Abstract
Objective
This study quantitatively examined the prevalence and correlates of short-term sex work cessation among female sex workers who inject drugs (FSW-IDUs) and determined whether injection drug use was independently associated with cessation.
Methods
We used data from FSW-IDUs (n=467) enrolled into an intervention designed to increase condom use and decrease sharing of injection equipment but was not designed to promote sex work cessation. We applied a survival analysis that accounted for quit-re-entry patterns of sex work over 1-year stratified by city, Tijuana and Ciudad Juarez, Mexico.
Results
Overall, 55% of participants stopped sex work at least once during follow-up. Controlling for other characteristics and intervention assignment, injection drug use was inversely associated with short-term sex work cessation in both cities. In Ciudad Juarez, women receiving drug treatment during follow-up had a 2-fold increase in the hazard of stopping sex work. In both cities, income from sources other than sex work, police interactions and healthcare access were independently and significantly associated with shorter-term cessation.
Conclusions
Short-term sex work cessation was significantly affected by injection drug use. Expanded drug treatment and counseling coupled with supportive services such as relapse prevention, job training, and provision of alternate employment opportunities may promote longer-term cessation among women motivated to leave the sex industry.
1. INTRODUCTION
Female sex workers (FSWs) experience increased rates of HIV and other sexually transmitted or blood-borne infections, which is elevated among FSWs who inject drugs (FSW-IDUs) (Strathdee et al., 2008). Given the nature of their work, FSWs are likely to experience violence, including physical and sexual abuse (Ulibarri et al., 2011; Urada et al., 2013) and isolation from health and social services (Rekart, 2005). As a result of experiences with psychological trauma, many women use substances as a coping mechanism (Ulibarri et al., 2013). For some, sex is primarily exchanged to finance a substance dependency (Ohlund and Gronbladh, 2009; Potterat et al., 1998).
However, among women that desire to leave the sex industry, multiple barriers exist (Sanders, 2007). Studies have described a combination of factors including financial necessity, drug addictions, intimate relationships, having children, coercion from others, criminal records, and lack of resources as reasons to remain in sex work (Baker et al., 2010; Cimino, 2012; Ingabire et al., 2012; Manopaiboon et al., 2003). Absent is an empirical assessment on the extent to which these factors independently predict cessation. Understanding this information may inform interventions addressing the health and social needs of women who use drugs and are attempting to leave the sex industry.
In cities situated along the Mexico-U.S. border sex work is quasi-legal. An estimated 9,000 FSWs in Tijuana, Mexico (adjacent to San Diego, California) and 4,000 FSWs in Ciudad Juarez, Mexico (adjacent to El Paso, Texas) operate from a mix of establishments (Patterson et al., 2008a). In Tijuana, sex work is tolerated in the city’s red-light district (Curtis and Arreola, 1991), whereas Ciudad Juarez dismantled its red-light district and displaced sex workers to more hidden locations (Wright, 2004). In 2006, HIV prevalence was estimated at 6% among FSWs and 12% among FSWs that injected drugs in these two cities. (Patterson et al., 2008b).
Tijuana and Ciudad Juarez are also situated along major drug trafficking routes into the United States. Both cities have experienced a rise in HIV prevalence and injection drug use (Bucardo et al., 2005) with IDUs estimated at 10,000 and 6,500, respectively (Ramos et al., 2009). Mexico’s growing HIV epidemic has been linked to structural conditions that increase HIV risk behaviors and other adverse outcomes among IDUs (Beletsky et al., 2013). Therefore, it is important to understand the context in which sex work and drug use are co-occurring in order to inform efforts that address sex work cessation.
Given that previous studies have primarily been qualitative with small sample sizes (Baker et al., 2010; Cimino, 2012; Ingabire et al., 2012; Manopaiboon et al., 2003), the goal of this study is to empirically examine the prevalence and correlates of stopping sex work during a one-year period among FSW-IDUs participating in an HIV prevention intervention to reduce sexual and injection risk behaviors, and determine whether injection drug use independently associates with cessation after controlling for other characteristics. Knowledge gained may aid in the development of support services promoting longer-term sex work cessation.
2. METHODS
2.1 Study Population
From October 2008– 2009, outreach workers recruited 584 HIV-negative FSW-IDUs into a behavioral intervention to reduce high risk HIV-related behaviors. Briefly, women were randomized into one of four groups combining either an interactive or didactic version of an intervention to promote condom use and the reduction of injection paraphernalia sharing. The interactive intervention incorporated theory-driven skill-building elements that focused on: 1) improving one’s ability to negotiate condom use within context of her or her partner’s substance use and/or 2) reduce receptive and/or distributive sharing of injection equipment. Under the didactic version, women received information on safer sex and/or safer injection in lecture-style formatted using printed materials provided from a local health center; there were no theory-driven skills-building elements under this version (see Vera et al., 2012 for a detailed description of the intervention).
Eligibility criteria included being ≥ 18 years; having unprotected vaginal or anal sex with a male client in the previous month; injecting illicit drugs and sharing injection equipment in the past month; test HIV-negative at baseline; speaking Spanish or English; no plans to move out of the city for a 12-month period; providing informed consent; and accepting free sexually transmitted infection (STI) testing and treatment. The present study includes an additional 33 participants that were HIV-positive at baseline who were randomized into an intervention group.
2.2 Data Collection
Participants were administered face-to-face interviews and biological testing for HIV/STIs at baseline with 3 follow-up visits occurring approximately at 4, 8, and 12 months after enrollment. Interviews covered a range of questions, including sociodemographics, health, sexual and drug using behaviors. Follow-up rates were 89.6% at 4-month, 87.7% at 8-month, and 87.1% at 12-month visits.
Trained nurses obtained biological samples from participants at each visit. HIV status was ascertained using the “Determine”® rapid HIV antibody test (Abbott Pharmaceuticals, Boston, MA). Syphilis serology was conducted using the rapid plasma regain test (Determine™ Syphilis TP; Abbott Pharmaceuticals, Boston, MA). Positive samples were subject to confirmatory testing. Neisseria gonorrhea (GC) and Chlamydia trachomatis (CT) were detected from vaginal swabs using a rapid test kit (BioStar® OIA® GC and CHLAMYDIA). Participants with a positive GC/CT test or symptoms were treated free on-site. The study was approved by the Institutional Review Boards at the University of California San Diego, the General Hospital in Tijuana, and the Universidad Autonoma de Ciudad Juarez.
2.3 Measures
2.3.1 Outcome
The outcome was short-term cessation of sex work, measured in days. Participants were identified as leaving sex work if they answered yes to the following question during follow-up “In the past 4 months, have you stopped trading sex for money, drugs, or other goods (food, clothing, etc.) for a period of at least 30 days?”. Of the n = 617 participants, we excluded 27% for the following reasons: 1) completed baseline interview only n=19, 2) death for reasons unrelated to study participation n=10 or 3) missed at least one follow-up visit n = 140. As these women were engaged in sex work and drug use, we could not assume their missed visits were random events; a requirement for censoring observations (see, for example, Ranganathan & Pramesh 2012). Our concern was that participants missed follow-up visits for reasons related to the study such as they had stopped sex work, they were institutionalized (e.g., incarcerated or in drug treatment), or they were entrenched in sex work and drug use; although reasons for missed visits were not assessed. Therefore, a total of 467 participants were included in the current analysis. Lastly, we allowed for recurrent events since 28% of the participants (n=132) stopped sex work more than once during follow-up.
2.3.2 Independent Variables
Several baseline covariates were considered: sociodemographics, years injecting drugs, sex work history, testing positive for HIV, Chlamydia, gonorrhea, and/or active syphilis (titers ≥ 1:8), lifetime pregnancies or induced abortions, condom availability, police extortion, history of forced/coerced sex with client, and history of physical abuse and rape. We only considered what was reported at study enrollment since there was little variation over time among these covariates.
Due to skip patterns in questionnaire items measuring substance use behavior among those who had not injected drugs between follow-up visits, we only included what was reported at baseline for the following: heroin, methamphetamine and cocaine use in the month prior to study enrollment, drug use with clients in the month prior to study enrollment, and a continuous measure of safer injection self-efficacy previously developed by a U.S. intervention study (Garfein et al., 2007).
Covariates that varied over the study period included housing status, injection frequency, income outside of sex work, healthcare access, drug treatment, police confiscation of drug paraphernalia, increased police presence, incarceration, and a continuous measures of condom use self-efficacy previously developed by a Mexico intervention study (Patterson et al., 2008a).
2.4 Recurrent Event Analysis
Given that participants could have recurrent reports of stopping sex work during follow-up, we applied a conditional proportional hazards model proposed by Prentice, Williams, and Peterson (1981) or PWP model using STATA 11 (StataCorp, LP, College Station, TX, USA). The PWP model assumes that a subject is not at risk for a later event until the all previous events have been experienced. The ordering of events is tracked by stratifying the data where the stratum indicates the event number for which the subject is at risk (see Ezell et al. 2003 for detailed description of PWP model and its application). Therefore, the model is conditional in the sense that a subject is not at risk for the 2nd event until the 1st event has occurred and the baseline hazard is event-specific.
The time interval in which a subject was at risk of experiencing the event was defined using a counting process formulation. Under the counting process, time at risk is not defined by the beginning of the study - similar to “resetting the clock” to zero each time an event occurred; rather time at risk is defined by the previous event (e.g., the right time of the prior event defines the left time of the next event). We applied this risk interval since we assumed subsequent reports of stopping sex work would be a function of time since the previous reported events. As a result, the PWP-counting process method allowed us to model the time to an event while simultaneously accounting for the repeated occurrence of the same type of event (e.g., stopping sex work) and the order in which these events occurred. We corrected for the correlation of events within a subject by adjusting the covariance matrix of the parameter estimates using a robust variance estimator (Lin and Wei, 1989).
The assumption of proportional hazard model was tested using a generalized least-squares score test (Grambsch and Therneau, 1994). Nonparametric methods were applied to generate estimates of the survival function by the different patterns of sex work cessation.
Models were stratified by site since sex work is regulated differently across cities. Univariate models tested for associations between sex work cessation and the covariates of interest. The multivariate model was manually built in a stepwise fashion by including covariates with a p-value < 0.25 from the univariate analysis followed by a backward selection eliminating covariates with a p-value > 0.10 in the multivariate model. To ensure that potential confounders were not prematurely removed, we re-entered covariates initially excluded and they were retained if the coefficient estimates of other variables changed by 10% and the Akaike information criterion decreased.
3. RESULTS
3.1 Sample Characteristics
The median age of participants across both cities was 33 years (Interquartile Range, IQR: 28–41) with a median of 12 years in sex work (IQR: 6–18) and 11 years of injection drug use (IQR: 5–18). The majority of women (97%, n=452) reported heroin use and slightly more than one-third reported methamphetamine use (38%, n = 179) or cocaine use (34%, n= 159) in the month prior to study enrollment.
3.2 Time to Stopping Sex Work
Over half (55%; n=256) of participants stopped trading sex for 30 days or longer at least once during follow-up. As shown in Table 1, nearly three-fourths of the Tijuana sample stopped sex work at least once during follow-up. By contrast, 33% stopped sex work at least once in Ciudad Juarez.
Table 1.
Number of reports on sex work cessation during follow-up by site (n=467)
| Number of Reports | Overall (n=467) | Tijuana (n=233) | Ciudad Juarez (n=234) |
|---|---|---|---|
| 0 | 211 (45.2%) | 55 (23.6%) | 156 (66.7%) |
| 1 | 124 (26.6%) | 68 (29.2%) | 56 (23.9%) |
| 2 | 83 (17.8%) | 68 (29.2%) | 15 (6.4%) |
| 3 | 49 (10.5%) | 42 (18.0%) | 7 (3.0%) |
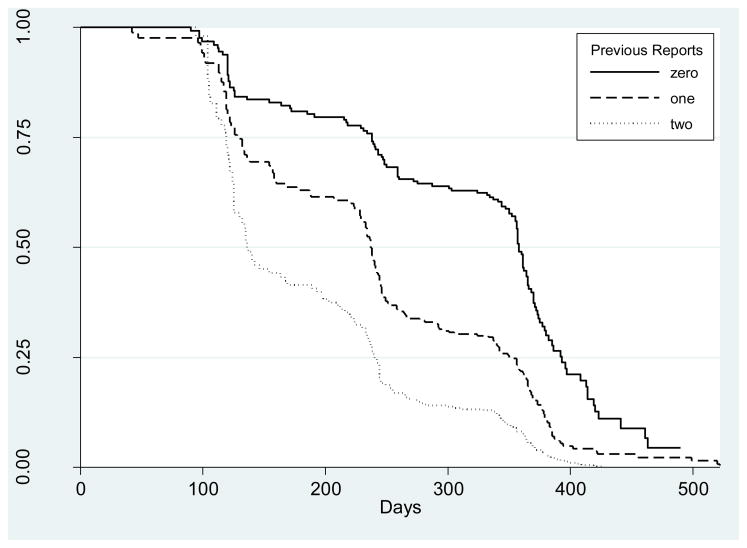
Across the entire sample, the time to sex work cessation decreased throughout follow-up and varied by the number of previous reports of stopping sex work (Figure 1). The median time to the first report of stopping sex work was 233 days followed by 113 days for the second occurrence; and among those with a least two prior reports, the median time to the third occurrence of sex work cessation was 22 days.
Figure 1.
Median time to sex work cessation dependent on previous reports of stopping sex work
3.3 Reasons for Stopping Sex Work
Across both cities, the most common reason for stopping sex work was a desire for a new life or being tired of sex work (Table 2). In Tijuana, additional reasons included: 1) entering drug treatment (33.7%), 2) incarceration (20.8%) or 3) health concerns (18%). In Ciudad Juarez, women mentioned their fear of acquiring HIV/STIs (11.5%) and health concerns (11.5%) as reasons to stop sex work.
Table 2.
Reasons for leaving sex work at least once during follow-up by site (n=256)
| Reason for Leaving Sex Work | Overall (n=256) | Tijuana (n=178) | Ciudad Juarez (n = 78) |
|---|---|---|---|
| Tired of trading sex/want a different life | 123 (48.0%) | 76 (42.7%) | 50 (64.1%) |
| In drug treatment | 65 (25.4%) | 60 (33.7%) | 5 (6.4%) |
| Incarcerated | 38 (14.8%) | 37 (20.8%) | 1 (1.3%) |
| Health concerns (including pregnancy) | 27 (10.5%) | 18 (10.1%) | 9 (11.5%) |
| Fear of getting HIV/STIs | 24 (9.4%) | 15 (8.4%) | 9 (11.5%) |
| Found another/better occupation | 20 (7.8%) | 16 (9.0%) | 4 (5.1%) |
| Family or partner concerns | 20 (7.8%) | 18 (10.1%) | 2 (2.6%) |
| Could not work for health or other reasons | 11 (4.3%) | 9 (5.1%) | 2 (2.6%) |
| Needed more money than sex work provided | 8 (3.1%) | 6 (3.4%) | 2 (2.6%) |
| Didn’t want/need the money | 8 (3.1%) | 4 (2.3%) | 4 (5.1%) |
| Fear of physical/sexual abuse | 6 (2.3%) | 5 (2.8%) | 1 (1.3%) |
| Fear of pregnancy | 3 (1.2%) | 2 (1.1%) | 1 (1.3%) |
3.4 Univariate Analysis
In both cities, sleeping somewhere other than ones’ own place and injection frequency significantly decreased the unadjusted hazard of sex work cessation, whereas having an income from sources other than sex work and receiving drug treatment significantly increased the unadjusted hazard of sex work cessation (Tables 3 and 4).
Table 3.
Unadjusted and Adjusted Hazard Ratios (95% CIs) for leaving sex work among FSW-IDUs in Tijuana (n=233)
| Unadjusted HR (95% CI) | p- value | Adjusted HR (95% CI) | p- value | |
|---|---|---|---|---|
| Sociodemographics | ||||
| Steady partner/spouse at enrollment | 0.71 (0.55, 0.92) | 0.010 | ||
| Has ≥ 1 financial dependents at enrollment | 0.80 (0.62, 1.03) | 0.088 | 0.73 (0.55, 0.96) | 0.026 |
| Children < 18 living with you at enrollment | 0.79 (0.61. 1.03) | 0.086 | ||
| Average monthly income < 3,500 pesos | 1.42 (1.08. 1.86) | 0.012 | 1.35 (0.98, 1.86) | 0.063 |
| Slept somewhere other than own place a | 0.58 (0.46, 0.73) | <0.001 | ||
| Lived in city of study enrollment entire life | 1.34 (1.03, 1.76) | 0.030 | ||
| Age (5-year increase) | 1.05 (0.97, 1.13) | 0.247 | ||
| Substance Use | ||||
| Heroin b | 1.86 (0.99, 3.42) | 0.051 | 1.87 (0.88, 3.99) | 0.104 |
| Methamphetamine b | 0.68 (0.52, 0.90) | 0.007 | 0.72 (0.54, 0.96) | 0.026 |
| Cocaine b | 0.78 (0.57, 1.07) | 0.130 | 0.78 (0.57, 1.06) | 0.109 |
| Often/always used drugs with clients b | 0.96 (0.72, 1.26) | 0.751 | ||
| Injected drugs in past month a | 0.44 (0.34, 0.57) | < 0.001 | 0.55 (0.43, 0.72) | < 0.001 |
| Years as injection drug user (5-year increase) | 1.01 (0.94, 1.08) | 0.853 | ||
| Injected more than once a day in past month a | 0.57 (0.44, 0.73) | <0.001 | ||
| Self-efficacy towards safer injection | 0.88 (0.71, 1.08) | 0.226 | ||
| Sex Work History | ||||
| Street-based sex worker | 1.10 (0.83, 1.45) | 0.513 | ||
| >50% of clients are regular | 1.07 (0.82, 1.39) | 0.625 | ||
| Ever paid a pimp | 0.66 (0.34, 1.28) | 0.217 | ||
| Poor working conditions | 1.22 (0.93, 1.58) | 0.146 | ||
| Income from sources other than sex work a | 4.66 (3.29, 6.60) | < 0.001 | 3.83 (2.64, 5.55) | < 0.001 |
| Started sex work before age 18 | 0.85 (0.65, 1.10) | 0.219 | 0.71 (0.54, 0.92) | 0.009 |
| Years as sex worker (1-year increase) | 1.01 (0.99, 1.02) | 0.360 | ||
| Sexual Health | ||||
| HIV positive | 1.24 (0.69, 2.25) | 0.474 | ||
| Self-efficacy towards condom use a | 0.91 (0.67, 1.23) | 0.547 | ||
| Any STI at enrollment | 0.87 (0.64, 1.19) | 0.386 | ||
| Had an induced abortion during lifetime | 1.06 (0.68, 1.64) | 0.792 | ||
| Number of pregnancies during lifetime (1- unit increase) | 1.02 (0.95, 1.09) | 0.591 | ||
| Structural Factors | ||||
| Increased access to health services a | 0.84 (0.62, 1.15) | 0.275 | 1.48 (1.10, 1.99) | 0.011 |
| Received drug treatment a | 1.46 (1.15, 1.83) | 0.001 | ||
| Police confiscated drug paraphernalia a | 0.74 (0.54, 1.03) | 0.073 | ||
| Increased police presence a | 0.67 (0.53, 0.83) | < 0.001 | ||
| Arrested a | 0.83 (0.64, 1.08) | 0.164 | ||
| Sexual abuse by police in lieu of arrest c | 1.36 (0.99, 1.87) | 0.059 | 2.22 (1.55, 3.17) | < 0.001 |
| Police took money in lieu of arrest c | 0.71 (0.54, 0.93) | 0.012 | 0.52 (0.39, 0.70) | < 0.001 |
| Ever forced/coerced into having sex with client | 1.04 (0.76, 1.42) | 0.829 | ||
| History of physical abuse by client | 0.99 (0.72, 1.35) | 0.967 | ||
| History of rape | 0.85 (0.65, 1.11) | 0.236 | ||
| Intervention Group | ||||
| Both didactic injection and sex risk (control) | 1.00 | 1.00 | ||
| Interactive injection risk and didactic sex risk | 0.93 (0.69, 1.26) | 0.643 | 0.92 (0.63, 1.33) | 0.653 |
| Interactive sex risk and didactic injection risk | 1.09 (0.81, 1.45) | 0.582 | 0.91 (0.64, 1.30) | 0.617 |
| Both interactive injection and sex risk | 0.93 (0.69, 1.26) | 0.645 | 1.01 (0.69, 1.46) | 0.976 |
Refers to an event occurring since last follow-up visit;
Refers to an event occurring 1 month prior to study enrollment;
Refers to an event occurring within 6 months prior to study enrollment.
Table 4.
Unadjusted and Adjusted Hazard Ratios (95% CIs) for leaving sex work among FSW-IDUs in Ciudad Juarez (n=234)
| Unadjusted HR (95% CI) | p- value | Adjusted HR (95% CI) | p- value | |
|---|---|---|---|---|
| Sociodemographics | ||||
| Steady partner/spouse at enrollment | 0.85 (0.53, 1.38) | 0.516 | ||
| Has ≥ 1 financial dependents at enrollment | 0.78 (0.49, 1.26) | 0.315 | ||
| Children < 18 living with you at enrollment | 1.41 (0.89. 2.22) | 0.144 | ||
| Average monthly income < 3,500 pesos | 1.20 (0.75, 1.92) | 0.450 | ||
| Slept somewhere other than own place a | 0.53 (0.36, 0.79) | 0.002 | ||
| Lived in city of study enrollment entire life | 1.50 (0.93, 2.43) | 0.096 | ||
| Age (5-year increase) | 1.09 (0.96, 1.23) | 0.196 | ||
| Substance Use | ||||
| Heroin b | 0.58 (0.14, 2.31) | 0.435 | ||
| Methamphetamine b | 1.54 (0.50, 4.71) | 0.448 | ||
| Cocaine b | 0.64 (0.39, 1.05) | 0.076 | ||
| Often/always used drugs with clients b | 0.80 (0.50, 1.27) | 0.349 | ||
| Injected drugs in past month a | 0.19 (0.13, 0.28) | < 0.001 | 0.45 (0.24, 0.86) | 0.016 |
| Years as injection drug user (5-year increase) | 1.02 (0.89, 1.16) | 0.811 | ||
| Injected more than once a day in past month a | 0.25 (0.16, 0.38) | < 0.001 | ||
| Self-efficacy towards safer injection | 0.93 (0.60, 1.43) | 0.728 | ||
| Sex Work History | ||||
| Street-based sex worker | 0.87 (0.55, 1.40) | 0.579 | 0.69 (0.40, 1.21) | 0.196 |
| >50% of clients are regular | 0.84 (0.33, 2.17) | 0.722 | ||
| Ever paid a pimp | 0.47 (0.09, 2.42) | 0.370 | 0.33 (0.12, 0.88) | 0.025 |
| Poor working conditions | 1.36 (0.84, 2.22) | 0.216 | ||
| Income from sources other than sex work a | 6.94 (4.22, 11.42) | < 0.001 | 4.42 (2.44, 8.02) | < 0.001 |
| Started sex work before age 18 | 0.58 (0.37, 0.93) | 0.023 | 0.63 (0.36, 1.09) | 0.098 |
| Years as sex worker (1-year increase) | 0.99 (0.96, 1.01) | 0.405 | ||
| Sexual Health | ||||
| HIV positive | 2.17 (1.18, 3.97) | 0.012 | ||
| Self-efficacy towards condom use a | 1.53 (1.06, 2.20) | 0.024 | ||
| Any STI at enrollment | 0.92 (0.54, 1.56) | 0.746 | ||
| Had an induced abortion during lifetime | 0.66 (0.21, 2.05) | 0.473 | ||
| Number of pregnancies during lifetime (1- unit increase) | 0.96 (0.87, 1.07) | 0.464 | ||
| Structural Factors | ||||
| Increased access to health services a | 1.63 (0.95, 2.82) | 0.077 | 3.29 (1.73, 6.27) | < 0.001 |
| Received drug treatment a | 4.79 (3.13, 7.32) | < 0.001 | 3.43 (1.86, 6.34) | < 0.001 |
| Police confiscated drug paraphernalia a | 0.71 (0.37, 1.40) | 0.325 | ||
| Increased police presence a | 0.88 (0.50, 1.52) | 0.623 | 0.48 (0.25, 0.90) | 0.023 |
| Arrested a | 0.80 (0.46, 1.40) | 0.441 | ||
| Sexual abuse by police in lieu of arrest c | 0.58 (0.30, 1.12) | 0.103 | ||
| Police took money in lieu of arrest c | 1.12 (0.67, 1.85) | 0.671 | ||
| Ever forced/coerced into having sex with client | 0.62 (0.35, 1.10) | 0.104 | ||
| History of physical abuse by client | 0.84 (0.50, 1.39) | 0.492 | ||
| History of rape | 0.77 (0.48, 1.22) | 0.260 | ||
| Intervention Group | ||||
| Both didactic injection and sex risk (control) | 1.00 | 1.00 | ||
| Interactive injection risk and didactic sex risk | 1.03 (0.62, 1.72) | 0.904 | 0.62 (0.30, 1.30) | 0.203 |
| Interactive sex risk and didactic injection risk | 0.93 (0.56, 1.56) | 0.787 | 1.04 (0.51, 2.14) | 0.909 |
| Both interactive injection and sex risk | 1.23 (0.72, 2.08) | 0.448 | 0.78 (0.36, 1.71) | 0.539 |
Refers to an event occurring since last follow-up visit;
Refers to an event occurring 1 month prior to study enrollment;
Refers to an event occurring within 6 months prior to study enrollment.
3.5 Multivariate Analysis
In the adjusted model, FSW-IDUs in Tijuana who had financial dependents, used methamphetamine, started sex work before age 18 or experienced sexual abuse by police were significantly more likely to stop sex work than those without these characteristics; those reporting extortion of money by police had a decreased hazard of stopping sex work (Table 3).
In Ciudad Juarez, FSW-IDUs with a history of paying a pimp or that reported increased police presence were less likely to stop sex work independent of other characteristics in the model (Table 4); whereas receiving drug treatment increased the hazard of sex work cessation.
Across both cities, injecting drugs during follow-up was inversely associated with stopping sex work (Tijuana adj HR: 0.55, 95% CI: 0.43, 0.72; Ciudad Juarez adj HR: 0.45, 95% CI: 0.24, 0.86); whereas income from sources other than sex work (Tijuana adj HR: 3.83, 95% CI: 2.64, 5.55; Ciudad Juarez adj HR: 4.42, 95% CI: 2.44, 8.02) and increased access to health services (Tijuana adj HR: 1.48, 95% CI: 1.10, 1.99; Ciudad Juarez adj HR: 3.29, 95% CI: 1.73, 6.27) increased the hazard of stopping sex work. Further, women receiving the sexual and/or injection risk intervention were not significantly more likely to stop sex work than those in the control group. There was substantial overlap in the 95% confidence intervals suggesting a similar effect between intervention groups in both cities.
4. DISCUSSION
This study identified individual and structural circumstances affecting short-term sex work cessation among FSW-IDUs that routinely received behavioral risk reduction counseling as part of a larger HIV prevention study. Although increased condom use and decreased sharing of injection equipment were the primary outcomes of the original study, a promising finding of the current study was that despite intervention assignment, decreased frequency of injection drug use, income from sources other than sex work, and healthcare access significantly and independently increased the hazard of leaving sex work. However, several differences were found between these cities, including receipt of drug treatment and police interactions, suggesting there are unique environmental structures shaping the transition out of sex work.
As demonstrated in qualitative studies (Ingabire et al., 2012; Manopaiboon et al., 2003), we found empirical evidence that injection drug use was an important correlate of short-term sex work cessation. Women that reported injecting drugs had a lower hazard of stopping sex work, independent of other characteristics (e.g., the odds for the time to stopping sex work was lower among those who continued to inject drugs compared to those that did not inject in the past month). This finding is consistent with an earlier study by our team that found a high proportion of women injected drugs before or concurrent to sex work initiation (Morris et al., 2013). Further, dependence on sex work to support addictions is one reason that women remain in sex work (Deering et al., 2011) and this is more prevalent in street-based sex workers (Cusick, 2006; Inciardi and Surratt, 2001). In the current study, nearly three-fourths of FSW-IDUs in Tijuana and half of FSW-IDUs in Ciudad Juarez primarily operated from street corners. For these women, it may be difficult to discontinue sex work given their entrenchment in a street subculture where violence, exploitation and drug markets coexist (Cimino, 2012; Dalla, 2006).
Among women motivated to leave the sex industry, access to effective drug treatment services and counseling may help them overcome addictions and cease sex work. For example, one study found that 97% of FSWs successfully treated for heroin dependence quit sex work during their first year of treatment (Gunne et al., 1995). In qualitative interviews conducted by our research team, drug using FSWs’ identified the lack of effective drug treatment and psychological support as a major barrier to stopping sex work (Goldenberg et al., 2013).
Our findings further illustrate this contention since receipt of drug treatment was positively associated with stopping sex work, although this was only significant in Ciudad Juarez after adjusting for other characteristics. A possible reason for this observation is that during the time of the study, Ciudad Juarez had a publicly funded methadone program, whereas only private methadone clinics were operating in Tijuana. Mexican policymakers are planning to scale-up opioid substitution treatment across the country. Our study findings suggest that in doing so, there may be benefits to the cessation of drug use and sex work.
Financial capacity was another important factor since income outside of sex work was positively associated with stopping sex work. Prior studies have found that legal employment opportunities and job stability not only enabled FSWs to leave sex work but also sustained their ability to avoid returning to sex work (Dalla, 2006; Ingabire et al., 2012). This suggests the need for interventions that target women’s economic situations through vocational training and/or micro finance programs, especially since financial necessity to support dependent children was frequently cited as a key reason for entering sex work in this region (Bucardo et al., 2004; Patterson et al., 2005).
Police interactions were also independently associated with short-term cessation of sex work. In Tijuana, FSW-IDUs who reported sexual abuse from police in lieu of arrest stopped sex work at twice the hazard of those not reporting such abuses. Violence such as physical or sexual assaults, more often reported by street-based FSWs, has been a catalyst for contemplating withdrawal from sex work due to FSWs’ concern for their physical safety (Sanders, 2007). Further, violence against FSWs has been associated with HIV risk in these cities and other settings (Beletsky et al., 2013; Shannon and Csete, 2010) and a women’s decision to leave sex work may be influenced by her perceived HIV risk (Manopaiboon et al., 2003).
In comparison, we found that extortion of money by police (in Tijuana only) and increased police presence (in Ciudad only) were inversely associated with sex work cessation. These women may have encountered the criminal justice system more frequently and felt compelled to remain in sex work to pay fines (Sanders, 2007) since they were actively injecting drugs at study enrollment. These findings may also be proxy for women feeling less in control of their environment.
By study design, this analysis has limitations that warrant consideration. First, differential recall of the exact time a participant left sex work is a potential source of bias since we often did not ascertain this until several months after it occurred. Instead, we used follow-up time as our time scale for the outcome variable, which has been suggested in other studies (Fieberg and DelGiudice, 2009; Pencina et al., 2007). This analytic approach allowed us to consider multiple reports rather than the first or any occurrence of sex work cessation and included characteristics that varied over time (for example, frequency of injection drug use, receiving drug treatment and income outside of sex work). Second, 27% of the original sample was excluded because of loss to follow-up. This may have biased our results if participants stopped trading sex or conversely, they did not attend their follow-up visit due to being entrenched in drugs and sex work. Women excluded from the analysis were significantly less likely to have ever received drug treatment or report any abuses by police at baseline. Lastly, our findings may not be generalizable to other drug using FSWs since our sample consisted of women engaged in risky behaviors (e.g., unprotected sex and sharing injection equipment). However, this lack of representation also makes our sample of high importance to public health and public policy given that these women engaged in behaviors that increases their likelihood of acquiring and transmitting HIV and other blood-borne infections.
5. CONCLUSIONS
The current study is among the first to quantitatively identify factors associated with short-term sex work cessation including the cessation of injection drug use. Although substantial barriers to stopping sex work exist, the current findings suggest a particular need for support services among those motivated to leave the industry. Expanded drug treatment and counseling, including relapse prevention, job training, employment, and micro finance programs may be the most important strategies to reduce women’s reliance on sex work and promote capacity towards the transition out of sex work (Cusick et al., 2011). However, future research should also consider the need for support services for those who desire to remain in sex work. Lastly, since sex work is regulated differently across jurisdictions, our results highlight the need for policy reforms focusing on exploitive policing practices that make it more difficult for women to leave sex work and expose them to multiple health problems.
HIGHLIGHTS.
We examined factors related to stopping sex work among female injection drug users
A survival analysis was applied to account for quit-re-entry patterns of sex work
Over half of participants stopped sex work during a 1-year period
Injection drug use was inversely associated with stopping sex work
Drug treatment and counseling combined with other supportive services are needed
Acknowledgments
Role of Funding Sources
This study was funded by the National Institute on Drug Abuse grants, K01DA034523, R01DA023877, 3R01DA028692-04S1. The funding source did not have any involvement in the conduct of the research nor in the preparation or submission of the manuscript.
We acknowledge support from the by the National Institute on Drug Abuse grants (K01DA034523, R01DA023877, 3R01DA028692-04S1).
Footnotes
Contributors
All of the authors contributed to the writing of the manuscript. TLG, SAS originated the study. TLG led in writing the draft of the manuscript and conducted data analysis; LU assisted with literature review; GM, GR supervised field activities relating to data collection; LU, SM, ER, TP, SAS assisted with interpretation of results. All authors critically reviewed multiple versions and approved final manuscript.
Conflict of Interest
All authors declare that they have no conflict of interest.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- Baker LM, Dalla RL, Williamson C. Exiting prostitution: An integrated model. Violence against Women. 2010;16:579–600. doi: 10.1177/1077801210367643. [DOI] [PubMed] [Google Scholar]
- Beletsky L, Lozada R, Gaines T, Abramovitz D, Staines H, Vera A, Rangel G, Arredondo J, Strathdee SA. Syringe confiscation as an HIV risk factor: The public health implications of arbitrary policing in Tijuana and Ciudad Juarez, Mexico. Journal of Urban Health. 2013;90:284–298. doi: 10.1007/s11524-012-9741-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bucardo J, Brouwer KC, Magis-Rodriguez C, Ramos R, Fraga M, Perez SG, Patterson TL, Strathdee SA. Historical trends in the production and consumption of illicit drugs in Mexico: Implications for the prevention of blood borne infections. Drug and Alcohol Dependence. 2005;79:281–293. doi: 10.1016/j.drugalcdep.2005.02.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bucardo J, Semple SJ, Fraga-Vallejo M, Davila W, Patterson TL. A qualitative exploration of female sex work in Tijuana, Mexico. Archives of Sexual Behavior. 2004;33:343–351. doi: 10.1023/B:ASEB.0000028887.96873.f3. [DOI] [PubMed] [Google Scholar]
- Cimino AN. A predictive theory of intentions to exit street-level prostitution. Violence against Women. 2012;18:1235–1252. doi: 10.1177/1077801212465153. [DOI] [PubMed] [Google Scholar]
- Collins SP, Goldenberg SM, Burke NJ, Bojorquez-Chapela I, Silverman JG, Strathdee SA. Situating HIV risk in the lives of formerly trafficked female sex workers on the Mexico-US border. AIDS Care. 2013;25:459–465. doi: 10.1080/09540121.2012.720361. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Curtis JR, Arreola DD. Zonas-de-tolerancia on the northern Mexican border. Geography Review. 1991;81:333–346. [Google Scholar]
- Cusick L. Widening the harm reduction agenda: From drug use to sex work. International Journal of Drug Policy. 2006;17:3–11. [Google Scholar]
- Cusick L, Brooks-Gordon B, Campbell R, Edgar F. ‘Exiting’ drug use and sex work: Career paths, interventions and government strategy targets. Drugs: Education, Prevention and Policy. 2011;18:145–156. [Google Scholar]
- Dalla RL. “You can’t hustle all your life”: An exploratory investigation of the exit process among street-level prostituted women. Psychology of Women Quarterly. 2006;30:276–290. [Google Scholar]
- Deering KN, Shoveller J, Tyndall MW, Montaner JS, Shannon K. The street cost of drugs and drug use patterns: relationships with sex work income in an urban Canadian setting. Drug and Alcohol Dependence. 2011;118:430–436. doi: 10.1016/j.drugalcdep.2011.05.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ezell ME, Land KC, Cohen LE. Modeling mulitple failure time data: A survey of variance-corrected proportional hazards models with emperical applications to arrest data. Sociological Methodology. 2003;33:111–167. [Google Scholar]
- Fieberg J, DelGiudice GD. What time is it? Choice of time origin and scale in extended proportional hazards models. Ecology. 2009;90:1687–1697. doi: 10.1890/08-0724.1. [DOI] [PubMed] [Google Scholar]
- Garfein RS, Golub ET, Greenberg AE, Hagan H, Hanson DL, Hudson SM, Kapadia F, Latka MH, Ouellet L, Purcell DW, Strathdee SA, Thiede H, Team DS. A peer-education intervention to reduce injection risk behaviors for HIV and hepatitis C virus infection in young injection drug users. AIDS. 2007;21:1923–1932. doi: 10.1097/QAD.0b013e32823f9066. [DOI] [PubMed] [Google Scholar]
- Goldenberg SM, Engstrom D, Rolon ML, Silverman JG, Strathdee SA. Sex workers perspectives on strategies to reduce sexual exploitation and HIV risk: A qualitative study in Tijuana, Mexico. PLoS One. 2013;8(8):e72982. doi: 10.1371/journal.pone.0072982. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goldenberg SM, Strathdee SA, Perez-Rosales MD, Sued O. Mobility and HIV in Central America and Mexico: A critical review. Journal of immigrant and minority health. 2012;14:48–64. doi: 10.1007/s10903-011-9505-2. [DOI] [PubMed] [Google Scholar]
- Grambsch PM, Therneau TM. Proportional hazards tests and diagnostics based on weighted residuals. Biometrika. 1994;81:515–526. [Google Scholar]
- Gunne LM, Gronbladh L, Ohlund LS. The street life and treatment response of 105 heroin-addicted women. In: Tagliamonte A, Maremmani I, editors. Drug Addiction and Related Clinical Problems. New York: Springer-Verlag; 1995. pp. 91–107. [Google Scholar]
- Hiller SP, Syvertsen JL, Lozada R, Ojeda VD. Social support and recovery among Mexican female sex workers who inject drugs. Journal of substance abuse treatment. 2013;45:44–54. doi: 10.1016/j.jsat.2012.12.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Inciardi JA, Surratt HL. Drug use, street crime, and sex-trading among cocaine-dependent women: Implications for public health and criminal justice policy. Journal of psychoactive drugs. 2001;33:379–389. doi: 10.1080/02791072.2001.10399923. [DOI] [PubMed] [Google Scholar]
- Ingabire MC, Mitchell K, Veldhuijzen N, Umulisa MM, Nyinawabega J, Kestelyn E, Van Steijn M, Van de Wijgert J, Pool R. Joining and leaving sex work: experiences of women in Kigali, Rwanda. Culture, Health & Sexuality. 2012;14:1037–1047. doi: 10.1080/13691058.2012.713120. [DOI] [PubMed] [Google Scholar]
- Lin DY, Wei LJ. The robust inference for the Cox proportional hazards model. Journal of the American Statistical Association. 1989;84:1074–1078. [Google Scholar]
- Loza O, Strathdee SA, Lozada R, Staines H, Ojeda VD, Martinez GA, Amaro H, Patterson TL, Proyecto Mujer. Correlates of early versus later Initiation into sex work in two Mexico-US border cities. The Journal of Adolescent Health. 2010;46:37–44. doi: 10.1016/j.jadohealth.2009.06.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Manopaiboon C, Bunnell RE, Kilmarx PH, Chaikummao S, Limpakarnjanarat K, Supawitkul S, St Louis ME, Mastro TD. Leaving sex work: barriers, facilitating factors and consequences for female sex workers in northern Thailand. AIDS Care. 2003;15:39–52. doi: 10.1080/012021000039743. [DOI] [PubMed] [Google Scholar]
- Morris MD, Lemus H, Wagner KD, Martinez G, Lozada R, Gomez RG, Strathdee SA. Factors associated with pathways toward concurrent sex work and injection drug use among female sex workers who inject drugs in northern Mexico. Addiction. 2013;108:161–170. doi: 10.1111/j.1360-0443.2012.04016.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ohlund LS, Gronbladh L. Patterns of deviant career in the history of female methadone clients: an exploratory study. International Journal of Social Welfare. 2009;18:95–101. [Google Scholar]
- Ojeda VD, Burgos JL, Hiller SP, Lozada R, Rangel G, Vera A, Artamonova I, Magis-Rodriguez C. Circular migration by Mexican female sex workers who are injection drug users: Implications for HIV in Mexican sending communities. Journal of Immigrant Health. 2012a;14:107–115. doi: 10.1007/s10903-011-9512-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ojeda VD, Burgos JL, Rangel MG, Lozada R, Vera A. U.S. drug use and migration experiences of Mexican female sex workers who are injection drug users. Journal of Health Care for the Poor and Underserved. 2012b;23:1733–1749. doi: 10.1353/hpu.2012.0177. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Patterson TL, Mausbach B, Lozada R, Staines-Orozco H, Semple SJ, Fraga-Vallejo M, Orozovich P, Abramovitz D, de la Torre A, Amaro H, Martinez G, Magis-Rodriguez C, Strathdee SA. Efficacy of a brief behavioral intervention to promote condom use among female sex workers in Tijuana and Ciudad Juarez, Mexico. American Journal of Public Health. 2008a;98:2051–2057. doi: 10.2105/AJPH.2007.130096. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Patterson TL, Semple SJ, Fraga M, Bucardo J, Davila-Fraga W, Strathdee SA. An HIV-prevention intervention for sex workers in Tijuana, Mexico: A pilot study. Hispanic Journal of Behavioral Sciences. 2005;27:82–100. [Google Scholar]
- Patterson TL, Semple SJ, Staines H, Lozada R, Orozovich P, Bucardo J, Philbin MM, Pu M, Fraga M, Amaro H, De la Torre A, Martinez G, Magis-Rodriguez C, Strathdee SA. Prevalence and correlates of HIV infection among female sex workers in 2 Mexico-US border cities. The Journal of Infectious Diseases. 2008b;197:728–732. doi: 10.1086/527379. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pencina MJ, Larson MG, D’Agostino RB. Choice of time scale and its effect on significance of predictors in longitudinal studies. Statistics in Medicine. 2007;26:1343–1359. doi: 10.1002/sim.2699. [DOI] [PubMed] [Google Scholar]
- Potterat JJ, Rothenberg RB, Muth SQ, Darrow WW, Phillips-Plummer L. Pathways to prostitution: The chronology of sexual and drug abuse milestones. Journal of Sex Research. 1998;35:333–340. [Google Scholar]
- Prentice RL, Williams BJ, Peterson AV. On the regression-analysis of mulitvariate failure time data. Biometrika. 1981;68:373–379. [Google Scholar]
- Ramos R, Ferreira-Pinto JB, Brouwer KC, Ramos ME, Lozada RM, Firestone-Cruz M, Strathdee SA. A tale of two cities: Social and environmental influences shaping risk factors and protective behaviors in two Mexico-US border cities. Health and Place. 2009;15:999–1005. doi: 10.1016/j.healthplace.2009.04.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ranganathan P, Pramesh CS. Censoring in survival analysis: Potential for bias. Perspectives in Clinical Research. 2012;3(1):40. doi: 10.4103/2229-3485.92307. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rekart ML. Sex-work harm reduction. Lancet. 2005;366:2123–2134. doi: 10.1016/S0140-6736(05)67732-X. [DOI] [PubMed] [Google Scholar]
- Sanders T. Becoming an ex-sex worker: Making transitions out of a deviant career. Feminist Criminology. 2007;2:1–19. [Google Scholar]
- Shannon K, Csete J. Violence, Condom Negotiation, and HIV/STI Risk Among Sex Workers. JAMA. 2010;304:573–574. doi: 10.1001/jama.2010.1090. [DOI] [PubMed] [Google Scholar]
- Strathdee SA, Philbin MM, Semple SJ, Pu M, Orozovich P, Martinez G, Lozada R, Fraga M, de la Torre A, Staines H, Magis-Rodriguez C, Patterson TL. Correlates of injection drug use among female sex workers in two Mexico-US border cities. Drug and Alcohol Dependence. 2008;92:132–140. doi: 10.1016/j.drugalcdep.2007.07.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ulibarri MD, Strathdee SA, Ulloa EC, Lozada R, Fraga MA, Magis-Rodriguez C, De La Torre A, Amaro H, O’Campo P, Patterson TL. Injection drug use as a mediator between client-perpetrated abuse and HIV status among female sex workers in two Mexico-US border cities. AIDS and Behavior. 2011;15:179–185. doi: 10.1007/s10461-009-9595-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ulibarri MD, Hiller SP, Lozada R, Rangel MG, Stockman JK, Silverman JG, Ojeda VD. Prevalence and characteristics of abuse experiences and depression symptoms among injection drug-using female sex workers in Mexico. Journal of Environmental and Public Health. 2013:Aritcle ID 631479. doi: 10.1155/2013/631479. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Urada LA, Strathdee SA, Morisky DE, Schilling RE, Simbulan NP, Estacio LR, Raj A. Sex work and its associations with alcohol and methamphetamine use among female bar and spa workers in the Philippines. Asian Pacific Journal of Public Health. 2013;26(2):138–46. doi: 10.1177/1010539512471969. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vera A, Abramovitz D, Lozada R, Martinez G, Rangel MG, Staines H, Patterson TL, Strathdee SA. Mujer mas segura (safer women): A combination prevention intervention to reduce sexual and injection risks among female sex workers who inject drugs. BMC Public Health. 2012;12:653. doi: 10.1186/1471-2458-12-653. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Villarreal A, Hamilton ER. Rush to the border? Market liberalization and urban- and rural-origin internal migration in Mexico. Social Science Research. 2012;41:1275–1291. doi: 10.1016/j.ssresearch.2012.02.007. [DOI] [PubMed] [Google Scholar]
- Wright MW. From protests to politics: Sex work, women’s worth, and Ciudad Juarez modernity. Annals of the Association of American Geographers. 2004;94:369–386. [Google Scholar]