Summary
Objective
We attempted to estimate the rate of total hip replacement (THR) using a national database and the prevalence of hip osteoarthritis (OA) from the reading of intravenous pyelograms (IVPs) in a Korean population.
Materials
Reimbursement records from all hospitals in South Korea were extracted from the Health Insurance Review Agency (HIRA) database. Records with both the procedure code corresponding to THR and containing the diagnosis code for hip OA were selected. We estimated the age- and sex-specific rates of THR from 2002 to 2006. Hip joints from 580 subjects older than 70 years old who underwent an IVP were assessed for the presence of OA.
Results
The rate of THR increased with age, reaching a peak over the age of 65–69 years, with the age-standardized risk ratios in women vs men of approximately 1.5. Although the rate of THR increased over the 5-year study period, it was significantly lower than that of total knee replacement (TKR) in Korean population (THR vs TKR 1:15.9). The prevalence of hip OA in the IVP cohort was 1.2% (1.7% for men and 0.7% for women).
Conclusion
The rate of THR was significantly lower than that of TKR in Korean population. Hip OA prevalence among the IVP subjects was 1.2%. Further studies on factors that account for the low prevalence of hip OA among Asians need to be conducted.
Keywords: Hip, Osteoarthritis, Arthroplasty, Replacement, Prevalence
Introduction
Osteoarthritis (OA) is a leading cause of disability in Western societies. In the United States, hip OA affects about 5% of the over the age of 60 years1 and approximately 360,000 hip replacement population surgeries are performed yearly, second only to knee replacement among musculoskeletal procedures2.
Several studies have found that the prevalence of hip OA is significantly lower among Asians while the prevalence of knee OA is as common as, or even higher than that reported for the US Caucasian population3–5. A few studies have also shown that the rate of total hip arthroplasty in Asian migrants was much lower than that among the Caucasian population6,7. To the best of our knowledge, no such epidemiologic data on hip replacement has been published in Asia, where over 60% of world population lives.
In this study, we describe the age and sex-specific incidence of total hip replacement (THR) from OA as well as the trend of THR utilization from the year 2002 to the year 2006, using national data collected by the Health Insurance Review Agency (HIRA) in South Korea. We also attempted to support the above findings by the reading of 580 intravenous pyelograms (IVPs) performed in a Korean hospital.
Materials and methods
DATA ACQUISITION
HIRA, established in 1989, is a non-profit agency sponsored by the Korean Ministry of Health and Welfare. The agency is responsible for the general administrative affairs of the Korean National Health Insurance covering all citizens of South Korea. The HIRA database contains reimbursement records from all medical facilities (approximately 5–6 million inpatient-visits per year in about 1100 hospitals and 25,000 private clinics) in South Korea. Information in the HIRA database includes a unique identification number for each patient, age, sex, primary diagnosis [based on the International Classification of Disease, Tenth Edition, Clinical Modification (ICD-10-CM)], and the date of surgery. In the current analysis, we used data collected from the year 2002 to the year 2006.
Records with a procedure code N0711, corresponding to THR, were selected from the HIRA database. In addition, the database adapted ICD-10-CM to code for the disease diagnosis. Hip OA was coded as M16. Revision hip arthroplasty was assigned a separate procedure code and was excluded from the current analysis.
GRADING OF HIP OA FROM IVPs
To estimate the prevalence of hip OA in Korean subjects that were not selected with respect to hip symptoms, we identified all subjects older than 70 years old who received an IVP at a university-affiliated hospital during 2004–2006. The use of clinical data was approved by the Hallym University Sacred Heart Hospital research ethics committee. The hip joints were assessed from the postmicturition radiograph, which was taken with a tube-to-film distance of 100 cm and the central ray centered approximately 10 cm higher in the midline. The position of the feet was typically about 30° external rotation. Radiographs were excluded if neither hip could be visualized adequately. All of the radiographs were read by two readers (an orthopedic surgeon and a radiologist), who were both experienced in the reading of hip OA radiographs. Atlas photographs illustrating the individual radiographic features of OA were used to standardize the readings8,9. Each hip was scored for joint space narrowing (JSN) (range 0–3, where 0 = none and 3 = complete loss of joint space) at two locations (superolateral and superomedial) and for osteophytes (range 0–3, where 0 = none and 3 = severe) at four locations (superior femoral, lateral acetabular, inferior femoral and acetabular). Subchondral sclerosis, cysts, and femoral neck deformity were also graded (range 0–1, where 0 = none and 1 = present). A summary grade of OA (range 0–4) for each hip was assigned, based on the number of individual radiographic features present, as has been reported previously10. We also measured the minimum joint space (in mm) using calipers according to a previously described method11.
A subject was characterized as having radiographic hip OA if (1) the summary grade was ≥2 (definite osteophytes ≥ grade2 or JSN ≥ grade2 plus subchondral sclerosis or cysts) or (2) a minimum joint space was ≤1.5 mm. The intra-reader reproducibility of the summary grade (OA vs no OA), based on repeat readings of a random sample of 50 images, was high (κ = 0.86). Twenty-six (4.5%) films with discrepancy about either the presence of ≥2 JSN or ≥2 osteophytes between the two readers were adjudicated by a panel, including the two original readers and a third reader.
STATISTICAL ANALYSIS
We divided the age of the subjects into 5-year categories. For each calendar year, we estimated the age- and sex-specific rates of THR by dividing the total number of THR cases that occurred in that year by the total number of subjects in each age and sex category, based on the Korean National Census data conducted in year 200512. We also estimated the prevalence of radiographic hip OA among the patients who had IVP images in a university-affiliated hospital during 2004–2006.
Results
From 2002 to 2006, 18,978 subjects had THR surgery. Of these subjects, 3983 were patients with hip OA (M16), 12,797 with avascular necrosis (AVN), 423 with inflammatory arthritis (e.g., rheumatoid arthritis, ankylosing spondylitis and unclassified arthritis), and only eight patients underwent surgery for a femoral neck fracture. Of 3983 subjects who had THR from hip OA, 39% were men.
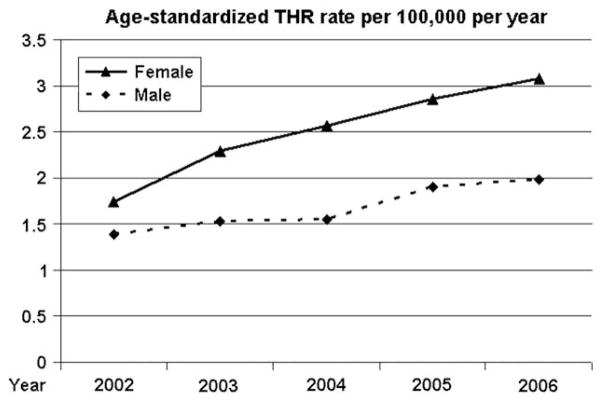
The rate of THR increased with age, reaching a peak over the age of 65–69 years for both women and men, after which it decreased (Table I). As shown in Fig. 1, the age-standardized THR rate increased in both sexes from 2002 to 2006, and the age-standardized risk ratios of THR in women vs men were 1.16, 1.41, 1.57, 1.40 and 1.41 for 2002, 2003, 2004, 2005, and 2006, respectively. The risk of THR due to hip OA was significantly lower than that of total knee replacement (TKR) due to knee OA in South Korea (THR vs TKR 1:15.9)13.
Table I.
Age-specific rates (per 100,000 per year) of THR by calendar year
| Age groups | Men (n = 1564)
|
Women (n = 2419)
|
||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| 2002 | 2003 | 2004 | 2005 | 2006 | 2002 | 2003 | 2004 | 2005 | 2006 | |
| 40–44 | 1.20 | 1.34 | 1.54 | 1.58 | 1.44 | 1.29 | 1.76 | 1.18 | 1.81 | 1.57 |
| 45–49 | 1.12 | 1.94 | 1.48 | 1.58 | 1.58 | 1.34 | 2.22 | 2.48 | 2.48 | 3.20 |
| 50–54 | 1.96 | 2.59 | 2.45 | 3.36 | 3.29 | 1.89 | 3.43 | 3.85 | 4.76 | 5.81 |
| 55–59 | 3.55 | 3.28 | 2.84 | 4.35 | 4.79 | 4.78 | 4.17 | 4.86 | 5.30 | 6.43 |
| 60–64 | 4.12 | 3.79 | 4.68 | 5.46 | 6.57 | 6.05 | 7.97 | 8.17 | 8.27 | 7.36 |
| 65–69 | 4.37 | 4.10 | 5.69 | 7.01 | 6.48 | 5.41 | 9.20 | 10.17 | 12.77 | 13.09 |
| 70–74 | 3.50 | 3.30 | 2.53 | 5.25 | 5.06 | 5.28 | 5.01 | 6.50 | 7.85 | 8.53 |
| 75–79 | 3.33 | 2.59 | 2.59 | 1.11 | 5.91 | 2.82 | 2.02 | 3.63 | 4.43 | 5.44 |
| ≥80 | 1.02 | 1.53 | 0.51 | 2.56 | 3.07 | 2.34 | 0.64 | 0.43 | 2.23 | 2.55 |
For each calendar year, we estimated the age-specific rates of THR by dividing the total number of THR cases that occurred in that year by the total number of subjects in each age category based on Korean National Census data conducted in year 2005.
Fig. 1.
Age- and sex-standardized THR rate in Korean population from year 2002 to 2006. Rates were calculated by dividing the total number of THR patients registered at the HIRA of Korea by the total population in the respective age and sex groups, according to data from the Korean Census 2005, and then standardized according to the age distribution in women.
Next, we identified 580 subjects older than 70 years who performed IVP between the year 2004 and 2006 from a university-affiliated hospital. One subject was excluded due to poor visualization of the hip joint. The mean age of the subjects was 78.3 years (range 71–95 years), and half of the subjects were men. The most common indications for IVP were benign prostatic hypertrophy (186 subjects, 32%), neuromuscular dysfunction of bladder (140 subjects, 24%), and evaluation of suspicious malignancy (67 subjects, 11.6%). Two subjects had bilateral THR, one had unilateral THR, and five had unilateral hemiarthroplasty. Of the remaining 1148 hips (577 patients), only six subjects (with one bilateral, three right hip, and two left hip) had hip OA (summary grade ≥ 2 or minimal joint space ≤1.5 mm). Of these subjects, four were men (Table II).
Table II.
Demographic and clinical features of subjects with abnormal hip joints in IVP
| Age | Sex | Radiographic finding
|
Clinical finding | ||
|---|---|---|---|---|---|
| Right | Left | ||||
| 1 | 77 | M | THR | THR | Unknown |
| 2 | 75 | M | THR | THR | Unknown |
| 3 | 72 | M | Grade1 | THR | AVN |
| 4 | 75 | F | Grade1 | Hemiarthroplasty | Osteoporotic femoral neck fracture |
| 5 | 82 | F | Hemiarthroplasty | Grade1 | Osteoporotic femoral neck fracture |
| 6 | 81 | F | Grade1 | Hemiarthroplasty | Osteoporotic femoral neck fracture |
| 7 | 83 | F | Grade1 | Hemiarthroplasty | Unknown |
| 8 | 83 | F | Grade1 | Hemiarthroplasty | Unknown |
| 9 | 78 | M | Grade4 | Grade1 | Old acetabular fracture |
| 10 | 76 | M | Grade2 | Grade2 | Hip pain |
| 11 | 80 | M | Grade1 | Grade2 | Hip pain |
| 12 | 80 | F | Grade2 | Grade1 | Unknown |
| 13 | 85 | F | Grade4 | Grade1 | Unknown |
| 14 | 74 | M | Grade1 | Minimum joint space 1.45 mm | Unknown |
Medical records of all the subjects with hip OA, THR, or hemiarthroplsaty were subsequently reviewed to obtain information on the presence of hip pain, previous diagnosis, and the reason for surgery. Among the three subjects with THR, one had AVN of the femoral head. Relevant information on the other two subjects with bilateral THR was not available. Among the five subjects with hemiarthroplasty, three had a femoral neck fracture due to osteoporosis at the operated hip, and information for the other two subjects was not available. Among the six subjects with hip OA, one subject with grade4 hip had an old traumatic acetabular fracture, and subsequently underwent THR. Two subjects with grade2 hip had a history of visiting the orthopedic department due to hip and back pain, and information for the remaining three subjects was not available. If it was presumed that the two subjects with THR underwent surgery due to OA and if the subject with traumatic fracture was excluded, the estimated prevalence of hip OA in this IVP cohort was 1.2% (1.7% for men, 0.7% for women).
Discussion
Using the national database for healthcare reimbursement in Korea, we found that the rate of THR increased from 2002 to 2006, but it was much lower than that of TKR. To the best of our knowledge, no epidemiological study has examined the rate of THR utilization among an Asian population. The prevalence of radiographic OA that was examined by IVP films was 1.2%.
It might not be appropriate to compare the rate of THR in Korea with that in Western countries, as a discrepancy may stem from the differences other than the prevalence of hip OA. Thus, we tried to compare the rate of THR and TKR due to OA in Korea, and found that compared to Western countries, the rate of THR is far lower than that of TKR (less than 1/15). For example, the rate of TKR in the US is about 20% higher than that of THR, while the rate of TKR in Sweden is lower than that of THR2,14,15. In addition, while primary OA accounted for only 18% of THR in Korea, it was the main indication for THR in Sweden with 75% of the THRs performed to treat OA15. This finding suggests that severe hip OA is much less common in Korea as compared to Western countries, and as compared to severe knee OA.
In order to support the low THR rate, we estimated the prevalence of hip OA in 580 subjects that underwent IVP who were over 70 years old. The prevalence of 1.2% in our subjects is in line with the prevalence of subjects ≥60 years old in a study performed in China3. Our prevalence may well have been overestimated as we presumed that the two bilateral THR subjects without clinical information underwent surgery due to OA. Another report showed that the prevalence of hip OA estimated by IVP among Chinese men aged 60–75 years was 5.4%16. While it is not possible to compare the prevalence of hip OA of previous reports with that of the current study due to differences in the grading system and radiographic method, lower prevalence of hip OA among Asians compared to Caucasian population is consistent.
What is the reason for the discrepancy of the prevalence of hip OA between Asians and Caucasians? First, differences in the frequency of acetabular dysplasia among different ethnic groups have been postulated. However, in studies involving Japanese and Chinese population16,17, the prevalence of acetabular dysplasia was not higher compared to British population, while the prevalence of hip OA was lower among the Japanese and Chinese population.
Second, genetic polymorphisms may account for the ethnic difference in the susceptibility to OA. It has been reported that the association of several candidate genes, such as asporin and calmudulin 1, with OA is strongly dependent on ethnicity and often on the involved joint18–23. Thus, it would be of interest to define and to characterize the genetic polymorphism that confers protection against hip OA in Asians.
While kneeling or squatting typical of traditional Asian lifestyle is postulated to have a detrimental role in the development of knee OA24, it may work in the opposite direction in the development of hip OA. This hypothesis may be proven by a prospective follow-up of young Asians who have adapted a Western lifestyle for the development of hip OA.
This study has limitations. First, disease misclassifications or coding errors could have occurred in the large-scale administrative databases. Second, we evaluated IVPs for the prevalence of hip OA. Although it is a frequently reported method for the evaluation of hip OA, differences in the placement of the hip and lack of the centralization of hip joints as compared to a standard pelvis radiograph might have affected the evaluation of the joint space. Finally, our IVP data was generated from a single institute, and our findings may not represent the overall incidence of hip OA in Korea.
In conclusion, the THR rate was significantly lower than that of TKR in South Korea. Studies on protective factors that account for the low prevalence of hip OA among Asians need to be conducted.
Acknowledgments
Supported by a grant from the Hallym University Sacred Heart Hospital Clinical Research (no. 01-2007-02) and a grant from Pfizer. The study sponsor had no involvement in the study design, the collection, analysis, and interpretation of data, in the writing of the manuscript or in the decision to submit the manuscript for publication.
Footnotes
Conflict of interest
No conflict of interest has been declared by the authors except for YW Song who receives research funding from Pfizer and DJ Hunter, who receives research funding from Pfizer, Merck, Don Joy and Astra Zeneca.
References
- 1.Felson DT, Zhang Y. An update on the epidemiology of knee and hip osteoarthritis with a view to prevention. Arthritis Rheum. 1998;41:1343–55. doi: 10.1002/1529-0131(199808)41:8<1343::AID-ART3>3.0.CO;2-9. [DOI] [PubMed] [Google Scholar]
- 2.Agency for Healthcare Research and Quality. [Accessed 07/11/2007];HCUP: a Tool for Identifying, Tracking, and Analyzing National Hospital Statistics. < http://www.hcup-us.ahrq.gov/reports/statbriefs/sb34.jsp>.
- 3.Nevitt MC, Xu L, Zhang Y, Lui LY, Yu W, Lane NE, et al. Very low prevalence of hip osteoarthritis among Chinese elderly in Beijing, China, compared with whites in the United States: the Beijing osteoarthritis study. Arthritis Rheum. 2002;46:1773–9. doi: 10.1002/art.10332. [DOI] [PubMed] [Google Scholar]
- 4.Zhang Y, Xu L, Nevitt MC, Aliabadi P, Yu W, Qin M, et al. Comparison of the prevalence of knee osteoarthritis between the elderly Chinese population in Beijing and whites in the United States: the Beijing Osteoarthritis Study. Arthritis Rheum. 2001;44:2065–71. doi: 10.1002/1529-0131(200109)44:9<2065::AID-ART356>3.0.CO;2-Z. [DOI] [PubMed] [Google Scholar]
- 5.Hoaglund FT, Yau AC, Wong WL. Osteoarthritis of the hip and other joints in southern Chinese in Hong Kong. J Bone Joint Surg Am. 1973;55:545–57. [PubMed] [Google Scholar]
- 6.Hoaglund FT, Oishi CS, Gialamas GG. Extreme variations in racial rates of total hip arthroplasty for primary coxarthrosis: a population-based study in San Francisco. Ann Rheum Dis. 1995;54:107–10. doi: 10.1136/ard.54.2.107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Oishi CS, Hoaglund FT, Gordon L, Ross PD. Total hip replacement rates are higher among Caucasians than Asians in Hawaii. Clin Orthop Relat Res. 1998;353:166–74. doi: 10.1097/00003086-199808000-00019. [DOI] [PubMed] [Google Scholar]
- 8.Lane NE, Nevitt MC, Genant HK, Hochberg MC. Reliability of new indices of radiographic osteoarthritis of the hand and hip and lumbar disc degeneration. J Rheumatol. 1993;20:1911–8. [PubMed] [Google Scholar]
- 9.Altman RD, Gold GE. Atlas of individual radiographic features in osteoarthritis, revised. Osteoarthritis Cartilage. 2007;15(Suppl A):A1–56. doi: 10.1016/j.joca.2006.11.009. [DOI] [PubMed] [Google Scholar]
- 10.Nevitt MC, Lane NE, Scott JC, Hochberg MC, Pressman AR, Genant HK, et al. Radiographic osteoarthritis of the hip and bone mineral density. The Study of Osteoporotic Fractures Research Group. Arthritis Rheum. 1995;38:907–16. doi: 10.1002/art.1780380706. [DOI] [PubMed] [Google Scholar]
- 11.Croft P, Cooper C, Wickham C, Coggon D. Defining osteoarthritis of the hip for epidemiologic studies. Am J Epidemiol. 1990;132:514–22. doi: 10.1093/oxfordjournals.aje.a115687. [DOI] [PubMed] [Google Scholar]
- 12.Korean Statistical Information Service. [Accessed 07/11/2007];Korean Census. 2000 < http://www.kosis.kr/index.html>.
- 13.Kim HA, Kim S, Seo YI, Choi HJ, Seong SC, Song YW, et al. The epidemiology of total knee replacement in South Korea: national registry data. Rheumatology (Oxford) 2008;47:88–91. doi: 10.1093/rheumatology/kem308. [DOI] [PubMed] [Google Scholar]
- 14.Robertsson O, Knutson K, Lewold S, Lidgren L. The Swedish Knee Arthroplasty Register 1975–1997: an update with special emphasis on 41,223 knees operated on in 1988–1997. Acta Orthop Scand. 2001;72:503–13. doi: 10.1080/000164701753532853. [DOI] [PubMed] [Google Scholar]
- 15.Malchau H, Herberts P, Eisler T, Garellick G, Söderman P. The Swedish total hip replacement register. J Bone Joint Surg Am. 2002;84-A(Suppl 2):2–20. doi: 10.2106/00004623-200200002-00002. [DOI] [PubMed] [Google Scholar]
- 16.Lau EM, Lin F, Lam D, Silman A, Croft P. Hip osteoarthritis and dysplasia in Chinese men. Ann Rheum Dis. 1995;54:965–9. doi: 10.1136/ard.54.12.965. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Yoshimura N, Campbell L, Hashimoto T, Kinoshita H, Okayasu T, Wilman C, et al. Acetabular dysplasia and hip osteoarthritis in Britain and Japan. Br J Rheumatol. 1998;37:1193–7. doi: 10.1093/rheumatology/37.11.1193. [DOI] [PubMed] [Google Scholar]
- 18.Kizawa H, Kou I, Iida A, Sudo A, Miyamoto Y, Fukuda A, et al. An aspartic acid repeat polymorphism in asporin inhibits chondrogenesis and increases susceptibility to osteoarthritis. Nat Genet. 2005;37:138–44. doi: 10.1038/ng1496. [DOI] [PubMed] [Google Scholar]
- 19.Kaliakatsos M, Tzetis M, Kanavakis E, Fytili P, Chouliaras G, Karachalios T, et al. Asporin and knee osteoarthritis in patients of Greek origin. Osteoarthritis Cartilage. 2006;14:609–11. doi: 10.1016/j.joca.2005.10.012. [DOI] [PubMed] [Google Scholar]
- 20.Mustafa Z, Dowling B, Chapman K, Sinsheimer JS, Carr A, Loughlin J. Investigating the aspartic acid (D) repeat of asporin as a risk factor for osteoarthritis in a UK Caucasian population. Arthritis Rheum. 2005;52:3502–6. doi: 10.1002/art.21399. [DOI] [PubMed] [Google Scholar]
- 21.Rodriguez-Lopez J, Pombo-Suarez M, Liz M, Gomez-Reino JJ, Gonzalez A. Lack of association of a variable number of aspartic acid residues in the asporin gene with osteoarthritis susceptibility: case–control studies in Spanish Caucasians. Arthritis Res. 2006;8:R55. doi: 10.1186/ar1920. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Mototani H, Mabuchi A, Saito S, Fujioka M, Iida A, Takatori Y, et al. A functional single nucleotide polymorphism in the core promoter region of CALM1 is associated with hip osteoarthritis in Japanese. Hum Mol Genet. 2005;14:1009–17. doi: 10.1093/hmg/ddi093. [DOI] [PubMed] [Google Scholar]
- 23.Loughlin J, Sinsheimer JS, Carr A, Chapman K. The CALM1 core promoter polymorphism is not associated with hip osteoarthritis in a United Kingdom Caucasian population. Osteoarthritis Cartilage. 2006;14:295–8. doi: 10.1016/j.joca.2005.11.001. [DOI] [PubMed] [Google Scholar]
- 24.Zhang Y, Hunter DJ, Nevitt MC, Xu L, Niu J, Lui LY, et al. Association of squatting with increased prevalence of radiographic tibiofemoral knee osteoarthritis: the Beijing Osteoarthritis Study. Arthritis Rheum. 2004;50:1187–92. doi: 10.1002/art.20127. [DOI] [PubMed] [Google Scholar]