Abstract
Objective
Network Support treatment was intended to help alcohol dependent patients alter their close social support networks to be more supportive of sobriety and less supportive of drinking. The purpose of the present study was to examine the differential influences of Network Support treatment on men and women.
Methods
Alcohol dependent men (n=122) and women (n=88) recruited from the community were randomly assigned to 1 of 3 12-week outpatient treatment conditions: Network Support (NS), Network Support + Contingency Management (NS+CM), or case management (CaseM; a control condition). Patients were then followed for a period of 27 months. Multilevel modeling was used to evaluate Sex X Treatment interaction effects on outcome variables over time. Tests of mediation were used to determine what factors might account for differential effectiveness for men or women in the NS conditions.
Results
Analyses of drinking-related outcome measures over the 27 months indicated that women fared less well overall, and particularly poorly in the Network Support conditions, relative to men. Tests of mediation indicated that self-efficacy change and change in the number of non-drinking close associates partially mediated the effect of NS treatments on outcome.
Conclusions
It was concluded that the NS conditions failed to alter women’s social networks, and may have had the effect of undermining women’s self-efficacy. Network Support treatment might be applicable for women and more effective generally if particular attention is paid to understanding preexisting social support networks.
Keywords: Alcohol Treatment, Gender Differences, Social Network, Network Support
1. Introduction
1.1 The Social Network for Women
In the alcohol literature the close social network of family and friends has been found to be very important, particularly for those in treatment trying to quit (Manuel, McCrady, Epstein, Cook, & Tonigan, 2007). The social network may be even more important for women than for men, in promoting both drinking and abstinence. A long history of research indicates that women, to a greater extent than men, rely on social support and social networks to cope with adversity (e.g., Ptacek, Smith, & Dodge, 1994; Tamres, Janicki, & Helgeson, 2002; Thoits, 1995). Falkin and Strauss (2003) noted that substance abusing women often have limited social networks, but that they rely on these networks for a variety of social and emotional needs. A treatment that makes that social network more supportive of abstinence should then be particularly effective for women.
1.2 Network Support Treatment: Altering the Close Social Network
Network Support Treatment (Litt, Kadden, Kabela-Cormier, & Petry, 2007) was developed to help alcohol dependent patients alter their close social support networks to make them more supportive of sobriety and less supportive of drinking. Given women’s reliance on the social network, women should fare better with a treatment that successfully builds such network support than with a treatment approach that does not. Indeed, Brown and colleagues (Brown, Seraganian, Tremblay, & Annis, 2002) found that women reported better alcohol outcomes with Twelve Step Facilitation (TSF) aftercare, which entails the building of new social networks, than their cohorts exposed to relapse prevention aftercare.
Networks supportive of drinking, however, may be particularly harmful for women. Davey-Rothwell and colleagues (Davey-Rothwell, Chander, Hester, & Latkin, 2011) noted that heavy episodic drinkers had fewer social network members generally than those who did not engage in heavy drinking, and that those they did have were more likely to drink and were less likely to have had any drug or alcohol treatment. These authors and others (McCrady, 2004) emphasized that women’s social networks may be either protective or predictive of pathological drinking, depending on their makeup.
1.3 The Present Study: Gender Effects in Network Support Treatment
The present study evaluated the relative efficacy of Network Support treatment for men and women. The Network Support trial included three arms: Network Support Treatment (NS), Network Support Treatment plus a contingency management component (NS+CM), which was intended to reinforce efforts to build new social networks, and Case Management (CaseM; a control condition). Each treatment was conducted in 12 weekly sessions, with follow-ups every three months out to 27 months.
It was expected that the Network Support approaches would be especially effective for women. In addition we wanted to find out what factors might account for any gender differences in response to Network Support treatment. Because of women’s reliance on their social networks, the NS conditions should have been more effective for women to the extent that they actually managed to change the social network to be more supportive. Social network variables (e.g., network size, network support for abstinence) and AA involvement were therefore analyzed as potential mediators of NS treatment outcomes for men versus women.
We also hypothesized that the effects of Network Support might be mediated by other factors that often account for the effects of treatment generally. That is, the establishment of more adaptive social networks was expected to have beneficial effects in several domains that would in turn affect drinking outcomes, including emotional distress/pathology (e.g., depression, anxiety), and cognitive/behavioral change processes (self-efficacy, use of coping skills, readiness for treatment).
2. Material and Methods
The following is a summary of methods and procedures. Complete details regarding these aspects of the study can be found in Litt et al. (2007; 2009). As documented in those articles, all measures and instruments had acceptable reliability and validity.
2.1 Participants
The participants were 122 men and 88 women, recruited from the community. Participants had to be at least 18 years old, and meet DSM-IV criteria for alcohol dependence or abuse. Individuals were excluded if they had acute medical or psychiatric problems requiring inpatient treatment (e.g., acute psychosis), current dependence on drugs (except nicotine and marijuana), or intravenous drug use in the previous 3 months, or if they had attended more than three AA meetings in the prior month.
The participants (58% male) had a mean age of 45 years (SD = 11.4), and were 86% White, 8% Black, 4% Hispanic, and 2% other. They had a mean of 13.7 years of schooling (SD = 2.1), 71% were employed at least part time outside the home, and 51% were living with a spouse or partner. All met criteria for alcohol dependence (99%) or abuse (1%) as per DSM-IV Axis I criteria, drank on average 72% of days in the 3 months prior to intake, and had a mean of 1.3 prior treatments for alcohol dependence (SD = 3.3). Assignment to treatment was as follows: NS (n=69; 31 women); NS+CM (n=71; 31 women); and CaseM (n=70; 26 women). At the final follow-up, 27 months post intake, 172 patients (82%) were interviewed.
2.2 Measures and Instruments
2.2.1 Drinking outcome data
Drinking data at baseline and at follow-ups were collected using the Form-90 structured interview (Miller & Del Boca, 1994). Drinking consequences (e.g., health, legal, social relations) were assessed using the Drinker Inventory of Consequences (DrInC; Miller, Tonigan, & Longabaugh, 1995).
2.2.2. Network support variables
Variables assessing social network support for drinking or for abstinence in the past 12 months were derived using the Important People and Activities structured interview (IPA; Clifford & Longabaugh, 1991). Five social network indices were used in the present study: Attitudinal Support for Abstinence, Attitudinal Support for Drinking, Behavioral Support for Abstinence, Behavioral Support for Drinking, and Social Support for Drinking. In addition, we included the number of close network associates (i.e., seen by the patient at least weekly) who were non-drinking (i.e., number of abstinent friends), a variable strongly predictive of outcome generally (Litt et al., 2009). Details regarding the scoring of these variables appear in Litt et al., (2007). Self-report of number of AA meetings attended in the 90 days prior to intake and at follow-ups (log-transformed) was also used as a process variable.
2.2.3 Emotional distress/psychopathology
Depression symptoms were measured using the Beck Depression Inventory (BDI; Beck, Ward, Mendelson, Mock, & Erbaugh, 1961). Anxiety was assessed using the state version of the Spielberger State-Trait Anxiety Inventory (STAI; Spielberger, Gorsuch, & Lushene, 1970). Anger, a frequent determinant of relapse (Marlatt & Gordon, 1985), was measured using the Spielberger Trait Anger Scale (TAS; Spielberger, Jacobs, Russel, & Crane, 1983).
2.2.4 Cognitive and behavioral change processes
Cognitive readiness for treatment was measured using the University of Rhode Island Change Assessment (URICA; DiClemente & Hughes, 1990). Self-efficacy was measured using the Alcohol Abstinence Self-Efficacy scale (AASE; DiClemente, Carbonari, Montgomery, & Hughes, 1994). The Coping Strategies Scale (CSS; Litt, Kadden, Cooney, & Kabela, 2003) was used to assess use of adaptive coping behaviors.
2.3 Procedures
2.3.1 Recruitment and initial contact
Participants were recruited through the use of newspaper and radio advertisements. Those who were eligible reviewed and signed an IRB-approved consent form and completed the intake assessment. Participants were assigned to treatment using an urn randomization procedure (Stout, Wirtz, Carbonari, & Del Boca, 1994) that balanced the three treatment conditions for gender, age, ethnicity and lifetime involvement with AA.
2.3.2 Data collection procedures
In-person follow-up interviews were conducted at months 3 (posttreatment), 9, 15, 21, and 27. Assessments at months 6, 12, 18 and 24 were conducted by telephone. Participants were compensated $40 for attending the initial intake assessment, $50 for each in-person follow-up assessment, and $20 for each telephone follow-up.
2.3.3 Treatments
Treatments were conducted in 12 weekly 60-minute outpatient sessions, employing detailed therapist manuals. Patients attended an average of 8.7 sessions, with no differences between treatment conditions, or between genders.
2.3.3.1 Case Management (CaseM)
The Case Management treatment (Steinberg et al., 2002) provided an active control condition that avoided any recommendations regarding social support or coping skills development. The therapist and participant used a problem checklist to identify problems in several domains that could be barriers to abstinence, including psychiatric, interpersonal (e.g., family), medical, employment, educational, financial, housing, legal, and transportation. The participant and therapist developed goals, and identified resources to address the goals using a comprehensive guide to local services. Attendance at AA was neither encouraged nor discouraged for CaseM participants.
2.3.3.2 Network Support treatment (NS)
The Network Support treatment was intended to help patients change their social support networks to be more supportive of abstinence and less supportive of drinking and was based on the Twelve-Step Facilitation (TSF) treatment created for Project MATCH (Nowinski, Baker, & Carroll, 1992). The program consisted of 6 core sessions (e.g., “Getting Active - changing one’s social network”), plus 6 elective sessions (from a selection of 9 topics; e.g., “Increasing Pleasant Activities”). Each session included assignment of recovery tasks (homework) geared toward expanding the sober social network and shrinking the drinking network.
2.3.3.3 Network Support + Contingency Management (NS+CM)
Participants in this condition received the same Network Support treatment as described above. In addition, reinforcements were provided contingent upon completion of assigned recovery tasks between sessions (e.g., attendance at AA meetings, having coffee with a non-drinking friend), using a fishbowl drawing procedure to determine amount of reinforcement (see Petry, 2000; Petry, Tedford, & Martin, 2001). During the 12 weeks of study participation a maximum of 234 draws could be earned. Patients in the NS+CM condition earned on average 56 draws and redeemed $250.00 worth of prizes, with no significant differences between men and women.
2.4 Data Analysis
The drinking outcome variables derived from the Form-90 were Proportion of Days Abstinent (PDA), Proportion Heavy Drinking Days (≥ 5 drinks for men, ≥ 4 drinks for women), and Continuous Abstinence for the 90-day period prior to each follow-up. The DrInC Total score was the psychosocial dependent variable. A measure of drinking intensity, Drinks per Drinking Day (log transformed), was also examined as a secondary outcome. Dependent variables were correlated with each other at about the r = .4 level.
Multilevel modeling with maximum likelihood estimation (Proc MIXED; SAS Institute, 1999) was used to analyze the continuously scaled dependent variables over time as a function of treatment condition and gender. Gender and Treatment conditions were both treated as fixed effects. Time (months since baseline) was treated as a fixed, repeated effect, and the intercept was included as a random effect. A generalized estimating equations (GEE; Proc GENMOD, SAS Institute, 1999) model was used to analyze the effect of treatment on the dichotomously scaled 90-day abstinence status prior to each of the follow-up points, with pretreatment PDA (transformed) as a covariate. For each of the dependent variables an a-priori contrast of NS and NS+CM versus CaseM was used to evaluate between-treatment differences by gender.
Multivariate analysis of variance (MANOVA) with univariate posttests was used to examine the pretreatment levels of the potential mediator variables by gender. This was done to determine if one gender might have been relatively disadvantaged prior to the start of treatment. These variables were grouped by domain to reduce the chance of Type 1 error.
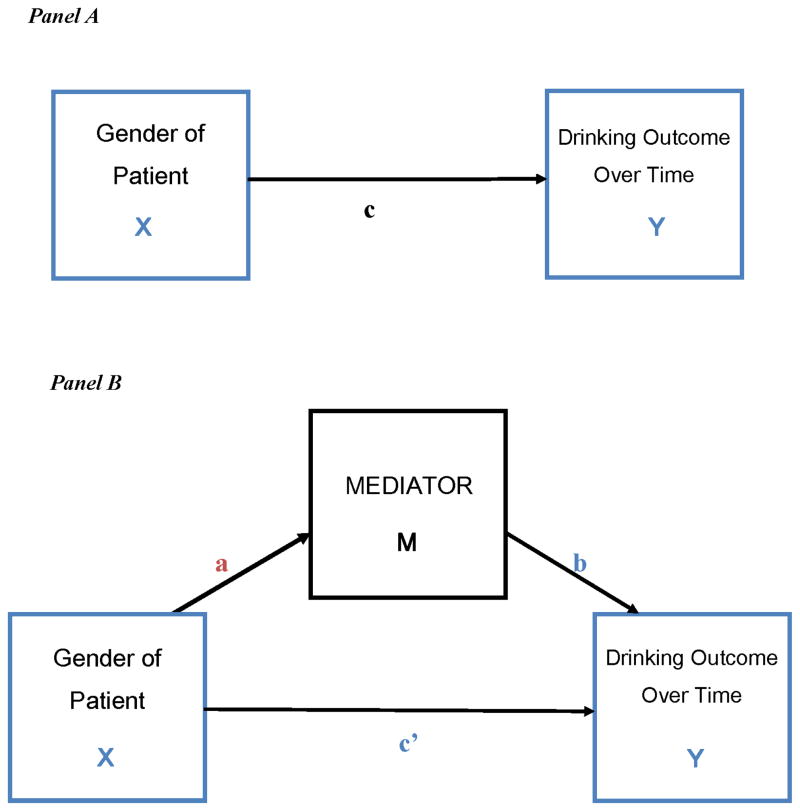
Finally, tests of mediation within the two Network Support conditions were conducted to determine what variables might account for any differential effects of gender on outcome in Network Support treatment. For these analyses PDA over time was used as the dependent variable. The tests were conducted using a procedure described by Krull and MacKinnon (2001), which employs the unstandardized estimates from multilevel models analyses as the coefficients for the direct and indirect paths from independent variables and mediators to the outcome. The mediation effect is estimated using a product of coefficients approach, and evaluated for significance as a Z score. Figure 1 illustrates the basic mediation analysis. In these analyses the mediator variables were calculated as difference scores from pre- to posttreatment, in order to reflect the direct effects of treatment on the mediator variables.
Figure 1.
Panel A: The direct effect. X (Patient Gender) affects Y (Drinking Outcome). Panel B: Illustration of a mediation design. X (Patient Gender) affects Y (Outcome) indirectly through M (emotional distress variables, social network variables, AA involvement, cognitive/behavioral change). Effect of X on Y though M is given by c′.
3. Results
3.1 Composition of Social Networks
Overall 50% of men and 46% of women were married. Of the married patients, 44% of the men and 35% of the women named his/her spouse among their closest contacts. Overall, however, these spouses tended to be supportive of abstinence, and 83% of spouses were either abstinent or classed as light drinkers (drinking 1 or fewer drinks per day) by patients. Those contacts who were heavy drinkers and those supportive of drinking tended to be persons outside of the immediate family, especially for women: of those who indicated that persons outside the family were their closest contact, 80% of women indicated that those persons were moderate to heavy drinkers (drinking 3–6 drinks daily), versus 55% of men.
3.2 Outcomes by Treatment and Gender
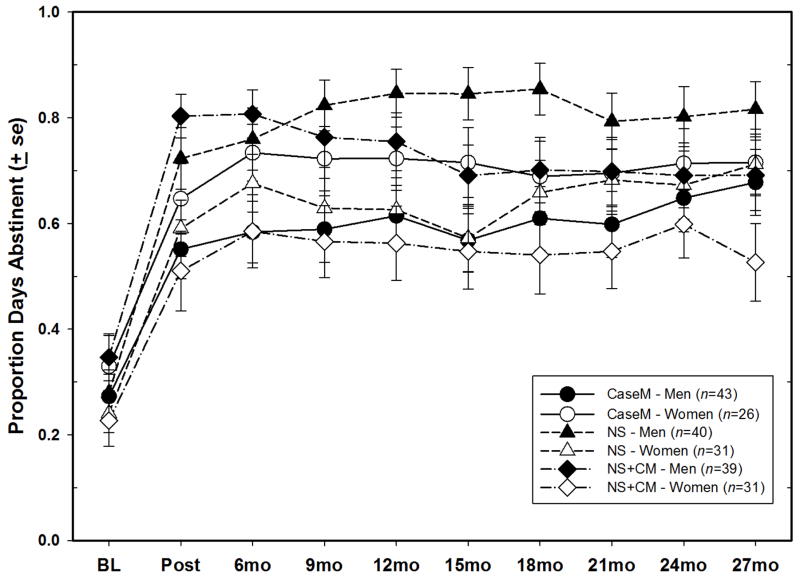
Table 1 shows the summary of the tests of treatment and gender on the outcome measures. As seen in the table, gender X treatment effects were seen in all dependent variables except for the DrInC measure of negative consequences. Furthermore, significant contrast effects of the NS conditions versus CaseM were seen in four of the six outcome measures. In each of the analyses in which significant gender X treatment interactions were found examination of means indicated that, in both of the Network Support treatment conditions, women failed to improve from pre to posttreatment to the same extent that men did, and that their performance continued at that lower level throughout the remainder of the follow-up period, another 24 months. As seen in Figure 2 for example, in terms of PDA, women performed most poorly in the NS+CM condition, but did not fare very much better in the NS condition, and for much of the trial women had their best outcomes with the CaseM treatment.
Table 1.
Summary of Tests of Effects of Gender and Treatment on Outcomes. Values Shown are F Values. N=210.
| Dependent Variable | Effect
|
Treatment Contrast: Gender X [NS; NS+CM] v. CaseM | ||||
|---|---|---|---|---|---|---|
| Gender (df = 1, 204) | Treatment (df=2, 204) | Time (df=9, 1607) | Gender X Treatment (df=2, 204) | Gender X Treatment X Time (df=45, 1607) | ||
| Proportion Days Abstinent (PDA) | 3.95* | 2.14 | 71.59*** | 5.68** | 1.26 | t(204) = 3.37** |
| Proportion Heavy Drinking Days (PDH) | 5.57* | 0.14 | 69.68*** | 4.28* | 0.95 | t(204) = 2.91** |
| Drinks/Drinking Day (DDD) (transformed) | 1.75 | 1.01 | 30.36*** | 4.43* | 1.51* | t(204) = 2.34* |
| Abstinencea | 8.24** | 2.38 | 20.36*** | 5.94* | 37.61 | t(204) = 3.02† |
| DrInC Total Scoreb | 1.86 | 1.46 | 58.82*** | 1.05 | 1.00 | t(204) = 1.32 |
Analysis performed by GEE; statistics shown are Wald χ2 values
Only five time intervals available for DrInC variable. Denominator degrees of freedom for analyses involving Time = 775.
p < .10;
p < .05;
p < .01;
p < .001
Figure 2.
Proportion Days Abstinent (PDA) by gender and treatment assignment.
3.3 Examination of Potential Mediators of Treatment by Gender
Results of MANOVAs on expected mediator variables by gender are shown in Table 2. As seen in the table, women were significantly different from men on each domain examined. Women tended to score higher than men on measures of emotional distress, but lower than men on baseline measures of cognitive change processes, particularly self-efficacy.
Table 2.
Comparison of Men and Women on Baseline Levels of Potential Mediators of Treatment Effects.
| Domain | Variable | Men (n = 122) | Women (n = 88) | F (1, 191) | Multivariate Test Wilks’ Lambda | ||
|---|---|---|---|---|---|---|---|
|
| |||||||
| Mean | SD | Mean | SD | ||||
| Social Network Variables | Abstinent People in Close Network | 1.40 | 1.22 | 1.22 | 1.18 | 1.00 | 0.92** |
| Attitudinal Support - Drinking | 2.74 | 0.67 | 2.84 | 0.65 | 1.21 | ||
| Behavioral Support - Abstinence | 0.37 | 0.33 | 0.29 | 0.27 | 3.50 | ||
| Behavioral Support – Drinking | 0.09 | 0.16 | 0.15 | 0.22 | 5.86* | ||
| Heavy Drinkers in Network | 0.40 | 0.74 | 0.55 | 0.76 | 2.01 | ||
| Social Support for Drinking | 5.66 | 1.12 | 5.97 | 0.93 | 4.20* | ||
| AA Involvement | AA Meetings Past 90 Days | 41.78 | 4.90 | 26.85 | 4.39 | 26.47*** | --.-- |
| Emotional Distress/Pathology | BDI | 12.34 | 7.45 | 16.31 | 9.09 | 10.32** | 0.91** |
| State Anxiety | 28.12 | 10.90 | 32.55 | 11.68 | 6.79** | ||
| Trait Anger | 26.12 | 6.81 | 27.42 | 8.83 | 1.23 | ||
| Cognitive/Behavioral Change Processes | Self-Efficacy | −4.59 | 27.96 | −19.66 | 25.37 | 14.68*** | 0.92** |
| Coping Total Score | 1.32 | 0.53 | 1.18 | 0.47 | 3.54 | ||
| Readiness Score | 80.43 | 12.22 | 81.31 | 12.12 | 0.24 | ||
Note:
p < .05;
p < .01;
p < .001.
In terms of variables indicative of social support for drinking or abstinence, women overall tended to report more support for drinking and less support for abstinence in their close social networks, and had made much less use of AA than men had. Although both men and women each averaged about 4.1 close social network members, the social networks of the women were more supportive of drinking.
3.4 Evaluation of Mediation of Network Support Treatment Effects for Men and Women
Mediation analyses were performed to determine what might account for the treatment differences between men and women in the two Network Support treatment conditions (N=141). As seen in Table 3, effects of treatment in the Network Support conditions for men and women were mediated by changes in self-efficacy and in number of close abstinent friends in the social network. Women compared to men reported a smaller (and non-significant) increase in the number of close non-drinking friends during treatment, which in turn accounted in part for poorer performance than men in the Network Support treatments. Likewise, women reported significantly smaller increases in abstinence self-efficacy from pre- to posttreatment than men did (51 point increase for men v. 20 point increase for women). Interestingly, the correlation of the self-efficacy measures with numbers of close abstinent friends was on the order of r=.20, indicating that abstinence self-efficacy and close non-drinking supports operated independently in promoting good drinking outcomes.
Table 3.
Results from Multilevel Mediation Analyses of PDA Over Time as a Function of Gender. NS and NS+CM Treatments Only. N=141.
| Mediator Domain and Variable | A-Path
|
B-Path
|
Indirect Effect (C′)
|
|||||
|---|---|---|---|---|---|---|---|---|
| B | SE | B | SE | B | Z | 95% CI
|
||
| Lower CI | Upper CI | |||||||
| Emotional Distress/Pathology Variables | ||||||||
| Beck Depression Score | 1.7913* | 0.792 | −0.0053* | 0.003 | −0.010 | −1.52 | −0.029 | 0.010 |
| State Anxiety Score | 2.9452* | 1.191 | −0.0034 | 0.002 | −0.010 | −1.50 | −0.030 | 0.010 |
| Trait Anger Score | 1.5178* | 0.520 | −0.0149 | 0.011 | −0.023 | −1.20 | −0.077 | 0.032 |
| Social Network Variables | ||||||||
| Abstinent Friends in Network | −0.1207* | 0.014 | 0.0453* | 0.019 | −0.005 | −2.30* | −0.008 | −0.003 |
| Attitudinal Support - Abstinence | −0.2029*** | 0.061 | 0.0567 | 0.033 | −0.012 | −1.52 | −0.030 | 0.007 |
| Attitudinal Support - Drinking | 0.1344* | 0.624 | −0.0442 | 0.034 | −0.006 | −0.21 | −0.020 | 0.188 |
| Behavioral Support - Abstinence | −0.0457 | 0.029 | 0.0981 | 0.072 | −0.004 | −1.03 | −0.024 | 0.015 |
| Behavioral Support – Drinking | 0.0582 | 0.165 | −0.0233* | 0.126 | 0.001 | 0.16 | −0.191 | 0.194 |
| Social Support for Drinking | 0.1734 | 0.091 | −0.0495* | 0.023 | −0.009 | −1.43 | −0.028 | 0.011 |
| AA Involvement | ||||||||
| AA Meetings | −3.8966* | 1.778 | 0.0026* | 0.001 | 0.010 | 1.58 | −0.009 | 0.029 |
| Cognitive/Behavioral Change Processes | ||||||||
| Self-Efficacy | −2.5328* | 0.365 | 0.0017* | 0.001 | −0.004 | −2.36* | −0.006 | −0.002 |
| Coping Total Score | −0.1496** | 0.488 | 0.0364 | 0.042 | −0.005 | −0.83 | −0.025 | 0.014 |
| Readiness Score | 0.7597 | 0.446 | 0.0051 | 0.608 | −0.001 | −0.01 | −0.275 | 0.274 |
p < .05;
p < .01;
p < .001
Note: A-Path: Effect of gender on the mediator. B-path: Effect of mediator on outcome (PDA over time). Indirect effect: Portion of the effect of gender on PDA over time that is accounted for by the mediator variable. Gender was coded as Men=1; Women=2.
4. Discussion
Network Support treatment was, overall, a rather successful program, yielding upwards of 83% days abstinent, sustained over 2 years, depending on the specific NS condition. It was, however, distinctly more successful for men than for women. The current study was intended to determine why such gender differences might have taken place.
First, as noted in Table 2, the women in this study were more vulnerable to relapse and continued drinking than were the men. Although pretreatment drinking rates were comparable between men and women, women tended to score as more depressed and more anxious than men, placing these women at increased risk (Haver, 2003; Kranzler, Del Boca, & Rounsaville, 1996). Additionally, women reported significantly lower scores than men on self-efficacy for achieving abstinence, a robust predictor of outcomes (Kadden & Litt, 2011). The women in the Network Support treatment conditions never made up these differences.
Most notable was that women had networks that were less supportive of abstinence than those of men, and were less likely than men to make it more supportive (see Table 3). It has been observed that if women’s confidants promote maladaptive behavior such as drinking, the effect of the close social network will be harmful (Pattison, Llamas, & Hurd, 1979). What we saw in this study was that the women in the Network Support treatments tended to have stable, but not helpful, social networks, and, unlike the men, they tended not to expand their network over the course of the study. One possible reason for such network stability could be that the closest associated are family members, especially spouses. That was not the case here, however. Interestingly, at least in this sample, the close network associates who supported drinking among women, even married women, tended to be outside the family. The failure to adopt a new network, or even add a single close non-drinking associate, may have been crucial (Litt et al., 2009).
For reasons that are not clear at this time, CaseM and NS differed in their effectiveness for women. In the NS conditions women were urged to change their social networks and thereby reduce their drinking. Their lower self-efficacy in the NS conditions may have reflected the difficulty women were having in changing what were stable, if not particularly adaptive, social networks. In CaseM, on the other hand, attention was directed to concrete actions that women could take in their lives that may or may not have been related to their drinking. It is possible that the achievement of concrete goals was sufficient to boost self-efficacy and produce good long-term outcomes. Change in self-efficacy was a significant predictor of PDA in the CaseM condition, and, unlike in the NS conditions, women in CaseM reported significantly greater change in self-efficacy than men did (an increase of 27.3 points for women v. 16.1 points for men).
5. Conclusions
We believe that Network Support treatment remains a compelling strategy for helping patients discontinue drinking. The treatment was primarily aimed at developing new network resources, with the implication being that old drinking friends would be replaced by non-drinking friends. From the results presented here it appears that it will also be important, especially for women, to specifically examine the degree to which the existing social network supports drinking. It may not be necessary for women to drop their close drinking associates, particularly drinking spouses, if they can also add some non-drinking ones. Prior results from this research suggest that the addition of even one non-drinking close associate to the social network is sufficient to significantly boost chances of abstinence in the long-term (Litt et al., 2009). These results indicate that attending to social network composition and self-efficacy may help us to improve the effectiveness of Network Support treatment, especially for women.
Highlights.
Network Support treatment was designed to help alcohol-dependent persons create a close social network that would support abstinence, and not drinking.
Overall, Network Support treatment was superior to a Case Management control treatment in reducing drinking, but women generally fared poorly in Network Support.
Analyses presented here indicate that women were more likely than men to preserve their maladaptive social networks, and that women had low self-efficacy regarding their ability to stay sober in Network Support treatment.
Acknowledgments
Role of Funding Sources
Support for this project was provided by grant 1 R01 AA12827 from the National Institute on Alcohol Abuse and Alcoholism (NIAAA). NIAAA had no role in the study design, collection, analysis or interpretation of the data, writing the manuscript, or the decision to submit the paper for publication.
The authors would like to acknowledge Elise Kabela-Cormier, Eileen Leonard, William Blakey, Kara Dion, and Abigail Young for their work in the conduct of this study. Portions of this article were presented at the June 2014 meeting of the Research Society on Alcoholism in Bellevue, Washington, USA.
Footnotes
Contributors
Authors Litt and Kadden designed the study and wrote the protocol. All authors conducted literature searches and provided summaries of previous research studies. Author Litt conducted the statistical analyses and wrote the first draft of the manuscript. Author Tennen reviewed and early draft and substantially edited the paper. All authors reviewed and edited the manuscript, and have approved the final draft.
Conflicts of Interest
None of the authors have any conflicts of interest related to this work.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Contributor Information
Mark D. Litt, Email: Litt@nso.uchc.edu.
Ronald M. Kadden, Email: Rkadden@uchc.edu.
Howard Tennen, Email: tennen@uchc.edu.
References
- Beck AT, Ward CH, Mendelson M, Mock J, Erbaugh J. An inventory for measuring depression. Archives of General Psychiatry. 1961;4:561–571. doi: 10.1001/archpsyc.1961.01710120031004. [DOI] [PubMed] [Google Scholar]
- Brown TG, Seraganian P, Tremblay J, Annis H. Matching substance abuse aftercare treatments to client characteristics. Addictive Behaviors. 2002;27:585–604. doi: 10.1016/s0306-4603(01)00195-2. [DOI] [PubMed] [Google Scholar]
- Clifford PR, Longabaugh R. Manual for the Important People and Activities Instrument. Providence, RI: Center for Alcohol and Addiction Studies, Brown University; 1991. [Google Scholar]
- Davey-Rothwell MA, Chander G, Hester L, Latkin CA. Social network characteristics and heavy episodic drinking among women at risk for HIV/sexually transmitted infections. Journal of Studies on Alcohol and Drugs. 2011;72:1041–1047. doi: 10.15288/jsad.2011.72.1041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- DiClemente CC, Carbonari JP, Montgomery RP, Hughes SO. The Alcohol Abstinence Self-Efficacy scale. Journal of Studies on Alcohol. 1994;55:141–148. doi: 10.15288/jsa.1994.55.141. [DOI] [PubMed] [Google Scholar]
- DiClemente CC, Hughes SO. Stages of change profiles in outpatient alcoholism treatment. Journal of Substance Abuse. 1990;2:217–235. doi: 10.1016/s0899-3289(05)80057-4. [DOI] [PubMed] [Google Scholar]
- Falkin GP, Strauss SM. Social supporters and drug use enablers: a dilemma for women in recovery. Addictive Behaviors. 2003;28:141–155. doi: 10.1016/s0306-4603(01)00219-2. [DOI] [PubMed] [Google Scholar]
- Haver B. Comorbid psychiatric disorders predict and influence treatment outcome in female alcoholics. European Addiction Research. 2003;9:39–44. doi: 10.1159/000067735. 67735. [DOI] [PubMed] [Google Scholar]
- Kadden RM, Litt MD. The role of self-efficacy in the treatment of substance use disorders. Addictive Behaviors. 2011;36:1120–1126. doi: 10.1016/j.addbeh.2011.07.032. S0306-4603(11)00242-5 [pii] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kranzler HR, Del Boca FK, Rounsaville BJ. Comorbid psychiatric diagnosis predicts three-year outcomes in alcoholics: a posttreatment natural history study. Journal of Studies on Alcohol. 1996;57:619–626. doi: 10.15288/jsa.1996.57.619. [DOI] [PubMed] [Google Scholar]
- Krull JL, MacKinnon DP. Multilevel modeling of individual and group level mediated effects. Multivariate Behavioral Research. 2001;36:249–277. doi: 10.1207/S15327906MBR3602_06. [DOI] [PubMed] [Google Scholar]
- Litt MD, Kadden RM, Cooney NL, Kabela E. Coping skills and treatment outcomes in cognitive-behavioral and interactional group therapy for alcoholism. Journal of Consulting and Clinical Psychology. 2003;71:118–128. doi: 10.1037//0022-006x.71.1.118. [DOI] [PubMed] [Google Scholar]
- Litt MD, Kadden RM, Kabela-Cormier E, Petry N. Changing network support for drinking: initial findings from the network support project. Journal of Consulting and Clinical Psychology. 2007;75:542–555. doi: 10.1037/0022-006X.75.4.542. [DOI] [PubMed] [Google Scholar]
- Litt MD, Kadden RM, Kabela-Cormier E, Petry NM. Changing network support for drinking: Network support project 2-year follow-up. Journal of Consulting and Clinical Psychology. 2009;77:229–242. doi: 10.1037/a0015252. 2009-03774-004 [pii] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Manuel JK, McCrady BS, Epstein EE, Cook S, Tonigan JS. The pretreatment social networks of women with alcohol dependence. Journal of Studies on Alcohol and Drugs. 2007;68:871–878. doi: 10.15288/jsad.2007.68.871. [DOI] [PubMed] [Google Scholar]
- Marlatt GA, Gordon JR. Relapse prevention: Maintenance strategies in the treatment of addictive behaviors. New York: Guilford; 1985. [Google Scholar]
- McCrady BS. To have but one true friend: implications for practice of research on alcohol use disorders and social network. Psychology of Addictive Behaviors. 2004;18:113–121. doi: 10.1037/0893-164X.18.2.113. [DOI] [PubMed] [Google Scholar]
- Miller WR, Del Boca FK. Measurement of drinking behavior using the Form 90 family of instruments. Journal of Studies on Alcohol Supplement. 1994;12:112–118. doi: 10.15288/jsas.1994.s12.112. [DOI] [PubMed] [Google Scholar]
- Miller WR, Tonigan JS, Longabaugh R. The Drinker Inventory of Consequences (DrInC) Rockville, MD: U.S. Government Printing Office; 1995. DHHS Publication No. 95–3911. [Google Scholar]
- Nowinski J, Baker S, Carroll K. Twelve Step Facilitation Therapy Manual: A Clinical research Guide for Therapists Treating Individuals with Alcohol Abuse and Dependence. Washington, D.C: U.S. Government Printing Office; 1992. pp. 92–1893. (DHHS Publication No. (ADM) [Google Scholar]
- Pattison EM, Llamas R, Hurd G. Social network mediation of anxiety. Psychiatric Annals. 1979;9:474–482. [Google Scholar]
- Petry NM. A comprehensive guide to the application of contingency management procedures in clinical settings. Drug and Alcohol Dependence. 2000;58:9–25. doi: 10.1016/s0376-8716(99)00071-x. [DOI] [PubMed] [Google Scholar]
- Petry NM, Tedford J, Martin B. Reinforcing compliance with non-drug-related activities. Journal of Substance Abuse Treatment. 2001;20:33–44. doi: 10.1016/s0740-5472(00)00143-4. [DOI] [PubMed] [Google Scholar]
- Ptacek JT, Smith RE, Dodge KL. Gender Differences in Coping with Stress - When stressor and appraisals do not differ. Personality and Social Psychology Bulletin. 1994;20:421–430. doi: 10.1177/0146167294204009. [DOI] [Google Scholar]
- SAS Institute. SAS/STAT software: Changes and enhancements through V7 and V8. Cary, NC: 1999. [Google Scholar]
- Spielberger CD, Gorsuch RL, Lushene RE. STAI Manual for the State-Trait Anxiety Inventory. Palo-Alto, CA: Consulting Psychologists Press; 1970. [Google Scholar]
- Spielberger CD, Jacobs G, Russel S, Crane RS. Assessment of anger: The State-Trait Anger Scale. In: Butcher JN, Spielberger CD, editors. Advances in Personality Assessment. Vol. 2. Hillsdale, N.J: Lawrence Erlbaum; 1983. pp. 159–187. [Google Scholar]
- Steinberg KL, Roffman RA, Carroll KM, Kabela E, Kadden R, Miller M, et al. Tailoring cannabis dependence treatment for a diverse population. Addiction. 2002;97(Suppl 1):135–142. doi: 10.1046/j.1360-0443.97.s01.5.x. [DOI] [PubMed] [Google Scholar]
- Stout RL, Wirtz PW, Carbonari JP, Del Boca FK. Ensuring balanced distribution of prognostic factors in treatment outcome research. Journal of Studies on Alcohol - Supplement. 1994;12:70–75. doi: 10.15288/jsas.1994.s12.70. [DOI] [PubMed] [Google Scholar]
- Tamres LK, Janicki D, Helgeson VS. Sex Differences in Coping Behavior: A Meta-Analytic Review and an Examination of Relative Coping. Personality and Social Psychology Review. 2002;6:2–30. [Google Scholar]
- Thoits PA. Stress, coping, and social support processes: where are we? What next? Journal of Health and Social Behavior. 1995:53–79. [PubMed] [Google Scholar]