Abstract
The concept of schizotypy represents a rich and complex psychopathology construct. Furthermore, the construct implies a theoretical model that has considerable utility as an organizing framework for the study of schizophrenia, schizophrenia-related psychopathology (eg, delusional disorder, psychosis-NOS (not otherwise specified), schizotypal, and paranoid personality disorder), and putative schizophrenia endophenotypes as suggested by Rado, Meehl, Gottesman, Lenzenweger, and others. The understanding (and misunderstanding) of the schizophrenia-related schizotypy model, particularly as regards clinical illness, as well as an alternative approach to the construct require vigilance in order to ensure the methodological approach continues to yield the fruit that it can in illuminating the pathogenesis of schizophrenia-related psychopathology. The articles in the Special Section in this issue of Schizophrenia Bulletin highlight methodological and theoretical issues that should be examined carefully.
Key words: schizotypy, schizophrenia, endophenotype, liability, latent structure, schizotype
Introduction
The concept of schizotypy represents a rich and complex construct. Furthermore, it implies a theoretical model that has considerable utility as an organizing framework for the study of schizophrenia, schizophrenia-related psychopathology (eg, delusional disorder, psychosis-NOS (not otherwise specified), schizotypal, and paranoid personality disorder), and putative schizophrenia endophenotypes, a view I have advocated for several decades.1–6 The leverage provided by the schizotypy model, especially as advocated by Meehl,7–9 for understanding schizophrenia and its pathogenesis has been shown to be appreciable. Moreover, the schizotypy model has helped to adjust the phenotypic boundaries of schizophrenia phenotype in the Diagnostic and Statistical Manual of Mental Disorders (DSM)-5 (eg, schizotypal pathology is now included with schizophrenia). Illuminating the nature of schizotypy may aid in unraveling the current puzzle of the very low conversion to schizophrenia rates seen in “prodromal” schizophrenia research.10 Finally, I have argued that the schizotypy framework may be useful in understanding configurations of genes relevant to schizophrenia variants4 (pp. 234-235), an idea that is beginning to gain traction.11 There is no doubt that incorporation of schizotypy indicators into genomic studies of schizophrenia increase their statistical power. The advantages of a cleaner unit of analysis (the schizotype) free from the effects of medication, institutionalization, and neurocognitive decline are axiomatic. However, the understanding (and misunderstanding) of the schizotypy model as well as alternative approaches to the construct require vigilance in order to ensure the approach continues to yield the fruit that it can.
When Drs Debbané and Mohr invited me to comment on the conference proceedings articles in this Special Section of Schizophrenia Bulletin, all of which hail from a conference held in 2013 in Switzerland, it gave me reason to reflect on the earlier NATO Scientific Workshop on schizotypy held in 1993 in Italy. That NATO workshop helped to chart a research agenda that has continued to yield fruit,12 some of which is reflected in these articles written some 20 years later. At that time, we were exploring the nexus of schizotypic pathology (notably schizotypal personality) and schizophrenia, with an eye toward accruing empirical laboratory data that bridged the 2 domains of pathology and suggesting a common underlying liability (ie, schizotypy). At that meeting there were present both schizotypy and schizophrenia researchers probing these issues (eg, J. Asarnow, R. Asarnow, R. Cancro, T. Cannon, L.J. Chapman, J.P. Chapman, G. Claridge, P.S. Holzman, M.F. Lenzenweger, S. Mednick, A. Raine, L.J. Siever, P. Venables, and others). One of the principal foci at the North Atlantic Treaty Organization (NATO) meeting was the latent structure of schizotypy, but many articles concerned the neurocognitive, neuroimaging, and neurobiological approaches as well as longitudinal outcome.12 The bridge between schizotypic psychopathology and schizophrenia as a theme reverberated throughout. The participants in the 2013 Lemanic Workshop on Schizotypy have produced a creditable set of articles following in this tradition. The conference proceedings in this issue build nicely upon the work discussed in 1993 and they offer useful vectors for continued research in the years to come. They also illustrate some of the problems faced in this area, particularly insofar as schizotypy is conceptualized.
My primary objectives are to (1) to provide a context or vantage point from which to view these articles (or, to pose questions the reader should ask about these articles), (2) point to areas of misunderstanding regarding what schizotypy is and is not, and (3) highlight interesting features of this set of articles within the overall schizotypy framework. The main points for the reader to take away from these articles are as follows. First, the study of schizotypic psychopathology provides considerable leverage on achieving a better understanding of the full range of manifestations of schizophrenia liability (beyond flagrant positive or negative symptoms in clinical disease states). Second, schizotypic psychopathology, as I have argued elsewhere, is not an analog condition that is used as a proxy for schizophrenia, rather it is a genuine manifestation of schizophrenia liability, and worthy of study in its own right. Third, the study of nonpsychotic schizotypic persons will continue to provide an organizing framework3–5 for genomic investigations related to schizophrenia and may come to help to illuminate the nature of “prodromal” cases that do not convert to schizophrenia (which is the vast majority of such cases, 70% or more). Finally, the study of schizotypes is not simply something done by university professors who lack access to schizophrenia patient populations (as one sometimes hears), rather the study of schizotypy represents a methodological and substantive research vector central to a full understanding of schizophrenia liability consistent with over 100 years of discussion, beginning with Kraepelin13 and Bleuler14 and continuing through Rado,15 Meehl,7,8 and others.
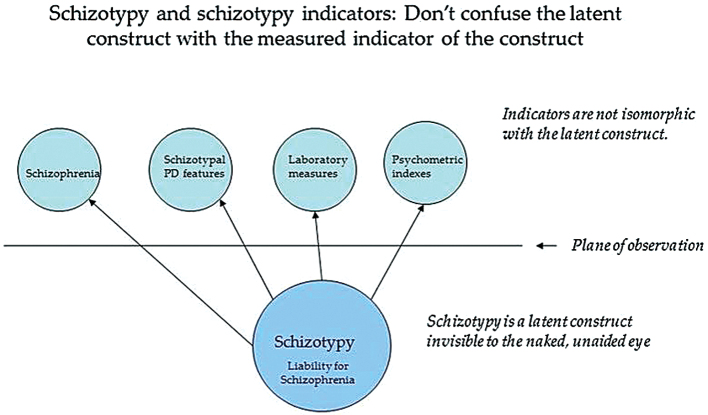
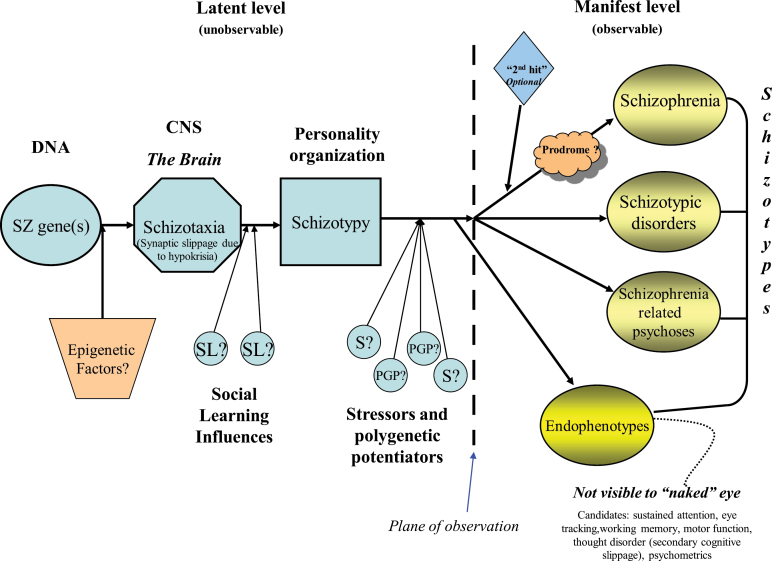
A focus on schizotypy in schizophrenia research is not new. For example, Kraepelin13 (p. 234) and Bleuler14 (p. 239) made note of what they termed “latent schizophrenia,” a personality aberration regarded as a quantitatively less severe expression of the clinical illness schizophrenia. Interestingly, Kraepelin and Bleuler believed that the signs and symptoms of the so-called latent schizophrenia were in fact continuous with the “principal malady” 13 (p. 234) or “manifest types of the disease” 14 (p. 239), respectively. They13,14 presaged the notion of a latent liability that underpins both flagrant psychosis as well as other schizophrenia-related variants. Bleuler actually suggested that nonpsychotic schizotypic pathology might be the most common expression of schizophrenia liability when he noted, “There is also a latent schizophrenia, and I am convinced that this is the most frequent form, although admittedly these people hardly ever come for treatment ...In this form we see in nuce all the symptoms and all combinations of symptoms which are present in the manifest types of the disease”14 (p. 239). As is well-known, Rado15 and, later, Meehl7,8 advocated that schizotypy represents a construct that harbors the latent liability for schizophrenia and related pathologies (see figure 1). Meehl was prescient in his proposals that essentially created the “diathesis-stressor model” in which a genetically influenced etiology for schizophrenia played itself out from DNA through neural functioning to a personality organization, an organization that could yield alternative variants of schizotypic outcomes ranging from clinical schizophrenia to subtle endophenotypic16,17 abnormalities detected through laboratory methods (see figure 2 for a model that incorporates these notions). Meehl’s model is not reviewed here in detail (see figure 2 caption for overview); the interested reader is referred elsewhere.7–9 It is important to bear in mind that Meehl’s model argued that one either harbored the liability for schizophrenia or one did not (ie, a categorical perspective). However, his model, even when positing multiple schizophrenia-related loci,18 is also congenial with a threshold effect model19 as well as is consistent with the possibility of different “types” or variants of schizophrenia (perhaps reflective of different configurations or combinations of schizophrenia-related genetic loci).11
Fig. 1.
This depicts the relationship between the latent construct schizotypy and indicators of schizotypy, such as clinical, psychometric, and laboratory measures. One should not speak of observed indicators of the latent construct as schizotypy, eg, schizotypal personality disorder features should be described as a schizotypy indicator. Copyright © 2010 by Mark F. Lenzenweger. Used with permission of the author.
Fig. 2.
Developmental model relating the genetic diathesis for schizophrenia, schizotaxia, and schizotypy and implied levels of analysis (inspired by Meehl7,8), with modifications by Lenzenweger4. Those factors to the left of the vertical broken line (ie, plane of observation) are “latent” and therefore unobservable with the unaided naked eye, whereas those factors to the right of the plane of observation are manifest (or observable). A DNA-based liability—primary synaptic slippage (embodied in Meehl’s hypothetical process denoted “hypokrisia”)—creates impaired CNS-based neural circuitry (schizotaxia) that eventuates in a personality organization (schizotypy) that harbors the liability for schizophrenia. Meehl7,8 viewed the genetically determined liability to be entirely taxonic in nature (ie, present or absent). However, this liability could also be determined by a confluence of genetic factors, probably many in number and of small effect, that have summed to pass a critical threshold (perhaps as many as 108 loci contribute to this liability, Schizophrenia Working Group of the Psychiatrics Genomics Consortium18). The “synaptic slippage” in this model is consistent with modern day concepts as diminished synaptic connectivity, abnormal connectivity, cognitive dysmetria, and so on. Social learning (SL) schedules interact with schizotaxia to yield schizotypy. Psychosocial stressors (S) and polygenic potentiators (PGP) interact with schizotypy to yield manifest outcomes across a range of clinical compensation. Various possible manifest developmental outcomes include schizophrenia (which may involve an optional “second hit,” eg, in utero exposure to maternal influenza), schizotypic psychopathology (eg, schizotypal and/or paranoid personality disorders), or schizophrenia-related psychoses (eg, delusional disorder). So-called “prodromal features” (withdrawal, reduced ideational richness, disorganized communication) may precede the onset of some (but not all) cases of schizophrenia. Endophenotypes (eg, sustained attention deficits, eye tracking dysfunction, working memory impairments, motor dysfunction, thought disorder (secondary cognitive slippage), and/or psychometric deviance (PAS); see Gottesman and Gould16), which are invisible to the unaided, “naked” eye (but detectable with appropriate technologies), are found below the plane of observation. Epigenetic factors refer to nonmutational phenomena, such as DNA methylation and histone acetylation (modification), that alter the expression of the schizophrenia gene (or genes). For example, there is the possibility that a hypermethylation process may serve to downregulate genes of relevance to schizophrenia. All individuals represented across this range of manifest outcomes are considered “schizotypes,” which does not necessarily imply an International Classification of Diseases (ICD) or DSM diagnosis. Finally, if there are genetically distinct variants of schizophrenia (Arnedo et al11), then each variant could follow a distinct developmental pathway comparable to that shown here but with different causal factors playing different roles across the variants. ©2010M.F. Lenzenweger, and used with permission.
Questions to Ponder Vis-a-Vis the Special Section Articles
The articles in this Special Section cover a diverse terrain, describing empirical studies from different theoretical and methodological perspectives. There are several matters to bear in mind when considering this collection of reports.
How is the Construct of “Schizotypy” Defined in these Articles? Is There a Consistent Definition Across Articles?
Schizotypy is defined variously in the articles in this Special Section and, importantly, the role of schizotypy in the pathogenesis of schizophrenia-related psychopathology described in these articles varies as well. This variation, on the one hand, could be viewed as vibrant diversity in discourse, on the other hand, it could be viewed as suggesting conceptual confusion that could challenge the reader.
Schizotypy in this set of articles is defined variously as a “risk factor” (Barrantes-Vidal et al; Herzig et al), a “set of commonly occurring personality traits” (Cohen et al), a “mediator” between early risk factors and high-risk states (Debbane and Barrantes-Vidal), a construct with apparent phenomenological overlap with schizophrenia (Ettinger et al), a “trait personality” construct (Fonseco-Pedrero et al), a measure of “healthy potential” (Mohr and Claridge), and set of enduring traits and phenotypic expression of the familial-genetic liability to schizophrenia (Wang et al). Each of these descriptions of schizotypy implies notable differences in the nature of schizotypy, but, more importantly, differences in the role of schizotypy in the nomological network linking schizotypy to its observable behavioral, neurocognitive, and/or psychopathological referents. Kwapil and Barrantes-Vidal advocate a position that places schizotypy within a network that links the construct to its schizophrenia-related outcomes. Their position bears similarity to a model I have advocated over the past several decades.1–5
Clearly, the schizotypy construct plays very different roles in the models advocated (either implicitly or explicitly) by these authors. One must therefore take care to distinguish between the hypothesized definitions and functions of schizotypy as (1) “personality organization that harbors the liability for schizophrenia,” (2) risk factor for schizophrenia, (3) a mediator between influences for schizophrenia and the clinical disorder, or (4) a “collection of personality traits.”
If a “Continuous” Model of Schizotypy Is Proferred, What Empirical Evidence Is Given in Support of the Continuous Model? (or, the “Latent Structure” Issue)
Some researchers have concluded that schizotypy, as a construct, has a continuous (quantitative) latent structure, suggesting that it is not qualitative (categorical), nor does it show marked threshold effects. The data in support of this position are thin. More importantly, this matter is an empirical question that should be resolved by statistical methods designed to illuminate the issue. It is not resolved through theoretical assertions or faulty inferences from phenotypic data. In some instances, it seems that phenotypic continuity is taken to imply quantitative latent variation. First and foremost, it is not the case that continuous phenotypic measurement implies continuity or quantitative variation in the latent construct.
In other instances, the assumption of latent continuity characterizing schizotypy has followed from inferences that cannot resolve or speak to the latent structure matter. In this vein, it is incorrect to assume the occurrence of psychotic-like experiences (PLE) in general population samples (in the absence of clinical schizophrenia) implies continuity in the latent schizotypy construct. There could be many reasons for people to report PLEs in the general population—ranging from liability to schizophrenia, liability for bipolar illness, through anxiety states, borderline personality disorder, drug-related experiences, alcohol-related experiences, religious experiences, sleep paralysis, and so on. That one can find PLEs amongst individuals in the general population does not necessarily tell us anything about the latent structure of schizophrenia liability. Consider some thought exercises. Imagine we are interested in viral spinal meningitis, which is associated with high fever. We could easily find a range of levels of elevated body temperatures (fever) in people drawn from the general population for any number of reasons (eg, influenza, common cold, Lyme disease, and so on), but such instances of fever (phenotypic quantitative variation) would not imply that the latent structure of the cause of spinal meningitis was continuous in nature. Consider the latent structure of the cognitive vulnerability to panic disorder, which includes attention to bodily sensations and appears to be taxonic in latent structure.20 Is it the case that finding instances of concern or worry over the meaning of odd physical sensations in the general population means that the cognitive liability for panic is continuous? No. A final example, one could construct a quantitative measure of “maleness/femaleness” and, indeed, acquire “dimensional” values on the “maleness/femaleness scale.” However, the continuous variation in the scores on this scale would not mean that biological sex has a continuous (quantitative, “difference by degree”) nature at the latent level. Similarly, finding instances of unusual thought content or PLEs in the general population does not necessarily mean that schizotypy, or the latent structure of schizophrenia liability, is continuous. One can surely measure a psychopathological feature, symptom, or character in a quantitative manner, but that, in and of itself, does not ensure or mean that the construct measured is dimensional at the latent level.
In point of fact, the vast majority of empirical results, using proper data analytic methods up to the job (eg, taxometric methods, finite mixture modeling) support the existence of a qualitative (ie, categorical) latent structure underlying schizotypy (4,5; see below). Depending on the manner in which one counts investigations, studies favoring a qualitative discontinuity underpinning schizotypy far outnumber studies that do not find such evidence occur at rates of anywhere between 10:1 to 3:1. Whether this qualitative discontinuity reflects a true typological distinction or a steep/severe jag on a schizophrenia liability continuum remains to be clarified. Factor analytic results from multivariate arrays of schizotypy indicators have no probative value with respect to the qualitative vs. quantitative latent structure issue.
Which Theoretical Model Is Used to Guide Subject Group Composition and to Direct Data Analysis in a Schizotypy Study? Do These Methodological and Statistical Procedures Accord Well With the Substantive Model Guiding the Work?
If an investigator holds a dimensional/continuous view of schizotypy, are the subjects in a study contained within a single sample for continuous data analysis? In fact, are statistical procedures associated with continuous data being employed in the data analyses (eg, correlations, multiple regression)? If the authors compose distinct subject groups (eg, high schizotypy vs low schizotypy), does that methodological decision accord better with the assumptions of a dimensional or categorical model? If one sees schizotypy as a continuum, would it not make sense to analyze the data continuously rather than culling out high vs low scorers (an approach often associated with the identification of a class of persons of interest)?
In Cases Where a Quantitative Measure Is Used to Tap Schizotypy, How Are High and Low Scores on the Schizotypy Measure Interpreted?
Essentially all psychometric measures of schizotypic features in current common use are unipolar in nature. This means that low scores represent the relative absence of deviance on the pathological construct of schizotypy, whereas elevated scores (deviance) suggest the presence of the pathological construct (or high levels of it). It is a conceptual mistake to suggest that relatively low scores on a measure of schizotypy represent “psychological health,” rather they only suggest absence of schizotypy-related deviance (see21 for rich discussion). For example, low scores on a depression measure only suggest the absence of depression, they do not suggest happiness or emotional health. Schizotypy measures are not bipolar in nature such that low scores represent a domain of healthy, psychologically adaptive functioning. In other words, the available psychometric measures tap only half of the Gaussian distribution, really just the pathological right tail. Scores at the low end of schizotypy measure are less informative in both substantive and psychometric terms,21 thus claims of “health” or “happiness” linked to low schizotypy scores are not well substantiated.
In a related vein, given that all psychopathology measurements (psychometric and otherwise) contain some degree of error and that no psychological or psychiatric measurement system carves the domain of psychological experience perfectly, it is to be expected that some persons may obtain elevated scores on such measures for reasons unrelated to the intended construct that is tapped. Thus one might occasionally find persons scoring higher on a measure of schizotypy, but such persons are not necessarily true-positives, so to speak, but could be false-positives.
Is It the Case That All Persons Who Score High on a Measure of Schizotypy Are Destined to Develop Schizophrenia?
This is clearly not the case, but this is a common misunderstanding of the schizotypy model and research framework. Only a fraction of those persons who have high scores on a schizotypy measure are destined to develop schizophrenia, another schizophrenia-related psychotic illness, or a diagnosable schizotypic disorder of another sort. This is not unlike the situation in the Ultra High-Risk paradigm where the vast majority of “prodromal” cases do not convert to schizophrenia, yet they are plausibly at risk for the illness. Similarly, not all children at risk for schizophrenia (genetic high-risk research) by virtue of having a schizophrenia affected biological parent will develop the illness. The reader of a schizotypy research report must bear these constraints on prediction in mind when considering the likely psychiatric outcome of schizotypic subjects as well.
On the Multidimensionality of Schizotypic Manifestations
A number of the articles in the Special section highlight the “multidimensionality” of schizotypy. Such empirical support for the multidimensionality of schizotypy accords well with what has long been known from both the theoretical and clinical perspectives. For example, Rado implicitly argued for at least 2 dimensions of schizotypy, Meehl embodied the very notion of multidimensionality in his famous Checklist for Schizotypic Signs that contained 25 features that were rated continuously. Factor analytic results of multiple diverse psychometric schizotypy indicators, for example, should support multidimensionality (factor analysis must extract factors and the larger the number of indicators, the more factors tend to be extracted). The reader should not, however, confuse evidence for multidimensionality with evidence supportive of continuity in the latent structure of schizotypy. Extraction of multiple dimensions of schizotypy from a multivariate array of schizotypy indicator data cannot differentiate between continuity or discontinuity at the latent level.
Maintain Clarity on Levels of Analysis: Indicators Vs Latent Constructs
Not all of the contributors to this Special Section have maintained clarity in discussing the distinction between phenotypic indicators and the latent construct giving rise to those indicators. In short, do not mistake the latent construct of schizotypy per se with its phenotypic manifestations or endophenotypic manifestations (see figure 1)—they are not isomorphic. Relatedly, as suggested previously, do not assume continuous measurement at the phenotypic indicator level (eg, psychometric index scores) implies quantitative variation at the latent level. Moreover, if there is quantitative variation at the latent level, do not assume it’s nature is necessarily similar to the same scaling used in measurements at the phenotypic level.
Schizotypy as a Schizophrenia-Related Latent Construct Vs Schizotypy as a Personality Trait Without a Schizophrenia-Related Basis
Most researchers in psychopathology hold the view that schizotypy is a construct that is intimately connected to a schizophrenia-related liability. This view has a long history dating from Kraepelin and Bleuler, through Rado and Meehl, and continues with many contemporary workers (including the present author). This view stands in opposition to a view that schizotypy is a normal range personality construct without a schizophrenia-liability connection. Some of the articles in the Special Section are based on the “schizotypy as normal personality dimension” model, a view frequently advanced by Claridge22 and others. This is a not a trivial difference in perspective and it should be unpacked for consideration. I have discussed this issue in considerable detail elsewhere.4,5
The view that schizotypy is a dimension of normal personality frequently suggests that schizotypy is a “benign” or “healthy” component of personality. To distinguish it from schizotypy as related to schizophrenia liability it can be referred to as “benign schizotypy” (BS) for purposes of discussion. The core propositions of the BS approach to schizotypy are as follows: (1) schizotypy is part of normal personality, (2) schizotypy expresses itself in “healthy” manifestations, and (3) schizotypy has a dimensional (quantitative) structure at the latent level.
As summarized recently by Rawlings, Williams, Haslam, & Claridge,23 “Claridge and his colleagues have investigated schizotypy from many points of view. They have concluded that psychotic traits constitute an essentially healthy dimension of personality (italics added), which in adaptive form contributes to psychological variations as creativity, nonthreatening hallucinations, and rewarding spiritual and mystical beliefs and experiences.”23 (p. 1670). The BS view of schizotypy as a normal personality trait varying by degree along a continuum adheres to both Eysenck’s methodological view of personality measurement as well as Eysenck’s conceptualization of “psychoticism” as a personality trait (Eysenck was Claridge’s mentor). Beyond a methodological preference for dimensions, what evidence is given that one should adopt the BS model (schizotypy as normal personality dimension) as distinct from a schizotypy as schizophrenia-liability model? One is hard pressed to find a model of “normal personality” that includes a dimension of schizotypy. Psychoticism (as a personality construct), included in early personality questionnaires (such as Eysenck’s), has essentially been abandoned in the normal personality literature as the construct was heterogeneous, largely denoting impulsivity. One does see reference to a revised variant of “psychoticism” in some contemporary measures of maladaptive personality such as the newly developed personality disorder questionnaire for DSM-5 24.
As pursued elsewhere,4,5 one must ask, what does it mean to argue that “psychotic traits constitute an essentially healthy dimension of personality”? To answer this one must consider what it means to designate an individual or behavior as “psychotic.” In traditional psychiatric usage, psychotic as a descriptive term has typically 1 of 3 potential meanings: (1) the impairment of reality testing as indicated by the presence of particular psychopathology signs and/or symptoms (hallucinations, delusions, thought disorder), (2) the depth or severity of an impairment (eg, a psychotic depression, meaning a very deep or profound case of depression) and/or, less frequently, (3) a degree of regression, within a psychodynamic framework, to a developmentally primitive stage of psychological organization wherein thought and experience are characterized by primary process (ie, not secondary process). In light of how the term psychotic is used in clinical applications and discussions, one cannot readily conceive of “psychotic traits” as being consistent with a “healthy dimension of personality?” (Resorting to the locution “psychotic-like” does not get one out of this conceptual conundrum if one is serious about the notion that psychotic traits are, in fact, representative of a healthy dimension of personality.) Those who see patients in intensive diagnostic or therapeutic capacities may find an eerie unfamiliarity in a concept such as “healthy psychotic” traits. Could one realistically speak of “healthy” schizophrenia or schizophrenia as a healthy dimension of personality? The reader of the articles in the Special Section will want to consider this issue in contemplating the 2 schizotypy models (schizophrenia-related schizotypy vs BS/”healthy psychosis”).
The third issue central to Claridge’s BS22,23 model concerns the basic nature of the construct’s latent structure. Is schizotypy quantitative in nature at both the phenotypic level and the latent level? This issue received considerable discussion during the 1993 NATO workshop.12 At that time, although adherents of the BS model maintained a strong commitment to a dimensional view, there were essentially no empirical data available to support a view that the schizotypy construct was quantitatively distributed—varying by degree (not kind)—at the latent level. All empirical evidence marshaled by BS model advocates arguing for a dimensional latent structure for schizotypy came from analytic techniques (ie, factor analysis) that could not determine whether a latent entity was quantitatively (dimensionally) or qualitatively (taxonically) structured at a deeper level. Without undertaking an extensive review here, the current empirical picture regarding the latent structure of schizotypy is one that supports discontinuity at the latent level, which is either representative of a latent taxon (class, natural subgroup) or severe step function (threshold) in the structure of the schizotypy construct. As noted above, one can surely measure a psychopathological feature, symptom, or character in a quantitative manner, but that, in and of itself, does not ensure or mean that the construct measured is dimensional at the latent level.
Caveat Emptor: Misconceptions About the Meehl Model
Many of the articles in the Special Section understandably make reference to Meehl’s well-known model of schizotypy, which is firmly rooted in a schizophrenia-liability perspective. His model has been invoked as a substantive platform for schizotypy research for over 50 years.9 At times, however, some imprecision creeps into interpretations of the Meehl model and, in light of the Special Section, it might be helpful to review several misconceptions of the model and frequent misunderstandings (see 4,5 for detail). The reader will want to be alert for the 6 issues highlighted here as one does see a lack of clarity in some discussions:
1. Meehl’s schizotypy construct is not isomorphic with the DSM-defined schizotypal personality disorder (SPD) entity. Schizotypy is a latent construct, whereas SPD is an observable phenomenological entity that can derive from schizotypy (see figures 1, 2).
2. Schizotypy, as a latent construct reflective of a personality organization that harbors the liability for schizophrenia, is known to be genetically influenced, but it is not entirely genetic in origin. It reflects input from genes (determining brain-based schizophrenia related dysfunction [termed “schizotaxia” by Meehl in figure 2]), epigenetic influences, and environmental factors (eg, social learning history).
3. For Meehl, the terms schizotype and schizotypy are not reserved only for those cases identified by DSM-defined Cluster A personality disorder features. As can be seen in figure 2, there are alternative developmental outcomes for schizotypy and these outcomes transcend the DSM nomenclature.
4. Not all schizotypes are expected to develop schizophrenia according to the Meehl model. Some schizotypes will develop (or convert to) schizophrenia, some will show some continued nonpsychotic evidence of schizotypic features across the lifespan, and some schizotypes will remain quietly nonsymptomatic (perhaps displaying evidence of their underlying personality organization on endophenotypic measures). The latter 2 theoretical possibilities are, perhaps, exemplified by the large proportion of nonconverting “prodromal” cases found in ultra high-risk studies.
5. Some observers (mis)believe that Meehl’s entire developmental model hinges on the presence of a single, schizophrenia-specific gene (a “schizogene”). We now know today that there is no single gene that causes schizophrenia. Meehl did speculate on the possibility of a “schizogene” in his early formulations (early 1960’s) and used it as starting point. However, the cascade of processes and outcomes in the model is entirely compatible with multiple genes contributing to the underlying schizotaxic brain/neural pathology, which then plays itself out developmentally as noted in figure 2 (see caption) and could incorporate a threshold effect.
6. Of critical conceptual importance, Meehl’s model does not represent a “quasi-dimensional” model as maintained in some of the articles in the Special Section. One sees reference to a differentiation advocated by Claridge22 and BS model adherents in which a so-called “fully dimensional model” of schizotypy is distinguished from what is claimed that Meehl advocated, with the assertion that Meehl’s model was/is a “quasi dimensional” model of schizotypy. In other words, it has been suggested that those advocating a model of schizotypy linked to schizophrenia-related liability are advancing a “quasi dimensional model.” This is incorrect. The schizotypy model associated with Meehl (and others holding similar views) is distinctly “nondimensional” in nature. In the Meehl model, there can be various phenotypic outcomes for the underlying schizotypic personality organization. However, these outcomes only emerge if one possesses schizotypy. Meehl7,8 himself was quite clear on this issue—he saw schizotypy as having a taxonic (qualitative) latent structure (present vs absent). Meehl did not even really entertain the notion of a threshold effect in his theorizing about the nature of schizotypy. (This is important as one could posit a threshold effect in relation to a quantitative model of liability as is done in the multifactorial polygenic threshold model of schizophrenia in which dichotomous phenotypes emerge (eg, 19).) In Meehl’s view there is no gradation or quantitative variation insofar as schizotypy is concerned. One was either a schizotype or not, there was no in-between level. The BS model advocated by Claridge,22 in contrast, advocates a fully dimensional view with continuous variation at both the latent and phenotypic levels; the BS model is most consistent with a simple polygenic model (without a threshold) that reflects a continuous additive model of genetic influences.
Future Directions: Hewing to the Schizophrenia Liability Core and Avoiding Conceptual Quicksand
Beyond Psychometrics
Let’s move beyond psychometric measures of schizotypy in future studies. Incorporation of laboratory measures of schizotypy will provide additional precision in future studies and will be useful in resolving latent structure questions.25
Parsimony in Language
I see no conceptual gain in introducing idiosyncratic concepts such as “psychometric schizotypy” or “self-report schizotypy.” If a measurement device is construct valid for the intended construct, how does the method of assessment being included in the name of the construct advance discourse? We do not speak of “structured-clinical interview depression,” “self-report panic disorder,” or “observer-rated personality disorder.”
From DNA to Social Functioning
Understand the construct of interest from the genome through its impact on occupational and social functioning. Research crossing the many levels of analysis4 from DNA, through neural circuitry and functional neuroanatomy, to neurobehavioral systems, personality functioning, on to interpersonal and social engagement is needed for schizotypy indicators of interest. At present, there may be 10818 or more genes of importance to schizophrenia liability and the clinical illness may indeed be a group of illnesses as suggested by Bleuler,11 thus creative research targeting liability defined by either summative/additive levels of these genes or configurations of these genes is warranted in the schizotypy area.
Clarity in Language in the Clinical Domain
There should be rigorous consideration of the implications of various monikers that have crept into the schizotypy discourse, such as “healthy psychosis,” “healthy schizotypy,” “dimensional psychosis,” and “benign schizotypy.” Do such terms advance the clarity of psychopathology discourse or do they represent conceptual quicksand? Do such terms make sense in light of clinical considerations and realities?
Accuracy in Model Description
Careful articulation of the nature of the model underlying one’s conceptualization of schizotypy: “dimensional” (Claridge) vs “categorical/taxonic” (Meehl) vs “threshold” (Gottesman). In this vein, it is recommended that the “fully dimensional” (Claridge) vs “quasi dimensional” dichotomy be abandoned given that it is technically inaccurate. As noted above, Meehl advocated a categorical model such that schizophrenia liability was either present or absent (originally proposing a single gene, but later willing to consider multiple genes contributing to a schizophrenia liability class or taxon). One should also consider the possibility of a threshold, severe step function, or jag in the underlying schizotypy construct (if one subscribes to a dimensional view). The seminal work of Gottesman on the multifactorial polygenic threshold model is relevant here.
Methods Should Follow the Model
One should be careful in the organization of study samples to ensure that one’s methodological approaches are consistent with one’s theoretical perspective. In short, dimensional views should correspond to dimensional subject ascertainment and continuous data analysis, whereas categorical/taxonic views should correspond to case identification and case-control data analytic methods should be used.
Concluding Comment
The articles in the Special Section represent a fascinating cross section of topics that will be of interest to many readers of the Bulletin. They build nicely upon the blueprints laid out at the 1993 NATO workshop on schizotypy. The current article provides an overview of issues that are relevant to this research area and highlight the heuristic potential of the study of schizotypy as a framework for research on schizophrenia and related psychopathologies.
Acknowledgment
The author has declared that there are no conflicts of interest in relation to the subject of this article.
References
- 1. Lenzenweger MF. Psychometric high-risk paradigm, perceptual aberrations, and schizotypy: an update. Schizophr Bull. 1994;20:121–135. [DOI] [PubMed] [Google Scholar]
- 2. Lenzenweger MF. Schizotypy and schizotypic psychopathology: Mapping an alternative expression of schizophrenia liability. In: Lenzenweger MF, Dworkin RH, eds. Origins and Development of Schizophrenia: Advances in Experimental Psychopathology. Washington, DC: American Psychological Association; 1998:93–121. [Google Scholar]
- 3. Lenzenweger MF. Schizotypy: an organizing framework for schizophrenia research. Curr Dir Psychol Sci. 2006;15:162–166. [Google Scholar]
- 4. Lenzenweger MF. Schizotypy and Schizophrenia: the View From Experimental Psychopathology. New York, NY: Guilford Press; 2010. [Google Scholar]
- 5. Lenzenweger MF. Schizotypic psychopathology: Theory, evidence, and future directions. In Blaney PH, Millon T, Krueger R, eds. Oxford Textbook of Psychopathology (3rd edn). New York, NY: Oxford University Press; 2015:729–767. [Google Scholar]
- 6. Lenzenweger MF, Loranger AW. Detection of familial schizophrenia using a psychometric measure of schizotypy. Arch Gen Psychiatry. 1989;46:902–907. [DOI] [PubMed] [Google Scholar]
- 7. Meehl PE. Schizotaxia, schizotypy, schizophrenia. Am Psychol. 1962;17:827–838. [Google Scholar]
- 8. Meehl PE. (1990). Toward an integrated theory of schizotaxia, schizotypy, and schizophrenia. J Personal Disord. 1994;4:1–99. [Google Scholar]
- 9. Lenzenweger MF. Schizotaxia, schizotypy, and schizophrenia: Paul E. Meehl’s blueprint for the experimental psychopathology and genetics of schizophrenia. J Abnorm Psychol. 2006;115:195–200. [DOI] [PubMed] [Google Scholar]
- 10. Fusar-Poli P, Borgwardt S, Bechdolf A, et al. The psychosis high-risk state: a comprehensive state-of-the-art review. JAMA Psychiatry. 2013;70:107–120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Arnedo J, Svrakic D, del Val C, Romero-Zaliz R, Hernandez-Cuervo H, Molecular Genetics of Schizophrenia Consortium et al. Uncovering the hidden risk architecture of the schizophrenias: Confirmation in three independent genome-wide association studies. Am J Psychiatry. In press; 2014. [DOI] [PubMed] [Google Scholar]
- 12. Raine A, Lencz T, Mednick S. Schizotypal Personality. New York, NY: Cambridge University Press; 1995. [Google Scholar]
- 13. Kraepelin E. Dementia Praecox and Paraphrenia (Barclay RM, Trans., Robertson GM, ed.). Huntington, NY: Krieger; 1919/1971. (Original work published 1909–1913; original translation of selected portions published 1919.) [Google Scholar]
- 14. Bleuler E. Dementia Praecox or the Group of Schizophrenias. (Zinkin J. Trans.). New York, NY: International Universities Press; 1911/1950. [Google Scholar]
- 15. Rado S. (1960). Theory and therapy: the theory of schizotypal organization and its application to the treatment of decompensated schizotypal behavior. In: Scher SC, Davis HR, eds. The Outpatient Treatment of Schizophrenia. New York, NY: Grune and Stratton; 1960:87–101. [Google Scholar]
- 16. Gottesman II, Gould TD. The endophenotype concept in psychiatry: etymology and strategic intentions. Am J Psychiatry. 2003;160:636–645. [DOI] [PubMed] [Google Scholar]
- 17. Lenzenweger MF. Thinking clearly about the endophenotype-intermediate phenotype-biomarker distinctions in developmental psychopathology research. Dev Psychopathol. 2013;25:1347–1357. [DOI] [PubMed] [Google Scholar]
- 18. Schizophrenia Working Group of the Psychiatric Genomics Consortium. (2014). Biological insights from 108 schizophrenia-associated genetic loci. Nature. 2014;511:421–427. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Gottesman II. Schizophrenia Genesis: The Origins of Madness. New York, NY: W.H. Freeman; 1991. [Google Scholar]
- 20. Schmidt NB, Kotov R, Lerew DR, Joiner TE, Ialongo NS. Evaluating latent discontinuity in cognitive vulnerability to panic: a taxometric investigation. Cognitive Therapy. 2005; 29:673–690. [Google Scholar]
- 21. Reise SP, Waller NG. Item response theory and clinical measurement. Annu Rev Clin Psychol. 2009;5:27–48. [DOI] [PubMed] [Google Scholar]
- 22. Claridge G. Theoretical background and issues. In: Claridge G. ed., Schizotypy: Implications for Illness and Health. Oxford, UK: Oxford University Press; 1997: 3–18. [Google Scholar]
- 23. Rawlings D, Williams B, Haslam N, Claridge G. Taxometric analysis supports a dimensional latent structure for schizotypy. Person Indiv Differ. 2008;44:1640–1651. [Google Scholar]
- 24. Krueger RF, Derringer J, Markon KE, Watson D, Skodol A. Initial construction of a maladaptive personality trait model and inventory for DSM-5. Psychol Med. 2012;42:1879–1890. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Lenzenweger MF, McLachlan G, Rubin DB. Resolving the latent structure of schizophrenia endophenotypes using expectation-maximization-based finite mixture modeling. J Abnorm Psychol. 2007;116:16–29. [DOI] [PubMed] [Google Scholar]