Abstract
Structured clinical data generated using standardized terminologies such as the Omaha System are available for evaluating health care quality and patient outcomes. New intervention management grouping approaches are needed to deal with large, complex clinical intervention data sets. We evaluated 56 intervention groups derived using four data management approaches with a data set of 165,700 interventions from 14 home care agencies to determine which approaches and interventions predicted hospitalizations among frail (n=386) and non-frail (n=1,364) elders. Hospitalization predictors differed for frail and non-frail elders. Low frequencies in some intervention groups were positively associated with hospitalization outcomes, suggesting that there may be a mismatch between the level of care that is needed and the level of care that is provided.
Keywords: Systems research/patterns of care, nursing care/interventions, homecare, computers/technology, statistical test development/refinement
Intervention effectiveness research is pivotal to implementing evidence-based practice in nursing and maximizing nursing-care influence on patient outcomes. However, most home care intervention effectiveness research continues from a black box perspective, which lacks detailed descriptions of the discrete, granular actions that co-occur during various points over an episode of care. With the rapid adoption of electronic health records, structured data are becoming available as a valuable resource for such research. Because nursing interventions are multi-dimensional and complex, the development of data management approaches (methods of meaningfully categorizing raw intervention data) is a fundamental requirement for use of the data in statistical models for analyzing patient outcomes from various interventions.
Two of the important concepts emerging in home care research are unplanned hospitalizations occurring during an episode of home care services and frailty of elderly home care clients (Bauer, Fitzgerald, Haesler, & Manfrin, 2009; Gobbens, Luijkx,Wijnen-Sponselee, & Schols, 2010; Peikes, Chen, Schore, & Brown, 2009). In a meta-analysis of 71 studies in home health care, the annual hospitalization rates for elders ranged from 14% to 20% (Miller & Weissert, 2001). In a recent study, Westra and colleagues (in review) found that the hospitalization rate was much higher for the oldest old (26.5%) or the disabled (51.9%). This finding is congruent with the literature (Levinson, 2006).
There is a critical need to better understand the relationships between complex home care nursing interventions and hospitalization outcomes for frail elderly home care clients. The overall purpose of this project was to develop and compare approaches for managing clinical intervention data (Phase I) and to employ the approaches in models linking interventions to patient outcomes (Phase II). In Phase I, we developed four data management approaches and compared their advantages and disadvantages in representing home care nursing interventions (Monsen, Westra, Yu, Ramados, & Kerr, 2009). The purpose of this paper is to describe our findings from Phase II, in which we modeled the associations of intervention groups, formed by the four approaches from Phase I, with hospitalization outcomes. The aims of Phase II were to:
Compare the ability of four intervention data management approaches to explain hospitalization outcomes for frail and non-frail elders separately.
Identify intervention groups associated with hospitalization for frail elders and non-frail elders.
Background
In this project, we employed intervention and outcome data generated by clinical documentation based on the Omaha System (Martin,2005), a standardized interface terminology that has been used extensively in home care settings (Martin, 2005; Martin & Scheet, 1992). During Phase I, we developed four meaningful, replicable approaches for managing raw intervention data: action category, theoretical, clinical expert consensus, and data-driven. When applied to a data set, each data management approach generates several intervention groups. The intervention groups were derived deductively for the action category, theoretical, and clinical expert consensus approaches, but they were derived inductively for the data-driven approach. Although some commonalities in intervention groups exist across the four data management approaches, operationally these approaches are four unique ways of categorizing clinical data. During Phase II, we modeled the four approaches with hospitalization outcomes for frail and non-frail elders because hospitalization is an important outcome for home care.
Four Data Management Approaches
Each of the four data management approaches was applied to an Omaha System intervention data set; thus Omaha System terms were foundational to the four approaches. For the action category approach, we used the four Omaha System category terms: teaching, guidance, and counseling; treatments and procedures; case management; and surveillance. Teaching, guidance and counseling is defined as activities designed to provide information and materials, encourage action and responsibility for self-care and coping, and assist the individual/family/community to make decisions and solve problems. Treatments and procedures is defined as technical activities such as wound care, specimen collection, resistive exercises, and medication prescriptions that are designed to prevent, decrease, or alleviate signs and symptoms of the individual/family/community. Case management is defined as activities such as coordination, advocacy, and referral that facilitate service delivery, improve communication among health and human service providers, promote assertiveness, and guide the individual/family/community toward use of appropriate resources. Surveillance is defined as activities such as detection, measurement, critical analysis, and monitoring intended to identify the individual/family/community's status in relation to a given condition or phenomenon (Martin, 2005, p. 373). This approach generated four deductively derived, mutually exclusive groups. Our assumptions underlying the action category approach were that there are four types of actions that may differentially affect outcomes; these four actions are the important aspects of the intervention.
For the theoretical approach, we employed a theory-based algorithm to generate intervention groups. The algorithm was developed for a previous family home visiting study based on a theoretical framework derived from a randomized trial of maternal-child intervention effectiveness (Barnard et al., 1988; Monsen, 2006). When applied to Omaha System intervention data, the algorithm assigns each intervention to a theoretically-based intervention group. For example, each teaching, guidance, and counseling intervention could be translated to an informing, supporting, or providing therapy intervention, based on the combination of problem and action terms. This approach generated five deductively derived, mutually exclusive groups. Our assumptions underlying the theoretical approach were that standardized clinical data can be used to operationalize and test a theoretical framework (Monsen et al., 2009).
For the clinical expert consensus approach we created a new clinical expert consensus algorithm by conceptualizing home care practice priorities using a method developed by Agency for Health Care Quality (AHRQ, 2008). Instead of looking at problems and actions separately as in the action category approach, this algorithm linked each intervention's action terms with patient problems, expanding the number of intervention groups from four in the action category approach to 23 in the clinical expert consensus approach. For example, the clinical expert consensus approach has several surveillance groups (e.g. monitoring injury prevention) vs. one surveillance group in the action category approach. When applied to Omaha System intervention data, the algorithm assigns each intervention to a clinical expert consensus intervention group. This approach generated 23 deductively derived, mutually exclusive groups. Our assumptions underlying the clinical expert consensus approach were that there are 23 types of actions for specific problems that may differentially affect outcomes (Monsen et al., 2009).
For the data-driven approach, we grouped co-occurring interventions inductively to reveal hidden patterns in the data, using data mining methods (K-means and Estimation Maximization). Such data-intensive scientific discovery uses computing to gain understanding from stored electronic health data, and has been used in previous intervention clustering studies (Hey, Tansley, & Tolle, 2009; Monsen, Banerjee, & Das, 2010). We then qualitatively interpreted the meanings of the data-driven groups, reaching consensus among clinical experts (the authors). We named each of intervention groups to reflect the diverse intervention content of problems and actions within the group. For example, assistance with medications and homemaking consisted of interventions for numerous problems and actions, including treatments and procedures, case management, and surveillance actions for the Residence and Medication reguneb problems. This approach generated 24 overlapping groups. Our assumptions underlying the data-driven approach were: the combination of problem, category, and target intervention terms is the fundamental unit of analysis for the intervention; each intervention may uniquely affect outcomes; unique interventions may co-occur in more than one group of interventions; and co-occurrence of interventions may uniquely affect outcomes (Monsen et al., 2009).
Hospitalization in Frail Home Care Elders
Hospitalization is defined as admission to a hospital for at least 48 hours during an episode of home care, regardless of the length of the care episode or the reason for hospitalization (Shaughnessy et al., 2002). Nationally, 29% of home care patients experience hospitalization (Briggs, 2006; Centers for Medicare & Medicaid Services, 2008). Because home care patients differ greatly in age and disease complexity, hospitalization rates may vary for frail and non-frail elders.
Frailty was defined by Gobbens and colleagues (2010) as “a dynamic state affecting an individual who experiences losses in one or more domains of human functioning (physical, psychological, social) that are caused by the influence of a range of variables and which increases the risk of adverse outcomes” (p. 85). Westra and colleagues (in review) used latent-class analysis to determine unique groups of patients with differing rates of hospitalization, congruent with the literature (Gobbens et al.). Hospitalization was determined using the Outcome and Assessment Information Set (OASIS) variable indicating that the patient was transferred to the hospital during an episode of care. The probabilities of correctly classifying patients into Class I (frail elders) was 92% and into Class II (non-frail elsers) was 97%. Class I patients had a hospitalization rate of 51.9% and Class II patients had a hospitalization rate of 26.5%. Table 1 presents results of significant variables occurring in physical, psychological, and social domains. Because frail and non-frail elders differ, it is likely that nursing interventions to prevent hospitalization for non-frail elders are different from those required by frail elders.
Table 1.
Differences between Frail and Non-frail Elderly Patients
| Variable | Frail elderly | Non-frail elderly |
|---|---|---|
| n = 386 (22%) | n = 1,364 (78%) | |
| Hospitalized | 52% | 27% |
| Prognosis | ||
| Poor or fair | 59% | 23% |
| Good | 41% | 78% |
| Cognitive Functioning | ||
| Alert and oriented | 43% | 83% |
| Requires prompting | 32% | 13% |
| Requires assistance or direction | 14% | 3% |
| Requires considerable assistance / totally dependent | 11% | 1% |
| Management of oral medications | ||
| No medication or takes independently | 5% | 57% |
| Takes if prepared or reminded | 33% | 41% |
| Requires administration by others | 61% | 3% |
| Activities of daily living [n, (S.D.)] | ||
| Activities of daily living (ADLs) a | 14.6 (5.6) | 5.6 (3.4) |
| Instrumental activities of daily living (IADLs) b | 13.5 (2.2) | 7.9 (2.6) |
| Lives alone | 5% | 42% |
| Assisting person resides in home | 81% | 50% |
| Urinary incontinence or urinary catheter | 59% | 32% |
ADL Dependency, minimal (1-5), moderate (6-10), substantial (11 - 20), severe (>20)
IADL Dependency, minimal (1 - 5), moderate (6 - 10), dependent (>10)
Methods
We used a retrospective cohort design and an existing observational data set of patient records from 14 home care agencies to address the two aims of Phase II. We defined inclusion criteria as patients aged 65 and older, admitted to a home health care agency between January 1, 2004 and December 31, 2004. The final sample included 1,750 home care patients (386 frail and 1,364 non-frail) with 165,700 intervention records. Of 11,088 possible unique Omaha System interventions terms, 1,131 were represented in the data. A single intervention as described using the Omaha System consists of linked defined terms describing the problem addressed by the intervention, the action addressing the problem, and one additional term that further specifies the nature of the intervention. An average of seven interventions (range = 1-128) occurred per visit.
We obtained approval for this study from the University of Minnesota Institutional Review Board. After signing an agreement with two proprietary software programs (CareFacts™ [St. Paul, MN] and CHAMP [Mankato, MN]), the vendors contacted their home care customers and obtained a signed agreement to share de-identifed data. The investigators were blinded to the identity of the agencies. The software vendors obtained descriptive data about the agencies for this study, which represented a convenience sample of 14 Medicare-certified home health care agencies located in the Midwest and one on the East Coast. Agencies offered a variety of services including: skilled nursing; home health aides; and physical, occupational, and speech therapy. They represented various types of ownership: government/ county (n = 10), hospital (n = 2), free-standing for profit (n = 1) and not for profit (n = 2). Eight of the 14 agencies reported the number of annual visits, ranging from 3,165 to 24,000 visits per year. Both software programs include the Omaha System the standardized interface terminology.
Variables in the final data set were Client ID, Agency ID, admission date, visit date (date on which the intervention occurred), problem-category-target intervention, number of visits, frequency of visits, frail/non-frail elders, and variables for each intervention data management approach: an action category variable (four groups), a theoretical variable (five groups), a clinical expert consensus variable (23 groups), 24 data-driven variables (each yes/no), and hospitalization during episode of care (yes/no).
For Aim 1 (compare the ability of four intervention data management approaches to explain hospitalization outcomes for frail and non-frail elders separately), we determined the receiver operating characteristic (ROC) curve for each of the models and computed the area under each ROC curve (AUC) for model comparison. AUC is a ranking-based measure of classification performance. Its value can be interpreted as the probability that a classifier is able to distinguish a randomly chosen positive example from a randomly chosen negative example. In contrast to many alternative performance measures, AUC is invariant to relative class distributions and class-specific error costs (Thompson & Zucchini, 1989). For Aim 2 (identify specific intervention groups associated with hospitalization for frail elders and non-frail elders), modeling intervention group associations with hospitalization outcomes using logistic regression, we created dummy variables for all intervention groups. Each intervention group had three levels (low, medium, and high based on frequency of interventions) for comparison with a reference value of no interventions in a group. We deemed that each intervention was a representative of its group and that all interventions in a group added together represented the frequency of interventions for that group. We used logistic regression (Proc GENMOD in SAS v9.1) and retained variables in the final model if they were significant at p < .05 (McCullagh & Nelder, 1989).
Table 2 provides a summary of all intervention groups and levels that were significantly associated with hospitalization. Results are reported for frail and non-frail elderly patients by intervention management approach.
Table 2.
Interventions Associated with Hospitalization for Frail and Non-frail Elderly Patients
| OR | Lower 95% CI | Upper 95% CI | p value | n | AUC value | |
|---|---|---|---|---|---|---|
| Frail elderly patients | ||||||
| Action category | 0.593 | |||||
| Treatments and procedures - Low | 3.67 | 1.57 | 8.57 | 0.003 | 97 | |
| Surveillance - Low | 2.68 | 1.06 | 6.74 | 0.036 | 115 | |
| Theoretical | 0.553 | |||||
| Monitoring - Low | 3.12 | 1.33 | 7.34 | 0.009 | 115 | |
| Clinical expert consensus | 0.544 | |||||
| Monitoring Injury Prevention - Low | 1.99 | 1.15 | 3.44 | 0.014 | 95 | |
| Data-driven | 0.627 | |||||
| Assist Meds & Homemaking - High | 11.92 | 2.64 | 53.85 | 0.001 | 29 | |
| Medication management - High | 0.16 | 0.04 | 0.62 | 0.008 | 79 | |
| Providing Injury Prevention Treatment - Low | 2.96 | 1.39 | 6.33 | 0.005 | 104 | |
| Non-frail elderly patients | ||||||
| Action category | 0.584 | |||||
| Teaching, guidance, and counseling - High | 0.36 | 0.14 | 0.91 | 0.031 | 359 | |
| Case management - Low | 2.76 | 1.49 | 5.13 | 0.001 | 191 | |
| Theoretical | 0.526 | |||||
| Informing - High | 0.36 | 0.14 | 0.92 | 0.032 | 365 | |
| Clinical expert consensus | 0.603 | |||||
| Coordinating other - Medium | 2.17 | 1.01 | 4.66 | 0.048 | 141 | |
| Providing medication treatment - Medium | 3.72 | 1.47 | 9.38 | 0.005 | 49 | |
| Data-driven | 0.545 | |||||
| none |
OR = Odds Ratio, CI = Confidence Interval, AUC = Area Under Curve
Results
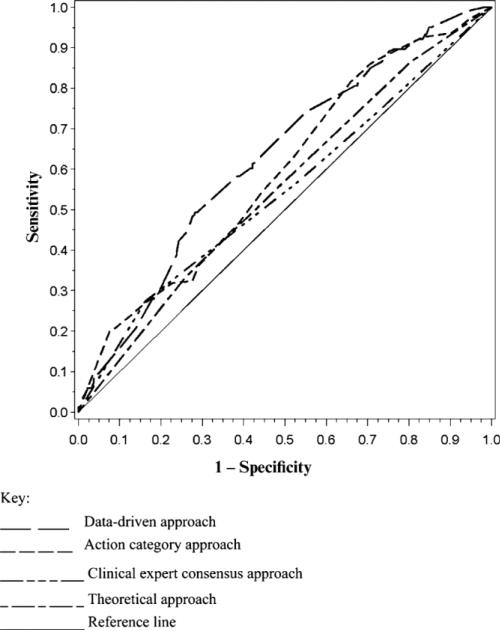
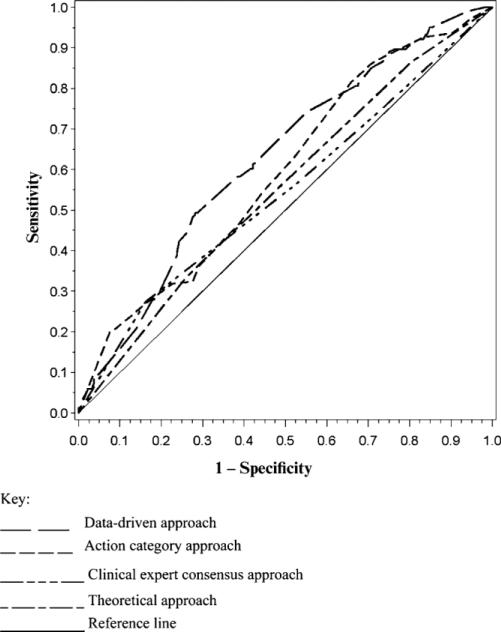
Aim 1 compared the abilities of intervention data management approaches for predicting the outcome of hospitalization during an episode of home care services. In the case of frail elders, AUC values ranged from .544 to .627, with the highest AUC value corresponding to the data-driven model (Figure 1). In the case of non-frail elders AUC values ranged from .526 to .603, with the highest AUC corresponding to the clinical expert consensus model (Figure 2).
FIGURE 1.
Receiver operating characteristic curves for frail elderly home care patients.
FIGURE 2.
Receiver operating characteristic curves for non-frail elderly home care patients.
Aim 2 of the study was to identify intervention groups associated with hospitalization for frail elders and non-frail elders. Intervention groups that were significantly associated with hospitalization for each of the four intervention data management approaches were different for frail and non-frail elderly patients. For frail elders, six intervention groups were associated with an increased likelihood of hospitalization, and one intervention group was associated with a decreased likelihood of hospitalization. For non-frail elders, four intervention groups were associated with an increased likelihood of hospitalization, and one intervention group was associated with a decreased likelihood of hospitalization (see Table 2).
Discussion
When we compared the ability of four intervention data management approaches to explain hospitalization outcomes for frail and non-frail elders, our findings showed that the data-driven approach was the best fit of the four intervention data management approaches for predicting hospitalization of frail elders. The multidimensional nature of the data-driven intervention groups may better reflect the complex needs of frail elders. For non-frail elders, none of the data-driven groups were significantly associated with hospitalization. The deductively derived clinical expert consensus model was the best fit of the four intervention data management approaches for non-frail elders. It is possible that the care of non-frail elders may be more straight-forward, dealing with particular health problems in less complex situations.
The theoretical models were the poorest overall fit of the four intervention data management approaches for predicting hospitalization for both groups. This may be due to the algorithm that sorted interventions based on the maternal-child health focus of the Clinical Nursing Models theory (Barnard et al., 1988). For example, problem, category, and target terms in supporting or providing therapy interventions may differ substantively in the care of elderly patients vs. maternal-child health clients simply due to differences in the problems experienced by the two client populations (Monsen, 2006). This finding supports the notion that the conceptual framework underlying the study matters. For further study, algorithms used in home care studies should be developed based on home care effectiveness theories.
Finally, the action category models were the second best fit of the four intervention data management approaches for both frail and non-frail elderly patients. This finding supports the use of Omaha System categories as an effective intervention data management approach.
Our study further showed that overall, 10 low and medium frequency intervention groups were associated with increased risk of hospitalization. A possible explanation for this finding is that there may be a mismatch between the level of care that is needed and the level of care that is provided. That is, too little care may result in hospitalization when patients have more intensive needs (Landi et al., 2004). Frail elders are more likely to be hospitalized if they have low frequencies of ‘treatments and procedures, surveillance, neuro-musculo-skeletal care, and monitoring injury prevention. Consistent with the literature, frail elders have poorer physical, psychological, and social functioning (Fortinsky et al., 2008; Gobbens et al., 2010; Landi et al., 2004). With increased need for assistance and inability to perform daily personal and household management, frail elders may need medium to high frequencies of these intervention groups to avoid hospitalization. Frail elders are also more likely to be hospitalized if they have a high frequency of assistance with medications and homemaking. This may be a spurious finding due to a few individuals (n = 29) who are dependent on medications and homemaking and are too frail to stay at home. Non-frail elders are more likely to be hospitalized if they have low frequencies of case management, and medium frequencies of case management-other (excluding supplies or typical community resources), suggesting that medium frequency of case management may either be insufficient, or that non-frail elders who need case management services may have more acute conditions. Previous researchers have focused on case management as critical for preventing poor outcomes for frail elders (Bauer et al., 2009). However, there is limited evidence that case management interventions in community settings are effective in reducing re-hospitalization (Peikes et al., 2009). Our findings suggest a need for further investigation of optimal case management dose for non-frail elders, as well as for frail elders. Non-frail elders who receive a medium frequency of providing medication treatment are more likely to be hospitalized suggesting that medium frequency of medication treatment may be insufficient, especially if medication treatment is being provided for more serious conditions that could require hospitalization. This finding is consistent with a previous study in which the majority of home care patients had an average of nine unique medications (range = 1-41) (Westra et al., in review).
In contrast, high intervention frequencies were associated with decreased risk of hospitalization for two intervention groups. Frail elders are less likely to be hospitalized if they have high frequency of medication management, suggesting that intensive medication management can help frail elders stay out of the hospital. Non-frail elders are less likely to be hospitalized if they have a high frequency of teaching, guidance, and counseling. Consistent with the literature, non-frail elders would be expected to have higher cognitive functioning, and thus be more likely to benefit from educational interventions (Landi et al., 2004). These findings suggest a possible match between patient needs and the care they receive. This interpretation demands examination of possible underlying health care quality issues that may be driven by insufficient resources or policies that limit care.
Medication focused interventions were both negatively and positively associated with hospitalization. This finding is consistent with the evidence that medication regimen adherence, drug-drug interactions, and poly-pharmacy issues are issues influencing hospitalization (Golden, Tewary, Dang, & Roos, 2010). The significance of medication focused interventions across multiple models emphasizes the importance of the home care nurse's role in assisting with medication management to ensure optimal patient outcomes. Therefore, medication focused interventions should be incorporated into standards of care for all types of home care patients.
When interpreting findings from observational data sets, it is necessary to consider confounding between practice description and client needs. Given that practitioners are tailoring interventions to each patient, it is likely that interventions describe the acuity of the problems experienced by the patient. For example, a high frequency of surveillance for a respiratory problem may indicate that the patient has a serious respiratory condition that requires frequent monitoring. It is optimal to replicate such studies with similar datasets to better interpret results and understand implications. Promising intervention strategies derived from these results should be tested in prospective randomized trials to improve confidence in the interpretation of complex relationships between the interventions and outcomes.
We were unable to obtain some related health system data that would facilitate and extend the interpretation of our findings. For example, agency factors such as type (Medicare/Non-Medicare), case mix, number of patients, number of nurses, size of patient load per nurse, visit average per day or per week, and educational preparation and experience of nurses would facilitate controlling for variations between agencies in intervention patterns and outcomes. In addition, the hospitalization outcome was a binary (yes/no) indicator from patients’ OASIS assessments. Limitations associated with these data were the inability to determine the level of care referred to as “hospitalization” by the practitioner, and where and when the transfer to hospital occurred. Furthermore, hospitalization may or may not have been related to the home health care admitting diagnosis. More detailed hospitalization data would improve interpretation of hospitalization outcome results. In addition, findings from this study are limited because the intervention data are sparse, with each patient receiving only a small fraction of the 1,131 interventions represented within the data. More observations would increase confidence in the results.
The need for high quality documentation cannot be overestimated. Efforts to improve documentation quality are advancing rapidly among Omaha System users. For example, public health nursing leaders in Washington state have developed and disseminated standards of care for maternal-child health services in the state using the Omaha System. They have implemented a systematic, standardized assessment process and core care plans for typical family health patients, as well as procedures for implementing these standards (Martin, Monsen, & Bowles, 2011). Similar efforts are underway in home care agencies in the Netherlands and in New Zealand (Monsen, Honey, & Wilson, 2010).
Conclusions
Four intervention data management approaches differentially predicted hospitalization outcomes of frail and non-frail elderly home care patients. Results suggest a possible mismatch between the level of care needed and the level of care provided. Further research using dense, high quality intervention data should continue to explore the relationship between nursing intervention and patient outcomes. Such research should employ intervention data management approaches that are suitable for the population and care provided. Analyses employing Omaha System action category intervention groups yielded meaningful findings and required no additional mapping or transformation. Thus, the action category approach offers a reasonable starting point for intervention data management.
Acknowledgments
Fang Yu was supported by a NIH K12 Career Advancement Award (RR023247-04).
Footnotes
Table 1 for the ADL section, are those means and SD? Please indicate. In the note, please italicize the response categories (e.g., minimal)
References
- Agency for Healthcare Research and Quality Clinical classification software for services and procedures: Healthcare cost and utilization project (HCUP). Retrieved October. 2008;24:2010. from www.hcup-us.ahrq.gov/toolssoftware/ccs_svcsproc/ccssvcproc.jsp. [Google Scholar]
- Barnard KE, Magyary D, Sumner G, Booth CL, Mitchell SK, Spieker S. Prevention of parenting alterations for women with low social support. Psychiatry. 1988;51:248–253. doi: 10.1080/00332747.1988.11024399. [DOI] [PubMed] [Google Scholar]
- Bauer M, Fitzgerald L, Haesler E, Manfrin M. Hospital discharge planning for frail older people and their family. Are we delivering best practice? A review of the evidence. Journal of Clinical Nursing. 2009;18:2539–2546. doi: 10.1111/j.1365-2702.2008.02685.x. [DOI] [PubMed] [Google Scholar]
- Briggs . Briggs® national quality improvement/hospitalization reduction study. Briggs Corporation; West Des Moines, IA: 2006. [Google Scholar]
- Centers for Medicare & Medicaid Services [October 24, 2010];OASIS - based home health agency patient outcome and case mix reports. 2008 from http://www.cms.hhs.gov/OASIS/09a_hhareports.asp.
- Fortinsky RH, Baker D, Gottschalk M, King M, Trella P, Tinetti ME. Extent of implementation of evidence-based fall prevention practices for older patients in home health care. Journal of the American Geriatric Society. 2008;56:737–743. doi: 10.1111/j.1532-5415.2007.01630.x. [DOI] [PubMed] [Google Scholar]
- Gobbens RJ, Luijkx KG, Wijnen-Sponselee MT, Schols JM. Toward a conceptual definition of frail community dwelling older people. Nursing Outlook. 2010;58:76–86. doi: 10.1016/j.outlook.2009.09.005. [DOI] [PubMed] [Google Scholar]
- Golden AG, Tewary S, Dang S, Roos BA. Care management's challenges and opportunities to reduce the rapid rehospitalization of frail community-dwelling older adults. The Gerontologist. 2010;50:451–458. doi: 10.1093/geront/gnq015. [DOI] [PubMed] [Google Scholar]
- Landi F, Onder G, Cesari M, Barillaro C, Lattanzio F, Carbonin PU, Bernabei R. Comorbidity and social factors predicted hospitalization in frail elderly patients. Journal of Clinical Epidemiology. 2004;57:832–836. doi: 10.1016/j.jclinepi.2004.01.013. [DOI] [PubMed] [Google Scholar]
- Hey T, Tansley S, Tolle K. The fourth paradigm. Microsoft Research; Redmond, WA: 2009. [Google Scholar]
- Levinson DR. Effect of the home health prospective payment system on the quality of home health care. 2006 Retrieved from http://oig.hhs.gov/oei/reports/oei-01-04-00160.pdf.
- Martin KS. The Omaha System: A key to practice, documentation, and information management. reprinted 2nd ed. Health Connections Press; Omaha, NE: 2005. [Google Scholar]
- Martin KS, Monsen KA, Bowles KH. The Omaha System and meaningful use: Applications in practice, education, and research. CIN. 2011;29(1):52–28. doi: 10.1097/NCN.0b013e3181f9ddc6. [DOI] [PubMed] [Google Scholar]
- Martin KS, Scheet NJ. The Omaha System: Applications for community health nursing. Saunders; Philadelphia, PA: 1992. [Google Scholar]
- McCullagh P, Nelder JA. Generalized linear models. 2nd ed. Chapman & Hall/CRC Press; Boca Raton, FL: 1989. [Google Scholar]
- Miller EA, Weissert WG. Incidence of four adverse outcomes in the elderly population: Implications for home care policy and research. Home Health Care Services Quarterly. 2001;20(4):17–47. doi: 10.1300/J027v20n04_02. [DOI] [PubMed] [Google Scholar]
- Monsen KA. Linking public health nurse home visiting interventions to patient outcomes. University of Minnesota; Minneapolis: 2006. Unpublished doctoral dissertation. [Google Scholar]
- Monsen KA, Banerjee A, Das P. Discovering client and intervention patterns in home visiting data. Western Journal of Nursing Research. 2010;32:1031–1054. doi: 10.1177/0193945910370970. [DOI] [PubMed] [Google Scholar]
- Monsen KA, Honey M, Wilson S. Meaningful use of a standardized terminology to support the electronic health record in New Zealand. Applied Clinical Informatics. 2010;1:368–376. doi: 10.4338/ACI-2010-06-CR-0035. http://dx.doi.org/10.4338/ACI-2010-06-CR-0035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Monsen KA, Westra BL, Yu F, Ramadoss VK, Kerr MJ. Data management for intervention effectiveness research: Comparing deductive and inductive approaches. Research in Nursing & Health. 2009;32:647–656. doi: 10.1002/nur.20354. [DOI] [PubMed] [Google Scholar]
- Peikes D, Chen A, Schore J, Brown R. Effects of care coordination on hospitalization, quality of care, and health care expenditures among Medicare beneficiaries: 15 randomized trials. JAMA. 2009;301:603–618. doi: 10.1001/jama.2009.126. [DOI] [PubMed] [Google Scholar]
- Shaughnessy PW, Hittle DF, Crisler KS, Powell MC, Richard AA, Kramer AM, Engle K. Improving patient outcomes of home health care: Findings from two demonstration trials of outcome-based quality improvement. Journal of the American Geriatrics Society. 2002;50:1354–1364. doi: 10.1046/j.1532-5415.2002.50356.x. [DOI] [PubMed] [Google Scholar]
- Thompson ML, Zucchini W. On the statistical analysis of ROC curves. Statistics in Medicine. 1989;8:1277–1290. doi: 10.1002/sim.4780081011. [DOI] [PubMed] [Google Scholar]
- Westra BL, Savik K, Holmes JH, Oancea C, Choromanski L. Acute care hospitalization for elderly home health care patients. in review. [Google Scholar]