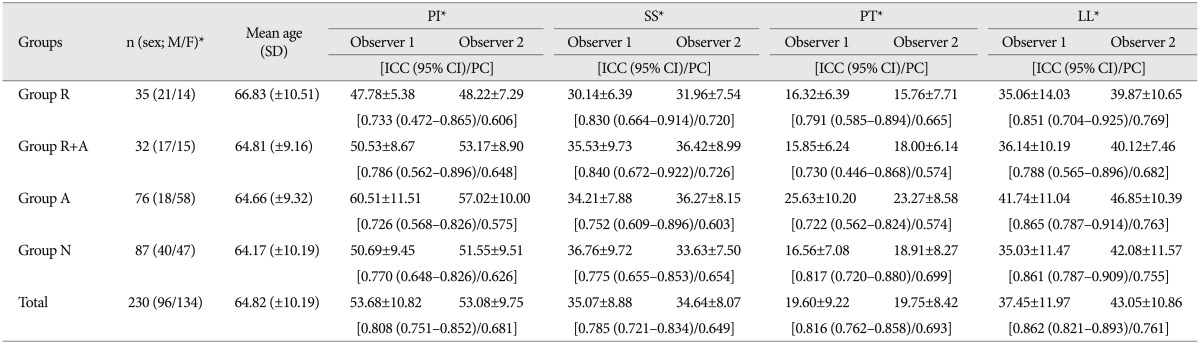
Group R : only retrolisthesis (35 patients), Group R+A : simultaneous retrolisthesis and anterolisthesis (32 patients), Group A : only anterolisthesis (76 patients), Group N : non-translation (87 patients). Chi-square test, one-way analysis of variance test, and Kruskal-Wallis test were used for statistical analysis. *p<0.05; Interclass correlation (ICC) and Pearson's coefficient (PC) were used for the reliability of sagittal parameter between two observers. CI : confidence interval, PI : pelvic incidence, PT : pelvic tilt, SS : sacral slope, LL : lumbar lordosis, SD : standard deviation
Sex
There was a significant difference in sex distribution across the four groups (p=0.001). Females dominated group A (Table 3).
Pelvic incidence
There was a significant statistical difference in the mean PI across the four groups (p=0.002 in observer 1, p=0.000 in observer 2). Group A has a tendency of greater PI compared to that of the other three groups (Table 3).
Sacral slope
There was a significant statistical difference in the mean LL across the four groups (p=0.002 in observer 1, p=0.019 in observer 2). Group R (in observer 1) or group R and N (in observer 2) has a tendency towards lower SS compared to that of other groups (Table 3).
Pelvic tilt
There was a significant statistical difference in the mean PT across the four groups (p=0.002 in observer 1, p=0.001 in observer 2). Group A has a tendency towards greater PT compared to that of the other three groups (Table 3).
Lumbar lordosis
There was a significant statistical difference in the mean LL across the four groups (p=0.002 in observer 1, p=0.000 in observer 2). Group A has a tendency towards more LL compared to that of the other three groups (Table 3).
The difference of LL in patients with L4 anterolisthesis in the presence of L3 retrolisthesis
There was a significant statistical difference of LL in patients with L4 anterolisthesis due to the presence of L3 retrolisthesis (p=0.03 in observer 1, p=0.005 in observer 2). The patients with L3 retrolisthesis presented a lower LL (Table 4).
Table 4. The difference of LL in patients with L4 anterolisthesis under the presence of L3 retrolisthesis.
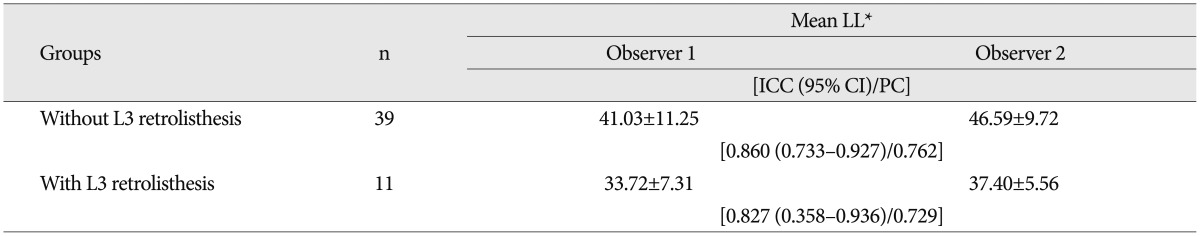
Patients with L4 anterolisthesis were selected from group A (only anterolisthesis) and R+A (simultaneous retrolisthesis and anterolisthesis). Student's t-test was used for statistical analysis. *p<0.05; interclass correlation (ICC) and Pearson's coefficient (PC) were used for the reliability of lumbar lordosis (LL) between two observers. CI : confidence interval
Correlations between sagittal parameters in all patients
The relations between parameters were presented as Pearson's coefficient (r). There were positive correlations between PI and other parameters including PT, SS, and LL; SS and LL; and negative correlations between PT and SS with statistical significance (p<0.05). However, there was no coincidence in statistical significance between observers (p=0.065 of observer 1 and p=0.022 of observer 2), although there was a negative correlation between PT and LL (Table 5).
Table 5. Correlations between sagittal parameters in all participants by Pearson's coefficient (r).
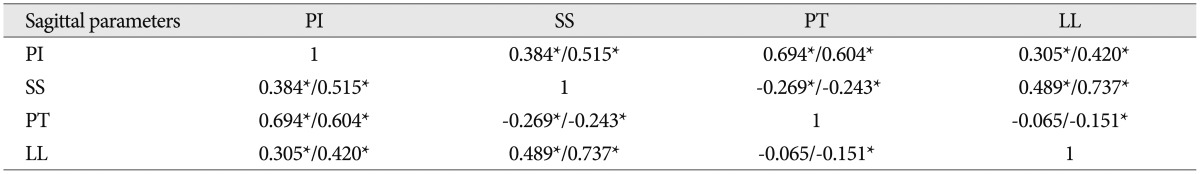
Pearson's coefficient (r) was used for statistical analysis. *p<0.05. PI : pelvic incidence, PT : pelvic tilt, SS : sacral slope, LL : lumbar lordosis
DISCUSSION
The patterns of degeneration in the lumbar spine have been extensively studied. Some studies have demonstrated that disc degeneration occurs first. Then, an increase in the rotational and transitional forces leads to the overloading of the facet joints. This, in turn, leads to a progressive degenerative change in the facet joint, with a lag of over two decades following the onset of disc degeneration6,7,10,11,12,15,23). Disc degeneration is believed to precede facet joint degeneration, and to be a primary cause of anterolisthesis6,17,24). Love et al.21) have concluded that a sagittal-oriented facet angle is the result of arthritic remodeling and not a primary cause of anterolisthesis. We also found that there was no statistically significant difference in the sagittal facet angle between anterolisthesis and retrolisthesis in this study.
Recent studies have suggested that factors such as global spinal sagittal alignment and pelvic parameters account for variations in degenerative patterns, including facet and disc pathology29). We think that the factors related to spinal sagittal balance may have a strong influence on the development of a different kind of spondylolisthesis, including retrolisthesis and anterolisthesis, based on the results in this study. Under specific conditions such as greater LL and high PI, anterolisthesis might develop with more overloaded power on the facet joint, which leads to facet joint degeneration as well as to disc degeneration. In contrast to the development of anterolisthesis, there was a greater aggravation of disc degeneration than of facet degeneration with lower overloading power on the facet joints in retrolisthesis under contrasting conditions of sagittal profiles.
Retrolisthesis may be observed in any spinal segment, but a specifically high incidence has been reported in the lower lumbar spine4). In contrast, other authors have reported that retrolisthesis was more common in men and in the upper lumbar (L2 and 3) spine18). Retrolisthesis is typically limited to 2-3 mm of slippage in the lumbar spine, and sometimes results in foraminal stenosis, and more rarely in central stenosis2). Reduced disc height, spinal sagittal alignment, endplate inclination, and the traction of erector spine muscles have been considered as causative factors related to retrolisthesis4,24).
Disc height was significantly reduced in segments with retrolisthesis, which underscores the importance of the disc for segmental stability ("flat tire syndrome")2). According to a previous study23), the relative kyphotic disposition of the lumbo-sacral segment (L5-S1) could be a trigger for a local compensatory mechanism such as retrolisthesis at L4-5. In our study, L3 was the dominant level that was prone to developing retrolisthesis, and the upper lumbar levels including L3 were the main sites at which anterolisthesis combined at the L4 level. In terms of the lumbar lordotic curve, anterolisthesis was associated with a relatively greater LL than with retrolisthesis. We assume that there is a different developmental mechanism between retrolisthesis and anterolisthesis. The greater LL leads to the development of anterolisthesis, especially on L4, because of the shearing force towards the anterior-inferior direction and the overloading power on the facet joint.
The most common opinion is that LL flattens out with spinal problems and subsequent age-related degenerative changes25). However, most studies did not find a significant association between age and lumbar lordotic curvature19,25,36,37). In addition, Oliver and Middleditch26) found no difference in the LL between males and females until middle age, but some studies found that females have a significantly greater lordosis angle (2-5 degrees) than males8,13,25,34,37). There is evidence of a difference based on gender, with female dominance in group A exhibiting greater LL than that of other groups, which supports the theory above. LL is significantly greater in individuals with a high body mass index25), and also increases in the late stages of pregnancy35).
Many researchers have found a high correlation between LL and pelvic and thoracic parameters in the sagittal profile. Greater LL correlates with a more horizontally inclined sacrum (increased sacral slope, more vertical sacral endplate), increased PI, and increased PT20,30,32). This tendency among the lumbar and pelvic parameters was also found in our results, and it can be understood from the view of hyperextension as a compensatory mechanism. The hyperextension of adjacent segments is a very common compensatory mechanism that limits the consequences of lumbar kyphosis in terms of gravity axis shift2). Hyperextension can be global (multi-segmental) or local (mono-segmental), and efficient for placing the upper spine posteriorly. We found that lower degrees of LL and PI were noted in patients with retrolisthesis. In contrast, there was high LL and PI in patients with anterolisthesis. As mentioned above, retrolisthesis may act in a compensatory role to move the gravity axis posteriorly in cases with low PI, which cannot increase a PT sufficiently as a compensatory mechanism. In patients with high PI, an increase in PT occurs as a compensatory mechanism when LL flattens out and the gravity axis moves anteriorly. In addition, an increase in SS according to the change in PT leads to an increase in LL and hyperextension as a compensatory mechanism.
In conclusion, we presumed two compensatory mechanisms, including lumbar hyperextension and increase of PT, in the case of a flattened lumbar spine. The group with high lumbar lordosis (group A) exhibited high PI and PT, and developed anterolisthesis because of their high lumbar lordotic curvature. In contrast, the group with low PI (group R) could not compensate for their sagittal imbalance by increasing their PT and hyperextension sufficiently. Retrolisthesis substitutes hyperextension as a compensatory mechanism by moving the upper or middle level lumbar vertebra directly in the posterior direction.
This study also has some limitations. We assumed that none of the patients who participated in this study had associated lumbar degenerative kyphosis, which shows excessive positive sagittal imbalance, based on their medical records. Patients with a stooping gait, which implies lumbar degenerative kyphosis, and a history of compression fracture, which can influence sagittal balance, were excluded. Nevertheless, the participants did not undergo imaging of their entire spine, which can facilitate the objective measurement of sagittal balance using sagittal parameters such as SVA.
CONCLUSION
There are different clinical features and developmental mechanisms between retrolisthesis and anterolisthesis. We think that anterolisthesis comes from the result of lumbar lordosis, and retrolisthesis may be a role of compensatory mechanism for moving the gravity axis posteriorly for correcting sagittal imbalance in the lumbar spine under the condition of low PI and insufficient intra-spinal compensation.
References
- 1.Arnoldi CC, Brodsky AE, Cauchoix J, Crock HV, Dommisse GF, Edgar MA, et al. Lumbar spinal stenosis and nerve root entrapment syndromes. Definition and classification. Clin Orthop Relat Res. 1976;(115):4–5. [PubMed] [Google Scholar]
- 2.Barrey C, Roussouly P, Perrin G, Le Huec JC. Sagittal balance disorders in severe degenerative spine. Can we identify the compensatory mechanisms? Eur Spine J. 2011;20(Suppl 5):626–633. doi: 10.1007/s00586-011-1930-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Been E, Kalichman L. Lumbar lordosis. Spine J. 2014;14:87–97. doi: 10.1016/j.spinee.2013.07.464. [DOI] [PubMed] [Google Scholar]
- 4.Berlemann U, Jeszenszky DJ, Bühler DW, Harms J. Mechanisms of retrolisthesis in the lower lumbar spine. A radiographic study. Acta Orthop Belg. 1999;65:472–477. [PubMed] [Google Scholar]
- 5.Boden SD, Riew KD, Yamaguchi K, Branch TP, Schellinger D, Wiesel SW. Orientation of the lumbar facet joints : association with degenerative disc disease. J Bone Joint Surg Am. 1996;78:403–411. doi: 10.2106/00004623-199603000-00012. [DOI] [PubMed] [Google Scholar]
- 6.Butler D, Trafimow JH, Andersson GB, McNeill TW, Huckman MS. Discs degenerate before facets. Spine (Phila Pa 1976) 1990;15:111–113. doi: 10.1097/00007632-199002000-00012. [DOI] [PubMed] [Google Scholar]
- 7.Eubanks JD, Lee MJ, Cassinelli E, Ahn NU. Does lumbar facet arthrosis precede disc degeneration? A postmortem study. Clin Orthop Relat Res. 2007;464:184–189. doi: 10.1097/BLO.0b013e3181583d4e. [DOI] [PubMed] [Google Scholar]
- 8.Fernand R, Fox DE. Evaluation of lumbar lordosis. A prospective and retrospective study. Spine (Phila Pa 1976) 1985;10:799–803. doi: 10.1097/00007632-198511000-00003. [DOI] [PubMed] [Google Scholar]
- 9.Fitzgerald JA, Newman PH. Degenerative spondylolisthesis. J Bone Joint Surg Br. 1976;58:184–192. doi: 10.1302/0301-620X.58B2.932080. [DOI] [PubMed] [Google Scholar]
- 10.Fujiwara A, Lim TH, An HS, Tanaka N, Jeon CH, Andersson GB, et al. The effect of disc degeneration and facet joint osteoarthritis on the segmental flexibility of the lumbar spine. Spine (Phila Pa 1976) 2000;25:3036–3044. doi: 10.1097/00007632-200012010-00011. [DOI] [PubMed] [Google Scholar]
- 11.Fujiwara A, Tamai K, An HS, Kurihashi T, Lim TH, Yoshida H, et al. The relationship between disc degeneration, facet joint osteoarthritis, and stability of the degenerative lumbar spine. J Spinal Disord. 2000;13:444–450. doi: 10.1097/00002517-200010000-00013. [DOI] [PubMed] [Google Scholar]
- 12.Fujiwara A, Tamai K, Yamato M, An HS, Yoshida H, Saotome K, et al. The relationship between facet joint osteoarthritis and disc degeneration of the lumbar spine : an MRI study. Eur Spine. 1999;8:396–401. doi: 10.1007/s005860050193. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Gelb DE, Lenke LG, Bridwell KH, Blanke K, McEnery KW. An analysis of sagittal spinal alignment in 100 asymptomatic middle and older aged volunteers. Spine (Phila Pa 1976) 1995;20:1351–1358. [PubMed] [Google Scholar]
- 14.Grobler LJ, Robertson PA, Novotny JE, Pope MH. Etiology of spondylolisthesis. Assessment of the role played by lumbar facet joint morphology. Spine (Phila Pa 1976) 1993;18:80–91. [PubMed] [Google Scholar]
- 15.Haher TR, O'Brien M, Dryer JW, Nucci R, Zipnick R, Leone DJ. The role of the lumbar facet joints in spinal stability. Identification of alternative paths of loading. Spine (Phila Pa 1976) 1994;19:2667–2670. discussion 2671. [PubMed] [Google Scholar]
- 16.Hambly MF, Wiltse LL, Raghavan N, Schneiderman G, Koenig C. The transition zone above a lumbosacral fusion. Spine (Phila Pa 1976) 1998;23:1785–1792. doi: 10.1097/00007632-199808150-00012. [DOI] [PubMed] [Google Scholar]
- 17.Herkowitz HN. Spine update. Degenerative lumbar spondylolisthesis. Spine (Phila Pa 1976) 1995;20:1084–1090. doi: 10.1097/00007632-199505000-00018. [DOI] [PubMed] [Google Scholar]
- 18.Iguchi T, Wakami T, Kurihara A, Kasahara K, Yoshiya S, Nishida K. Lumbar multilevel degenerative spondylolisthesis : radiological evaluation and factors related to anterolisthesis and retrolisthesis. J Spinal Disord Tech. 2002;15:93–99. doi: 10.1097/00024720-200204000-00001. [DOI] [PubMed] [Google Scholar]
- 19.Kalichman L, Li L, Hunter DJ, Been E. Association between computed tomography-evaluated lumbar lordosis and features of spinal degeneration, evaluated in supine position. Spine J. 2011;11:308–315. doi: 10.1016/j.spinee.2011.02.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Lim JK, Kim SM. Difference of Sagittal Spinopelvic Alignments between Degenerative Spondylolisthesis and Isthmic Spondylolisthesis. J Korean Neurosurg Soc. 2013;53:96–101. doi: 10.3340/jkns.2013.53.2.96. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Love TW, Fagan AB, Fraser RD. Degenerative spondylolisthesis. Developmental or acquired? J Bone Joint Surg Br. 1999;81:670–674. doi: 10.1302/0301-620x.81b4.9682. [DOI] [PubMed] [Google Scholar]
- 22.Matsunaga S, Sakou T, Morizono Y, Masuda A, Demirtas AM. Natural history of degenerative spondylolisthesis. Pathogenesis and natural course of the slippage. Spine (Phila Pa 1976) 1990;15:1204–1210. doi: 10.1097/00007632-199011010-00021. [DOI] [PubMed] [Google Scholar]
- 23.Mehta JS, Kochhar S, Harding IJ. A slip above a slip : retrolisthesis of the motion segment above a spondylolytic spondylolisthesis. Eur Spine J. 2012;21:2128–2133. doi: 10.1007/s00586-012-2239-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Moore RJ, Crotti TN, Osti OL, Fraser RD, Vernon-Roberts B. Osteoarthrosis of the facet joints resulting from anular rim lesions in sheep lumbar discs. Spine (Phila Pa 1976) 1999;24:519–525. doi: 10.1097/00007632-199903150-00003. [DOI] [PubMed] [Google Scholar]
- 25.Murrie VL, Dixon AK, Hollingworth W, Wilson H, Doyle TA. Lumbar lordosis : study of patients with and without low back pain. Clin Anat. 2003;16:144–147. doi: 10.1002/ca.10114. [DOI] [PubMed] [Google Scholar]
- 26.Oliver J, Middleditch A. Functional anatomy of the spine. Oxford, Boston: Butterworth-Heinemann; 1991. p. ppviii, 328. [Google Scholar]
- 27.Rosenberg NJ. Degenerative spondylolisthesis. Predisposing factors. J Bone Joint Surg Am. 1975;57:467–474. [PubMed] [Google Scholar]
- 28.Rothman SL, Glenn WV, Jr, Kerber CW. Multiplanar CT in the evaluation of degenerative spondylolisthesis. A review of 150 cases. Comput Radiol. 1985;9:223–232. doi: 10.1016/0730-4862(85)90079-4. [DOI] [PubMed] [Google Scholar]
- 29.Roussouly P, Gollogly S, Berthonnaud E, Dimnet J. Classification of the normal variation in the sagittal alignment of the human lumbar spine and pelvis in the standing position. Spine (Phila Pa 1976) 2005;30:346–353. doi: 10.1097/01.brs.0000152379.54463.65. [DOI] [PubMed] [Google Scholar]
- 30.Roussouly P, Nnadi C. Sagittal plane deformity : an overview of interpretation and management. Eur Spine J. 2010;19:1824–1836. doi: 10.1007/s00586-010-1476-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Sato K, Wakamatsu E, Yoshizumi A, Watanabe N, Irei O. The configuration of the laminas and facet joints in degenerative spondylolisthesis. A clinicoradiologic study. Spine (Phila Pa 1976) 1989;14:1265–1271. doi: 10.1097/00007632-198911000-00022. [DOI] [PubMed] [Google Scholar]
- 32.Schwab F, Patel A, Ungar B, Farcy JP, Lafage V. Adult spinal deformity-postoperative standing imbalance : how much can you tolerate? An overview of key parameters in assessing alignment and planning corrective surgery. Spine (Phila Pa 1976) 2010;35:2224–2231. doi: 10.1097/BRS.0b013e3181ee6bd4. [DOI] [PubMed] [Google Scholar]
- 33.Sihvonen T, Lindgren KA, Airaksinen O, Manninen H. Movement disturbances of the lumbar spine and abnormal back muscle electromyographic findings in recurrent low back pain. Spine (Phila Pa 1976) 1997;22:289–295. doi: 10.1097/00007632-199702010-00012. [DOI] [PubMed] [Google Scholar]
- 34.Vialle R, Levassor N, Rillardon L, Templier A, Skalli W, Guigui P. Radiographic analysis of the sagittal alignment and balance of the spine in asymptomatic subjects. J Bone Joint Surg Am. 2005;87:260–267. doi: 10.2106/JBJS.D.02043. [DOI] [PubMed] [Google Scholar]
- 35.Whitcome KK, Shapiro LJ, Lieberman DE. Fetal load and the evolution of lumbar lordosis in bipedal hominins. Nature. 2007;450:1075–1078. doi: 10.1038/nature06342. [DOI] [PubMed] [Google Scholar]
- 36.Youdas JW, Garrett TR, Egan KS, Therneau TM. Lumbar lordosis and pelvic inclination in adults with chronic low back pain. Phys Ther. 2000;80:261–275. [PubMed] [Google Scholar]
- 37.Youdas JW, Garrett TR, Harmsen S, Suman VJ, Carey JR. Lumbar lordosis and pelvic inclination of asymptomatic adults. Phys Ther. 1996;76:1066–1081. doi: 10.1093/ptj/76.10.1066. [DOI] [PubMed] [Google Scholar]


