Abstract
Background
Discordant practice patterns may be a consequence of evidence–practice gaps or deficiencies in knowledge translation. We examined the current strategies used by hepato-pancreatico-biliary (HPB) surgeons in Canada for the perioperative management of pancreaticoduodenectomy (PD).
Methods
We generated a web-based survey that focused on the perioperative measures surrounding PD. The survey was distributed to all members of the Canadian Hepato-Pancreatico-Biliary Association.
Results
The survey was distributed to 74 surgeons and received a response rate of 50%. Many similarities in surgical techniques were reported; for example, most surgeons (86.5%) reconstruct the pancreas with pancreaticojejunostomy rather than pancreaticogastrostomy. In contrast, variable techniques regarding the use of peritoneal drainage tubes, anastomotic stents, octreotide and other intraoperative modalities were reported. Most surgeons (75.7%) reported that their patients frequently required preoperative biliary drainage, yet there was minimal agreement with the designated criteria. There was variability in postoperative care, including the use of epidural analgesia and timing of postoperative oral nutrition.
Conclusion
We identified heterogeneity among Canadian HPB surgeons, suggesting a number of evidence–practice gaps within specific domains of pancreatic resections. Focused research in these areas may facilitate technical agreement and improve patient outcomes following PD.
Abstract
Contexte
La discordance entre les modes de pratique pourrait être due à des lacunes au plan des pratiques fondées sur des preuves ou à une déficience du transfert des connaissances. Nous avons étudié les stratégies actuellement utilisées par les chirurgiens hépato-pancréato-biliaires (HPB) au Canada pour la prise en charge périopératoire de la pancréatoduodénectomie (PD).
Méthodes
Nous avons préparé un questionnaire électronique sur les mesures périopératoires entourant la PD. Le questionnaire a été distribué à tous les membres de l’Association hépato-pancréato-biliaire canadienne.
Résultats
Le questionnaire a été distribué à 74 chirurgiens et a généré un taux de réponse de 50 %. De nombreuses similitudes dans les techniques chirurgicales ont été signalées : par exemple, la majorité des chirurgiens (86,5 %) reconstruisent le pancréas par pancréatojéjunostomie plutôt que par pancréatogastrostomie. En revanche, on a observé une variabilité dans les techniques d’utilisation des drains péritonéaux, des endoprothèses anastomotiques, des octréotides et autres modalités peropératoires. La majorité des chirurgiens (75,7 %) ont signalé que leurs patients avaient souvent besoin de drains biliaires préopératoires et pourtant, les critères désignés ne semblaient pas faire l’unanimité. On a aussi noté des différences dans les soins postopératoires, y compris en ce qui concerne le recours à l’analgésie péridurale et le moment de la reprise de l’alimentation orale après la chirurgie.
Conclusion
Nous avons observé une hétérogénéité dans la pratique des chirurgiens HPB canadiens, ce qui donne à penser qu’il existe des lacunes au plan des pratiques fondées sur des preuves pour certains aspects précis des résections pancréatiques. Une recherche plus approfondie sur ces aspects pourrait favoriser le consensus technique et améliorer les résultats chez les patients après une PD.
Pancreatic ductal adenocarcinoma is the fourth leading cause of cancer-related deaths worldwide.1 In 2014, there were an estimated 4700 new cases of pancreatic cancer in Canada and 4400 deaths, with a 5-year relative survival rate of 8%.2 Although there have been recent advances in understanding the underlying pathophysiology of pancreatic cancer as well as the diagnosis, staging and treatment of early-stage tumours, minimal progress has been made in the early detection, prevention and treatment of late-stage disease.3,4
Surgery remains the only potential curative intervention; however, owing to the late clinical presentation of disease only 15%–20% of pancreatic tumours are technically resectable.5 The treatment of choice for resectable tumours found within the pancreatic head or uncinate process is pancreaticoduodenectomy (PD), also known as a Whipple resection.6 Pancreaticoduodenectomy is a high-risk procedure that is typically performed by specialized surgeons at high-volume centres;7 however, despite significant reductions in postoperative mortality and morbidity over the past few decades, overall prognosis after resection for patients with pancreatic adenocarcinoma remains poor.8–10
The improved perioperative outcomes may be credited to recent technical advancements in the surgical management of pancreatic malignancies; however, rapid evolution of perioperative care has the potential to introduce heterogeneity into surgical practice.11,12 The process of translating new research findings into routine clinical practice may be stagnant and inconsistent, yet failing to do so (known as an evidence–practice gap) can negatively affect the quality of patient care.13–15
Our objective was to survey Canadian surgeons who perform PD to understand current perioperative practice patterns. We sought to elucidate the existence of evidence–practice gaps in this population and identify domains in which future research opportunities may yield fruitful findings.
Methods
We generated a survey to evaluate the current practice patterns in Canada for the surgical treatment of pancreatic cancer. The survey contained 41 questions with multiple domains of interest, including training and practice; perioperative management of all pancreatic cancer; and preoperative, intraoperative and postoperative measures for PD. Three hepato-pancreatico-biliary (HPB) surgeons piloted the survey, and we used their feedback to optimize the clarity of the survey.
This web-based survey was designed and distributed using the online survey tool SurveyMonkey. It was distributed by email to all members of the Canadian Hepato-Pancreatico-Biliary Association and to surgeons affiliated with the HPB CONCEPT Team, a national collaborative group of HPB surgeons. Following a modified Dillman method,16 we gave recipients 5 weeks to respond to the survey and sent them weekly electronic reminders. After this 5-week period, each nonresponder was sent an individualized reminder to complete the survey. All responses were collected anonymously. We conducted a random draw for a token gift as an incentive for recipients to complete our survey.
Survey data were descriptively analyzed and illustrated using GraphPad Prism software version 5.03 (GraphPad Software, Inc.).
Results
Of the 74 Canadian surgeons invited to participate, 37 (50.0%) completed the survey in its entirety. Nearly all respondents practised in academic hospitals located in urban centres (Table 1). Most surgeons had subspecialty training in HPB (73.0%), followed by transplantation (43.2%) and surgical oncology (27.0%). Most participants (67.6%) devoted more than 75% of their practices to HPB surgeries, with a diverse range of years in practice and in the volume of surgeries performed annually. All surgeons actively performed PD.
Table 1.
Characteristics of study population (n = 37)
| Charactertistic | No. (%) |
|---|---|
| Province of practice | |
| Alberta | 4 (10.8) |
| British Columbia | 1 (2.7) |
| Manitoba | 1 (2.7) |
| New Brunswick | 0 (0.0) |
| Newfoundland & Labrador | 1 (2.7) |
| Nova Scotia | 2 (5.4) |
| Ontario | 22 (59.5) |
| Prince Edward Island | 0 (0.0) |
| Quebec | 5 (13.5) |
| Saskatchewan | 1 (2.7) |
| Territories | 0 (0.0) |
| Years in practice | |
| < 5 | 9 (24.3) |
| 5–10 | 11 (29.7) |
| 11–15 | 6 (16.2) |
| > 15 | 11 (29.7) |
| Practice setting (population) | |
| > 250 000 | 35 (94.6) |
| 100 000–250 000 | 2 (5.4) |
| < 100 000 | 0 (0.0) |
| Practice setting | |
| Academic (university-affiliated) | 36 (97.3) |
| Community | 1 (2.7) |
| Subspecialty/fellowship training | |
| Laparoscopy | 3 (8.1) |
| HPB | 27 (73.0) |
| Surgical oncology | 10 (27.0) |
| Transplantation | 16 (43.2) |
| None | 1 (2.7) |
| Percentage of practice devoted to HPB surgery | |
| < 25% | 3 (8.1) |
| 25–50% | 3 (8.1) |
| 51–75% | 6 (16.2) |
| > 75% | 25 (67.6) |
| No. of HPB surgeries performed in past year* | |
| < 20 | 0 (0.0) |
| 20–40 | 8 (21.6) |
| 41–60 | 6 (16.2) |
| 61–80 | 9 (24.3) |
| 81–100 | 9 (24.3) |
| > 100 | 5 (13.5) |
HPB = hepato-pancreatico-biliary.
Includes transplants.
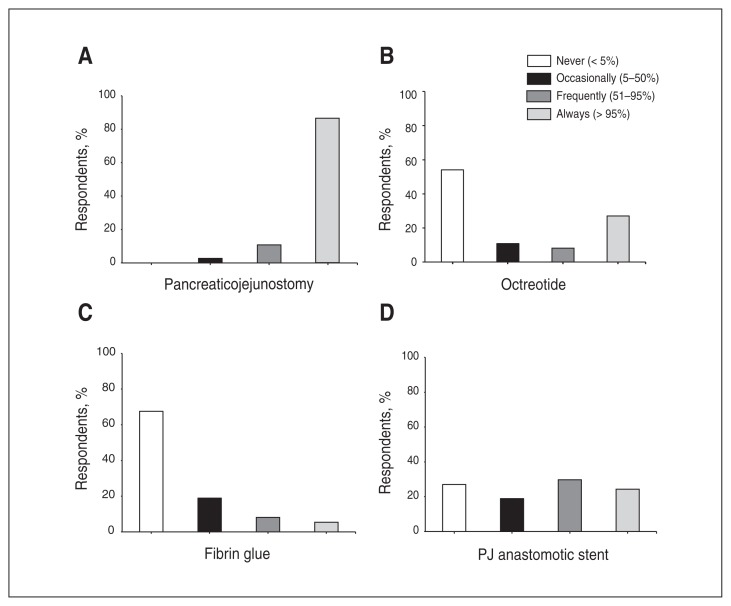
Participants were asked a variety of questions regarding perioperative techniques when performing the pancreaticoenteric reconstruction during PD. Nearly all surgeons (86.5%) reported always performing pancreaticojejunostomy (PJ) rather than pancreaticogastrostomy (PG) (Fig. 1A). Furthermore, nearly all surgeons (94.4%) reported using the duct-to-mucosa method rather than the dunking method when performing PJ. The use of octreotide and other somatostatin analogues was polarized, with the majority of respondents either never (54.1%) or always (27.0%) administering it (Fig. 1B). Hemostatic agents, such as fibrin glue or Tisseel, were not commonly used, with most surgeons citing occasionally or not at all using them (Fig. 1C). In contrast, there was great variability regarding the use of PJ anastomotic stents (Fig. 1D).
Fig. 1.
Frequency of various perioperative techniques used for pancreaticoenteric anastomosis during pancreaticoduodenectomy (PD). PJ = pancreaticojejunostomy.
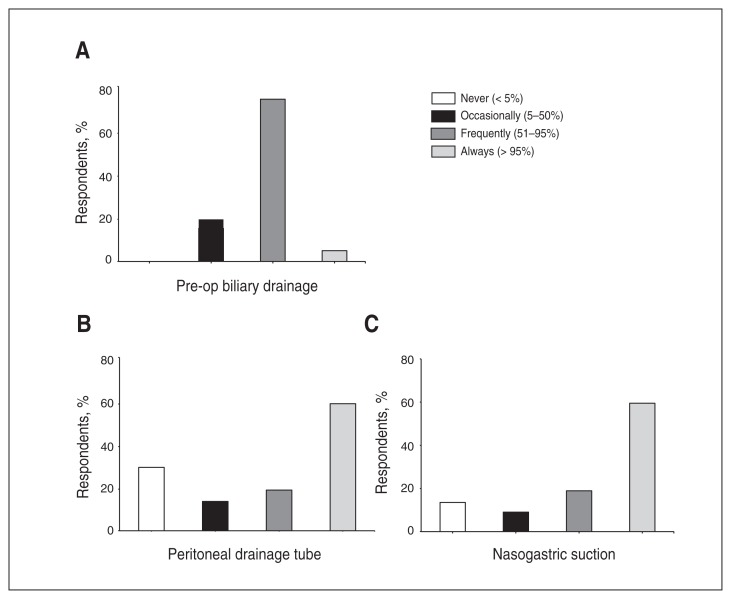
Participants were asked about their use of various drains and endoluminal catheters. Most surgeons reported that their patients frequently undergo preoperative biliary drainage (75.7%; Fig. 2A). There was significant variability in the criteria used to select patients for stenting, including laboratory tests (liver function tests, serum bilirubin), clinical symptoms (jaundice) and surgical wait times. There was minimal agreement on the intraoperative placement of peritoneal drainage tubes (Fig. 2B). Just over half (59.5%) of surgeons reported always using nasogastric (NG) suction tubes (Fig. 2C).
Fig. 2.
Frequency of various perioperative drainage procedures surrounding pancreaticoduodenectomy (PD).
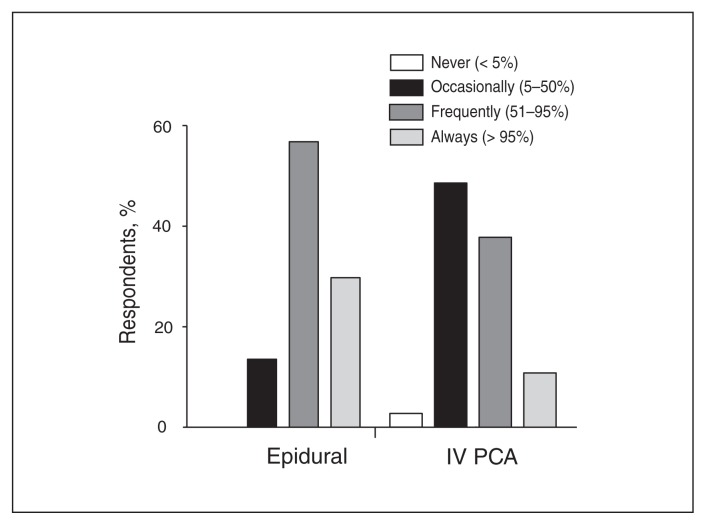
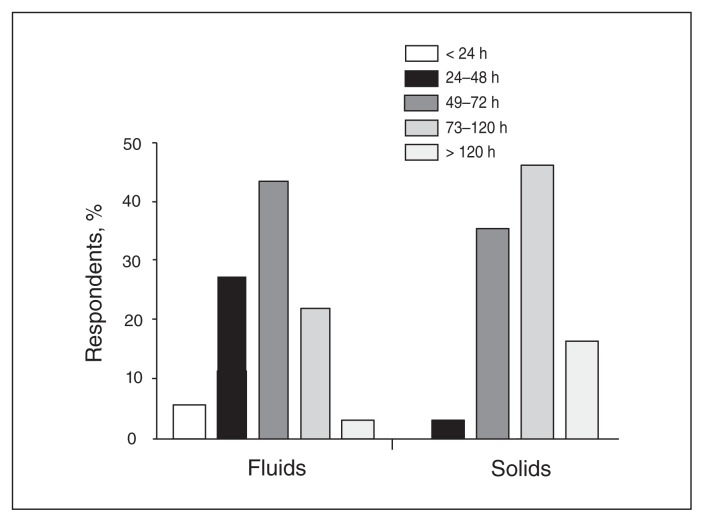
In the postoperative setting, there is no discernible consensus for the ideal method of analgesia after PD. A greater number of surgeons reported always (29.7%) or frequently (56.8%) using epidural analgesia than surgeons who reported always (10.8%) or frequently (37.8%) using intravenous patient-controlled analgesia (IV PCA; Fig. 3). Two surgeons described occasionally using transversus abdominis plane (TAP) blocks. Heterogeneity was also observed regarding the timing of oral nutrition introduction postoperatively. A large proportion of respondents reported that they start clear fluids at 49–72 hours (43.3%) and solid foods at 73–120 hours (45.9%), yet many surgeons cited earlier and later times (Fig. 4). Interestingly, only a small number of participants (37.8%) described implementing standardized postoperative pathways, such as an enhanced recovery after surgery (ERAS) program.
Fig. 3.
The use of various methods to manage postoperative pain following pancreaticoduodenectomy (PD). IV PCA = intravenous patient-controlled analgesia.
Fig. 4.
Time to the initiation of postoperative oral nutrition following pancreaticoduodenectomy (PD).
Discussion
Reconstruction of pancreaticoenteric continuity is a critical step following PD owing to its association with major postoperative complications. A leak of the pancreatic anastomosis and subsequent fistula formation remains the most significant contributor to morbidity and mortality.17 Potential interventions that are subject to ongoing debate include the anastomotic technique, octreotide, hemostatic agents and anastomotic stents.
In the present study, there was remarkable agreement among surgeons regarding the preferred reconstruction technique, with the majority always performing PJ compared with PG. Many studies have compared PJ with PG, and a consensus over the most effective technique remains to be determined; although several reports have shown similar outcomes between the 2 manoeuvres,18–21 others have found that PG reduces the incidence of postoperative fistula.22–24 Given the overwhelming preference for PJ over PG, quality evidence supporting a single technique has the potential to drastically change the postoperative course for patients undergoing PD.
Octreotide and other somatostatin analogues function to inhibit the release of endocrine and exocrine pancreatic secretions,25 a process that effectively reduces the volume of secretions and may decrease the incidence of anastomotic leaks and pancreatic fistulas. The precise role of prophylactic octreotide remains controversial; a number of recent studies have reported inconsistent effects on postoperative complications, yet a Cochrane review on the subject concluded that perioperative complications were reduced following somatostatin analogue treatment during pancreatic resections.26 Interestingly, despite this evidence most Canadian surgeons do not administer somatostatin analogues. It is unclear whether this apparent lack of knowledge translation is a result of knowledge deficits or critical appraisal of the existing data.
Other modalities that have been investigated in an attempt to optimize the pancreaticoenteric reconstruction have not been shown to be of great benefit. Hemostatic agents, such as a fibrin glue sealant, have recently been found to have no significant impact on the incidence of pancreatic leak, fistula formation or other postoperative complications.27,28 Moreover, PJ anastomotic stents, which have been hypothesized to facilitate drainage of secretions from the pancreatic duct and reduce the rate of leaks and fistulas, have not been convincingly shown to be of benefit.29,30
There remains considerable controversy surrounding the role of biliary stenting before PD. Patients with pancreatic cancer often present with obstructive jaundice due to biliary obstruction, placing them at risk for coagulation disturbances, hepatic dysfunction and cholangitis, thus promoting biliary decompression. More recently, the routine use of preoperative biliary drainage has been linked to increased perioperative infectious complications, morbidity and mortality.31 Despite this evidence, the use of biliary drains has increased over the last 2 decades.32 Given this apparent discordance between strong level-I evidence and actual clinical practice, the development of guidelines regarding the role for preoperative biliary drainage are needed. Indications may include the presence of cholangitis, liver dysfunction, severe jaundice and delayed time to surgery.33 This is a target for future research and knowledge translation to avoid unnecessary preoperative biliary drainage and associated complications.
The use of prophylactic intraperitoneal drains has historically been routine practice following pancreatic surgery with the intent to remove postoperative fluid collections and to facilitate early detection of anastomotic leaks, fistulas and hemorrhages. Contrary to this dogma, a growing body of evidence has failed to demonstrate a decrease in the frequency and severity of postoperative complications or the necessity for intervention and that the use of intraperitoneal drains after PD should not be mandatory.34–37 However, a randomized controlled trial was recently stopped early by the Data Safety Monitoring Board because mortality increased from 3% to 12% in patients undergoing PD without intraperitoneal drainage; these patients also had increased frequency and severity of complications.38 The authors cautioned against abandoning the use of intraperitoneal drains in all patients undergoing PD, explicitly stating that this would not be safe. This study’s divergent findings from the literature emphasize that further investigation into the utility and safety of this practice are of paramount importance.
Nasogastric suction has also historically been standard practice after major intra-abdominal procedures. Proponents postulate that NG suction decreases the risk of postoperative complications, such as ileus, anastomotic leaks, fistulas and wound dehiscence.39 More recent studies challenge this dogma and suggest that routine NG decompression is not warranted after elective abdominal surgeries.40 Specifically, routine NG tubes after PD may negatively impact the postoperative course and result in unnecessary patient discomfort. They also contribute to prolonged hospital stays, and their early removal is a critical component of fast-track surgical pathways.41 Thus, many authors advocate NG placement selectively in patients with delayed gastric emptying.42,43 Our data demonstrate that the majority of respondents always or frequently use NG suction after PD, indicating an important evidence–practice gap in the surveyed population.
Our study identified further variability regarding the optimal method of postoperative analgesia, with epidural analgesia somewhat favoured over IV PCA. Interestingly, this observation reflects the general opinion throughout the surgical literature. Epidural analgesia provides superior pain relief after PD than IV PCA;44 however, the impact of epidural analgesia on postoperative morbidity and mortality is not completely understood. Recent studies have suggested that epidural use results in fewer postoperative complications;45 in contrast, epidural analgesia has been found to promote hemodynamic instability following PD and possibly contributes to an increased incidence of various gastrointestinal and respiratory complications.46 Further research is warranted to determine the appropriate method of analgesia following PD in order to optimize pain relief and minimize complications.
The ERAS program is a novel, multimodal, structured concept that is designed to accelerate postoperative recovery, shorten the length of stay in hospital and decrease the rate of complications. The ERAS program has recently been safely applied to major pancreatic resections, such as PD, with demonstrated improved short-term outcomes.41,47–49 One of the most reproducible predictors of successful ERAS is early oral nutrition, with clear fluids often initiated on postoperative day 1 and solid foods on postoperative days 3–5; this is earlier than reported by the majority of our study population, who are mostly not practising ERAS. Other critical features of ERAS include minimizing epidural use, limiting postoperative NG suction, removing drains early and ambulating early. Many of these measures have been described in the present study, and ERAS is one strategy to promote their use and narrow the evidence–practice gap.
Limitations
Our study has some limitations. We relied on surgeons self-reporting practice patterns rather than auditing actual practice patterns; it is possible that surgeons perceive or report practising differently than they actually do. There were a moderate absolute number of respondents; however, this is intrinsic to the study given that HPB care is centralized to high-volume, academic centres in Canada compared with other countries.7 Despite this homogeneous survey population, our study still demonstrated heterogeneous responses, contesting the impact of any possible selection bias. Finally, our study was limited by its descriptive nature and the inability to determine why there is disagreement among surgeons’ practices. Further research is needed to determine whether the variability identified is associated with ineffective knowledge translation or evidence–practice gaps.
Conclusion
We have evaluated Canadian practice patterns for PD. Our primary objective was to determine areas of agreement in perioperative technique and to identify evidence–practice gaps between what procedures are supported throughout the literature versus those that are routinely practised. Given the rapid evolution of surgical practices and the growing number of pancreatic cancer diagnoses and subsequent resections,2 these conflicts may significantly impact morbidity and mortality. We identified significant heterogeneity in perioperative techniques and the existence of numerous evidence–practice gaps, indicating opportunities to guide future effective research and knowledge translation strategies.
Footnotes
Competing interests: None declared.
Contributors: All authors designed the study and acquired and analyzed the data. D. Cyr wrote the article, which all authors reviewed and approved for publication.
References
- 1.Hariharan D, Saied A, Kocher HM. Analysis of mortality rates for pancreatic cancer across the world. HPB. 2008;10:58–62. doi: 10.1080/13651820701883148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Canadian Cancer Society’s Steering Committee on Cancer Statistics. Canadian Cancer Statistics 2014. Toronto, ON: Canadian Cancer Society; 2014. [accessed 2015 Feb. 23]. Available: www.cancer.ca/~/media/cancer.ca/CW/cancer%20information/cancer%20101/Canadian%20cancer%20statistics/Canadian-Cancer-Statistics-2014-EN.pdf. [Google Scholar]
- 3.Hidalgo M. Pancreatic cancer. N Engl J Med. 2010;362:1605–17. doi: 10.1056/NEJMra0901557. [DOI] [PubMed] [Google Scholar]
- 4.Li D, Xie K, Wolff R, et al. Pancreatic cancer. Lancet. 2004;363:1049–57. doi: 10.1016/S0140-6736(04)15841-8. [DOI] [PubMed] [Google Scholar]
- 5.He J, Page AJ, Weiss M, et al. Management of borderline and locally advanced pancreatic cancer: Where do we stand? World J Gastroenterol. 2014;20:2255–66. doi: 10.3748/wjg.v20.i9.2255. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Whipple AO, Parsons WB, Mullins CR. Treatment of carcinoma of the ampulla of vater. Ann Surg. 1935;102:763–79. doi: 10.1097/00000658-193510000-00023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Dixon E, Vollmer CM, Bathe O, et al. Training, practice, and referral patterns in hepatobiliary and pancreatic surgery: survey of general surgeons. J Gastrointest Surg. 2005;9:109–14. doi: 10.1016/j.gassur.2004.03.008. [DOI] [PubMed] [Google Scholar]
- 8.Crist DW, Sitzmann JV, Cameron JL. Improved hospital morbidity, mortality, and survival after the Whipple procedure. Ann Surg. 1987;206:358–65. doi: 10.1097/00000658-198709000-00014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Sener SF, Fremgen A, Menck HR, et al. Pancreatic cancer: a report of treatment and survival trends for 100,313 patients diagnosed from 1985–1995, using the National Cancer Database. J Am Coll Surg. 1999;189:1–7. doi: 10.1016/s1072-7515(99)00075-7. [DOI] [PubMed] [Google Scholar]
- 10.Winter JM, Cameron JL, Campbell KA, et al. 1423 pancreaticoduodenectomies for pancreatic cancer: a single-institution experience. J Gastrointest Surg. 2006;10:1199–210. doi: 10.1016/j.gassur.2006.08.018. discussion 1210–1. [DOI] [PubMed] [Google Scholar]
- 11.Sandhu L, Fox A, Nhan C, et al. Assessing the management of hepatic colorectal cancer metastases: Is treatment consistent in Ontario? HPB. 2012;14:409–13. doi: 10.1111/j.1477-2574.2012.00467.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Wei AC, Sandhu L, Devitt KS, et al. Practice patterns for the management of hepatic metastases from colorectal cancer: a mixed methods analysis. Ann Surg Oncol. 2013;20:1567–74. doi: 10.1245/s10434-012-2698-3. [DOI] [PubMed] [Google Scholar]
- 13.McGlynn EA, Asch SM, Adams J, et al. Quality of health care delivered to adults in the United States. N Engl J Med. 2003;348:2635–45. doi: 10.1056/NEJMsa022615. [DOI] [PubMed] [Google Scholar]
- 14.Westfall JM, Mold J, Fagnan L. Practice-based research — “blue highways” on the NIH Roadmap. JAMA. 2007;297:403–6. doi: 10.1001/jama.297.4.403. [DOI] [PubMed] [Google Scholar]
- 15.Grimshaw JM, Eccles MP, Lavis JN, et al. Knowledge translation of research findings. Implement Sci. 2012;7:50. doi: 10.1186/1748-5908-7-50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Dillman DA, Phelps G, Tortora R, et al. Response rate and measurement differences in mixed-mode surveys using mail, telephone, interactive voice response (IVR) and the internet. Soc Sci Res. 2009;38:1–18. [Google Scholar]
- 17.Gouma DJ, van Geenen RC, van Gulik TM, et al. Rates of complications and death after pancreaticoduodenectomy: risk factors and the impact of hospital volume. Ann Surg. 2000;232:786–95. doi: 10.1097/00000658-200012000-00007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Wellner UF, Sick O, Olschewski M, et al. Randomized controlled single-center trial comparing pancreatogastrostomy versus pancreaticojejunostomy after partial pancreatoduodenectomy. J Gastrointest Surg. 2012;16:1686–95. doi: 10.1007/s11605-012-1940-4. [DOI] [PubMed] [Google Scholar]
- 19.Wente MN, Shrikhande SV, Müller MW, et al. Pancreaticojejunostomy versus pancreaticogastrostomy: systematic review and meta-analysis. Am J Surg. 2007;193:171–83. doi: 10.1016/j.amjsurg.2006.10.010. [DOI] [PubMed] [Google Scholar]
- 20.Duffas J-P, Suc B, Msika S, et al. A controlled randomized multicenter trial of pancreatogastrostomy or pancreatojejunostomy after pancreatoduodenectomy. Am J Surg. 2005;189:720–9. doi: 10.1016/j.amjsurg.2005.03.015. [DOI] [PubMed] [Google Scholar]
- 21.Yeo CJ, Cameron JL, Maher MM, et al. A prospective randomized trial of pancreaticogastrostomy versus pancreaticojejunostomy after pancreaticoduodenectomy. Ann Surg. 1995;222:580–8. doi: 10.1097/00000658-199510000-00014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Shen Y, Jin W. Reconstruction by pancreaticogastrostomy versus pancreaticojejunostomy following pancreaticoduodenectomy: a meta-analysis of randomized controlled trials. Gastroenterol Res Pract. 2012;2012:1–7. doi: 10.1155/2012/627095. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Topal B, Fieuws S, Aerts R, et al. Pancreaticojejunostomy versus pancreaticogastrostomy reconstruction after pancreaticoduodenectomy for pancreatic or periampullary tumours: a multicentre randomised trial. Lancet Oncol. 2013;14:655–62. doi: 10.1016/S1470-2045(13)70126-8. [DOI] [PubMed] [Google Scholar]
- 24.McKay A, Mackenzie S, Sutherland FR, et al. Meta-analysis of pancreaticojejunostomy versus pancreaticogastrostomy reconstruction after pancreaticoduodenectomy. Br J Surg. 2006;93:929–36. doi: 10.1002/bjs.5407. [DOI] [PubMed] [Google Scholar]
- 25.Lembcke B, Creutzfeldt W, Schleser S, et al. Effect of the somatostatin analogue sandostatin (MS 201-995) on gastrointestinal, pancreatic and biliary function and hormone release in normal men. Digestion. 1987;36:108–24. doi: 10.1159/000199408. [DOI] [PubMed] [Google Scholar]
- 26.Koti RS, Gurusamy KS, Fusai G, et al. Meta-analysis of randomized controlled trials on the effectiveness of somatostatin analogues for pancreatic surgery: a Cochrane review. HPB. 2010;12:155–65. doi: 10.1111/j.1477-2574.2010.00157.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Martin I, Au K. Does fibrin glue sealant decrease the rate of anastomotic leak after a pancreaticoduodenectomy? Results of a prospective randomized trial. HPB. 2013;15:561–6. doi: 10.1111/hpb.12018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Lillemoe KD, Cameron JL, Kim MP, et al. Does fibrin glue sealant decrease the rate of pancreatic fistula after pancreaticoduodenectomy? Results of a prospective randomized trial. J Gastrointest Surg. 2004;8:766–72. doi: 10.1016/j.gassur.2004.06.011. [DOI] [PubMed] [Google Scholar]
- 29.Xiong JJ, Altaf K, Mukherjee R, et al. Systematic review and meta-analysis of outcomes after intraoperative pancreatic duct stent placement during pancreaticoduodenectomy. Br J Surg. 2012;99:1050–61. doi: 10.1002/bjs.8788. [DOI] [PubMed] [Google Scholar]
- 30.Sachs TE, Pratt WB, Kent TS, et al. The pancreaticojejunal anastomotic stent: Friend or foe? Surgery. 2013;153:651–62. doi: 10.1016/j.surg.2012.11.007. [DOI] [PubMed] [Google Scholar]
- 31.Van der Gaag NA, Rauws EAJ, van Eijck CHJ, et al. Preoperative biliary drainage for cancer of the head of the pancreas. N Engl J Med. 2010;362:129–37. doi: 10.1056/NEJMoa0903230. [DOI] [PubMed] [Google Scholar]
- 32.Jinkins LJ, Parmar AD, Han Y, et al. Current trends in preoperative biliary stenting in patients with pancreatic cancer. Surgery. 2013;154:179–89. doi: 10.1016/j.surg.2013.03.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Iacono C, Ruzzenente A, Campagnaro T, et al. Role of preoperative biliary drainage in jaundiced patients who are candidates for pancreatoduodenectomy or hepatic resection: highlights and drawbacks. Ann Surg. 2013;257:191–204. doi: 10.1097/SLA.0b013e31826f4b0e. [DOI] [PubMed] [Google Scholar]
- 34.Conlon KC, Labow D, Leung D, et al. Prospective randomized clinical trial of the value of intraperitoneal drainage after pancreatic resection. Ann Surg. 2001;234:487–93. doi: 10.1097/00000658-200110000-00008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Fisher WE, Hodges SE, Silberfein EJ, et al. Pancreatic resection without routine intraperitoneal drainage. HPB. 2011;13:503–10. doi: 10.1111/j.1477-2574.2011.00331.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Adham M, Chopin-Laly X, Lepilliez V, et al. Pancreatic resection: Drain or no drain? Surgery. 2013;154:1069–77. doi: 10.1016/j.surg.2013.04.017. [DOI] [PubMed] [Google Scholar]
- 37.Mehta VV, Fisher SB, Maithel SK, et al. Is it time to abandon routine operative drain use? A single institution assessment of 709 consecutive pancreaticoduodenectomies. J Am Coll Surg. 2013;216:635–42. doi: 10.1016/j.jamcollsurg.2012.12.040. [DOI] [PubMed] [Google Scholar]
- 38.Van Buren G, Bloomston M, Hughes SJ, et al. A randomized prospective multicenter trial of pancreaticoduodenectomy with and without routine intraperitoneal drainage. Ann Surg. 2014;259:605–12. doi: 10.1097/SLA.0000000000000460. [DOI] [PubMed] [Google Scholar]
- 39.Sagar PM, Kruegener G, MacFie J. Nasogastric intubation and elective abdominal surgery. Br J Surg. 1992;79:1127–31. doi: 10.1002/bjs.1800791105. [DOI] [PubMed] [Google Scholar]
- 40.Nelson R, Tse B, Edwards S. Systematic review of prophylactic nasogastric decompression after abdominal operations. Br J Surg. 2005;92:673–80. doi: 10.1002/bjs.5090. [DOI] [PubMed] [Google Scholar]
- 41.Robertson N, Gallacher PJ, Peel N, et al. Implementation of an enhanced recovery programme following pancreaticoduodenectomy. HPB. 2012;14:700–8. doi: 10.1111/j.1477-2574.2012.00521.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Kunstman JW, Klemen ND, Fonseca AL, et al. Nasogastric drainage may be unnecessary after pancreaticoduodenectomy: a comparison of routine vs selective decompression. J Am Coll Surg. 2013;217:481–8. doi: 10.1016/j.jamcollsurg.2013.04.031. [DOI] [PubMed] [Google Scholar]
- 43.Fisher WE, Hodges SE, Cruz G, et al. Routine nasogastric suction may be unnecessary after a pancreatic resection. HPB. 2011;13:792–6. doi: 10.1111/j.1477-2574.2011.00359.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Choi DX, Schoeniger LO. For patients undergoing pancreatoduodenectomy, epidural anesthesia and analgesia improves pain but increases rates of intensive care unit admissions and alterations in analgesics. Pancreas. 2010;39:492–7. doi: 10.1097/MPA.0b013e3181bdfc76. [DOI] [PubMed] [Google Scholar]
- 45.Amini A, Patanwala AE, Maegawa FB, et al. Effect of epidural analgesia on postoperative complications following pancreaticoduodenectomy. Am J Surg. 2012;204:1000–4. doi: 10.1016/j.amjsurg.2012.05.022. discussion 1004–6. [DOI] [PubMed] [Google Scholar]
- 46.Pratt WB, Steinbrook RA, Maithel SK, et al. Epidural analgesia for pancreatoduodenectomy: a critical appraisal. J Gastrointest Surg. 2008;12:1207–20. doi: 10.1007/s11605-008-0467-1. [DOI] [PubMed] [Google Scholar]
- 47.Di Sebastiano P, Festa L, De Bonis A, et al. A modified fast-track program for pancreatic surgery: a prospective single-center experience. Langenbecks Arch Surg. 2011;396:345–51. doi: 10.1007/s00423-010-0707-1. [DOI] [PubMed] [Google Scholar]
- 48.Balzano G, Zerbi A, Braga M, et al. Fast-track recovery programme after pancreaticoduodenectomy reduces delayed gastric emptying. Br J Surg. 2008;95:1387–93. doi: 10.1002/bjs.6324. [DOI] [PubMed] [Google Scholar]
- 49.Berberat PO, Ingold H, Gulbinas A, et al. Fast track-different implications in pancreatic surgery. J Gastrointest Surg. 2007;11:880–7. doi: 10.1007/s11605-007-0167-2. [DOI] [PubMed] [Google Scholar]