Abstract
Solid pseudo-papillary epithelial neoplasm (SPEN) is a rare epithelial tumor of pancreas with a low malignant potential occurs most commonly in young females. We report a case of 40 years old woman presented with extensive liver metastasis from SPEN of pancreatic body for which she was operated four years ago. Due to the extensive nature of metastatic disease she was offered Transarterial chemoembolisation (TACE) using gemcitabine as chemotherapeutic agent. Short term follow up after a month of TACE with multiphase computed tomography showed > 90% resolution in the viable tumor with significant clinical improvement. TACE ensures targeted delivery of chemotherapeutic drugs in higher doses with least systemic toxicity and is more effective and safe than systemic chemotherapy. TACE with gemcitabine was found to be very effective in our patient with numerous liver metastasis.
Keywords: Solid pseudopapillary epithelial neoplasm, Liver metastases, Transarterial chemoembolization, Gemcitabine
Core tip: Solid pseudo-papillary epithelial neoplasm (SPEN) is a rare epithelial tumor of pancreas which is generally less aggressive and patients rarely present with liver metastasis. Our patient is a middle aged lady presented with extensive liver metastasis several years after the removal of primary tumor. Transarterial chemoembolisation (TACE) is a recognized treatment modality for inoperable hepatocellular carcinoma and metastasis from certain tumors. However, this novel technique is reported to be used only once for a patient with SPEN metastasis. In our patient, we performed TACE with gemcitabine as chemotherapeutic agent with encouraging short term results.
INTRODUCTION
Solid pseudo-papillary epithelial neoplasm (SPEN) is a rare epithelial tumor of pancreas with a low malignant potential[1]. After the first description of the entity in 1959, more cases are reportedinliterature in the last decades[2]. Local aggressiveness and metastasisarereported in less than 15% cases[3]. Surgical resection is optimal in localized disease. Surgery is also frequently offered in locally aggressive tumors and oligo-metastatic lesions in liver because of indolent nature of the disease and younger ages of presentation. There are sporadic reports in literature discussing chemo-radiotherapy in disseminated disease[4-7]. We present a case of multiple hepatic metastasis from SPEN, developing four years after primary treatment of pancreatic lesion, treated with transarterial chemoembolization (TACE).
CASE REPORT
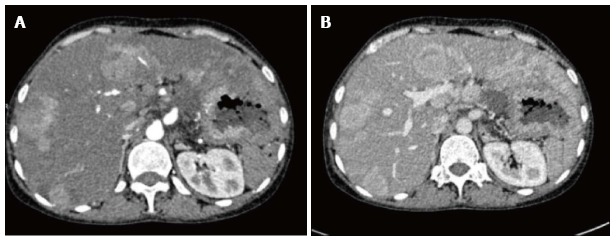
A 40-year-old woman presented to the gastrointestinal surgery clinic with abdominal pain for one month duration. Clinical examination was unremarkable except for hepatomegaly. She had a past history of surgery (Distal pancreatectomy) for pancreatic tumor (Figure 1) four years ago which was histopathologically proven as SPEN. Presently, she was evaluated with ultrasonography which showed multiple hypoechoic focal lesions in both lobes of liver with fatty infiltration (Figure 2). Subsequently multiphase contrast enhanced computed tomography (CT) was done, which showed multiple arterial enhancing lesions in both lobes of liver with no significant washout in venous and delayed phases (Figure 3). No capsule was seen. There was no recurrent or residual lesion at the primary site. Fine needle aspiration cytology of the new liver lesions was suggestive of metastases from pancreatic SPEN.
Figure 1.

Axial computed tomography scan shows a well defined heterogeneous mass lesion arising from body and tail of pancreas with marked central necrosis which was proven as solid pseudo-papillary epithelial neoplasm after surgery.
Figure 2.

Ultrasonography image showing multiple well defined hypoechoic lesions in the background of fatty liver, suggestive of metastases.
Figure 3.
Arterial (A) and venous (B) phases of multiphase contrast enhanced axial computed tomography images showing multiple arterial enhancing focal lesions in liver with no significant wash out in venous phase.
Due to the presence of numerous liver metastasis involving both lobes, chemotherapy was planned. After a detailed discussion with the gastroenterologist, gastrointestinal surgeons and oncologists it was decided to treat the patient with TACE using gemcitabine as the chemotherapeutic drug. Through the transfemoral route, both hepatic arteries were catheterized selectively and the drug was injected. Gemcitabine (dose 1 g) was mixed with 20 mL of lipiodol (Lipiodol ultra-fluid, Guerbet, United States) and saline was mixed to make a solution of about 80 mL. About 40 mL each was injected into right and left hepatic arteries separately followed by embolisation of the arteries with gelfoam slurry. Post embolization images showed significant retention of lipiodol within the lesions (Figure 4). Patient did not experience any procedure related complications. The patient was subsequently followed up with CT scan after one month of TACE. It showed significant (> 90%) reduction in the size and enhancement of the lesions suggesting marked necrosis and complete response (Figure 5). The patient is currently (after 6 mo of TACE) asymptomatic and is on regular follow up.
Figure 4.
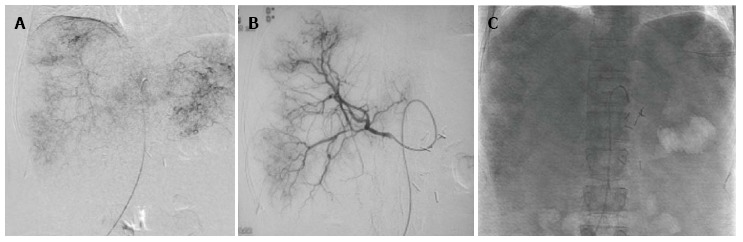
DSA: (A) Common hepatic artery and (B) right hepatic artery angiography showing multiple tumor blush in the liver, (C) post embolisation spot image showing lipiodol retention within the lesions.
Figure 5.
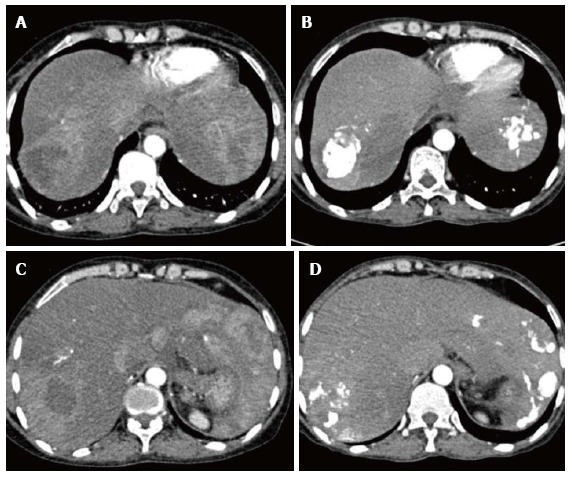
Pre and Post transarterial chemoembolization. A and C showing arterial enhancing lesions in pre transarterial chemoembolisation (TACE) images; B and D are corresponding post TACE images showing lipiodol retention with significant reduction in enhancing component of the lesions.
DISCUSSION
SPEN accounts for less than 2% of exocrine tumors of pancreas with a low malignant potential and has high incidence in young females. Metastasis from SPEN is seen in 10%-15% of cases with liver being the commonest target organ[2]. Although the mean interval for liver metastasis from initial diagnosis of primary tumor is 8.5 years, it is reported as late as 15.8 years after the resection of primary neoplasm[8,9]. Most of the patients of SPEN present with abdominal pain and lump. Incidental detection of cases during imaging for other purposes is also not infrequent. Ultrasonography, CT scan and Magnetic Resonance Imaging are the imaging modalities used in assessing the primary lesion and in staging the tumor. These tumors have solid and cystic areas on imaging with frequent detection of haemorrhage.
Localised SPEN is usually managed by surgical resection. Solitary and resectable metastatic lesions are also managed by surgery. Patients with aggressive tumors and multiple metastasis are offered chemotherapy or radiotherapy. Although no guidelines could be found in literature regarding chemotherapy for metastatic SPEN, the various drugs used are mitomycin, cisplatin, gemcitabine and 5-fluorouracil in different combinations[4,5]. Most of the reports have managed liver metastases with systemic chemotherapy. Hormone therapy has also been tried in patients with tumors positive for estrogen-progesterone receptors with varying results[7].
TACE is an accepted method of palliative chemotherapy in unresectable primary and secondary malignant neoplasms of liver. Apart from hepatic metastasis from colorectal malignancies, it also has been found useful in metastatic pancreatic cancers[10]. TACE is preferred over systemic chemotherapy due to the fact that the preferential hepatic arterial supply of the metastatic lesions allow delivery of higher doses of chemotherapeutic drugs, ensuring targeted delivery of drug in optimal doses with less chances of systemic toxicity. Administration of chemotherapeutic drugs with lipiodol during TACE allows optimal retention of agents in the tumor, increasing the contact period. Degree of lipiodol retention is used as an indicator of treatment adequacy on follow up. Gelfoam embolisation of the feeding vessel causes ischemia in tumor cells increasing the efficacy of chemotherapy apart from facilitating the contact period of drug with the tumor. Gemcitabine is an established chemotherapeutic agent used for palliation in extensive disease of pancreatic adenocarcinoma. Gemcitabine is often used in combination with 5-fluorouracil in advanced pancreatic malignancies[10].
Only one case report of TACE in the management of liver metastasis from pancreatic SPEN was found in English literature by Matsuda et al[6]. They performed intraarterial chemoinfusion of doxorubicin followed by gelfoam embolization of only right hepatic artery. On follow up, there was 28% and 15% shrinkage in the size of the lesions in right lobe and left lobe respectively, signifying the role of gel foam embolization. In our case, TACE with gemcitabine and lipiodol followed by gelfoam embolization gave optimum short term results.
In conclusion, liver metastasis is unusual in pancreatic SPEN. Although solitary metastasis is managed by surgery, extensive liver lesions require palliative chemotherapy. TACE ensures targeted delivery of chemotherapeutic drugs in higher doses with least systemic toxicity and is more effective and safe than systemic chemotherapy. TACE with gemcitabine was found to be very effective in our patient with numerous liver metastasis. However further large and long term studies are required to establish this technique in liver metastasis from SPEN.
COMMENTS
Case characteristics
Middle aged lady with history of distal pancreatectomy for solid pseudo-papillary epithelial neoplasm (SPEN) four years ago, presented with abdominal pain for one month.
Clinical diagnosis
On physical examination she had tender hepatomegaly.
Differential diagnosis
Malignant tumors (metastatic tumors, hepatocelluar carcinoma), benign neoplasms (focal nodular hyperplasia, hemangioma and adenoma), and abscess.
Laboratory diagnosis
Lab investigations revealed normal findings.
Imaging diagnosis
USG and enhanced spiral computerized tomography showed multiple focal liver lesions.
Pathological diagnosis
FNAC from liver lesions suggested liver metastasis from pancreatic SPEN.
Treatment
Transarterial chemoembolisation (TACE) using gemcitabine as chemotherapeutic agent.
Related reports
Only one case report of TACE in the management of liver metastasis from pancreatic SPEN was found in English literature by Matsuda et al.
Term explanation
SPEN is a rare epithelial tumor of pancreas with a low malignant potential.
Experiences and lessons
TACE with gemcitabine is found to be very effective in patients with inoperable liver metastasis from SPEN.
Peer-review
Well written case report.
Footnotes
P- Reviewer: Bester L, Bhosale P, Smart NJ S- Editor: Ji FF L- Editor: A E- Editor: Lu YJ
Ethics approval: The study was reviewed and approved.
Informed consent: This is to state that all the details revealing the identity of the patient are omitted from the manuscript. Informed consent was waived off because of the retrospective nature of the case report.
Conflict-of-interest: None.
Open-Access: This article is an open-access article which was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution Non Commercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: http://creativecommons.org/licenses/by-nc/4.0/
Peer-review started: November 16, 2014
First decision: December 26, 2014
Article in press: February 12, 2015
References
- 1.Yu PF, Hu ZH, Wang XB, Guo JM, Cheng XD, Zhang YL, Xu Q. Solid pseudopapillary tumor of the pancreas: a review of 553 cases in Chinese literature. World J Gastroenterol. 2010;16:1209–1214. doi: 10.3748/wjg.v16.i10.1209. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Papavramidis T, Papavramidis S. Solid pseudopapillary tumors of the pancreas: review of 718 patients reported in English literature. J Am Coll Surg. 2005;200:965–972. doi: 10.1016/j.jamcollsurg.2005.02.011. [DOI] [PubMed] [Google Scholar]
- 3.Mao C, Guvendi M, Domenico DR, Kim K, Thomford NR, Howard JM. Papillary cystic and solid tumors of the pancreas: a pancreatic embryonic tumor? Studies of three cases and cumulative review of the world’s literature. Surgery. 1995;118:821–828. doi: 10.1016/s0039-6060(05)80271-5. [DOI] [PubMed] [Google Scholar]
- 4.Strauss JF, Hirsch VJ, Rubey CN, Pollock M. Resection of a solid and papillary epithelial neoplasm of the pancreas following treatment with cis-platinum and 5-fluorouracil: a case report. Med Pediatr Oncol. 1993;21:365–367. doi: 10.1002/mpo.2950210511. [DOI] [PubMed] [Google Scholar]
- 5.Das G, Bhuyan C, Das BK, Sharma JD, Saikia BJ, Purkystha J. Spleen-preserving distal pancreatectomy following neoadjuvant chemotherapy for papillary solid and cystic neoplasm of pancreas. Indian J Gastroenterol Off J Indian Soc Gastroenterol. 2004;23:188–189. [PubMed] [Google Scholar]
- 6.Matsuda Y, Imai Y, Kawata S, Nishikawa M, Miyoshi S, Saito R, Minami Y, Tarui S. Papillary-cystic neoplasm of the pancreas with multiple hepatic metastases: a case report. Gastroenterol Jpn. 1987;22:379–384. doi: 10.1007/BF02774265. [DOI] [PubMed] [Google Scholar]
- 7.Sclafani LM, Reuter VE, Coit DG, Brennan MF. The malignant nature of papillary and cystic neoplasm of the pancreas. Cancer. 1991;68:153–158. doi: 10.1002/1097-0142(19910701)68:1<153::aid-cncr2820680128>3.0.co;2-n. [DOI] [PubMed] [Google Scholar]
- 8.Vollmer CM, Dixon E, Grant DR. Management of a solid pseudopapillary tumor of the pancreas with liver metastases. HPB (Oxford) 2003;5:264–267. doi: 10.1080/13651820310001397. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Gomez P, Yorke R, Ayala AG, Ro JY. Solid-pseudopapillary neoplasm of pancreas with long delayed liver metastasis. Ann Diagn Pathol. 2012;16:380–384. doi: 10.1016/j.anndiagpath.2011.02.008. [DOI] [PubMed] [Google Scholar]
- 10.Tajima H, Kitagawa H, Tsukada T, Okamoto K, Nakanuma SI, Sakai S, Makino I, Furukawa H, Hayashi H, Oyama K, et al. Hepatic arterial infusion chemotherapy with gemcitabine and 5-fluorouracil or oral S-1 improves the prognosis of patients with postoperative liver metastases from pancreatic cancer. Mol Clin Oncol. 2013;1:869–874. doi: 10.3892/mco.2013.152. [DOI] [PMC free article] [PubMed] [Google Scholar]


