Abstract
Background
Delays in tuberculosis (TB) diagnosis and treatment is a major barrier to effective management of the disease. Determining the factors associated with patient and provider delay of TB diagnosis and treatment in Asia may contribute to TB prevention and control.
Methods
We searched the PubMed, EMBASE and Web of Science for studies that assessed factors associated with delays in care-seeking, diagnosis, or at the beginning of treatment, which were published from January 1992 to September 2014. Two reviewers independently identified studies that were related to our meta-analysis and extracted data from each study. Independent variables were categorized in separate tables for patient and provider delays.
Results
Among 45 eligible studies, 40 studies assessed patient delay whereas 30 assessed provider delay. Cross-sectional surveys were used in all but two articles, which included 17 countries and regions. Socio-demographic characteristics, TB-related symptoms and medical examination, and conditions of seeking medical care in TB patients were frequently reported. Male patients and long travel time/distance to the first healthcare provider led to both shorter patient delays [odds ratio (OR) (95% confidence intervals, CI) = 0.85 (0.78, 0.92); 1.39 (1.08, 1.78)] and shorter provider delays [OR (95%CI) = 0.96 (0.93, 1.00); 1.68 (1.12, 2.51)]. Unemployment, low income, hemoptysis, and positive sputum smears were consistently associated with patient delay [ORs (95%CI) = 1.18 (1.07, 1.30), 1.23 (1.02, 1.49), 0.64 (0.40, 1.00), 1.77 (1.07, 2.94), respectively]. Additionally, consultation at a public hospital was associated with provider delay [OR (95%CI) = 0.43 (0.20, 0.91)].
Conclusions
We propose that the major opportunities to reduce delays involve enabling socio-demographic factors and medical conditions. Male, unemployed, rural residence, low income, hemoptysis, positive sputum smear, and long travel time/distance significantly correlated with patient delay. Male, long travel time/distance and consultation at a public hospital were related to provider delay.
Introduction
The severe epidemic situation of tuberculosis (TB) in Asia is well documented, and TB prevention and control is a top priority for public health. TB can cause enormous social and economic disruption, cause a series of serious consequences [1], and hamper a nation’s development [2]. In 2012, there were an estimated 8.6 million new TB cases and 1.3 million TB deaths [3]. Of the 22 high-TB burden countries, which account for approximately 80% of the world’s TB cases [4], almost all are developing countries where one-quarter of the world’s poorest populations lives. Southeast Asia and the Western Pacific region collectively accounted for 58% of the world’s TB cases in 2012, and India and China had the largest number of cases (26% and 12% of the global total, respectively). Moreover, as reported by the World Health Organization (WHO) [3], approximately 75% of the estimated 2.9 million cases were either not diagnosed or diagnosed but not reported to national tuberculosis programs in 12 countries, including India (31% of the global total), South Africa, Bangladesh, Pakistan, Indonesia, China, Democratic Republic of the Congo, Mozambique, Nigeria, Ethiopia, the Philippines, and Myanmar.
TB is preventable if people can access health care for prompt diagnosis and treatment. However, diagnosis and treatment delays are inevitable, and can be categorized as patient delays, provider delays (including health system or doctor delays), diagnostic delays (sometimes the sum of patient and provider delays), and treatment delays. Delays are significant regarding disease prognosis and complications at the individual level, as well as for transmission within the community, the reproductive rate of the TB epidemic [5], and the possibility of higher mortality [6, 7]. Delays can affect the rate of infection among close contacts [8], and the emergence of multidrug-resistant TB [9]. Thus, identifying when delays occur and the factors that correlate with different types of delay can aid tuberculosis control programs and help medical providers improve diagnosis and treatment efforts [10]. TB control programs must identify the reasons for delays in order to improve the control strategies.
It has been reported that one-third of the world’s TB burden, or approximately 4.9 million prevalent cases, are found in Southeast Asia [11]. Although similar systematic reviews have addressed delays in diagnosis and treatment and have reported the average (median or mean) total diagnosis delay, patient delay, and health system delay as 25–185 days, 4.9–162 days, and 2–87 days, respectively, for both low and high income countries [12], as well as India [13], no study has focused solely on Asia. One meta-analysis [14] described factors associated with patient and diagnostic delays in Chinese TB patients, and another analyzed factors associated with patient and health care system delays for TB in sub-Saharan African countries [15]. Thus, a systematic analysis of factors associated with patient and provider delays for TB that focuses on Asian countries is necessary to help design interventional studies suited to the culture, economic, and co-morbid patterns of this region. We sought studies conducted in adults in Asian countries to identify factors correlated to patient and provider delays in TB diagnosis. Our results may contribute to the practical work of TB prevention and control.
Methods
Inclusion and exclusion criteria
We used the following inclusion criteria: (1) studies that included TB patients (or suspected TB patients) in Asia; (2) studies that investigated factors that correlated with patient or provider delays in TB diagnosis and treatment; (3) studies designed as observational studies (cross-sectional, case—control, or cohort studies); and (4) studies that provided enough information to calculate the odds ratio (OR) and 95% confidence intervals (CI). If there was more than one article with the same population or data, the study with the largest population and most complete data was selected.
Our exclusion criteria were: (1) studies that included other diseases; (2) studies that did not investigate the associated factors; (3) duplicate studies; and (4) review articles, case reports, or comments without original data.
Two authors (JC, XW) independently screened the titles and abstracts of the studies that were initially included to assess their eligibility based on the inclusion and exclusion criteria. When there was a disagreement regarding the qualifications of the studies, the reviewers discussed whether the studies should be included until a consensus was reached.
Search strategy
Studies published in English from January 1992 to September 2014 that described original research were searched worldwide [16]. Eligible studies involved at least one factor related to delays in care-seeking, diagnosis, or at the beginning of treatment. We searched the PubMed, EMBASE, and Web of Science databases from January 1992 to September 2014. The search was limited to studies in humans. Search terms, including ‘tuberculosis’, ‘patient delay’, ‘provider delay’, ‘diagnosis delay’, ‘treatment delay’, ‘health system delay’, ‘Asia’ and countries in Asia, were searched in the title and abstract. We reviewed the references of the included studies and reviews. If it was unclear whether studies were eligible, the full texts were reviewed. The PubMed search strategy is shown in Table 1.
Table 1. PubMed databases search terms and strategy.
| Search terms | |
|---|---|
| 1 | provider delay |
| 2 | diagnosis late |
| 3 | delay treatment |
| 4 | patient delay |
| 5 | health seeking OR care-seeking |
| 6 | treatment seek |
| 7 | case detection OR case finding OR case diagnosis |
| 8 | delay present OR delay diagnosis OR diagnostic errors OR early diagnosis OR undiagnosed |
| 9 | 1 OR 2 OR 3 OR 4 OR 5 OR 6 OR 7 OR 8 |
| 10 | Tuberculosis |
| 11 | Asia OR China OR Hong Kong OR Macao OR Taiwan OR Japan OR Korea OR Mongolia OR myanmar OR Cambodia OR Indonesia OR Malaysia OR the Philippines OR Singapore OR Thailand OR Vietnam OR Bangladesh OR India OR maldives OR Nepal OR Pakistan OR Afghanistan OR Iran OR Israel OR Saudi Arabia OR Turkey |
| 12 | 9 AND 10 AND 11 |
Quality assessment
We rated the quality of all included studies using the Newcastle Ottawa Quality Assessment Scale (NOS) for non-randomized studies in meta-analyses [17] (Table 2).
Table 2. Characteristics of the 45 included studies.
| Author, year | Location | Study design | Sample | NOS score |
|---|---|---|---|---|
| Wang W (2007)[18] | China | Cross sectional study | n = 222; newly PTB patients; 76% aged 20–40 years; sex not recorded | 4 |
| Leung EC (2007)[19] | Hongkong | Retrospective study | n = 1249; pulmonary TB; 68.4% male; 47.7% were aged ≥60 years | 4 |
| Huong NT (2007) [20] | Vietnam | Cross sectional study | n = 2093; Smear-positive PTB patients; 71% male; 22.6% were ≥65 years | 5 |
| Enkhbat S (1996)[21] | Mongolia | Cross sectional study | n = 107; ≥16 years TB patients; 54% male; Mean age = 33 years | 4 |
| Yamasaki-Nakagawa M (2001) [22] | Nepal | Cross sectional study | n = 390; new TB cases + began to receive Direct Observation Therapy, Short-course; 67.9% male; Median age in men = 37 years, in women = 30 years | 5 |
| Chiang CY (2005)[23] | Taiwan | Cross sectional study | n = 206; new sputum-positive PTB patients; 69.4% male, Mean(range) age = 59.2 (17–91) years | 5 |
| Rojpibulstit M (2006) [24] | Thailand | Cross sectional study | n = 192; newly diagnosed smear-positive and smear-negative PTB patients; 75% male; Mean (SD, range) = 43.3 (16.2, 15–83) years | 5 |
| Li X (2012)[25] | China | Cross sectional study | n = 323; >18 years + migrant + new PTB; 63.8% male; median (inter-quartile range) = 30 (24–38) years | 5 |
| Lock WA (2011)[26] | Indonesia | Cross sectional study | n = 194; TB suspects; 54% male; Mean (SD) = 39 (14.1) years | 5 |
| Zhou C (2012)[27] | China | Cross sectional study | n = 314; TB patients being treated or had finished standard treatment within 6 months; 63.4% male; age mean (range, median) = 31.8 years (15–70, 28) | 5 |
| Chang CT (2007)[28] | Malaysia | Cross sectional study | n = 316; new smear-positive PTB patients + adult; 61.1% male; age mean (range, median) = 44.2 (15–7, 45) years | 5 |
| Lin X (2008)[29] | China | Cross sectional study | n = 10356; smear-positive PTB cases; 65.5% male; Median (IQR) = 38 (27–54) years | 5 |
| Basnet R (2009) [30] | Nepal | Cross sectional study | n = 307; new TB patients; 59.0% male; 70.7% 15–54 years | 5 |
| Guneylioglu D (2004) [31] | Turkey | Cross sectional study | n = 204; smear-positive PTB + hospitalized patients; 59.8% male; Mean age = 33 years | 4 |
| Hoa NB (2011) [32] | Vietnam | Cross sectional study | n = 7040; TB suspects + >15 years; 62.9% male; Mean age (SD) = 48.9 (0.3) years | 5 |
| Xu B (2007) [33] | China | Cross sectional study | n = 1204; TB suspects; 61.6% male; 40–59 years 36.0% | 4 |
| Ahmad RA (2013) [34] | Indonesia | Cross sectional study | n = 746; TB suspects + ≥15 years; 38% male; ≥60 years 45.4% | 4 |
| Phoa LL (2005) [35] | Singapore | Cross sectional study | n = 375; adult PTB patients (sputum culture-positive and cough); M/F ratio 3:1, Median (range) = 49 years (15–90 years) | 6 |
| Xu X (2013) [36] | China | Cross sectional study | n = 4677; suspected TB cases; 64% male; 15–30 years 60.3% | 5 |
| Rundi C (2011) [37] | Malaysia | Cross sectional study | n = 296; smear-positive TB patients + ≥18 years; age and sex were not presented | 6 |
| Zhao X (2014) [38] | China | Cross sectional study | n = 819; TB patients + >15 years; 72.5% male; Median (range) = 53 (15–90) years | 5 |
| Cheng G (2005) [39] | China | Cross sectional study | n = 190; smear positive PTB patients; 65.3% male; Mean age (SD) = 48.1 (16.6) years | 5 |
| Tobe RG (2013) [40] | China | Cross sectional study | n = 314; smear positive PTB patients; 63.4% male; age was not presented | 6 |
| Choudhari M (2012) [41] | Nepal | Cross sectional study | n = 215; PTB patients; 65.6% male; Mean age = 39.6 years | 6 |
| Shu W (2014) [42] | China | Cohort study | n = 260; active TB patients; age and sex were not presented | 7 |
| Ngamvithayapong J (2001) [43] | Thailand | Cross sectional study | n = 557; smear positive PTB patients + >15 years; sex was not presented; Median (range) = 37 (29–52) years old | 5 |
| Selvam JM (2003) [44] | India | Cross sectional study | n = 667; new adult TB patients; 73% male; Mean age = 43 years | 5 |
| Chen HG (2014) [45] | China | Cross sectional study | n = 1126; PTB patients; age and sex were not presented | 6 |
| Kelkar-Khambete A (2008) [46] | India | Cross sectional study | n = 117; new sputum-positive TB patients; 60% male; 15–44 years 82% | 5 |
| Ayé R (2010) [47] | Tajikistan | Cross sectional study | n = 168; new PTB patients + ≥15 years; age and sex were not presented | 4 |
| Tobgay KJ (2006) [48] | India | Cross sectional study | n = 323; TB patients cough for ≥3 weeks; 58.8% male; Median = 30 years | 6 |
| Rumman KA (2008) [49] | Jordan | Cross sectional study | n = 1544; TB suspects + >15 years; 57.3% male; >35 years 62.6% | 6 |
| Wang Y (2008) [50] | China | Cross sectional study | n = 1005; adult suspected TB cases + >15 years; 54.1% male; ≥60 years 41.4% | 6 |
| Mor Z, (2013) [51] | Israel | Cross sectional study | n = 1005; adult suspected TB cases + >15 years; Citizen: 60.8% male; Mean age (SD) = 53.7 (19.7) years; Migrant: 45.5% male; Mean age (SD) = 35.0 (9.8) years | 5 |
| Rifat M (2011) [52] | Bangladesh | Cross sectional study | n = 7280; new smear-positive PTB patients; age and sex were not presented | 5 |
| Bai LQ (2004) [53] | China | Cross sectional study | n = 318; smear-positive PTB patients + ≥15 years; 72.0% male; Mean age (SD) = 38.2 (12.0) years | 6 |
| Tamhane A (2012) [54] | India | Cross sectional study | n = 150; newly smear-positive PTB patients + ≥18 years; 50% male; Median = 30 years | 5 |
| Sabawoon W (2012) [55] | Afghanistan | Cross sectional study | n = 122; smear-positive PTB patients + ≥15 years; 45.9% male; Mean age (SD) = 42.2 (17.7) years | 4 |
| Karim F (2007) [56] | Bangladesh | Cross sectional study | n = 1000; smear-positive PTB patients; 50% male; Mean age = 37.7 years | 5 |
| Thakur R (2010) [57] | India | Cross sectional study | n = 234; smear-positive PTB patients; 66.7% male; ≥35 years 50.9% | 5 |
| Lönnroth K (1999) [58] | Vietnam | Cross sectional study | n = 422; new TB patients + ≥15 years; 70.4% male; 51.1% were aged 15–34 | 4 |
| Rajeswari R (2002) [59] | India | Cross sectional study | n = 531; new smear- positive TB patients; 72% male; 62%<45 years | 5 |
| Lin HP (2009) [60] | Taiwan | Cross sectional study | n = 78118; new PTB patients; 69.4%were male; 42648 (54.6%) patients were aged over 65 years | 5 |
| Wang WB (2006) [61] | China | Cross sectional study | n = 493; newly TB patients; 72.4% male; 40–60 years 38.1% | 4 |
| Lin CY (2010) [62] | Taiwan | Cross sectional study | n = 193; culture-proven, new hospitalized PTB patients; 67.9% male; Mean age (SD) = 63.47 (18.04) years | 5 |
Data extraction
Two authors (JC, XW) independently extracted the data from the eligible studies. Differences were resolved by discussion between the reviewers to reach a consensus. Available information was extracted from each study including the authors, publication year, location, starting points and endpoints of delays, study design, method of data collection, characteristics of samples, measurements of the dependent variables, data source, and conclusions.
Statistical analyses
We summarized related characteristics and independent variables from the 18 selected studies using separate tables for patient and provider delays. The overall effect of factors related to delays was estimated in more than two studies by conducting a meta-analysis based on ORs and 95% CIs. If ORs and 95% CIs were not reported in the original article but sufficient data were provided, we used the calculator in Review Manager Software 5.2 (Cochrane Collaborative, Oxford, United Kingdom) to calculate ORs and 95% CIs. We used Q tests and the I-squared statistic [I2 = 100% × (Q-df)/Q] to quantify heterogeneity. Because of the small number of studies and the small sample size of some of the included studies, we used a P-value of 0.10 and an I2 of 50% to determine statistical significance. If the P-value of the Q statistic ≥0.10, or if P <0.10 but I2 ≤50%, we used fixed effect models; otherwise, random effect models were used.
Results
Identification of eligible studies
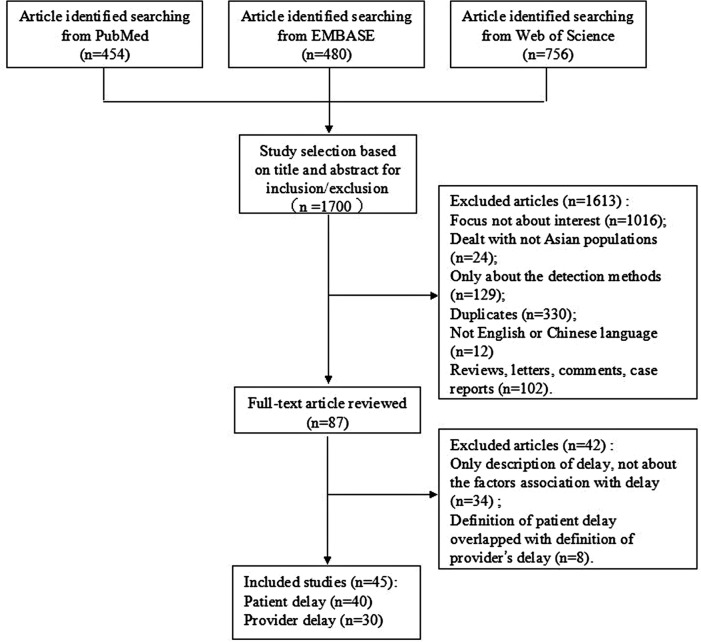
There were 1700 articles regarding factors associated with patient (care-seeking) delays or provider (health-system, doctor, or diagnostic) delays identified from the databases. We excluded 1613 articles after browsing the titles and abstracts, primarily because they did not have a dependent relationship with the topic. In addition, we also excluded reviews, letters, comments, or case reports. After searching 87 full texts, another 34 studies were excluded because although their initial aim focused on delays, correlated factors were not discussed. Eight articles were excluded because the endpoint of patient delay was the start of treatment, which overlaps with the definition of provider delay. Finally, 45 studies were included in this meta-analysis (Table 2). Fig. 1 shows a flow chart of the literature search for studies regarding patient and provider delays (Fig. 1).
Fig 1. Flow Chart of literature search for studies on the patient delay and provider delays.
This figure is a description of the full search process.
Study characteristics
The included articles were published between 1997 and 2014 (Table 3). The 45 articles covered 17 countries and regions, including mainland China (k = 14), India (k = 6), Vietnam (k = 3), Nepal (k = 3), Taiwan (k = 3), Indonesia (k = 2), Malaysia (k = 2), Thailand (k = 2), Bangladesh (k = 2), Turkey (k = 1), Mongolia (k = 1), Hong Kong (k = 1), Singapore (k = 1), Tajikistan (k = 1), Jordan (k = 1), Israel (k = 1), and Afghanistan (k = 1). Sample sizes in the studies ranged from 107 to 78,118. All studies except six conducted patient interview surveys (cross-sectional or cohort design), and used a consecutive method of patient sampling. In all the studied samples, the proportion of male patients was greater than 50%. Most studies were conducted in both rural and urban areas (k = 37). Finally, there were 41,185 TB cases on patient delay and 103,427 TB cases on provider delay.
Table 3. Factors assessed for association with patient delay (k = 40).
| Citation | Delay = 1st sx to (interval) | Male sex | Old age | Education | Unemployed | Rural residence | Income low level | Hemoptysis | Cough | Positive sputum smear | Chest radiographs | Consult with a public hospital | Long travel time/distance |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Wang W (2007)[18] | 1st consult (21 days) | x | x | x | x | — | ↑ | ↓ | — | — | x | — | — |
| Leung EC (2007)[19] | 1st consult (20days) | — | — | — | ↑ | — | — | ↓ | — | — | — | — | — |
| Huong NT (2007) [20] | 1st consult (6 weeks) | x | x | — | — | ↑ | — | — | — | — | — | x | — |
| Enkhbat S (1996)[21] | 1st consult (1 month) | x | x | — | — | x | x | — | — | — | — | x | — |
| Yamasaki-Nakagawa M (2001)[22] | 1st consult (1 months or 7 months) | — | — | — | — | — | — | — | — | — | — | — | — |
| Chiang CY (2005)[23] | 1st consult (7 days) | x | ↑ | — | — | — | — | x | x | x | x | x | — |
| Rojpibulstit M (2006)[24] | 1st consult (interval not recorded) | x | x | — | — | — | — | — | — | x | — | — | — |
| Li X (2012)[25] | 1st consult (10 days) | x | x | — | x | — | — | ↓ | — | — | — | — | — |
| Lock WA (2011) [26] | 1st consult (2weeks) | x | x | x | — | x | x | — | — | — | — | ↑ | ↑ |
| Zhou C (2012)[27] | 1st consult (14 days) | x | x | x | — | x | ↑ | — | — | — | — | — | ↑ |
| Chang CT (2007)[28] | 1st consult (30days) | ↓ | — | — | — | — | x | — | — | — | — | — | — |
| Lin X (2008)[29] | 1st consult (60 days) | — | ↓ | — | x | — | ↓ | — | — | — | — | — | — |
| Basnet R (2009) [30] | 1st consult (30 days) | x | x | x | — | — | x | — | — | ↑ | — | — | x |
| Guneylioglu D (2004) [31] | 1st consult (30 days) | x | x | x | — | x | ↑ | ↓ | ↓ | — | — | — | — |
| Hoa NB (2011) [32] | 1st consult (interval not recorded) | ↓ | — | — | — | ↓ | x | — | — | — | — | — | — |
| Xu B (2007) [33] | 1st consult (interval not recorded) | x | x | x | — | — | x | — | — | — | — | — | — |
| Ahmad RA (2013) [34] | 1st consult (interval not recorded) | ↓ | — | — | x | — | — | — | — | — | — | — | — |
| Phoa LL (2005) [35] | 1st consult (4 weeks) | x | ↓ | — | x | — | — | — | — | ↑ | — | — | — |
| Xu X (2013) [36] | 1st consult (3 weeks) | ↓ | x | — | — | — | — | — | — | ↑ | — | — | — |
| Rundi C (2011) [37] | 1st consult (30 days) | x | x | — | — | x | x | — | — | — | — | x | x |
| Zhao X (2014) [38] | 1st consult (30 days) | ↓ | x | x | x | — | x | — | — | — | — | — | x |
| Cheng G (2005) [39] | 1st consult (interval not recorded) | x | x | ↓ | — | — | x | — | — | — | — | x | x |
| Tobe RG (2013) [40] | 1st consult (2 weeks) | x | — | x | — | x | ↑ | — | — | — | — | — | ↑ |
| Choudhari M (2012) [41] | 1st consult (30 days) | x | ↑ | — | x | x | x | — | — | — | — | — | ↑ |
| Shu W (2014) [42] | 1st consult (interval not recorded) | — | x | — | — | — | — | — | — | — | — | — | — |
| Ngamvithayapong J (2001) [43] | 1st consult (21 days) | x | x | x | — | — | — | — | — | — | — | — | — |
| Selvam JM (2003) [44] | 1st consult (28 days) | x | x | x | x | — | — | — | — | — | — | x | x |
| Chen HG (2014) [45] | 1st consult (30 days) | x | ↑ | — | — | — | — | — | — | ↑ | Cavity:↑ | — | — |
| Kelkar-Khambete A (2008) [46] | 1st consult (21 days) | x | x | x | — | x | x | — | — | — | — | — | — |
| Ayé R (2010) [47] | 1st consult (interval not recorded) | x | x | — | — | x | — | — | — | — | — | — | — |
| Tobgay KJ (2006) [48] | 1st consult (30 days) | x | x | — | — | — | — | — | — | — | — | ↑ | — |
| Rumman KA (2008) [49] | 1st consult (3 weeks) | ↓ | ↑ | ↑ | x | ↑ | ↑ | ↑ | — | — | — | — | x |
| Wang Y (2008) [50] | 1st consult (2 weeks) | ↓ | ↓ | ↓ | x | — | ↓ | — | — | — | — | — | — |
| Mor Z (2013) [51] | 1st consult (25 days) | x | x | — | x | — | — | — | — | ↑ | — | — | — |
| Rifat M (2011) [52] | 1st consult (4 weeks) | x | x | — | — | ↑ | — | — | — | — | — | — | — |
| Bai LQ (2004) [53] | 1st consult (14 days) | — | — | — | — | — | — | ↓ | — | — | — | — | — |
| Tamhane A (2012) [54] | 1st consult (20 days) | — | — | — | x | — | — | x | — | — | — | — | — |
| Sabawoon W (2012) [55] | 1st consult (interval not recorded) | — | — | — | — | — | — | — | — | — | — | ↓ | ↑ |
| Karim F (2007) [56] | 1st consult (interval not recorded) | x | x | — | — | — | — | — | — | — | — | — | — |
| Thakur R (2010) [57] | 1st consult (33.5 days) | x | x | x | — | x | ↑ | — | — | — | — | ↑ | — |
x. Assessed but P ≥ 0.05
↓. Negatively correlated with delay, P < 0.05
↑. Positively correlated with delay, P < 0.05
—. Not assessed.
Patient delay studies
Patient delay was measured using patients’ recall of first TB symptoms as the starting point, (usually described as the onset of a persistent cough) and the date of the first health facility consultation as the endpoint. All studies measured delay as a dichotomous variable, typically based on a median split from 7 to 60 days. Nearly all studies reported their definition of delay; however, some (k = 9) did not mention the specific interval of delay.
Factors assessed
Forty studies assessed associated factors, including patient socio-demographic characteristics, TB-related symptoms, medical examinations, and conditions of seeking medical care (Table 3). Socio-demographic characteristics included gender, age, education, occupation, rural residence, and income level. Thirty-three studies analyzed the relationship between male sex and delay, and seven showed male sex negatively correlated with delay. Thirty-one studies evaluated the role of age in delay, and 13 studies addressed unemployment and patient delay. Education level was discussed in 14 studies. Fourteen studies reported correlations between rural residence and patient delay. Nineteen studies paid attention to income level. TB symptoms were associated with patient delay in eight studies, in which cough was analyzed as the first symptom (k = 2) and hemoptysis (k = 8) was associated with patient severity. Positive sputum smears and chest radiographs were taken at the first consultation in seven and three studies, respectively. Consulting a public hospital was associated with delay in ten studies. Long travel time or distance to the first healthcare provider was investigated in 11 studies.
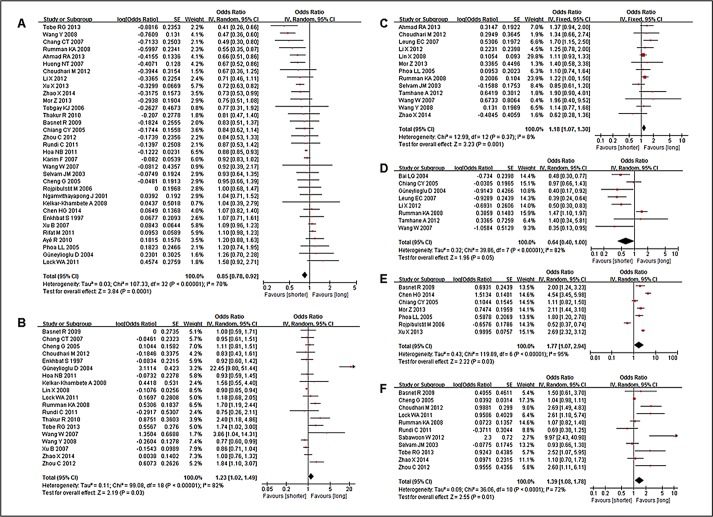
Meta-analysis
Male, unemployed, low income level, hemoptysis, positive sputum smears, chest radiographs, and long travel time or distance to the first healthcare provider all significantly correlated with patient delay (Table 4). Male and hemoptysis were negatively associated with patient delay, whereas the other three factors were positively associated (P<0.05). There were no significant relationships between delay and older age, education level, rural residence, chest radiographs, or consultation with a public hospital (Fig. 2). Cough and other factors could not be evaluated due to a lack of data in the studies.
Table 4. Results of meta-analyses and test for heterogeneity of patient delay.
| Variable | k | OR (95% CI) a | Heterogeneity between studies | Test for overall effect (P) | ||
|---|---|---|---|---|---|---|
| Q statistic | P-value | I2 | ||||
| Male sex | 33 | 0.85 (0.78, 0.92) | 107.33 | <0.00001 | 70% | 0.0001 |
| Unemployed | 13 | 1.18 (1.07, 1.30) | 12.99 | 0.37 | 8% | 0.001 |
| Income (Low) | 19 | 1.23 (1.02, 1.49) | 99.08 | <0.00001 | 82% | 0.03 |
| Haemoptysis | 8 | 0.64 (0.40, 1.00) | 39.86 | <0.00001 | 82% | 0.05 |
| Positive smear | 7 | 1.77 (1.07, 2.94) | 119.89 | <0.00001 | 95% | 0.03 |
| Long travel time/distance to the first healthcare provider | 11 | 1.39 (1.08, 1.78) | 36.06 | <0.0001 | 72% | 0.01 |
| Age (older) | 31 | 1.01 (0.91, 1.11) | 144.10 | <0.00001 | 79% | 0.87 |
| Education(illiterate) | 14 | 0.99 (0.78, 1.24) | 45.23 | <0.0001 | 71% | 0.90 |
| Rural residence | 14 | 1.15 (0.99, 1.34) | 42.25 | <0.0001 | 69% | 0.06 |
| Chest radiographs | 3 | 1.42 (0.78, 2.58) | 27.72 | <0.0001 | 93% | 0.25 |
| Consult with a public hospital | 10 | 0.99 (0.65, 1.50) | 66.39 | <0.00001 | 86% | 0.96 |
a. P-value for homogeneous studies (Q statistic, P≥0.10, or P<0.10, but I2≤50%)—fixed-effect model; otherwise, P-value for significantly heterogeneous studies (Q statistic, P<0.10, but I2>50%)—random effects model.
Fig 2. Forest plots of meta-analysis of factors associated with patient delay.
This figure shows forest plots for the meta-analysis of five factors associated with patient delay. OR and 95% CI for each factor are given. Notes: A- Male sex; B- Low income; C- Unemployed occupation; D- Haemoptysis; E- Smear positive; F- Long travel time/distance to the first healthcare provider.
Provider delay studies
The provider (usually described as the health care system, doctor, or diagnostician) delay studies all used the first consultation at a health facility as the starting point. However, 18 studies used diagnosis as the endpoint, whereas 12 others used the start of anti-TB treatment. Moreover, different endpoint definitions may not necessarily be different points in time. The duration was ranged from 7 to 79 days.
Factors assessed
There were 30 studies associated with provider delay. The associated factors may be related to the aspect of provider delay for diagnosis and treatment. Among socio-demographic factors, 24 studies mentioned a connection between male sex and provider delay: two studies showed a positive relationship, two showed a negative relationship, and 20 showed no relationship. Other factors included older age (k = 24), illiterate or lack of education (k = 10), rural residence (k = 8), low income (k = 10), and unemployed (k = 4). Other factors, such as symptoms (cough, k = 2; hemoptysis, k = 8), examination (positive sputum smears: k = 8; chest radiographs: k = 5), and consulting with a public hospital (k = 12), were found to be correlated with provider delay in at least one study. Finally long travel time or distance from the patient’s home to the health facility was reported to be correlated with provider delay in seven studies. (Table 5)
Table 5. Factors assessed for association with provider delay (k = 30).
| Citation | Delay = 1st sx to (interval) | Male sex | Old age | Education | Unemployed | Rural residence | Income low level | Haemoptysis | Cough | Smear positive | Chest radiographs | Consult with a public hospital | Long travel time/distance |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Wang W (2007) [18] | Diagnosis (8 days) | x | x | x | x | — | x | x | — | — | x | — | — |
| Yamasaki-Nakagawa M (2001) [22] | Diagnosis (1 month) | — | — | — | — | — | — | — | — | — | — | — | — |
| Rojpibulstit M (2006) [24] | Diagnosis (interval ot recorded) | x | ↑ | — | — | — | — | — | — | x | — | ↑ | — |
| Zhou C (2012) [27] | Diagnosis (14 days) | x | ↓ | x | — | x | x | — | — | — | — | ↓ | ↑ |
| Chang CT (2007) [28] | Diagnosis (22 days) | x | — | — | — | — | x | x | — | — | — | — | — |
| Basnet R (2009) [30] | Diagnosis (30 days) | x | x | x | — | — | x | — | — | x | — | — | x |
| Xu X (2013) [36] | Diagnosis (2 weeks) | x | x | — | — | — | — | — | — | ↓ | — | — | — |
| Cheng G (2005) [39] | Diagnosis (interval not recorded) | ↑ | x | x | — | — | x | — | — | — | — | x | x |
| Shu W (2014) [42] | Diagnosis (interval not recorded) | — | — | — | — | — | — | — | — | ↓ | — | — | — |
| Ngamvithayapong J (2001) [43] | Diagnosis (7 days) | ↓ | x | x | — | — | — | — | — | — | — | — | — |
| Kelkar-Khambete A (2008) [46] | Diagnosis (7 days) | x | x | x | — | x | ↑ | — | — | — | — | — | — |
| Bai LQ (2004) [53] | Diagnosis (14 days) | — | — | — | — | — | — | x | — | — | — | — | — |
| Sabawoon W (2012) [55] | Diagnosis (interval not recorded) | — | — | — | — | — | — | — | — | — | — | — | ↑ |
| Karim F (2007) [56] | Diagnosis (interval not recorded) | x | x | — | — | — | — | — | — | — | — | — | — |
| Lönnroth K (1999) [58] | Diagnosis (4 weeks) | ↓ | — | — | — | ↓ | — | ↓ | — | — | — | ↑ | — |
| Rajeswari R (2002) [59] | Diagnosis (7days) | x | ↑ | x | ↑ | x | x | — | — | — | — | x | ↑ |
| Lin HP (2009) [60] | Diagnosis (9 days) | x | ↑ | — | — | — | — | — | — | ↓ | Aberrant: ↓ | — | — |
| Wang WB (2006) [61] | Diagnosis (interval not recorded) | x | x | x | — | — | x | ↑ | — | — | x | — | — |
| Leung EC (2007) [19] | Anti-TB treatment (20 days) | — | ↑ | — | — | — | — | — | — | — | ↓ | — | — |
| Huong NT (2007) [20] | Anti-TB treatment (6 weeks) | x | x | — | — | ↓ | — | — | — | — | — | ↑ | — |
| Enkhbat S (1996) [21] | Anti-TB treatment (1 month) | x | x | — | — | x | x | — | — | — | — | x | — |
| Chiang CY (2005) [23] | Anti-TB treatment (23 days) | ↑ | x | — | — | — | — | ↑ | ↓ | ↑ | ↑ | ↑ | — |
| Selvam JM (2003) [44] | Anti-TB treatment (14 days) | x | x | ↑ | x | — | — | — | — | — | — | ↓ | ↑ |
| Ayé R (2010) [47] | Anti-TB treatment (interval not recorded) | x | x | — | — | x | — | — | — | — | — | x | — |
| Tobgay KJ (2006) [48] | Anti-TB treatment (7 days) | x | x | — | — | — | — | — | — | — | — | ↓ | — |
| Mor Z (2013) [51] | Anti-TB treatment (79 days) | x | x | — | x | — | — | — | — | x | — | — | — |
| Rifat M (2011) [52] | Anti-TB treatment (9 weeks) | x | ↑ | — | — | ↑ | — | — | — | — | — | — | — |
| Tamhane A (2012) [54] | Anti-TB treatment (14 days) | — | x | x | — | — | x | x | — | — | — | — | x |
| Thakur R (2010) [57] | Anti-TB treatment (1 day) | x | x | x | — | x | x | — | — | — | — | ↓ | — |
| Lin CY (2010) [62] | Anti-TB treatment (7 days) | x | ↑ | — | — | — | — | x | x | ↓ | — | — | — |
x. Assessed but P ≥ 0.05
↓. Negatively correlated with delay, P < 0.05
↑. Positively correlated with delay, P < 0.05
—. Not assessed.
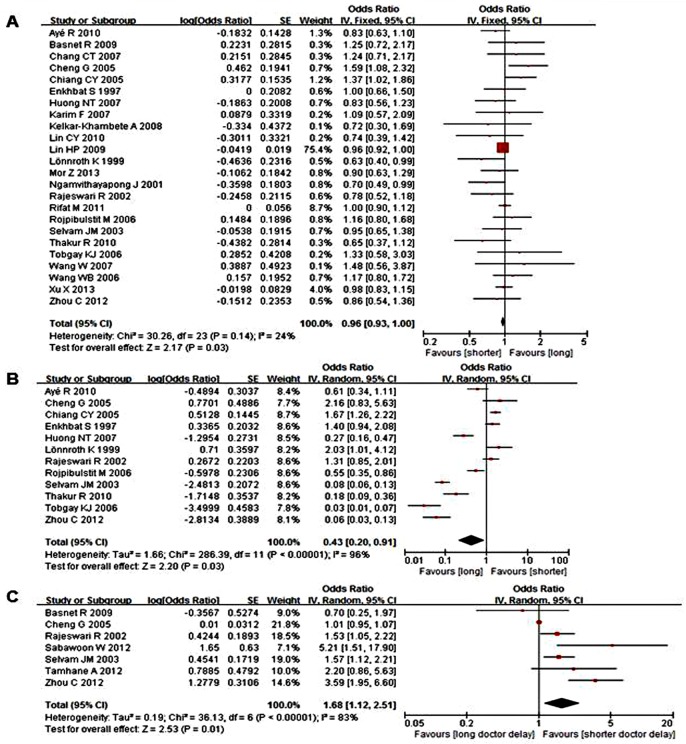
Meta-analysis
Male sex, older age, illiterate or lack of education, unemployment, rural residence, low income, hemoptysis, positive sputum smears, consulting with a public hospital, and long travel time or distance had sufficient information to calculate ORs and 95% CIs. Only male sex and consultation with a public hospital negatively correlated with provider delays, whereas long travel time or distance to the first healthcare provider positively associated with provider delay (P<0.05). The pooled effect size for the factors in these studies are shown in Table 6, indicating that male patients and the first consultation with a public hospital had shorter provider delays, whereas long travel time or distance to the first healthcare provider may have longer delays (Fig. 3).
Table 6. Results of meta-analyses and test for heterogeneity of provider delay.
| Variable | k | OR (95% CI) a | Heterogeneity between studies | Test for overall effect (P) | ||
|---|---|---|---|---|---|---|
| Q statistic | P-value | I2 | ||||
| Male sex | 24 | 0.96 (0.93, 1.00) | 30.26 | 0.14 | 24% | 0.03 |
| Consult with a public hospital | 12 | 0.43 (0.20, 0.91) | 286.39 | <0.00001 | 96% | 0.03 |
| Long travel time/distance to the first healthcare provider | 7 | 1.68 (1.12, 2.51) | 36.13 | <0.00001 | 83% | 0.01 |
| Age (older) | 24 | 1.17 (0.91, 1.51) | 962.61 | <0.00001 | 98% | 0.21 |
| Education (illiterate) | 10 | 0.88 (0.74, 1.05) | 7.32 | 0.60 | 0% | 0.15 |
| Rural residence | 8 | 1.20 (0.76, 1.88) | 62.37 | <0.00001 | 89% | 0.44 |
| Income (low) | 10 | 1.13 (0.80, 1.58) | 27.44 | 0.0010 | 67% | 0.50 |
| Unemployed | 4 | 1.68 (0.72, 3.94) | 38.51 | <0.00001 | 92% | 0.23 |
| Haemoptysis | 8 | 0.78 (0.42, 1.44) | 53.68 | <0.00001 | 87% | 0.42 |
| Positive smear | 8 | 0.61 (0.13, 2.96) | 2313.32 | <0.00001 | 100% | 0.54 |
| Chest radiographs | 5 | 0.72 (0.31, 1.70) | 182.38 | <0.00001 | 98% | 0.46 |
a. P-value for homogeneous studies (Q statistic, P≥0.10, or P<0.10, but I2≤50%)—fixed-effect model; otherwise, P-value for significantly heterogeneous studies (Q statistic, P<0.10, but I2>50%)—random effects model.
Fig 3. Forest plots of meta-analysis of factors associated with provider delay.
This figure shows forest plots for the meta-analysis of male sex factor associated with provider delay. OR and 95% CI for the factor are given. Notes: A- Male sex; B- Consult with a public hospital; C- Long travel time/distance to the first healthcare provider.
Discussion
Although the prevalence of TB in most Asian countries has been decreasing annually in recent years [63], there is still an epidemiological challenge for TB control. Moreover, case detection is often late. This meta-analysis reviewed the factors correlated to delays in TB diagnosis and treatment, which could provide valuable data for TB programs. A meta-analysis regarding TB treatment delays in Asia was not previously conducted. Understanding the factors that are closely associated with delays is essential to effectively controlling TB, accessing TB services, as well as reducing delays for seeking prompt diagnosis and treatment [64]. As reported by Glanz et al. [65], individual-level factors include socio-demographics, TB symptoms, knowledge, attitudes, and behaviors. Furthermore, due to the ease of data collection, socio-demographic characteristics were the majority of independent variables that were assessed for correlation with patient or provider delays.
Our data showed that male sex served as an important determinant of both patient and provider delays. Despite the cross-sectional nature and sufficient sample size to detect correlations with delay, male sex negatively correlated with delays in seeking diagnosis and treatment for TB. Similar findings were reported in studies from other countries [66, 67]. In addition, cultural factors are likely to be involved in gender differences. Because of the higher TB prevalence in males, TB is likely suspected and investigated more readily in men [68]. Therefore, men are likely to seek health care earlier when symptoms appeared; thus, TB propaganda regarding disease control and diagnosis is more necessary for men. Moreover, biological differences between males and females with respect to TB incidence and the sensitivity of smear examinations may play an essential role [69]. In addition, gender-specific themes were particularly pervasive within financial, stigma, and health literacy barriers. Studies [70, 71] for gender-related differences in barriers and delays in TB diagnosis and treatment services found that women experienced greater financial barriers and greater stigma than men; the identified barriers were gender-specific in the majority of studies. It is therefore challenging to overcome gender-specific barriers that require intervention. We propose that female patients with symptoms suggestive of TB should receive more attention before and after seeking care.
Regarding the behavior of patients, long travel time or distance to the first healthcare provider was found to be a significant determinant that correlated with both patient and provider delays. Previous reviews of the factors associated with patient and diagnostic delays in China and sub-Saharan African countries [14, 15] reported that the majority of factors associated with delays in TB diagnosis and treatment were related to the place of first consultation, travel time, or distance from the health facility. A study conducted in rural Ethiopia agreed that the difficulty of geographic access to health facilities was identified as one of the primary reasons for patient delay [72], indicating that geographic issues can also influence the timeliness of medical service, particularly in remote and poor areas.
This meta-analysis highlights that socio-demographic factors, including low level of income and unemployment, were positively associated with long patient delay. According to WHO determinants of TB control, risk factors of delayed diagnosis can be divided into three levels: socio-economic, clinical, and health system factors [73]. Most Asian countries have a considerable rural population due to their developing economics. Due to lower incomes, potential TB patients may be less likely to seek care after persistent cough for 3 weeks compared to higher-income individuals [74]. Additionally, there are fewer health facilities in low-economic areas and it is more difficult for patients to seek health-care, subsequently affecting patient delay. Previous studies have shown that unemployment is an independent risk factor for delay in seeking treatment [58]. Pooling the factors together, the data indicate that poverty may discourage patients from seeking health care in a timely manner. Community health workers should design individualized and community-based propaganda and education to address the symptoms of TB. Moreover, community health workers can be effective in the referral of potential patients to rural and national TB control institutions. Therefore, when there is a global emphasis on the use of community health service personnel for disease prevention and control at the rural level, rural health workers could play a key role in the fight against TB [75].
Another factor associated with patient delay was hemoptysis, which negatively correlated with delay. The presence of hemoptysis may be the most characteristic and severe symptom of TB, and it is not surprising that it prompts the initial health consultation [25]. A previous study suggested why hemoptysis can lead to timely physical examinations and a TB diagnosis [76]. It is important to balance the TB severity and the costs associated with seeking care to continue with diagnosis and treatment. In the current report, consultation with a public hospital for the first visit negatively correlated with provider delays. Storla et al. [77] reported similar results in a systematic review, showing that selection of a traditional practitioner for the first visit is associated with prolonged delays in diagnosis in a range of studies. It was also reported that the number and type of provider first consulted were the most important risk factors for diagnosis delay [13]. Thus, understanding how patients seek health care and to attempt to provide sufficient public health care is very important for TB control.
This meta-analysis was limited by the study designs of the included articles, which may explain the heterogeneity to some extent. Almost all included studies were cross-sectional in design, which used a consecutive method of sampling. Cross-sectional studies have a number of inherent limitations that potentially bias the results, such as its low comparability and that it is includes certain confounders. Thus, these studies do not obtain the causality of the observed associations. Although some of the studies were controlled by logistic regressions for these confounders, their residual effect might still have introduced bias. In addition, although the NOS scores of included studies were a little low, they were still in the moderate quality (most 5 or 6 scores) [78,79]. Therefore, it should make the the reliability of this review.
The available studies had different definitions of provider delay, as well as multiple classifications of socio-demographic variables, such as income, education, and types of health facility consulted by TB patients, which limit the comparability of these studies. Although there were varying cut-off points for delay duration (particularly for provider delay), most studies used the same starting point and end point (provider delay had two different end points). However, when the two types of delay are combined, the correlated factors of delays can be better analyzed [24].
Conclusion
This meta-analysis confirms that socio-demographic characteristics, symptoms of TB patients, and long travel distance to the first provider have critical roles in patient delay in TB diagnosis and treatment. However, only male sex and long travel distance to the first provider correlated to both patient and provider delays, suggesting that availability, and particularly timeliness, of public healthcare providers should be primary concerns of policymakers. However, these studies are not comparable because of their weak and sole study designs and various cut-off points for the duration of delays, particularly for provider delay. Future studies are required that use stronger designs (cohort or case-control studies) and can establish causality among affected factors. Moreover, a standard definition of delay will allow for more appropriate comparisons across studies.
Supporting Information
(DOC)
(DOC)
(DOC)
(DOC)
Data Availability
All relevant data are within the paper and its Supporting Information files.
Funding Statement
The authors thank The National Natural Science Funds (81172662/H2603) (http://159.226.244.22/portal/Proj_List.asp) and Specialized Research Fund for the Doctoral Program of Higher Education (20123706110004) (http://www.cutech.edu.cn/cn/kyjj/gdxxbsdkyjj/2013/02/1354173488080563.htm) for the grants supporting the study. The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
References
- 1. Goodchild M, Sahu S, Wares F, Dewan P, Shukla RS, Chauhan LS, et al. A cost-benefit analysis of scaling up tuberculosis control in India. Int J Tuberc Lung Dis. 2011;15(3): 358–362. [PubMed] [Google Scholar]
- 2. WHO. China: health, poverty and economic development. 2005. Dec [cited 17 August 2014] Geneva: World Health Organization; Available: www.who.int/macrohealth/action/CMH_China.pdf. [Google Scholar]
- 3. WHO. Global Tuberculosis Report 2013. 2013. Nov [cited 17 August 2014] Geneva: World Health Organization; Available: http://apps.who.int/iris/bitstream/10665/91355/1/9789241564656_eng.pdf. [Google Scholar]
- 4. WHO. Fact sheets on tuberculosis. 2013. [cited 17 August 2014] Geneva: World Health Organization; Available: http://www.who.int/tb/publications/factsheet_global.pdf?ua=1. [Google Scholar]
- 5. Bjune G. Tuberculosis in the 21st century: an emerging pandemic? Nor Epidemiol. 2005;15(2): 133–139. [Google Scholar]
- 6. Yimer S, Bjune G, Alene G. Diagnostic and treatment delay among pulmonary tuberculosis patients in Ethiopia: a cross sectional study. BMC Infect Dis. 2005;5: 112 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Ward HA, Marciniuk DD, Pahwa P, Hoeppner VH. Extent of pulmonary tuberculosis in patients diagnosed by active compared to passive case finding. Int J Tuberc Lung Dis. 20048(5): 593–597. [PubMed] [Google Scholar]
- 8. Aldhubhani AH, lzham MI, Pazilah I, Anaam MS. Effect of delay in diagnosis on the rate of tuberculosis among close contacts of tuberculosis patients. East Mediterr Health J. 2013;19(10): 837–842. [PubMed] [Google Scholar]
- 9. Nkosi D, Janssen S, Padanilam X, Louw R, Menezes CN, Grobusch MP. Factors influencing specialist care referral of multidrug- and extensively drug-resistant tuberculosis patients in Gauteng/South Africa: a descriptive questionnaire-based study. BMC Health Serv Res. 2013;13: 268 10.1186/1472-6963-13-268 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Farah MG, Rygh JH, Steen TW, Selmer R, Heldal E, Bjune G. Patient and health care system delays in the start of tuberculosis treatment in Norway. BMC Infect Dis. 2006;6: 33 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. WHO. Tuberculosis in the WHO South-East Asia Region. 2010. [cited 17 August 2014] Geneva: World Health Organization; Available: http://www.who.int/bulletin/volumes/88/3/09-073874/en/. 10.2471/BLT.09.073874 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Sreeramareddy CT, Panduru KV, Menten J, Van den Ende J. Time delays in diagnosis of pulmonary tuberculosis: a systematic review of literature. BMC Infect Dis. 2009;9: 91 10.1186/1471-2334-9-91 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Sreeramareddy CT, Qin ZZ, Satyanarayana S, Subbaraman R, Pai M. Delays in diagnosis and treatment of pulmonary tuberculosis in India: a systematic review. Int J Tuberc Lung Dis. 2014;18(3): 255–266. 10.5588/ijtld.13.0585 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Li Y, Ehiri J, Tang S, Li D, Bian Y, Lin H, et al. Factors associated with patient, and diagnostic delays in Chinese TB patients: a systematic review and meta-analysis. BMC Med. 2013;11: 156 10.1186/1741-7015-11-156 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Finnie RK, Khoza LB, van den Borne B, Mabunda T, Abotchie P, Mullen PD. Factors associated with patient and health care system delay in diagnosis and treatment for TB in sub-Saharan African countries with high burdens of TB and HIV. Trop Med Int Health. 2011;16(4): 394–411. 10.1111/j.1365-3156.2010.02718.x [DOI] [PubMed] [Google Scholar]
- 16. Glynn JR. Resurgence of tuberculosis and the impact of HIV infection. Br Med Bull. 1998;54(3): 579–593. [DOI] [PubMed] [Google Scholar]
- 17.Wells GA, Shea B, O’connell D, Peterson JEA, Welch V, Losos M, et al. The Newcastle-Ottawa Scale (NOS) for assessing the quality of nonrandomised studies in meta-analyses. 2000. Available: http://www.medicine.mcgill.ca/rtamblyn/Readings/The%20Newcastle%20-%20Scale%20for%20assessing%20the%20quality%20of%20nonrandomised%20studies%20in%20meta-analyses.pdf.
- 18. Wang W, Jiang Q, Abdullah AS, Xu B. Barriers in accessing to tuberculosis care among non-residents in Shanghai: a descriptive study of delays in diagnosis. Eur J Public Health. 2007;17(5): 419–423. [DOI] [PubMed] [Google Scholar]
- 19. Leung EC, Leung CC, Tam CM. Delayed presentation and treatment of newly diagnosed pulmonary tuberculosis patients in Hong Kong. Hong Kong Med J. 2007;13(3): 221–227. [PubMed] [Google Scholar]
- 20. Huong NT, Vree M, Duong BD, Khanh VT, Loan VT, Co NV, et al. Delays in the diagnosis and treatment of tuberculosis patients in Vietnam: a cross-sectional study. BMC Public Health. 2007;7: 110 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Enkhbat S, Toyota M, Yasuda N, Ohara H. Differing influence on delays in the case-finding process for tuberculosis between general physicians and specialists in Mongolia. J Epidemiol. 1997;7(2): 93–98. [DOI] [PubMed] [Google Scholar]
- 22. Yamasaki-Nakagawa M, Ozasa K, Yamada N, Osuga K, Shimouchi A, Ishikawa N, et al. Gender difference in delays to diagnosis and health care seeking behaviour in a rural area of Nepal. Int J Tuberc Lung Dis. 2001;5(1): 24–31. [PubMed] [Google Scholar]
- 23. Chiang CY, Chang CT, Chang RE, Li CT, Huang RM. Patient and health system delays in the diagnosis and treatment of tuberculosis in Southern Taiwan. Int J Tuberc Lung Dis. 2005;9(9): 1006–1012. [PubMed] [Google Scholar]
- 24. Rojpibulstit M, Kanjanakiritamrong J, Chongsuvivatwong V. Patient and health system delays in the diagnosis of tuberculosis in Southern Thailand after health care reform. Int J Tuberc Lung Dis. 2006;10(4): 422–428. [PubMed] [Google Scholar]
- 25. Li X, Jiang S, Li X, Mei J, Zhong Q, Xu W, et al. Predictors on delay of initial health-seeking in new pulmonary tuberculosis cases among migrants population in East China. PLoS One. 2012;7(2): e31995 10.1371/journal.pone.0031995 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Lock WA, Ahmad RA, Ruiter RA, van der Werf MJ, Bos AE, Mahendradhata Y, et al. Patient delay determinants for patients with suspected tuberculosis in Yogyakarta province, Indonesia. Trop Med Int Health. 2011;16(12): 1501–1510. 10.1111/j.1365-3156.2011.02864.x [DOI] [PubMed] [Google Scholar]
- 27. Zhou C, Tobe RG, Chu J, Gen H, Wang X, Xu L. Detection delay of pulmonary tuberculosis patients among migrants in China: a cross-sectional study. Int J Tuberc Lung Dis. 2012;16(12): 1630–1636. 10.5588/ijtld.12.0227 [DOI] [PubMed] [Google Scholar]
- 28. Chang CT, Esterman A. Diagnostic delay among pulmonary tuberculosis patients in Sarawak, Malaysia: a cross-sectional study. Rural Remote Health. 2007;7(2): 667 [PubMed] [Google Scholar]
- 29. Lin X, Chongsuvivatwong V, Geater A, Lijuan R. The effect of geographical distance on TB patient delays in a mountainous province of China. Int J Tuberc Lung Dis. 2008;12(3): 288–293. [PubMed] [Google Scholar]
- 30. Basnet R, Hinderaker SG, Enarson D, Malla P, Mørkve O. Delay in the diagnosis of tuberculosis in Nepal. BMC Public Health. 2009;9: 236 10.1186/1471-2458-9-236 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Güneylioglu D, Yilmaz A, Bilgin S, Bayram U, Akkaya E. Factors affecting delays in diagnosis and treatment of pulmonary tuberculosis in a tertiary care hospital in Istanbul, Turkey. Med Sci Monit. 2004;10(2): CR62–67. [PubMed] [Google Scholar]
- 32. Hoa NB, Tiemersma EW, Sy DN, Nhung NV, Vree M, Borgdorff MW, et al. Health-seeking behaviour among adults with prolonged cough in Vietnam. Trop Med Int Health. 2011;16(10):1260–1267. 10.1111/j.1365-3156.2011.02823.x [DOI] [PubMed] [Google Scholar]
- 33. Xu B, Diwan VK, Bogg L. Access to tuberculosis care: what did chronic cough patients experience in the way of healthcare-seeking? Scand J Public Health. 2007;35(4): 396–402. [DOI] [PubMed] [Google Scholar]
- 34. Ahmad RA, Richardus JH, de Vlas SJ. Care-seeking behaviour among individuals with TB symptoms in Jogjakarta Province, Indonesia: a community-based study. Int Health. 2013. March;5(1):51–7. 10.1093/inthealth/ihs002 [DOI] [PubMed] [Google Scholar]
- 35. Phoa LL, Teleman MD, Wang YT, Chee CB. Characteristics of patients with delayed diagnosis of infectious pulmonary tuberculosis. Respirology. 2005;10(2): 196–200. [DOI] [PubMed] [Google Scholar]
- 36. Xu X, Liu JH, Cao SY, Zhao Y, Dong XX, Liang Y, et al. Delays in care seeking, diagnosis and treatment among pulmonary tuberculosis patients in Shenzhen, China. Int J Tuberc Lung Dis. 2013;17(5): 615–620. 10.5588/ijtld.12.0231 [DOI] [PubMed] [Google Scholar]
- 37. Rundi C, Fielding K, Godfrey-Faussett P, Rodrigues LC, Mangtani P. Delays in seeking treatment for symptomatic tuberculosis in Sabah, East Malaysia: factors for patient delay. Int J Tuberc Lung Dis. 2011;15(9): 1231–1238, 10.5588/ijtld.10.0585 [DOI] [PubMed] [Google Scholar]
- 38. Zhao X, Yang P, Gai R, Mei L, Wang X, Xu L. Determinants of health care-seeking delay among tuberculosis patients in Shandong Province, China. Eur J Public Health. 2014;24(5): 757–761. 10.1093/eurpub/ckt113 [DOI] [PubMed] [Google Scholar]
- 39. Cheng G, Tolhurst R, Li RZ, Meng QY, Tang S. Factors affecting delays in tuberculosis diagnosis in rural China: a case study in four counties in Shandong Province. Trans R Soc Trop Med Hyg. 2005;99(5): 355–362. [DOI] [PubMed] [Google Scholar]
- 40. Tobe RG, Xu L, Zhou C, Yuan Q, Geng H, Wang X. Factors affecting patient delay of diagnosis and completion of Direct Observation Therapy, Short-course (DOTS) among the migrant population in Shandong, China. Biosci Trends. 2013;7(3): 122–128. [PubMed] [Google Scholar]
- 41. Choudhari M, Jha N, Yadav DK, Chaudhary D. Factors associated with patient delay in diagnosis of pulmonary tuberculosis in a district. J Nepal Health Res Counc. 2012;10(22): 234–238. [PubMed] [Google Scholar]
- 42. Shu W, Chen W, Zhu S, Hou Y, Mei J, Bai L, et al. Factors causing delay of access to tuberculosis diagnosis among new, active tuberculosis patients: a prospective cohort study. Asia Pac J Public Health. 2014;26(1):33–41. 10.1177/1010539513502523 [DOI] [PubMed] [Google Scholar]
- 43. Ngamvithayapong J, Yanai H, Winkvist A, Diwan V. Health seeking behaviour and diagnosis for pulmonary tuberculosis in an HIV-epidemic mountainous area of Thailand. Int J Tuberc Lung Dis. 2001;5(11): 1013–1020. [PubMed] [Google Scholar]
- 44. Selvam JM, Wares F, Perumal M, Gopi PG, Sudha G, Chandrasekaran V, et al. Health-seeking behaviour of new smear-positive TB patients under a DOTS programme in Tamil Nadu, India, 2003. Int J Tuberc Lung Dis. 2007;11(2): 161–167. [PubMed] [Google Scholar]
- 45. Chen HG, Liu M, Jiang SW, Gu FH, Huang SP, Gao TJ, et al. Impact of diabetes on diagnostic delay for pulmonary tuberculosis in Beijing. Int J Tuberc Lung Dis. 2014;18(3): 267–271. 10.5588/ijtld.13.0140 [DOI] [PubMed] [Google Scholar]
- 46. Kelkar-Khambete A, Kielmann K, Pawar S, Porter J, Inamdar V, Datye A, et al. India's Revised National Tuberculosis Control Programme: looking beyond detection and cure. Int J Tuberc Lung Dis. 2008;12(1): 87–92. [PubMed] [Google Scholar]
- 47. Ayé R, Wyss K, Abdualimova H, Saidaliev S. Patient's site of first access to health system influences length of delay for tuberculosis treatment in Tajikistan. BMC Health Serv Res. 2010;10: 10 10.1186/1472-6963-10-10 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Tobgay KJ, Sarma PS, Thankappan KR. Predictors of treatment delays for tuberculosis in Sikkim. Natl Med J India. 2006;19(2): 60–63. [PubMed] [Google Scholar]
- 49. Rumman KA, Sabra NA, Bakri F, Seita A, Bassili A. Prevalence of tuberculosis suspects and their healthcare-seeking behavior in urban and rural Jordan. Am J Trop Med Hyg. 2008;79(4): 545–551. [PubMed] [Google Scholar]
- 50. Wang Y, Long Q, Liu Q, Tolhurst R, Tang S. Treatment seeking for symptoms suggestive of TB: comparison between migrants and permanent urban residents in Chongqing, China. Trop Med Int Health. 2008;13(7): 927–933. 10.1111/j.1365-3156.2008.02093.x [DOI] [PubMed] [Google Scholar]
- 51. Mor Z, Kolb H, Lidji M, Migliori G, Leventhal A. Tuberculosis diagnostic delay and therapy outcomes of non-national migrants in Tel Aviv, 1998–2008. Euro Surveill. 2013;18(12): pii 20433. [PubMed] [Google Scholar]
- 52. Rifat M, Rusen ID, Islam MA, Enarson DA, Ahmed F, Ahmed SM, et al. Why are tuberculosis patients not treated earlier? A study of informal health practitioners in Bangladesh. Int J Tuberc Lung Dis. 2011;15(5): 647–651. 10.5588/ijtld.10.0205 [DOI] [PubMed] [Google Scholar]
- 53. Bai LQ, Xiao SY. Factors associated with diagnostic delay for patients with smear-positive pulmonary tuberculosis in rural Hunan, China. Zhonghua Jie He He Hu Xi Za Zhi. 2004;27(9): 617–620. [PubMed] [Google Scholar]
- 54. Tamhane A, Ambe G, Vermund SH, Kohler CL, Karande A, Sathiakumar N. Pulmonary tuberculosis in mumbai, India: factors responsible for patient and treatment delays. Int J Prev Med. 2012;3(8): 569–580. [PMC free article] [PubMed] [Google Scholar]
- 55. Sabawoon W, Sato H, Kobayashi Y. Delay in the treatment of pulmonary tuberculosis: a report from Afghanistan. Environ Health Prev Med. 2012;17(1): 53–61. 10.1007/s12199-011-0219-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56. Karim F, Islam MA, Chowdhury AM, Johansson E, Diwan VK. Gender differences in delays in diagnosis and treatment of tuberculosis. Health Policy Plan. 2007;22(5): 329–334. [DOI] [PubMed] [Google Scholar]
- 57. Thakur R, Murhekar M. Delay in diagnosis and treatment among TB patients registered under RNTCP Mandi, Himachal Pradesh, India, 2010. Indian J Tuberc. 2013;60(1): 37–45. [PubMed] [Google Scholar]
- 58. Lönnroth K, Thuong LM, Linh PD, Diwan VK. Delay and discontinuity—a survey of TB patients' search of a diagnosis in a diversified health care system. Int J Tuberc Lung Dis. 1999;3(11): 992–1000. [PubMed] [Google Scholar]
- 59. Rajeswari R, Chandrasekaran V, Suhadev M, Sivasubramaniam S, Sudha G, Renu G. Factors associated with patient and health system delays in the diagnosis of tuberculosis in South India. Int J Tuberc Lung Dis. 2002;6(9): 789–795. [PubMed] [Google Scholar]
- 60. Lin HP, Deng CY, Chou P. Diagnosis and treatment delay among pulmonary tuberculosis patients identified using the Taiwan reporting enquiry system, 2002–2006. BMC Public Health. 2009;9: 55 10.1186/1471-2458-9-55 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61. Wang WB, Xiu Y, Jiang WL, Jiang QW, Xu B. Diagnostic delay and its factors in access to tuberculosis care in northern rural Jiangsu province. Fudan Xuebao (Yixuekexueban). 2006; 33(1): 33–38. [Google Scholar]
- 62. Lin CY, Lin WR, Chen TC, Lu PL, Huang PM, Tsai ZR, et al. Why is in-hospital diagnosis of pulmonary tuberculosis delayed in southern Taiwan? J Formos Med Assoc. 2010;109(4): 269–277. 10.1016/S0929-6646(10)60052-6 [DOI] [PubMed] [Google Scholar]
- 63. WHO. Cases: Mortality and prevalence by country (all years). 2007. [cited 17 August 2014] Geneva: World Health Organization; Available: http://apps.who.int/gho/data/view.main.57020ALL?lang=en [Google Scholar]
- 64. WHO. Early detection of tuberculosis: an overview of approaches, guidelines and tools. 2011. [cited 17 August 2014] Geneva: World Health Organization; Available: https://extranet.who.int/iris/restricted/bitstream/10665/70824/1/WHO_HTM_STB_PSI_2011.21_eng.pdf. [Google Scholar]
- 65. Glanz KR, Rimer BK, Viswanath K. Health behavior and health education: Theory, research, and practice. 4th ed. John Wiley & Sons; 2008. [Google Scholar]
- 66. Sendagire I, Schim Van der Loeff M, Mubiru M, Konde-Lule J, Cobelens F. Long delays and missed opportunities in diagnosing smear-positive pulmonary tuberculosis in Kampala, Uganda: a cross-sectional study. PLoS One. 2010;5(12): e14459 10.1371/journal.pone.0014459 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67. Jurcev-Savicevic A, Mulic R, Kozul K, Ban B, Valic J, Bacun-Ivcek L, et al. Health system delay in pulmonary tuberculosis treatment in a country with an intermediate burden of tuberculosis: a cross-sectional study. BMC Public Health. 2013;13: 250 10.1186/1471-2458-13-250 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68. Jurcev-Savicevic A, Kardum G. Health-care seeking behaviour for tuberculosis symptoms in Croatia. Eur J Public Health. 2012;22(4): 573–577. 10.1093/eurpub/ckr132 [DOI] [PubMed] [Google Scholar]
- 69. Long NH, Diwan VK, Winkvist A. Difference in symptoms suggesting pulmonary tuberculosis among men and women. J Clin Epidemiol. 2002;55(2): 115–120. [DOI] [PubMed] [Google Scholar]
- 70. Yang WT, Gounder CR, Akande T, De Neve JW, McIntire KN, Chandrasekhar A, et al. Barriers and delays in tuberculosis diagnosis and treatment services: does gender matter? Tuberc Res Treat. 2014;2014: 461935 10.1155/2014/461935 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71. Krishnan L, Akande T, Shankar AV, McIntire KN, Gounder CR, Gupta A, et al. Gender-related barriers and delays in accessing tuberculosis diagnostic and treatment services: a systematic r1eview of qualitative studies. Tuberc Res Treat. 2014;2014: 215059 10.1155/2014/215059 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72. Tadesse T, Demissie M, Berhane Y, Kebede Y, Abebe M. Long distance travelling and financial burdens discourage tuberculosis DOTs treatment initiation and compliance in Ethiopia: a qualitative study. BMC Public Health. 2013;13: 424 10.1186/1471-2458-13-424 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73. WHO. The global plan to stop TB 2011–2015: transforming the fight towards elimination of tuberculosis. 2010. [cited 17 August 2014] Geneva: World Health Organization; Available: http://apps.who.int/iris/bitstream/10665/44437/1/9789241500340_eng.pdf?ua=1. 10.1371/journal.pone.0108591 [DOI] [Google Scholar]
- 74. Zhang T, Tang S, Jun G, Whitehead M. Persistent problems of access to appropriate, affordable TB services in rural China: experiences of different socio-economic groups. BMC Public Health. 2007;7: 19 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75. Hipgrave D. Communicable disease control in China: From Mao to now. J Glob Health. 2011;1(2): 224–238. [PMC free article] [PubMed] [Google Scholar]
- 76. Meyssonnier V, Li X, Shen X, Wang H, Li DY, Liu ZM, et al. Factors associated with delayed tuberculosis diagnosis in China. Eur J Public Health. 2013;23(2): 253–257. 10.1093/eurpub/cks037 [DOI] [PubMed] [Google Scholar]
- 77. Storla DG, Yimer S, Bjune GA. A systematic review of delay in the diagnosis and treatment of tuberculosis. BMC Public Health. 2008;8: 15 10.1186/1471-2458-8-15 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78. van Dijk GM, Maneva M, Colpani V, Dhana K, Muka T, Jaspers L, et al. The association between vasomotor symptoms and metabolic health in peri- and postmenopausal women: A systematic review. Maturitas. 2015;80(2): 140–147. 10.1016/j.maturitas.2014.11.016 [DOI] [PubMed] [Google Scholar]
- 79. Bechard LJ, Rothpletz-Puglia P, Touger-Decker R, Duggan C, Mehta NM. Influence of obesity on clinical outcomes in hospitalized children: a systematic review. JAMA Pediatr. 2013;167(5): 476–482. 10.1001/jamapediatrics.2013.13 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
(DOC)
(DOC)
(DOC)
(DOC)
Data Availability Statement
All relevant data are within the paper and its Supporting Information files.