Abstract
Objective
To develop a method for quantifying leakage in composite resin restorations after curing, using non-destructive X-ray micro-computed tomography (micro-CT) and image segmentation.
Methods
Class-I cavity preparations were made in 20 human third molars, which were divided into 2 groups. Group I was restored with Z100 and Group II with Filtek LS. Micro-CT scans were taken for both groups before and after they were submerged in silver nitrate solution (AgNO3 50%) to reveal any interfacial gap and leakage at the tooth restoration interface. Image segmentation was carried out by first performing image correlation to align the before- and after-treatment images and then by image subtraction to isolate the silver nitrate penetrant for precise volume calculation. Two-tailed Student’s t-test was used to analyze the results, with the level of significance set at p<0.05.
Results
All samples from Group I showed silver nitrate penetration with a mean volume of 1.3 ± 0.7 mm3. In Group II, only 2 out of the 10 restorations displayed infiltration along the interface, giving a mean volume of 0.3 ± 0.3 mm3. The difference between the two groups was statistically significant (p < 0.05). The infiltration showed non-uniform patterns within the interface.
Significance
We have developed a method to quantify the volume of leakage using non-destructive micro-CT, silver nitrate infiltration and image segmentation. Our results confirmed that substantial leakage could occur in composite restorations that have imperfections in the adhesive layer or interfacial debonding through polymerization shrinkage. For the restorative systems investigated in this study, this occurred mostly at the interface between the adhesive system and the tooth structure.
Keywords: Interfacial debonding, composite resins, dental adhesives, micro-CT, leakage, secondary caries
1. INTRODUCTION
One of the major functions of a dental restoration is to cover the exposed dental tissues following caries removal. A tight seal around the margin will provide protection against pulpal damage and recurrent tooth decay [1]. Despite the many advances in adhesive technologies, it remains a challenge to adequately seal the restoration margins and prevent leakage for a sufficiently long period of time. Therefore, new adhesive systems and composite materials are still being developed which require assessment [2].
Several techniques have been used to assess interfacial gap formation and microleakage, but the results vary considerably [3]. The majority of them involve the use of dyes as tracers: a dental restoration is immersed in a specific dye solution for a period of time, after which the specimen is sectioned for visual examination of dye penetration around the restorative material [1]. One of the main drawbacks of this method is that it only provides a qualitative assessment, namely, confirmation of the presence or absence of the dye in the particular section studied. A variant of this approach incorporates a non-parametric scale, providing a semi-quantitative score according to the degree of dye penetration. However, the score definitions and the scale used vary among the studies, making the results from them not comparable. This qualitative or semi-quantitative evaluation makes the test itself not very reliable or discriminative. In addition, evaluation can only be carried out in the plane through which the sample is sectioned, which can be misleading because dye infiltration does not occur uniformly throughout the interface (see later). Therefore, it is necessary to develop techniques to accurately quantify interfacial leakage.
X-ray micro-computed tomography (micro-CT) has been used recently to study composite shrinkage, gap formation and microleakage [4–8]. It allows 3D reconstruction of the entire dental restoration and its surrounding tissues. The different components are identified based on the differences in their ability to attenuate the X-ray, with the differences being converted into a range of greyscale values. Micro-CT has the advantage of being non-destructive, i.e., the specimens do not need to be destroyed, allowing them to be reused for temporal assessment, for example.
In order to use micro-CT to study interfacial integrity in composite restorations, a radiopaque dye is often necessary [5, 6]. This is because the low density of most dental adhesives makes it difficult to distinguish them from any gaps that may form at the tooth-restoration interface. Previous studies exploring marginal infiltration of glass-ionomer sealant [5] and Class-II composite restorations [6] showed that marginal leakage along the interface could be traced when micro-CT is used in combination with a radiopaque dye. However, in both of these studies only a cross-sectional analysis was performed, with a non-parametric scale being applied to assess infiltration. The assessments were therefore only semi-quantitative, as explained above.
3D analysis of polymerization shrinkage of a dental composite and the resulting gap formation has been performed using micro-CT to predict microleakage [7, 8]. In [7], composites placed in plastic holders with different volumes were studied. To evaluate shrinkage, the volume of the composite before and after curing was calculated after 3D reconstruction. Also, direct measurement of the gap between the composite and the holder was performed to predict leakage. Gap formation and, hence, the predicted microleakage was shown to be non-uniform around the interface, being highly dependent on the C-factor, i.e. the ratio between the bonded and unbonded surfaces, and the composite volume [7]. A later study reported similar results when composite restorations were placed in human molars [8]. These studies showed that 3D quantitative assessment of microleakage could be obtained with micro-CT, which overcame one of the main disadvantages of conventional techniques for microleakage analysis. However, in both of these studies an adhesive was not used in order to simplify the system, possibly because the radiolucency of the adhesive would make it difficult to differentiate it from a gap in the micro-CT images. Needless to say, clinically, the adhesive plays an important role in the formation of interfacial gaps and must therefore be included when microleakage and gap formation are being studied. Additionally, in the latter study [8] the dental restoration was placed only in the dentin portion of the cavity, leaving bonding to the enamel surface out of the investigation. The reason for this omission was the difficulty to separate the grey values of enamel and those of the restoration in the CT images.
In order to properly assess leakage, it is important to replicate the clinical situation as closely as possible in any in vitro study by involving all the components in a restored tooth. To overcome the limitations associated with the techniques mentioned above, the aim of this study is to propose an improved and more comprehensive method using micro-CT to quantify interfacial leakage in dental restorations.
Recently, interfacial debonding of composites restorations that occurred during polymerization was monitored in situ using the Acoustic Emission (AE) technique [9]. AE events were recorded in real time from human molars with Class-I cavities restored with either Z100™ (Z100) or Filtek™ LS (LS) (both from 3M ESPE, St. Paul, MN, USA) during curing. The number of AE events recorded from the specimens restored using Z100 was much higher than that found in the specimens restored with LS. The results were confirmed by micro-CT imaging which showed clear interfacial debonding in the former but not the latter. These AE results will be compared directly with the volumetric calculation of the dye penetrant obtained in this study.
2. MATERIALS AND METHODS
2.1 Sample preparation
Twenty human third molars were selected for this study. The use of human molars was approved by the University of Minnesota Institutional Review Board. The teeth were cleaned by removing the soft tissues and hard deposits attached to the surface and then kept in 0.1% thymol solution. Class-I cavity preparations, approximately 2-mm high, 2-mm wide and 4-mm long, were made on the occlusal surface of each tooth. The teeth were divided randomly into two groups of 10. Group I was restored with Z100 (Table 1), which was considered for the purpose of this paper as a high-shrinkage composite. Group II was filled with LS (Table 1), a low-shrinkage composite by comparison. For Group I, total etching of the tooth cavity was performed with 37% Scotchbond™ Etchant for 20 s, followed by rinsing with the triple syringe for 40 s. Adper™ Single Bond II (3M ESPE, St. Paul, MN, USA) was then used as the bonding system. For Group II, Filtek™ LS System Adhesive (3M ESPE, St. Paul, MN, USA), a self-etch primer and bonding system, was used. The manufacturer’s guidelines were followed closely when applying the bonding systems. After placing the bonding system, the corresponding composite, either Z100 or LS (both A2 shade), was placed incrementally into the cavity. Each layer of composite, which was no more than 2-mm thick, was cured for 40 s, utilizing an Elipar™ S10 LED curing light (3M ESPE, St. Paul, MN, USA) with an irradiance of 1200 mW/cm2. Thereafter, each restoration was polished by using a polishing cup.
Table 1.
Compositions of composites and adhesives used for Class-I restorations (obtained from manufacturer’s data sheets (3M ESPE))
| Z100™ Restorative | Silane treated ceramic, triethylene glycol dimethacrylate (TEGDMA), bisphenol a diglycidyl ether dimethacrylate (BISGMA), 2-benzotriazolyl-4-methylphenol. | N362970 |
| Filtek™ LS Low Shrink Posterior Restorative | Silane treated quartz, 3,4 epoxycyclohexylcyclopolymethylsiloxane, bis-3,4 epoxycyclohexylethyl-phenyl-methylsilane, yttrium trifluoride, mixture of other by-products mixture of epoxymono-silanole by-products, mixture of epoxyfunctional di-and oligo-siloxane by-products, mixture of alpha-substituted by-products borate(1-), tetrakis(pentafluorophenyl)-[4-(methylethyl)phenyl](4-methylphenyl)iodonium. | N296926 |
| Adper Single Bond Plus | Ethyl alcohol, silane treated silica (nanofiller), bisphenol a diglycidyl ether dimethacrylate (BISGMA), 2-hydroxyethyl methacrylate(HEMA), glycerol 1,3-dimethacrylate, copolymer of acrylic and itaconic acids, water, diurethane dimethacrylate (UDMA) diphenyliodonium hexafluorophosphate, ethyl 4-dimethyl aminobenzoate (EDMAB). | N509492 |
| Filtek™ LS System Adhesive Self-Etch Primer and Bond | Primer: Bisphenol a diglycidyl ether dimethacrylate (BISGMA), 2-hydroxyethyl methacrylate (HEMA), Phosphoric acid-methacryloxy-hexylesters mixture, ethanol, water, silane treated silica, 1,6-hexanediol dimethacrylate, (dimethylamino)ethyl methacrylate, Copolymer of acrylic and itaconic acid, Phosphine oxide, Dl-camphorquinone, Ethyl 4-dimethyl aminobenzoate, Methyl alcohol Bond: Substituted dimethacrylate, silane treated silica, triethylene glycol dimethacrylate (TEGDMA), phosphoric acid methacryloxy- hexylesters mixture, Dl-camphorquinone, 1,6-hexanediol dimethacrylate. |
N348567 |
| N391675 |
Each sample was then positioned in a plastic holder and fixed with acrylic resin with the purpose of avoiding sample movement during the experiment (Fig. 1). The holder was specially machined to generate an interlock with the supporting base attached to the stage inside the micro-CT chamber so that the sample could be placed in the same position and orientation for scanning before and after treatment with silver nitrate. The crown was covered with nail polish, leaving a gap of ~1 mm around the tooth-restoration interface. This allowed the silver nitrate to penetrate the interfacial gaps that might form and prevented it from entering the interface through other defects on the crown surfaces.
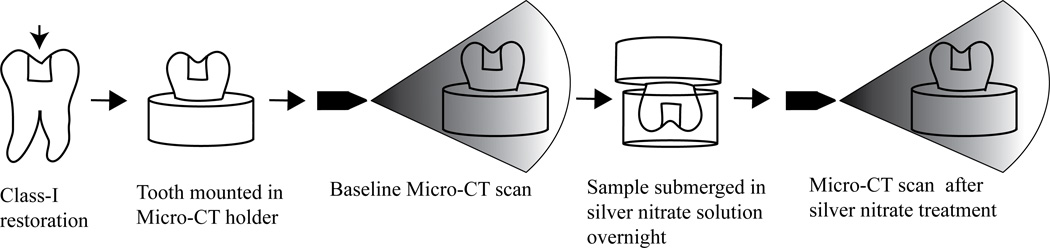
Figure 1.
Experimental set up and workflow for the leakage study: A Class-I restoration was placed on the occlusal surface of a third molar. The restored tooth was then fixed within a holder with acrylic resin for micro-CT scanning. A baseline scan was first obtained before the restored tooth was submerged in AgNO3. After that, a second micro-CT scan was taken using the same position and operational parameters as for the baseline.
2.2 Scanning and AgNO3 Treatment
Scanning of the specimens was performed using a Micro-CT machine (XT H 225, Nikon Metrology Inc., Brighton, MI, USA); see Fig. 1. The scanning parameters used were 90 kV, 90 µA, 708 ms of exposure, 720 projections and 4 frames per projection. The position of each specimen within the micro-CT machine for the baseline scan was stored in a file that could be loaded in a subsequent scan to return it back to the same position (Fig. 1). The total scanning time was approximately 30 minutes for each specimen. A small piece of wet cotton was used to cover the specimen to prevent it from drying and cracking during scanning.
To reveal any interfacial defects or debonding between the restoration and the tooth structure after curing, the specimens were submerged in a radiopaque silver nitrate solution (AgNO3, 50% w/w) [6] overnight (Fig 1). The pH of the AgNO3 solution was measured as ~3.3.
Both groups were subjected to a second scan after submersion in the AgNO3 solution (Fig 1). The same scanning parameters as those for the baseline scans were used to ensure consistency in the greyscale values. The baseline sample position was then loaded to ensure that each specimen was rescanned in the same position within the micro-CT machine to minimize misalignment of the two image sets.
2.3 Image processing
3D reconstructions were done using the software CT Pro 3D (Nikon metrology, Inc., Brighton, MI, USA). The same volume of interest (VOI) was used for both the baseline and post-treatment scans to give the same spatial resolution. Initial visualization and 3D rendering was performed using VGStudio MAX 2.1 (Volume Graphics GmbH, Heidelberg, Germany). All the reconstructed images were scrutinized, slice-by-slice, for silver nitrate penetration, as indicated by a bright line formed by the radiopaque dye along the interface. For comparison, a series of bucco-lingual cross-sectional images were retrieved from both the baseline and the post-treatment scans for each of the samples.
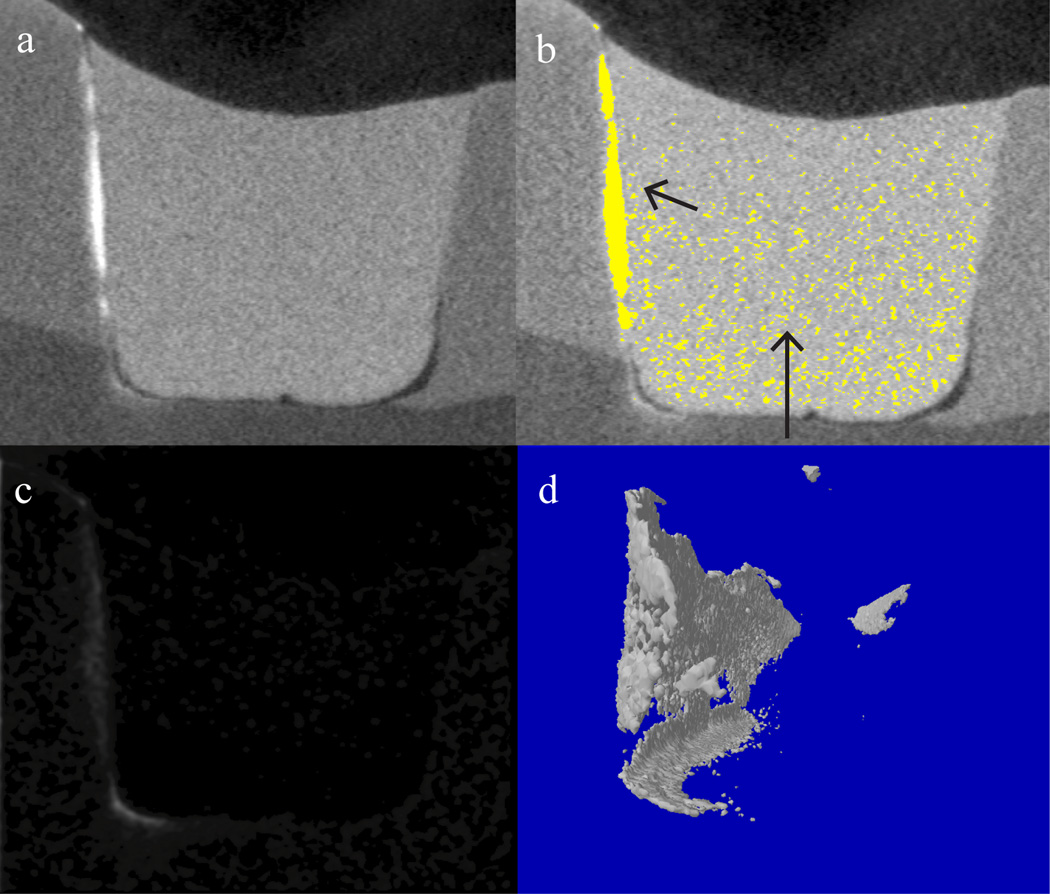
It was not possible to completely isolate the voxels corresponding to the penetrant in the post-treatment images (Fig. 2a) by simply selecting the narrow range of grey values for this material because some of the components of the restoration also had similar grey values. This can be seen in Fig. 2b in which the silver nitrate and the dense components in the restoration are highlighted by the same false color. To overcome this issue, an image correlation function was used to align the images taken before and after dye penetration as-shifting of images in space was likely the result of play in the fixture and/or the moving table of the micro-CT system [10]. The image alignment was followed by image subtraction to remove the composite restoration and dental tissues from the images, leaving behind the silver nitrate only (Fig. 2c). Thus, the grey values of the baseline images were subtracted from those of the post-treatment images. The image processing was carried out using MATLAB and the Image Processing Toolbox (Mathwork®) [11]. The image subtraction procedure resulted in new image stacks, which could then be rendered to reveal the thin layer of silver nitrate in 3D space (Fig 2d). The final subtracted images were exported as bmp extension files for further analysis.
Figure 2.
a) Image from a Group-I sample of the penetrant along the tooth-restoration interface. b) A false color plot illustrating the difficulty to isolate the silver nitrate penetrant which shares the same grey values with the dense components in the restoration. c) Image of the penetrant isolated after image subtraction. d) 3D rendering of the silver nitrate penetrant using the subtracted image stack.
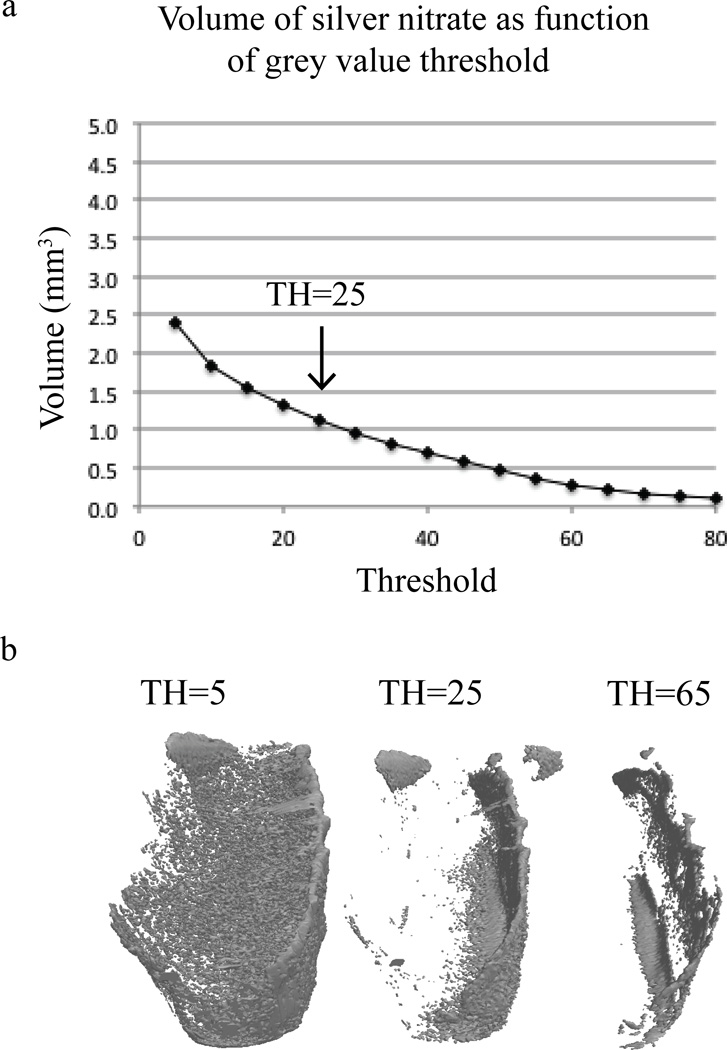
In theory, only the voxels corresponding to the silver nitrate penetrant would have non-zero grey values after image subtraction. However, the presence of noise resulted in regions with non-zero grey values that were not occupied by silver nitrate. To better quantify the silver nitrate penetration, the resulting subtracted images were further processed using SkyScan CT-analyzer Version 1.1 (Bruker microCT, Kontich, Belgium). First, a region of interest was defined to remove most of the background information. A threshold grey value was then selected to remove the remaining background and to reduce the noise for the subsequent image binarization step. The threshold value was chosen such that the amount of silver nitrate identified at the tooth-restoration interface was not altered significantly while removing the remaining background and noise elsewhere, as shown in Figs. 3a–b. The resulting binary images were visually compared with the post-treatment images to further confirm that the threshold value selected was appropriate. 3D rendering of the silver nitrate penetration was then performed, followed by calculation of its volume and the mean value for each group of specimens.
Figure 3.
a) Threshold grey value used to isolate volume of silver nitrate infiltration (indicated by the arrow) b) An example of 3D rendering of the silver nitrate with different threshold (TH) grey values.
2.4 Scanning electron microscopy (SEM)
To further confirm the presence of silver nitrate, SEM was performed using a tabletop environmental scanning electron microscope (TM-3000, Hitachi, High-Technologies Corporation, Tokyo, Japan). This equipment allowed uncoated samples to be scanned. The crown was separated from the root and several cross-sections were obtained from it using an Isomet™ diamond saw (Buehler, Lake Bluff, IL, USA). The SEM settings were: ×50 magnification, COMPO mode and an operating voltage of 15 kV. The COMPO mode gives not only topographical details but also contrast to the image due to different average atomic number composition within the sample. The higher the atomic number the brighter the image. Electron dispersive spectroscopy (EDS) was also performed to confirm the presence of silver nitrate.
2.5 Statistical analysis
A two-tailed Student’s t-test (Microsoft® Excel® 2011, version 14.2.4) was carried out to determine if there was a statistically significant difference in the mean volume of silver nitrate penetration between the two groups. The level of statistical significance was set at p <0.05.
3. RESULTS
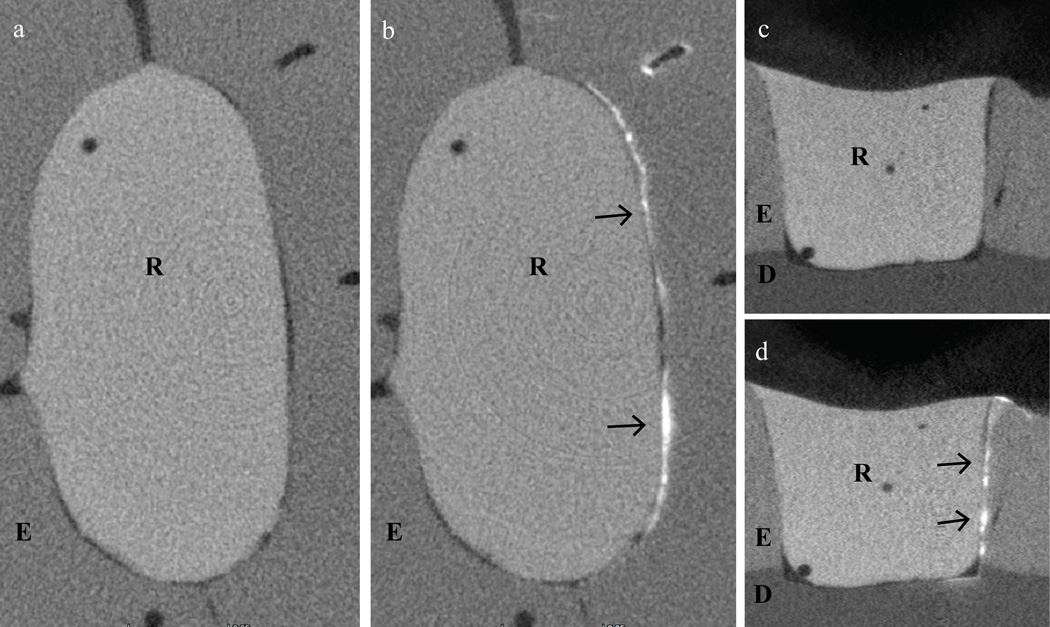
At initial examination, all samples from Group I showed silver nitrate penetration to some degree (Fig. 4). Whereas in Group II, only 2 out of the 10 restorations displayed infiltration along the interface, and preliminary inspection showed that the amount of penetration was lower than that found in Group I (Fig. 5).
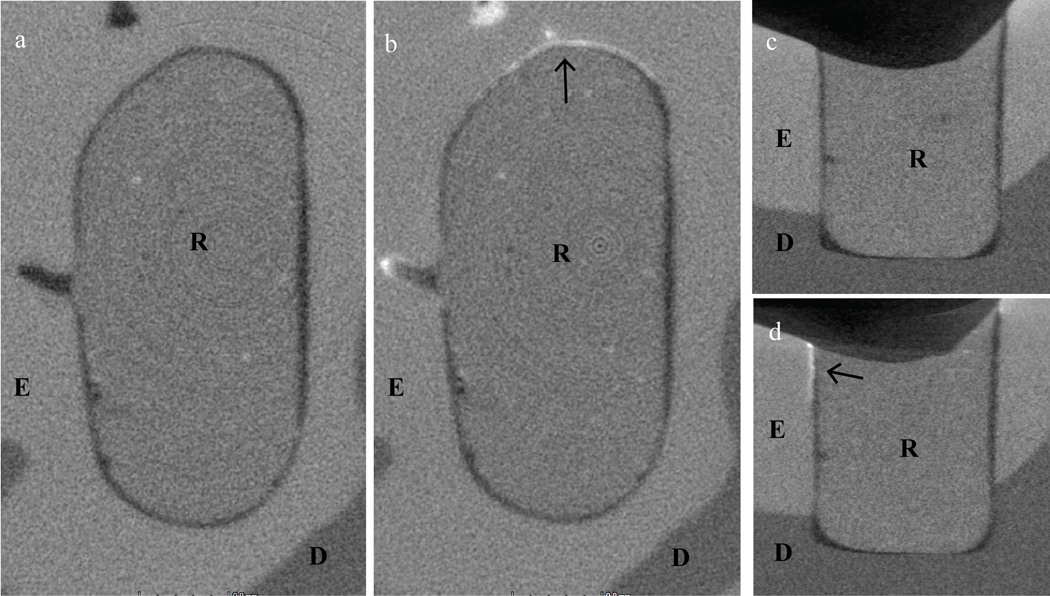
Figure 4.
a) and c) are cross-sections from the top view and front view, respectively, of a sample from Group I before treatment with silver nitrate. b) and d) show the same cross-sections after treatment with silver nitrate. The arrows indicate where traces of silver nitrate were found. R= restoration, E=enamel, D=dentin.
Figure 5.
a) and c) are cross-sections from the top view and front view, respectively, of a sample from Group II before treatment with silver nitrate. b) and d) show the same cross-sections after treatment with silver nitrate. In this case, while traces of silver nitrate were found, as indicated by the arrows, the quantity was less than that in the Group-I sample (Fig. 4). R= restoration, E=enamel, D=dentin.
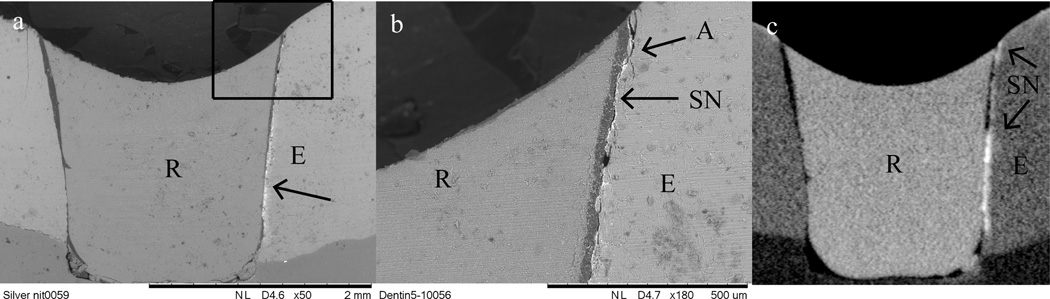
It can be seen that the silver nitrate penetration was non-uniform around the tooth-restoration interface, and tended to be on one side of the interface only. With regard to its exact position, it was found that the penetration mainly occurred between the adhesive system and the dental tissue for both materials. Figures 6a and 6b show SEM images of the sample selected from Group I, which confirmed that silver nitrate penetration had taken place between the adhesive (dark grey) and the tooth tissues (light grey). The same trace of silver nitrate can be seen in the micro-CT image of approximately the same section of the same sample in Fig. 4c, albeit at a lower resolution.
Figure 6.
a) Silver nitrate penetration (shown in white and indicated by the arrow) under SEM examination. b) A magnified view of a), showing that the infiltration and hence debonding took place between the enamel and the adhesive. c) A micro-CT image of the cross-section examined by SEM that shows the same infiltration of the penetrant. A= adhesive system, R= restoration, E= enamel, D= dentin and SN= silver nitrate.
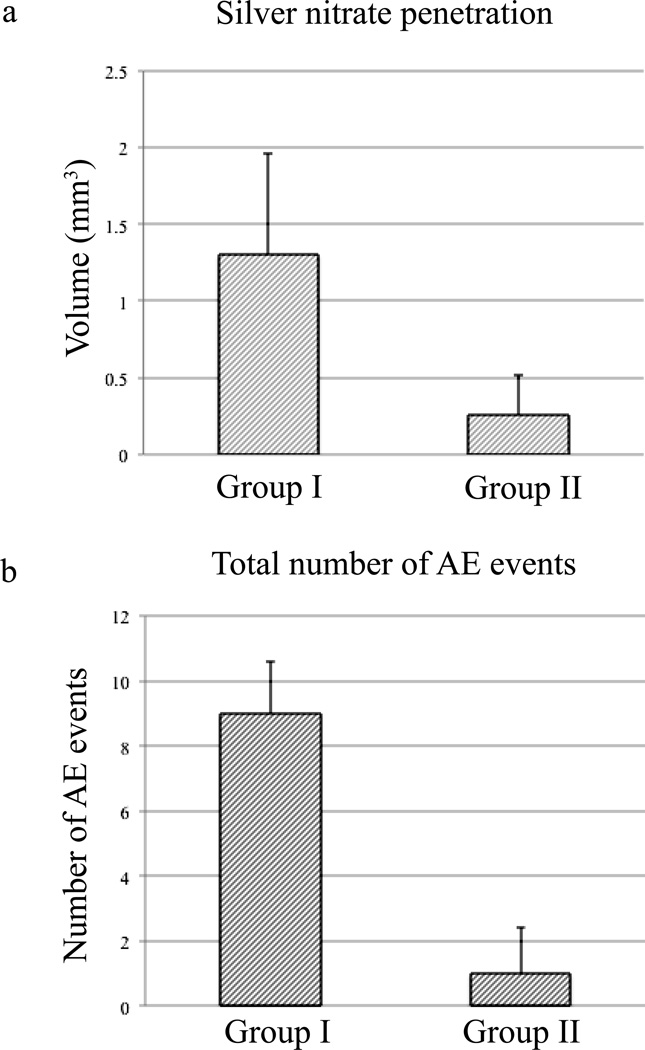
Calculation of the volume of silver nitrate penetration (Table 2) showed that the specimens prepared with the high-shrinkage composite (Group I) displayed a higher amount of silver nitrate infiltration when compared to those made with the low-shrinkage composite (Group II). The mean values for Group I and Group II were 1.3 ± 0.7 and 0.3 ± 0.3 mm3, respectively (Fig. 7a). The difference between the two groups was statistically significant (p < 0.05). Similar results can be seen in the number of AE events recorded (Fig. 7b) for specimens prepared with the same two composites [9].
Table 2.
Volume of silver nitrate penetration (mm3) along the interface in Class-I preparations restored with either a high- or low-shrinkage composite
| Sample No. | Group Ia | Group IIb |
|---|---|---|
| 1 | 1.4 | 0.0d |
| 2 | 2.0 | 0.0d |
| 3 | 1.4 | 0.0d |
| 4 | 1.9 | 0.1 |
| 5 | 0.6 | 0.4 |
| 6 | 2.6 | 0.0d |
| 7 | 0.7 | 0.0d |
| 8 | 1.0 | 0.0d |
| 9 | 0.9 | 0.0d |
| 10 | 0.7 | 0.0d |
| Mean | 1.3 (0.7)c | 0.3 (0.3)c |
Group I = Class-I preparations restored with Z100 (high-shrinkage composite)
Group II= Class-I preparations restored with LS (low-shrinkage composite)
Standard deviation
Where silver nitrate was not found visually the volume of microleakage was assumed to be 0.0 mm3
Figure 7.
a) Mean values of silver nitrate penetration along the tooth-restoration interface for Groups I and II. b) Mean number of AE events recorded for Groups I and II. Taken from Li et al. [19]. Group I are samples restored with Z100, while Group II are samples restored with LS.
4. DISCUSSION
Given that failure of composite restorations due to secondary caries is still a major concern in operative dentistry [12, 13], issues such as polymerization shrinkage of composites, interfacial gap formation and leakage continue to be important research topics. We have presented here a technique, using radiopaque dye penetration, Micro-CT and image segmentation, to quantify leakage at the tooth-restoration interface. This approach has the advantage of being non-destructive, quantitative and 3D in its analysis. Specifically, it allows the spatial distribution of the interfacial leakage along the cavity walls and floor to be visualized in 3D, which cannot be obtained easily using traditional techniques that require sectioning of the specimen. These features make this method much more comprehensive and quantitative. In contrast, traditional methods for microleakage studies can only provide limited, or even unrepresentative, information, unless multiple sections of the sample are analyzed.
The use of a radiopaque dye to highlight the defective or debonded areas is still necessary with the new technique if the low radiopacity of the adhesive systems, as was the case in this study, renders them indistinguishable from the background or the defects are too small for micro-CT to resolve.
As mentioned previously, micro-CT has been used to obtain 3D mapping of the polymerization shrinkage to predict microleakage [7]. In that study, gap formation was calculated as the distance between the delaminated composite and the wall of a polymethyl-methacrylate mold that simulated the tooth cavity. Gaps greater than 16µm were considered to be “leaking”. However, an adhesive was not used in that study. As a result, the interfacial gap formed was likely to be unrealistically large due to the lack of bonding, even though some of it could have been overcome by the shrinkage stress had an adhesive been used. A later study [8] reported that shrinkage mainly occurred at the top surface and gradually diminished with depth. However, leakage was predicted only qualitatively from the shrinkage profiles. Again, no bonding system was used in this later study. Therefore, the predicted leakage was probably overestimated.
The proposed technique, specifically the precise alignment and subsequent subtraction of images taken before and after submersion in silver nitrate, can overcome the aforementioned shortcomings, allowing the study of gap formation and leakage to be undertaken in a more realistic scenario, with all the components of a restored tooth being involved in the study.
Using image correlation and image subtraction, the volume of the silver nitrate penetration along the tooth-restoration interface could be calculated without interference from the restoration and the dental tissues. The remaining background and noise were separated from the images by setting to black the pixels with a grey value below a certain threshold during the binarization. The threshold selection was guided by observation of the original post-treatment images before image subtraction.
The results presented herein showed a significantly greater amount of dye penetration in the samples restored with Z100, a high-shrinkage composite, when compared to those restored with LS, a low-shrinkage restorative material (Fig. 7a). These data are in agreement with a previous study that used AE to quantify debonding at the tooth-restoration interface during curing of the restorations [9]. In that study, samples restored with Z100 displayed a much higher number of AE events during curing than those restored with the low-shrinkage composite LS (Fig. 7b). The current results showed that, for both groups, the infiltration mainly occurred between the bonding agent and the tooth structure. The adhesive-tooth interface therefore seemed to be the weakest part of the restorative system.
Our results also agree with those from Krifka et al. [14] in which Class-V restorations made with Filtek LS showed the lowest dye penetration before and after thermal and mechanical challenge, when compared to a group of methacrylate-based composite resins with varying viscosities. Bagis et al. [15] also found no microleakage in Class-II MOD restorations prepared with Filtek LS in comparison with restorations of nano-hybrid methacrylate based composites, made with either oblique or vertical layering techniques. However, in their study, only one cross-section per specimen was used and only the gingival aspect was assessed. Contrary to all the above results, a recent microleakage study that evaluated bucco-lingual sections of Class-V restorations in primary canines after thermo-cycling reported that LS performed better than methacrylate composite only when the adhesive system was used with acid etching. LS had the highest microleakage scores when used as indicated by the manufacturer [16].
Despite the use of incremental filling, significant leakage still occurred in the Z100 samples. It may be the case that the shrinkage stress, albeit reduced, was still high enough to cause gap formation. However, as shown by Sano et al. [17], the hybrid layer in this restorative system may contain imperfections. Their work demonstrated penetration of silver nitrate into the hybrid layer even in the absence of micro-sized interfacial gaps. The observed leakage was thought to occur through nano-sized paths and porosities within the hybrid layer or within demineralized submicron spaces that failed to be completely sealed by the adhesive. The much lower dye penetration shown in the LS group might be explained by its low polymerization shrinkage, but LS uses a two-step self-etching adhesive that is different from the total etch and rinse used for Z100. Self-etch adhesives reduce the risk of incomplete resin infiltration by being able to infiltrate the exposed collagen with adhesive up to the same depth of demineralization [18]. For this reason, some two-step self-etch adhesives have shown less nanoleakage when compared with a total etch adhesive [19, 20]. It should also be noted that the penetration of the silver nitrate into the interfacial gap might not be complete. Also, when the silver nitrate reached the dentin, it could penetrate into the tubules. Therefore, the volume of leakage does not necessarily equal to that of the interfacial imperfections or gaps formed, although they are expected to be highly correlated.
5. CONCLUSIONS
We have developed a more comprehensive method to study interfacial leakage. Using silver nitrate infiltration and image subtraction, we were able to use micro-CT to quantify leakage in 3D, overcoming previous limitations with this technique. Our results confirmed that leakage occurred mostly at the interface between the adhesive system and the tooth structure. The same technique can be used to analyze leakage in other restorations types, for example sealants and dental implants.
Highlights.
Leakage is quantified using micro-CT, AgNO3 infiltration and image segmentation.
Substantial leakage occurs in restorations with interfacial imperfection/debonding.
Leakage occurs mostly at the adhesive-tooth interface of the systems investigated.
ACKNOWLEDGMENT
We would like to acknowledge the Minnesota Supercomputer Institute (MSI), University of Minnesota, for the provision of Matlab software used for image alignment and subtraction; Dr. Robert Jones for his assistance in this study; and the National Institute of Health, USA, for their financial support through Grant 1 R01 DE021366.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
REFERENCES
- 1.De Munck J, Van Landuyt K, Peumans M, Poitevin A, Lambrechts P, Braem M, et al. A critical review of the durability of adhesion to tooth tissue: methods and results. J Dent Res. 2005;84:118–132. doi: 10.1177/154405910508400204. [DOI] [PubMed] [Google Scholar]
- 2.Hilton TJ. Can modern restorative procedures and materials reliably seal cavities? In vitro investigations. Part 1. Am J Dent. 2002;15:198–210. [PubMed] [Google Scholar]
- 3.Hilton TJ. Can modern restorative procedures and materials reliably seal cavities? In vitro investigations. Part 2. Am J Dent. 2002;15:279–289. [PubMed] [Google Scholar]
- 4.Sun J, Lin-Gibson S. X-ray microcomputed tomography for measuring polymerization shrinkage of polymeric dental composites. Dent Mater. 2008;24:228–234. doi: 10.1016/j.dental.2007.05.001. [DOI] [PubMed] [Google Scholar]
- 5.Chen X, Cuijpers V, Fan M, Frencken JE. Marginal leakage of two newer glass-ionomer-based sealant materials assessed using micro-CT. J Dent. 2010;38:731–735. doi: 10.1016/j.jdent.2010.05.018. [DOI] [PubMed] [Google Scholar]
- 6.Eden E, Topaloglu-Ak A, Cuijpers V, Frencken JE. Micro-CT for measuring marginal leakage of Class II resin composite restorations in primary molars prepared in vivo. Am J Dent. 2008;21:393–397. [PubMed] [Google Scholar]
- 7.Sun J, Eidelman N, Lin-Gibson S. 3D mapping of polymerization shrinkage using X-ray micro-computed tomography to predict microleakage. Dent Mater. 2009;25:314–320. doi: 10.1016/j.dental.2008.07.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Zeiger DN, Sun J, Schumacher GE, Lin-Gibson S. Evaluation of dental composite shrinkage and leakage in extracted teeth using X-ray microcomputed tomography. Dent Mater. 2009;25:1213–1220. doi: 10.1016/j.dental.2009.04.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Li H, Li J, Yun X, Liu X, Fok AS. Non-destructive examination of interfacial debonding using acoustic emission. Dent Mater. 2011;27:964–971. doi: 10.1016/j.dental.2011.06.002. [DOI] [PubMed] [Google Scholar]
- 10.L S, G S. Computer vision. Prentice Hall; 2001. [Google Scholar]
- 11.The MathWorks, Image Processing Toolbox User's guide [Google Scholar]
- 12.Bernardo M, Luis H, Martin MD, Leroux BG, Rue T, Leitao J, et al. Survival and reasons for failure of amalgam versus composite posterior restorations placed in a randomized clinical trial. J Am Dent Assoc. 2007;138:775–783. doi: 10.14219/jada.archive.2007.0265. [DOI] [PubMed] [Google Scholar]
- 13.Demarco FF, Correa MB, Cenci MS, Moraes RR, Opdam NJ. Longevity of posterior composite restorations: not only a matter of materials. Dent Mater. 2012;28:87–101. doi: 10.1016/j.dental.2011.09.003. [DOI] [PubMed] [Google Scholar]
- 14.Krifka S, Federlin M, Hiller KA, Schmalz G. Microleakage of silorane- and methacrylate-based class V composite restorations. Clin Oral Investig. 2012;16:1117–1124. doi: 10.1007/s00784-011-0619-7. [DOI] [PubMed] [Google Scholar]
- 15.Bagis YH, Baltacioglu IH, Kahyaogullari S. Comparing microleakage and the layering methods of silorane-based resin composite in wide Class II MOD cavities. Oper Dent. 2009;34:578–585. doi: 10.2341/08-073-LR. [DOI] [PubMed] [Google Scholar]
- 16.Poureslami HR, Sajadi F, Sharifi M, Farzin Ebrahimi S. Marginal Microleakage of Low-shrinkage Composite Silorane in Primary Teeth: An In Vitro Study. J Dent Res Dent Clin Dent Prospects. 2012;6:94–97. doi: 10.5681/joddd.2012.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Sano H, Takatsu T, Ciucchi B, Horner JA, Matthews WG, Pashley DH. Nanoleakage: leakage within the hybrid layer. Oper Dent. 1995;20:18–25. [PubMed] [Google Scholar]
- 18.Manuja N, Nagpal R, Pandit IK. Dental adhesion: mechanism, techniques and durability. J Clin Pediatr Dent. 2012;36:223–234. [PubMed] [Google Scholar]
- 19.Reis AF, Giannini M, Pereira PN. Long-term TEM analysis of the nanoleakage patterns in resin-dentin interfaces produced by different bonding strategies. Dent Mater. 2007;23:1164–1172. doi: 10.1016/j.dental.2006.10.006. [DOI] [PubMed] [Google Scholar]
- 20.Yuan Y, Shimada Y, Ichinose S, Tagami J. Qualitative analysis of adhesive interface nanoleakage using FE-SEM/EDS. Dent Mater. 2007;23:561–569. doi: 10.1016/j.dental.2006.03.015. [DOI] [PubMed] [Google Scholar]