Abstract
Introduction
Few, if any, studies have systematically examined the relationship between substance use and teen pregnancy using population-based samples. We aim to provide a comprehensive examination of substance use among pregnant adolescents in the United States.
Method
Employing data from the National Survey on Drug Use and Health between 2002 and 2012 (n = 97,850), we examine the prevalence of past 12-month and past 30-day substance use and substance use disorders among pregnant and non-pregnant adolescents (ages 12-17). We also examine psychosocial and pregnancy-related correlates of current substance use among the subsample of pregnant adolescents (n = 810).
Results
Pregnant teens were significantly more likely to have experimented with a variety of substances and meet criteria for alcohol (AOR = 1.65, 95% CI = 1.26-2.17), cannabis (AOR = 2.29, 95% CI = 1.72-3.04), and other illicit drug use disorders (AOR = 2.84, 95% CI = 1.92-4.19). Pregnant early adolescents (ages 12-14; AOR = 4.34, 95% CI = 2.28-8.26) were significantly more likely and pregnant late adolescents (ages 15-17; AOR = 0.71, 95% CI = 0.56-0.90) significantly less likely than their non-pregnant counterparts to be current substance users.
Conclusions
Study findings point not only to a relationship between pregnancy and prior substance use, but also suggest that substance use continues for many teens during pregnancy. We found that substance use is particularly problematic among early adolescents that the prevalence of substance use attenuates dramatically as youth progress from the first to the second and third trimesters of pregnancy.
Keywords: Substance use, teen pregnancy, sexual risk behavior, early adolescence
The reduction of adolescent substance use and teen pregnancy are objectives and leading health indicators identified by Healthy People 2020 (U.S. Department of Health and Human Services, 2014). In 2010, underage drinking alone cost the United States an estimated $62 billion in medical care, work loss, and pain and suffering (Pacific Institute, 2011), and teen pregnancy and childbirth are estimated to have added an additional $9 billion in costs to U.S. taxpayers in 2011 (Center for Disease Control and Prevention, 2014). Additionally, both adolescent substance use and pregnancy have been found to place youth at risk for a host of adverse academic, socioeconomic, interpersonal, and health outcomes during adolescence and subsequent developmental stages (Boden, Fergusson, & Horwood, 2008; Grant et al., 2006; Klein, 2005; Paranjothy, Broughton, Adappa, & Fone, 2009; Tapert, Aarons, Sedlar, & Brown, 2001). Simply, substance use and teen pregnancy represent important challenges in terms of the health of the nation and the healthy development of adolescents in the United States.
Prior research on adolescent substance use and sexual risk behavior suggests that substance use and teen pregnancy are intertwined. Such research has highlighted the overlapping etiology of substance use with involvement in sexual risk behaviors, such as unprotected sexual intercourse, that place youth at risk for early pregnancy (Hawkins, Catalano, & Arthur, 2002; Resnick et al., 1997). That is, various biological (e.g., genetic, temperamental), intrapersonal (e.g., attitudes, social norms), and ecodevelopmental (e.g., parental support and control, school engagement) factors have been found to conjointly impact the likelihood of substance use and pregnancy-related outcomes (DeLisi & Vaughn, 2014; Prado et al., 2009; Shneyderman & Schwartz, 2012; Vaughn, DeLisi, & Matto, 2013). Epidemiological studies have also documented the comorbidity of health-risk behaviors, including substance use and sexual behaviors that place youth at risk for early pregnancy (Ramrakha, Caspi, Dickson, Moffitt, & Paul, 2000; Salas-Wright, Olate, & Vaughn, 2014a, 2014b; Teplin et al., 2005; Vaughn, Salas-Wright, DeLisi, & Maynard, 2014).
Beyond overlapping etiology and comorbidity, evidence also points to the instrumental role of adolescent substance use in sexual behaviors that place youth in jeopardy for early pregnancy (Odgers et al., 2008; Stueve & O'Donnell, 2005). For instance, research suggests that many adolescents use licit and illicit substances prior to intercourse (Fortenberry, 1995) and to facilitate sexual encounters (Bellis et al., 2008). This is noteworthy as intercourse under the influence of alcohol or drugs has been found to be associated with decreased condom use, particularly when the intercourse is unplanned (Poulin, & Graham, 2001). Such findings converge with experimental studies demonstrating the disinhibiting effects and impaired cognitive functioning of alcohol and other substances (Cooper & Orcutt, 1997; Fromme, D'Amico, & Katz, 1999; Poulos, Parker, & Le, 1998), all of which are associated with increased risk for involvement in sexual risk behavior (Dausey & Desai, 2003; Logan, Cole, & Leukefeld, 2002). Evidence also suggests that substance use can contribute to the increased likelihood of sexual risk behavior by means of exposing youth to peer groups endorsing more lenient sexual norms (Huock et al., 2006). It has also been noted that exposure to high-risk peer groups may weaken the relationship of adolescents with prosocial family and peer networks that can serve to protect against involvement in sexual risk behavior (Fergus & Zimmerman, 2005).
While a rather extensive body of literature has examined the relationship between adolescent substance use and sexual risk behaviors that place youth at risk for early or unplanned pregnancy (Cook & Clark, 2005; Fortenberry, 1995; Kotchick, Shaffer, Miller, & Forehand, 2001; Leigh, 2002), surprisingly few studies have systematically examined the links between substance use and teen pregnancy. A recent review by Chapman and Wu (2013) identified only a handful of studies focused on adolescent alcohol or drug use prior to and during pregnancy (Amaro, Zuckerman, & Cabral, 1989; Barnet, Duggan, Wilson, & Joffe, 1995; De Genna, Cornelius, & Donovan, 2009; Gilchrist, Hussey, Gillmore, Lohr, & Morrison, 1996; Kaiser & Hays, 2005; Spears, Stein, & Koniak-Griffin, 2010; Morrison, Spencer, & Gilmore, 1998). Results from these investigations suggest that pregnant teens tend to report elevated levels of substance use prior to pregnancy, but report a dramatic decrease in use during pregnancy. This suggests that—while substance use may place youth at risk for early or unintended pregnancy— many youth refrain from use during pregnancy, perhaps due to concerns about the impact of substance use on neonatal health and development (Huizink & Mulder, 2006; Smith et al., 2008).
Despite the contributions of previous research, however, several important shortcomings should be noted. First, the aforementioned studies examining substance use prior to and during pregnancy rely exclusively on relatively small and geographically circumscribed samples comprised of pregnant or postpartum youth in predominantly urban areas. These sampling limitations raise important questions about the generalizability of the findings regarding the links between substance use and teen pregnancy. Second, prior studies have tended to report the use of only a limited number of substances (e.g., alcohol, cannabis) and have typically failed to examine substance use disorders. A more nuanced examination of a far-reaching array of substances as well as substance use disorders can shed light on the interrelatedness of substance use and teen pregnancy. Finally, although evidence suggests that both substance use and teen pregnancy vary substantially across the developmental spectrum of adolescence (Costello, Mustillo, Erkanli, Keeler, & Angold, 2003; Kline, 2005), previous research has tended to overlook the developmental complexity in terms of the relationship between substance use and teen pregnancy.
The Present Study
The present study aims to provide a comprehensive examination of substance use and teen pregnancy by employing data from a large, population-based study (National Survey on Drug Use and Health [NSDUH]) of adolescent females in the United States between 2002 and 2012. Specifically, in order to assess the relationship between prior substance use and teen pregnancy, we examine the prevalence of the use of a wide array of substances and substance use disorders among pregnant and non-pregnant youth over the previous 12 months. Additionally, in order to examine the relationship between current substance use and teen pregnancy, we examine the prevalence of the use of a variety of substances among pregnant and non-pregnant youth over the previous 30 days and across each trimester among the pregnant teens. Further, we examine the intrapersonal, ecodevelopmental, and pregnancy-related correlates of current substance use among the subsample of pregnant adolescent females.
Method
Sample and Procedures
Study findings are based on data from the NSDUH between 2002 and 2012. The NSDUH provides population estimates of substance use and health-related behaviors in the U.S. general population. It utilizes multistage area probability sampling methods to select a representative sample of the U.S. civilian, non-institutionalized population aged 12 years or older for participation in the study. A more detailed description of the NSDUH design and procedures is available elsewhere (SAMHSA, 2012). The current study restricted analyses to female respondents between the ages of 12 and 17 (n = 97,850).
Measures
Teen Pregnancy
Respondents were classified as pregnant (0 = no, 1 = yes) on the basis of the following question: “Are you currently pregnant?” Respondents who reported not knowing their pregnancy status (< 0.50% of respondents) were coded as missing. Respondents endorsing pregnancy were also asked if they were in the first, second, or third trimesters of pregnancy.
Substance Use Disorders
We examined past 30-day and past 12-month measures of substance use as well as measures of alcohol, cannabis, and other illicit drug use disorder based on the Diagnostic and Statistical Manual of Mental Disorders, 4th edition (DSM-IV) criteria (American Psychiatric Association, 2000).
Parental Involvement
We examined two measures of parental involvement over the previous 12 months. Positive reinforcement was measured by asking respondents “How often did your parents tell you they were proud of you for something you had done?” Parental control was measured by asking respondents “How often did your parents limit the amount of time you went out with friends on school nights?” For both items, youth reporting consistent parental reinforcement/control (i.e., “always”) were coded as 1 and all others (i.e., “sometimes”, “seldom”, “never”) were coded as 0.
School Engagement
Two measures of school engagement were examined. First, youth were asked how they “Felt overall about going to school during the past 12 months?” Youth reporting a clear positive assessment of school attendance (i.e., “liked a lot”) were coded as 1 and all other youth (i.e. “kind of liked”, “didn't like”, and “hated”) were coded as 0. Youth were also asked report, “What were your grades for the last semester or grading period you completed?” Consistent with research identifying school failure as a risk factor for substance use (Hawkins, Catalano, & Miller, 1992) and externalizing behavior (Farrington, 1989), youth were coded as either “passing” or “failing”.
Religiosity
Two measures of religiosity were examined: religious service attendance and the influence of religious beliefs. Religious service attendance was measured by asking, “During the past 12 months, how many times did you attend religious services?” The influence of religious beliefs was measured by asking respondents the degree to which they agreed with the following: “Your religious beliefs influence how you make decisions in your life.”
Sociodemographic Factors
Demographic variables included: age, race/ethnicity, total annual household income, and the absence of mother/father from the household.
Statistical Analyses
Statistical analyses were conducted in several steps. First, logistic regression analyses were systematically executed to compare pregnant and non-pregnant teens in terms of sociodemographic and substance use characteristics. We also examined the prevalence of substance use and substance use disorders while stratifying by developmental subgroups. Finally, logistic regression analyses were conducted with the pregnant teens (n = 810) to examine the correlates of substance use during pregnancy. Weighted prevalence estimates and standard errors were computed using Stata 13.1 SE software (StataCorp, 2013).
Results
What are the Sociodemographic Characteristics of Pregnant Teens in the United States?
As displayed in Table 1, logistic regression analyses examining the sociodemographic characteristics of respondents revealed that, compared to their non-pregnant counterparts, pregnant teens are more likely to be between the ages of 15 and 17 (AOR = 7.04, 95% CI = 5.23-5.46). Pregnant teens are also more likely to be African-American (1.40, 95% CI = 1.11-1.77) or Hispanic (AOR = 1.79, 95% CI = 1.41-2.27) and to reside in a household earning less than less than $20,000 (AOR = 4.00, 95% CI = 1.75-3.33), between $20,000-$49,999 (AOR = 2.41, 95% CI = 1.75-3.33), or between $50,000-$74,999 per year (AOR = 1.72, 95% CI = 1.17-2.54). Pregnant teens are also significantly more likely to report that their mother (AOR = 1.85, 95% CI = 1.45-2.35) and/or father (AOR = 1.56, 95% CI = 1.26-1.93) is absent from the household.
Table 1.
Sociodemographic characteristics of pregnant teenagers in the United States
| Are you currently pregnant? | Unadjusted | Adjusted | ||||||
|---|---|---|---|---|---|---|---|---|
| No (n = 96,520; 99.24%) | Yes (n = 810; 0.76%) | |||||||
| % | 95% CI | % | 95% CI | OR | (95% CI) | OR | (95% CI) | |
| Sociodemographic Factors | ||||||||
| Age | ||||||||
| 12-14 years | 49.52 | (49.1-49.9) | 12.11 | (9.3-15.6) | 1.00 | 1.00 | ||
| 15-17 years | 50.48 | (50.1-50.9) | 87.89 | (84.4-90.7) | 7.12 | (5.30-9.56) | 7.04 | (5.23-9.46) |
| Race/Ethnicity | ||||||||
| Non-Hispanic white | 59.45 | (59.0-59.9) | 40.23 | (35.9-44.7) | 1.00 | 1.00 | ||
| African-American | 15.00 | (14.7-15.3) | 24.64 | (21.1-28.6) | 2.43 | (1.94-3.03) | 1.40 | (1.11-1.77) |
| Hispanic | 18.34 | (18.0-18.7) | 30.49 | (26.2-35.2) | 2.46 | (1.95-3.09) | 1.79 | (1.41-2.27) |
| Other | 7.21 | (7.0-7.4) | 4.65 | (3.1-6.9) | 0.95 | (0.61-1.47) | 0.81 | (0.52-1.26) |
| Household Income | ||||||||
| < $20,000 | 17.53 | (17.2-17.9) | 40.58 | (36.2-45.1) | 6.81 | (4.99-9.30) | 4.00 | (1.75-3.33) |
| $20,000-$49,999 | 32.13 | (31.7-32.5) | 36.57 | (32.3-41.0) | 3.35 | (2.45-4.58) | 2.41 | (1.75-3.33) |
| $50,000-$74,999 | 18.33 | (18.0-18.7) | 11.98 | (9.3-15.3) | 1.92 | (1.31-2.83) | 1.72 | (1.17-2.54) |
| > $75,000 | 32.00 | (31.6-32.4) | 10.87 | (8.3-14.0) | 1.00 | 1.00 | ||
| Mother Absent from Household | ||||||||
| No | 92.01 | (91.8-92.2) | 79.59 | (75.6-83.1) | 1.00 | 1.00 | ||
| Yes | 7.99 | (7.8-8.2) | 20.41 | (16.9-24.4) | 2.95 | (2.34-3.72) | 1.85 | (1.45-2.35) |
| Father Absent from Household | ||||||||
| No | 73.13 | (72.8-73.5) | 48.21 | (43.6-52.8) | 1.00 | 1.00 | ||
| Yes | 26.87 | (26.5-27.2) | 51.79 | (47.2-56.3) | 2.92 | (2.43-3.52) | 1.56 | (1.26-1.93) |
Note: Adjusted odds ratios adjusted for adjusted for age, race/ethnicity, household income, and mother/father in household. Odds ratios and confidence intervals in bold are statistically significant.
Are pregnant teens more likely than non-pregnant teens to have used substances in the previous 12 months?
Table 2 examines the prevalence of substance use and substance use disorders among pregnant and non-pregnant teens over the previous 12 months. Controlling for age, race/ethnicity, household income, and the absence of mother/father in household, pregnant teens were significantly more likely to report using nearly all substances examined over the previous 12 months. The only nonsignificant finding was with respect to the use of inhalants. Particularly large adjusted odds ratios were observed for cocaine/crack (AOR = 2.66, 95% CI = 1.74-4.06), methamphetamine (AOR = 2.70, 95% CI = 1.48-4.91), and opiates (AOR = 2.75, 95% CI = 1.54-4.91). Controlling for the same list of sociodemographic confounds, the prevalence of alcohol (AOR = 1.65, 95% CI = 1.26-2.17), cannabis (AOR = 2.29, 95% CI = 1.72-3.04), and other illicit drug use disorders (AOR = 2.84, 95% CI = 1.92-4.19) was also significantly higher among pregnant teens.
Table 2.
Substance use characteristics of pregnant teenagers in the United States
| Are you currently pregnant? | Unadjusted | Adjusted | ||||||
|---|---|---|---|---|---|---|---|---|
| No (n = 96,520; 99.24%) | Yes (n = 810; 0.76%) | |||||||
| % | 95% CI | % | 95% CI | OR | (95% CI) | OR | (95% CI) | |
| Substance Use (Last 12 Months) | ||||||||
| Alcohol | ||||||||
| No | 67.97 | (67.4-68.2) | 46.84 | (42.3-51.4) | 1.00 | 1.00 | ||
| Yes | 32.21 | (31.8-32.6) | 53.16 | 48.6-57.7) | 2.39 | (1.99-2.87) | 1.44 | (1.18-1.76) |
| Cannabis | ||||||||
| No | 87.02 | (86.7-87.3) | 68.40 | (64.2-72.3) | 1.00 | 1.00 | ||
| Yes | 12.98 | (12.7-13.3) | 31.60 | (27.7-35.8) | 3.10 | (2.56-3.74) | 1.79 | (1.45-2.20) |
| Cocaine/Crack | ||||||||
| No | 98.64 | (98.5-98.7) | 94.06 | (91.5-95.9) | 1.00 | 1.00 | ||
| Yes | 1.36 | (1.3-1.5) | 5.94 | (4.1-8.5) | 4.57 | (3.09-6.75) | 2.66 | (1.74-4.06) |
| Ecstasy | ||||||||
| No | 98.42 | (98.3-98.5) | 95.43 | (93.2-96.9) | 1.00 | 1.00 | ||
| Yes | 1.58 | (1.5-1.7) | 4.57 | (3.0-6.8) | 2.99 | (1.95-4.59) | 1.76 | (1.12-2.76) |
| Hallucinogens | ||||||||
| No | 97.27 | (97.1-97.4) | 93.17 | (90.7-95.0) | 1.00 | 1.00 | ||
| Yes | 2.73 | (2.6-2.9) | 6.83 | (4.9-9.3) | 2.62 | (1.86-3.68) | 1.72 | (1.20-2.47) |
| Inhalants | ||||||||
| No | 95.85 | (95.7-96.0) | 96.22 | (94.3-97.5) | 1.00 | 1.00 | ||
| Yes | 4.15 | (4.0-4.3) | 3.78 | (2.5-5.7 | 0.91 | (0.59-1.39 | 1.04 | (0.67-1.61) |
| Methamphetamine | ||||||||
| No | 99.41 | (99.3-99.5) | 97.77 | (96.1-98.7) | 1.00 | 1.00 | ||
| Yes | 0.59 | (0.52-0.65) | 2.23 | (1.3-3.8) | 3.87 | (2.18-6.87) | 2.70 | (1.48-4.91) |
| Stimulants | ||||||||
| No | 97.99 | (97.9-98.1) | 95.31 | (93.2-96.8) | 1.00 | 1.00 | ||
| Yes | 2.01 | (1.9-2.1) | 4.69 | (3.2-6.8) | 2.40 | (1.60-3.60) | 1.83 | (1.19-2.80) |
| Tranquilizers | ||||||||
| No | 97.71 | (97.6-97.8) | 93.77 | (91.3-95.6) | 1.00 | 1.00 | ||
| Yes | 2.29 | (2.2-2.4) | 6.22 | (4.4-8.7) | 2.83 | (1.96-4.10) | 1.82 | (1.23-2.70) |
| Opiates | ||||||||
| No | 99.08 | (98.9-99.2) | 96.47 | (94.1-97.9) | 1.00 | 1.00 | ||
| Yes | 0.92 | (0.84-1.01) | 3.53 | (2.1-5.9) | 3.92 | (2.26-6.80) | 2.75 | (1.54-4.91) |
| Substance Use Disorders (Abuse/Dependence) | ||||||||
| Alcohol | ||||||||
| No | 94.69 | (94.5-94.9) | 88.08 | (85.1-90.5) | 1.00 | 1.00 | ||
| Yes | 5.31 | (5.1-5.5) | 11.92 | (9.5-14.9) | 2.41 | (1.86-3.12) | 1.65 | (1.26-2.17) |
| Cannabis | ||||||||
| No | 96.92 | (96.8-97.1) | 89.27 | (86.5-91.5) | 1.00 | 1.00 | ||
| Yes | 3.08 | (2.9-3.2) | 10.73 | (8.5-13.5) | 3.78 | (2.90-4.93) | 2.29 | (1.72-3.04) |
| Other Illicit Drugs | ||||||||
| No | 97.77 | (97.6-97.9) | 92.27 | (89.3-94.5) | 1.00 | 1.00 | ||
| Yes | 2.23 | (2.1-2.4) | 7.72 | (5.5-10.7) | 3.66 | (2.54-5.29) | 2.84 | (1.92-4.19) |
Note: Adjusted odds ratios adjusted for adjusted for age, race/ethnicity, household income, and mother/father in household. Odds ratios and confidence intervals in bold are statistically significant
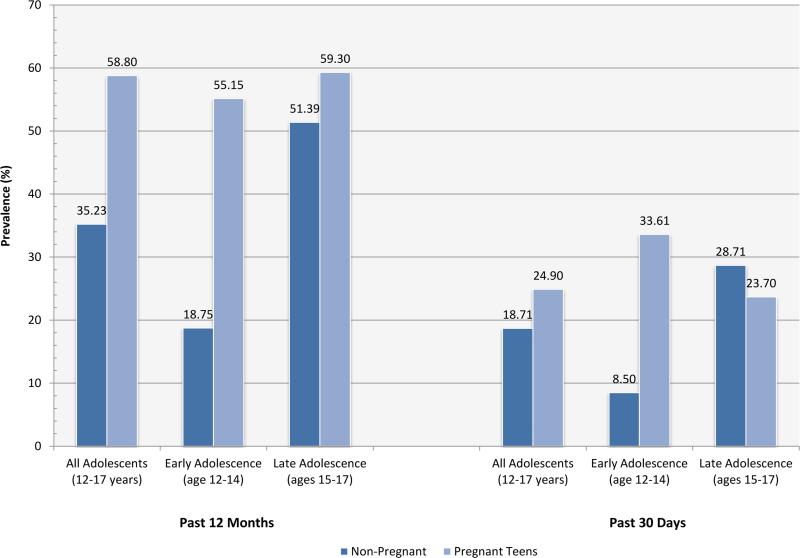
We also examined the stability of the relationship between teen pregnancy and substance use /SUDs across the developmental periods of early (i.e. 12-14 years) and late adolescence (i.e. 15-17 years). Figure 1 displays the prevalence of the use of any substance over the previous 12 months among all adolescents as well as among the early adolescent and late adolescent subsamples. Nearly 3 in 5 (58.80%) pregnant teens in the United States reported having used one or more substances in the previous 12 months. This rate, which is nearly 2 times greater than that of non-pregnant teens in the United States (35.23%), is significantly greater than that of non-pregnant teens even when controlling for sociodemographic and parental confounds (AOR = 1.57, 95% CI = 1.28-1.93). Notably, this relationship is significant across the developmental stage of adolescence, but effects are significantly larger during early adolescence (ages 12-14; AOR = 4.55, 95% CI = 2.42-8.58) as compared to the late adolescent stage (ages 15-17; AOR = 1.36, 95% CI = 1.11-1.67).
Figure 1.
Prevalence of last 12-months and last 30-days substance use among pregnant and non-pregnant teens by developmental subgroups.
Supplementary analyses were conducted to examine this relationship in terms of particular types of substances. Compared to non-pregnant early adolescents, pregnant early adolescents were significantly more likely to report having used alcohol (AOR = 4.24, 95% CI = 2.42-8.01), cannabis (AOR = 7.18, 95% CI = 3.46-14.91), or other illicit drugs (AOR = 4.96, 95% CI = 2.77-8.86) in the previous 12 months. Among the late adolescent subsample, pregnant teens were also significantly more likely to have used alcohol (AOR = 1.26, 95% CI = 1.03-1.54), cannabis (AOR = 1.57, 95% CI = 1.27-1.93), and other illicit drugs (AOR = 1.33, 95% CI = 1.01-1.75) in the previous 12 months. Notably, as evidenced by non-overlapping 95% confidence intervals, the magnitude of the relationship between teen pregnancy and substance use was significantly greater among early than late adolescents.
Are pregnant teens more likely than their non-pregnant counterparts to be current (i.e. past 30 days) substance users?
As illustrated in Figure 1, among adolescents in general, the 24.90% of pregnant teens reported consuming one or more substances over the previous month compared to 18.71% of non-pregnant teens. Notably, however, when controlling for sociodemographic and parental factors, pregnant teens were significantly less likely than their non-pregnant counterparts to have used one or more substances over the previous 30 days (AOR = 0.78, 95% CI = 0.62-0.99). We also examined the prevalence of substance use among pregnant and non-pregnant teens among the early and late adolescent subsamples. This revealed a distinct pattern in which pregnant early adolescents (AOR = 4.34, 95% CI = 2.28-8.26) were significantly more likely and pregnant late adolescents (AOR = 0.71, 95% CI = 0.56-0.90) were significantly less likely than their non-pregnant counterparts to be current substance users.
What substances are being used by teens during pregnancy?
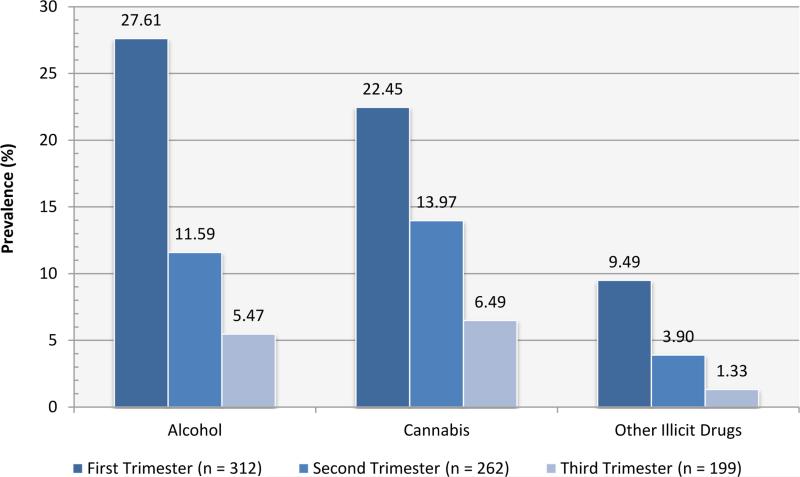
We found that the most commonly used substance by pregnant teens is alcohol (15.85%) followed closely by cannabis (14.55%) and finally other illicit drugs (5.30%). Notably, however, the prevalence of substance use does not appear to remain consistent throughout pregnancy. As illustrated in Figure 2, we see a marked reduction in substance use among pregnant teens from the first to second trimester for alcohol, cannabis, and other illicit drugs. The proportion of pregnant teens using alcohol and other illicit drugs during the first trimester (alcohol = 27.61%, other illicit drugs = 9.49) drops by more than half by the second trimester (alcohol = 11.59%, other illicit drugs = 3.90). Notably, a slightly smaller proportional decrease was observed for cannabis between the first (22.45%) and second (13.97%) trimesters. The prevalence of use of all of the aforementioned substances drops again by roughly half between the second and third trimesters.
Figure 2.
Prevalence of current substance use (past month) among pregnant teens by pregnancy trimester
What Are the Correlates of Substance Use during Pregnancy?
Table 3 examines the correlates of substance use among the subsample of pregnant teens in the United States. Pregnant teens reporting current substance use are less likely to report consistent positive reinforcement from their parents (AOR = 0.50, 95% CI = 0.32-0.77) and consistent parental control (AOR = 0.57, 95% CI = 0.35-0.94). Similarly, pregnant teens reporting substance use were significantly less likely to report clear positive feelings about school (AOR = 0.47, 95% CI = 0.26-0.87) and academic success (AOR = 0.49, 95% CI = 0.28-0.85). Pregnant teens reporting current substance use were also significantly less likely to be in either their second (AOR = 0.48, 95% CI = 0.30-0.80) or third (AOR = 0.18, 95% CI = 0.09-0.35) trimesters of pregnancy.
Table 3.
Correlates of Current Substance Use among Pregnant Teens in the United States
|
Any Substance
Use (Past Month) |
||||||
|---|---|---|---|---|---|---|
| No (n = 602, 75.10%) | Yes (n = 208, 24.90%) | Adjusted | ||||
| % | 95% CI | % | 95% CI | AOR | (95% CI) | |
| Parental Involvement | ||||||
| Positive Reinforcement | ||||||
| Sometimes/seldom/never | 51.52 | (46.1-56.9) | 68.98 | (60.2-76.5) | 1.00 | |
| Always | 48.48 | (43.1-53.9) | 31.02 | (23.5-39.7) | 0.50 | (0.32-0.77) |
| Parental Control | ||||||
| Sometimes/seldom/never | 61.93 | (56.0-67.5) | 74.04 | (65.3-81.2) | 1.00 | |
| Always | 38.07 | (32.4-44.0) | 25.96 | (18.8-34.7) | 0.57 | (0.35-0.94) |
| School Engagement | ||||||
| How Felt About Going to School | ||||||
| Kind of liked/didn't like/hated | 71.06 | (65.2-76.3) | 84.72 | (76.9-90.2) | 1.00 | |
| Liked a lot | 28.94 | (23.7-34.8) | 15.28 | (9.8-23.0) | 0.47 | (0.26-0.87) |
| Grades | ||||||
| Failing (i.e. D or lower) | 12.02 | (8.7-16.4) | 20.95 | (14.7-28.9) | 1.00 | |
| Passing | 87.98 | (83.6-91.3) | 79.05 | (71.1-85.3) | 0.49 | (0.28-0.85) |
| Religiosity | ||||||
| Religious Service Attendance | ||||||
| No/limited attendance | 82. 39 | (77.9-86.1) | 83.02 | (75.5-88.6) | 1.00 | |
| Bimonthly Attendance or more | 17.61 | (13.9-20.1) | 16.98 | (11.4-24.5) | 0.84 | (0.48-1.49) |
| Religious Beliefs Influence Decision-Making | ||||||
| Strongly disagree/disagree/agree | 77. 88 | (73.2-81.9) | 81.53 | (74.2-87.1) | 1.00 | |
| Strongly agree | 22.12 | (18.0-26.8) | 18.47 | (12.9-25.8) | 0.75 | (0.45-1.26) |
| Pregnancy-Related Factors | ||||||
| Trimester | ||||||
| First | 31. 56 | (26.9-36.6) | 59.79 | (50.6-68.3) | 1.00 | |
| Second | 36.03 | (30.9-41.4) | 30.43 | (22.6-39.5) | 0.48 | (0.30-0.80) |
| Third | 31.41 | (27.5-37.8) | 9.78 | (5.6-16.5) | 0.18 | (0.09-0.35) |
Note: Adjusted odds ratios adjusted for adjusted for age, race/ethnicity, household income, and mother/father in household. Odds ratios and confidence intervals in bold are statistically significant.
Discussion
To our knowledge, this is the largest study to date on the relationship between substance use and teen pregnancy. Results suggest that pregnant adolescent females are significantly more likely to have experimented with alcohol, cannabis, and other illicit drugs and are far more likely to meet criteria for substance use disorders compared to their non-pregnant counterparts. This finding extends previous research highlighting the shared etiology (Hawkins et al., 2002; Resnick et al., 1997) and comorbidity of health risk behaviors among youth (Salas-Wright et al., 2014a, 2014b; Vaughn et al., 2014) as well as evidence that substance use is related to the increased likelihood of risky sexual behaviors and outcomes, including unprotected intercourse and early pregnancy (Klein, 2005; Thompson, Kao, & Thomas, 2005; Odgers et al., 2008). This relationship was observed across adolescence, but the link between substance use and teen pregnancy was significantly greater among early adolescents than among late adolescents.
Beyond examining the links between teen pregnancy and prior substance use (i.e., last 12 months), we also examined the prevalence of current substance use (i.e., last 30 days) among pregnant teens vis-à-vis their non-pregnant counterparts. We found that while fewer than one in 10 (9%) non-pregnant early adolescents were current substance users, more than one third (34%) of all pregnant early adolescents reported having used one or more substances over the previous 30 days. Notably, our results also indicate that the prevalence of substance use tends to attenuate substantially as pregnant teens progress from the first to the second and third trimesters of pregnancy. Given the links between substance use during pregnancy and neonatal health and behavioral outcomes (Huizink & Mulder, 2006; Smith et al., 2008), these findings are disconcerting and point to the importance multicomponent interventions designed to target substance use among pregnant teens (Brandon, 2014; Ickovics, 2008; Toumbourou et al., 2007).
We also examined several psychosocial correlates. We found that those reporting consistent parental reinforcement and control were less likely to be current substance users as compared to those reporting lower levels of parental consistency. Very similar effects were identified for pregnant teens reporting successful academic engagement. These findings converge with previous research pointing to the importance of parental factors in the etiology of adolescent substance use (Cleveland et al., 2012; Salas-Wright, Hernandez, Maynard, Saltzman, & Vaughn, 2014) and highlight the importance of parental support and academic engagement among pregnant teens and teen mothers (Doğan-Ates, & Carrión-Basham, 2007; Kalil & Ziol-Guest, 2008; Logsdon, Birkimer, Simpson, & Looney, 2005; Meade & Ickovics, 2005). Despite recent evidence of the protective effect of religiosity for substance use (Spears, Stein, & Koniak-Griffin, 2010; Salas-Wright et al., 2012; Salas-Wright, Vaughn, Maynard, Clark, & Snyder, 2014; Yonker, Schnabelrauch, & DeHaan, 2012), neither religious service attendance nor religious beliefs were significantly linked with the decreased likelihood of substance use among pregnant teens.
Study Limitations
Our study findings should be interpreted in the context of several limitations. First, although data from 2002 to 2012 were pooled to increase the analytic sample size, the NSDUH is fundamentally a cross-sectional study and, as such, a longitudinal assessment of the causal relationship between pregnancy and substance use is not possible (Rashad & Kaestner, 2004). Second, respondents may have failed to report that they were pregnant, been unaware of their pregnancy status, or reported being pregnant when they were not. However, the use of self-report measures of pregnancy is considered to be a valid and reliable approach in epidemiological research (Overbeek et al., 2013). The self-report nature of substance use also allows for the possible under-reporting of use among pregnant teens (Bessa, Mitsuhiro, Chalem, Barros, & Guinsburg, 2010). Third, while we examined a number of parental, school, and pregnancy-related factors, the NSDUH does not include important biological (e.g., pubertal timing) and contextual (e.g., neighborhood and community) factors that might provide important information as to the use of licit and illicit substances among pregnant and non-pregnant teens (Deardorff, Gonzales, Christopher, Roosa, & Millsap, 2005). Finally, it should be noted that the use of past 12-month and past-30 day measures of substance use does not provide a precise categorization of use prior to and during pregnancy. As such, it is possible that misclassification could take place if, for example, an adolescent were three weeks pregnant and used alcohol prior to conception but still within the previous 30-day period. Given this possibility, we exercise caution in our interpretation of the relevance of study findings to our understanding of substance use prior to or during pregnancy.
Conclusions
In sum, present study findings indicate that, compared to non-pregnant teens, females who become pregnant during adolescence are far more likely to have experimented with a variety of licit and illicit substances over the previous 12-months, and to meet criteria for substance use disorders. Our results suggest that, while this relationship holds for both early and late adolescents, the link between substance use and teen pregnancy is far stronger among younger teens. Additionally, our results point not only to a relationship between pregnancy and prior substance use, but also suggest that substance use continues for many teens during pregnancy. Specifically, we found that substance use appears to be particularly problematic among early adolescents and that the prevalence of substance use attenuates dramatically as youth progress from the first to the second and third trimesters of pregnancy. Evidence also suggests that pregnant teens who benefit from consistent parental support and control and those who are successfully engaged academically are significantly less likely to use substances.
Acknowledgments
This research was supported in part by grant numbers R25 DA026401 (PI: Valdez) and R25 DA030310 (PI: Anthony) from the National Institute on Drug Abuse at the National Institutes of Health.
Dr. Salas-Wright designed the study, conducted the statistical analysis, and lead the writing of the manuscript. Dr. Vaughn provided statistical consultation and contributed to the introduction and discussion sections. Jenny Ugalde and Jelena Todic helped with the literature review and provided feedback in the introduction and discussion sections. All authors contributed to and have approved the final manuscript.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Declaration of Interest:
The authors declare that there are no conflicts of interest associated with this manuscript
References
- American Psychiatric Association . Diagnostic and Statistical Manual of Mental Disorders DSM-IV-TR Fourth Edition (Text Revision) American Psychiatric Association; Washington, D.C.: 2000. [Google Scholar]
- Barnet B, Duggan AK, Wilson MD, Joffe A. Association between postpartum substance use and depressive symptoms, stress, and social support in adolescent mothers. Pediatrics. 1995;96(4):659–666. [PubMed] [Google Scholar]
- Bert SC. The influence of religiosity and spirituality on adolescent mothers and their teenage children. Journal of Youth and Adolescence. 2011;40(1):72–84. doi: 10.1007/s10964-010-9506-9. [DOI] [PubMed] [Google Scholar]
- Bessa MA, Mitsuhiro SS, Chalem E, Barros MM, Guinsburg R, Laranjeira R. Underreporting of use of cocaine and marijuana during the third trimester of gestation among pregnant adolescents. Addictive Behaviors. 2010;35(3):266–269. doi: 10.1016/j.addbeh.2009.10.007. [DOI] [PubMed] [Google Scholar]
- Boden JM, Fergusson DM, John Horwood L. Early motherhood and subsequent life outcomes. Journal of Child Psychology and Psychiatry. 2008;49(2):151–160. doi: 10.1111/j.1469-7610.2007.01830.x. [DOI] [PubMed] [Google Scholar]
- Brandon AR. Psychosocial Interventions for Substance Use During Pregnancy. The Journal of Perinatal & Neonatal Nursing. 2014;28(3):169–177. doi: 10.1097/JPN.0000000000000041. [DOI] [PubMed] [Google Scholar]
- Cleveland MJ, Feinberg ME, Osgood DW, Moody J. Do peers' parents matter? A new link between positive parenting and adolescent substance use. Journal of Studies on Alcohol and Drugs. 2012;73(3):423. doi: 10.15288/jsad.2012.73.423. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cook RL, Clark DB. Is there an association between alcohol consumption and sexually transmitted diseases? A systematic review. Sexually Transmitted Diseases. 2005;32(3):156–164. doi: 10.1097/01.olq.0000151418.03899.97. [DOI] [PubMed] [Google Scholar]
- Cooper ML, Orcutt HK. Drinking and sexual experience on first dates among adolescents. Journal of Abnormal Psychology. 1997;106:191–202. doi: 10.1037//0021-843x.106.2.191. [DOI] [PubMed] [Google Scholar]
- Costello EJ, Mustillo S, Erkanli A, Keeler G, Angold A. Prevalence and development of psychiatric disorders in childhood and adolescence. Archives of General Psychiatry. 2003;60(8):837–844. doi: 10.1001/archpsyc.60.8.837. [DOI] [PubMed] [Google Scholar]
- Dausey DJ, Desai RA. Psychiatric comorbidity and the prevalence of HIV infection in a sample of patients in treatment for substance abuse. The Journal of Nervous and Mental Disease. 2003;191(1):10–17. doi: 10.1097/00005053-200301000-00003. [DOI] [PubMed] [Google Scholar]
- De Genna NM, Cornelius MD, Donovan JE. Risk factors for young adult substance use among women who were teenage mothers. Addictive Behaviors. 2009;34(5):463–470. doi: 10.1016/j.addbeh.2008.12.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Deardorff J, Gonzales NA, Christopher FS, Roosa MW, Millsap RE. Early puberty and adolescent pregnancy: the influence of alcohol use. Pediatrics. 2005;116(6):1451–1456. doi: 10.1542/peds.2005-0542. [DOI] [PubMed] [Google Scholar]
- DeLisi M, Vaughn MG. Foundation for a temperament-based theory of antisocial behavior and criminal justice system involvement. Journal of Criminal Justice. 2014;42(1):10–25. [Google Scholar]
- Doğan-Ateş A, Carrión-Basham CY. Teenage pregnancy among Latinas: Examining risk and protective factors. Hispanic Journal of Behavioral Sciences. 2007;29(4):554–569. [Google Scholar]
- Farrington DP. Early predictors of adolescent aggression and adult violence. Violence and Victims. 1989;4(2):79–100. [PubMed] [Google Scholar]
- Fergus S, Zimmerman MA. Adolescent resilience: A framework for understanding healthy development in the face of risk. Annual Review of Public Health. 2005;26:399–419. doi: 10.1146/annurev.publhealth.26.021304.144357. [DOI] [PubMed] [Google Scholar]
- Fortenberry JD. Adolescent substance use and sexually transmitted diseases risk: a review. Journal of Adolescent Health. 1995;16(4):304–308. doi: 10.1016/1054-139X(94)00062-J. [DOI] [PubMed] [Google Scholar]
- Fromme K, D'Amico EJ, Katz EC. Intoxicated sexual risk taking: An expectancy or cognitive impairment explanation? Journal of Studies on Alcohol. 1999;60:54–63. doi: 10.15288/jsa.1999.60.54. [DOI] [PubMed] [Google Scholar]
- Gilchrist LD, Hussey JM, Gillmore MR, Lohr MJ, Morrison DM. Drug use among adolescent mothers: prepregnancy to 18 months postpartum. Journal of Adolescent Health. 1996;19(5):337–344. doi: 10.1016/S1054-139X(96)00052-3. [DOI] [PubMed] [Google Scholar]
- Grant JD, Scherrer, Lynskey MT, Lyons MJ, Eisen SA, Tsuang MT, Bucholz KK. Adolescent alcohol use is a risk factor for adult alcohol and drug dependence: Evidence from a twin design. Psychological Medicine. 2006;26:109–118. doi: 10.1017/S0033291705006045. [DOI] [PubMed] [Google Scholar]
- Hawkins JD, Catalano RF, Arthur MW. Promoting science-based prevention in communities. Addictive Behaviors. 2002;27(6):951–976. doi: 10.1016/s0306-4603(02)00298-8. [DOI] [PubMed] [Google Scholar]
- Hawkins JD, Catalano RF, Miller JY. Risk and protective factors for alcohol and other drug problems in adolescence and early adulthood: implications for substance abuse prevention. Psychological Bulletin. 1992;112(1):64. doi: 10.1037/0033-2909.112.1.64. [DOI] [PubMed] [Google Scholar]
- Houck CD, Lescano CM, Brown LK, Tolou-Shams M, Thompson J, DiClemente R, Fernandez MI, Pugatch D, Schlenger WE, Silver BJ. “Islands of risk”: Subgroups of adolescents at risk for HIV. Journal of Pediatric Psychology. 31(6):619–629. doi: 10.1093/jpepsy/jsj067. [DOI] [PubMed] [Google Scholar]
- Huizink AC, Mulder EJ. Maternal smoking, drinking or cannabis use during pregnancy and neurobehavioral and cognitive functioning in human offspring. Neuroscience & Biobehavioral Reviews. 2006;30(1):24–41. doi: 10.1016/j.neubiorev.2005.04.005. [DOI] [PubMed] [Google Scholar]
- Ickovics JR. “Bundling” HIV prevention: Integrating services to promote synergistic gain. Preventive Medicine. 2008;46(3):222–225. doi: 10.1016/j.ypmed.2007.09.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kaiser MM, Hays BJ. Health‐risk behaviors in a sample of first-time pregnant adolescents. Public Health Nursing. 2005;22(6):483–493. doi: 10.1111/j.0737-1209.2005.220611.x. [DOI] [PubMed] [Google Scholar]
- Kalil A, Ziol-Guest KM. Teacher support, school goal structures, and teenage mothers' school engagement. Youth & Society. 2008;39(4):524–548. [Google Scholar]
- Klein JD. Adolescent pregnancy: Current trends and issues. Pediatrics. 2005;116(1):281–286. doi: 10.1542/peds.2005-0999. [DOI] [PubMed] [Google Scholar]
- Kotchick BA, Shaffer A, Miller KS, Forehand R. Adolescent sexual risk behavior: A multi-system perspective. Clinical Psychology Review. 2001;21(4):493–519. doi: 10.1016/s0272-7358(99)00070-7. [DOI] [PubMed] [Google Scholar]
- Leigh BC. Alcohol and condom use: a meta-analysis of event-level studies. Sexually Transmitted Diseases. 2002;29(8):476–482. doi: 10.1097/00007435-200208000-00008. [DOI] [PubMed] [Google Scholar]
- Logan TK, Cole J, Leukefeld C. Women, sex, and HIV: Social and contextual factors, meta-analysis of published interventions, and implications for practice and research. Psychological Bulletin. 2002;128:851–885. doi: 10.1037/0033-2909.128.6.851. [DOI] [PubMed] [Google Scholar]
- Logsdon MC, Birkimer JC, Simpson T, Looney S. Postpartum depression and social support in adolescents. Journal of Obstetric, Gynecologic, & Neonatal Nursing. 2005;34(1):46–54. doi: 10.1177/0884217504272802. [DOI] [PubMed] [Google Scholar]
- Mann JR, Mannan J, Quiñones LA, Palmer AA, Torres M. Religion, spirituality, social support, and perceived stress in pregnant and postpartum Hispanic women. Journal of Obstetric, Gynecologic, & Neonatal Nursing. 2010;39(6):645–657. doi: 10.1111/j.1552-6909.2010.01188.x. [DOI] [PubMed] [Google Scholar]
- Meade CS, Ickovics JR. Systematic review of sexual risk among pregnant and mothering teens in the USA: pregnancy as an opportunity for integrated prevention of STD and repeat pregnancy. Social Science & Medicine. 2005;60(4):661–678. doi: 10.1016/j.socscimed.2004.06.015. [DOI] [PubMed] [Google Scholar]
- Morrison DM, Spencer MS, Gillmore MR. Beliefs about substance use among pregnant and parenting adolescents. Journal of Research on Adolescence. 1998;8(1):69–95. doi: 10.1207/s15327795jra0801_4. [DOI] [PubMed] [Google Scholar]
- Odgers CL, Caspi A, Nagin DS, Piquero AR, Slutske WS, Milne BJ, Moffitt TE. Is it important to prevent early exposure to drugs and alcohol among adolescents? Psychological Science. 2008;19(10):1037–1044. doi: 10.1111/j.1467-9280.2008.02196.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Overbeek A, van den Berg MH, Hukkelhoven CWPM, Kremer LC, van den Heuvel-Eibrink MM, Tissing WJE, van Dulmen-den Broeder E. Validity of self-reported data on pregnancies for childhood cancer survivors: A comparison with data from a nationwide population-based registry. Human Reproduction. 2012;28(3):819–827. doi: 10.1093/humrep/des405. [DOI] [PubMed] [Google Scholar]
- Paranjothy S, Broughton H, Adappa R, Fone D. Teenage pregnancy: who suffers? Archives of Disease in Childhood. 2009;94(3):239–245. doi: 10.1136/adc.2007.115915. [DOI] [PubMed] [Google Scholar]
- Poulos CX, Parker JL, Le DA. Increased impulsivity after injected alcohol predicts later alcohol consumption in rats: evidence for “loss of control drinking” and marked individual differences. Behavioral Neuroscience. 1998;112(5):1247–1257. doi: 10.1037//0735-7044.112.5.1247. [DOI] [PubMed] [Google Scholar]
- Prado GJ, Schwartz SJ, Maldonado-Molina M, Huang S, Pantin HM, Lopez B, Szapocznik J. Ecodevelopmental× intrapersonal risk: Substance use and sexual behavior in Hispanic adolescents. Health Education & Behavior. 2008;36(1):45–61. doi: 10.1177/1090198107311278. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ramrakha S, Caspi A, Dickson N, Moffitt TE, Paul C. Psychiatric disorders and risky sexual behaviour in young adulthood: Cross sectional study in birth cohort. BMJ. 2000;321(7256):263–266. doi: 10.1136/bmj.321.7256.263. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rashad I, Kaestner R. Teenage sex, drugs and alcohol use: problems identifying the cause of risky behaviors. Journal of Health Economics. 2004;23(3):493–503. doi: 10.1016/j.jhealeco.2003.09.009. [DOI] [PubMed] [Google Scholar]
- Resnick MD, Bearman PS, Blum RW, Bauman KE, Harris KM, Jones J, Udry JR. Protecting adolescents from harm: Findings from the National Longitudinal Study on Adolescent Health. Journal of the American Medical Association. 1997;278(10):823–832. doi: 10.1001/jama.278.10.823. [DOI] [PubMed] [Google Scholar]
- Salas-Wright CP, Hernandez L, R. Maynard B, Y. Saltzman L, Vaughn MG. Alcohol Use among Hispanic early adolescents in the United States: An examination of behavioral risk and protective profiles. Substance Use & Misuse. 2014;49(7):864–877. doi: 10.3109/10826084.2014.880725. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Salas-Wright CP, Olate R, Vaughn MG. Preliminary findings on the links between violence, crime, and HIV risk among young adults with substance use disorders in El Salvador. Journal of Substance Use. 2014a Advance online publication. doi: 10.3109/14659891.2014.949317. [Google Scholar]
- Salas-Wright CP, Olate R, Vaughn MG. Substance use, violence, and HIV risk behavior among at-risk youth in El Salvador and the United States: Cross-national profiles of the SAVA Syndemic. Victims & Offenders. 2014b Advance online publication. doi: 10.1080/15564886.2014.940435. [Google Scholar]
- Salas-Wright CP, Vaughn MG, Maynard BR, Clark TT, Snyder S. Public or private religiosity: Which one is protective for adolescent substance use and by what pathways? Youth & Society. in press Advance online publication. doi: 10.1177/0044118X14531603. [Google Scholar]
- Salas-Wright CP, Vaughn MG, Hodge DR, Perron BE. Religiosity profiles of American youth in relation to substance use, violence, and delinquency. Journal of Youth and Adolescence. 2012;41(12):1560–1575. doi: 10.1007/s10964-012-9761-z. [DOI] [PubMed] [Google Scholar]
- Salas-Wright CP, Vaughn MG, Maynard BR. Religiosity and violence among adolescents in the United States: Findings from the National Survey on Drug Use and Health 2006-2010. Journal of Interpersonal Violence. 2013;29(7):1178–1200. doi: 10.1177/0886260513506279. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shneyderman Y, Schwartz SJ. Contextual and intrapersonal predictors of adolescent risky sexual behavior and outcomes. Health Education and Behavior. 2013;40:400–414. doi: 10.1177/1090198112447800. [DOI] [PubMed] [Google Scholar]
- Smith LM, LaGasse LL, Derauf C, Grant P, Shah R, Arria A, Lester BM. Prenatal methamphetamine use and neonatal neurobehavioral outcome. Neurotoxicology and Teratology. 2008;30(1):20–28. doi: 10.1016/j.ntt.2007.09.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spears GV, Stein JA, Koniak–Griffin D. Latent growth trajectories of substance use among pregnant and parenting adolescents. Psychology of Addictive Behaviors. 2010;24(2):322. doi: 10.1037/a0018518. [DOI] [PMC free article] [PubMed] [Google Scholar]
- StataCorp. Stata Statistical Software: Release 13. StataCorp LP.; College Station, TX: 2013. [Google Scholar]
- Stueve A, O'Donnell LN. Early alcohol initiation and subsequent sexual and alcohol risk behaviors among urban youths. American Journal of Public Health. 2005;95(5):887. doi: 10.2105/AJPH.2003.026567. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Teplin LA, Elkington KS, McClelland GM, Abram KM, Mericle AA, Washburn JJ. Major mental disorders, substance use disorders, comorbidity, and HIV-AIDS risk behaviors in juvenile detainees. Psychiatric Services. 2005;56(7):823–828. doi: 10.1176/appi.ps.56.7.823. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thompson JC, Kao TC, Thomas RJ. The relationship between alcohol use and risk-taking sexual behaviors in a large behavioral study. Preventive Medicine. 2005;41(1):247–252. doi: 10.1016/j.ypmed.2004.11.008. [DOI] [PubMed] [Google Scholar]
- Toumbourou JW, Stockwell T, Neighbors C, Marlatt GA, Sturge J, Rehm J. Interventions to reduce harm associated with adolescent substance use. The Lancet. 2007;369(9570):1391–1401. doi: 10.1016/S0140-6736(07)60369-9. [DOI] [PubMed] [Google Scholar]
- U.S. Department of Health and Human Services. Office of Disease Prevention and Health Promotion . Healthy People 2020. U.S. Department of Health and Human Services; Washington, DC: 2014. [Google Scholar]
- Vaughn MG, DeLisi M, Matto H. Human Behavior: A Cell to Society Approach. John Wiley and Sons; Hoboken, NJ: 2013. [Google Scholar]
- Vaughn MG, Salas-Wright CP, DeLisi M, Maynard BR. Violence and externalizing behavior among youth in the United States: Is there a severe 5%? Youth Violence and Juvenile Justice. 2014;12(1):3–21. [Google Scholar]
- Yonker JE, Schnabelrauch CA, DeHaan LG. The relationship between spirituality and religiosity on psychological outcomes in adolescents and emerging adults: A meta-analytic review. Journal of Adolescence. 2012;35(2):299–314. doi: 10.1016/j.adolescence.2011.08.010. [DOI] [PubMed] [Google Scholar]