Abstract
Context:
Hormonal and mechanical factors make obstetric patients need strict dose calculations of local anesthetics intrathecally for spinal anesthesia. Any greater dose of local anesthetics can cause hemodynamic instability, maternal morbidity and any lesser dose can produce inadequate block. Hence, we hypothesized in our study that by using low dose of bupivacaine with fentanyl can maintain stable hemodynamics and provide better analgesia.
Aim:
The aim was to compare the hemodynamics and duration of analgesia using a low dose (7.5 mg) bupivacaine fentanyl mixture to a conventional dose (10 mg) of hyperbaric bupivacaine for cesarean section.
Settings and Design:
Double-blinded, randomized, controlled prospective study was conducted at a tertiary academic hospital from 2008 to 2011.
Materials and Methods:
Fifty singleton parturient, scheduled for elective caesarean section were randomly allocated into two groups. Study group (group-S) received a combination of 25 μg fentanyl and 7.5 mg of hyperbaric bupivacaine, whereas the control group (group-C) received 10 mg of hyperbaric bupivacaine. Maternal hemodynamics, sensory and motor block, duration of analgesia and the Apgar score of the newborn were compared between the groups.
Statistical Analysis Used:
Observational descriptive statistics, statistical package for social sciences (SPSS Inc. Released 2006, SPSS for Windows, Version 15.0. Chicago), paired t-test was used as applicable.
Results:
The blood pressure significantly decreased with >25% fall from the baseline in group-C (98.76 ± 8.36) than in group-S (117.32 ± 12.21) with P < 0.001. The duration of effective analgesia was significantly prolonged in the study group than in the control group (P < 0.001).
Conclusion:
The combination of low dose bupivacaine and fentanyl in comparison to bupivacaine alone is hemodynamically stable and prolonged duration of analgesia in caesarean section.
Keywords: Anesthesia spinal, local, anesthetics, apgar score, cesarean section, fentanyl
INTRODUCTION
Spinal anesthesia is the most common method of regional block in caesarean section.[1] Many physiological and anatomical changes during pregnancy affect spinal anesthesia. The hormonal and mechanical factors make pregnant women require less local anesthetic than nonpregnant women to attain the same level of spinal anesthesia.[2] They stand at a greater risk of toxicity to local anesthetics due to the increased penetration through tissue membranes, decreased plasma protein binding and progesterone enhanced cardiotoxicity.[3] Any dose alterations can cause hemodynamic instability leading to increased maternal and neonatal morbidity and mortality.
Studies on hemodynamic alterations in spinal anesthesia show that the hypotension after spinal anesthesia is caused due the enhanced sympathetic segmental block due to higher doses of local anesthetic.[4] Among the local anesthetics hyperbaric bupivacaine is the preferred local anesthetic. The unique characteristics of this drug are the highest potency, slow onset of action (5-8 min) and longer duration. Further, studies have shown that the combination of isobaric bupivacaine and fentanyl produce less hypotension.[5] Studies have also shown that by adding intrathecal opioids to bupivacaine in caesarean section enhance the quality of surgical analgesia.[6]
Among the synthetic opioids, fentanyl is favorable due to greater potency, faster onset of action and rapid redistribution with an associated decrease in the plasma concentration of the drug[7] and thus enhancing the early postoperative analgesia.[8]
However, these studies have used varied dosage and baricity of bupivacaine and have not defined the minimum dose required to avoid hypotension without affecting surgical anesthesia. Hence, we conducted the present study to hypothesize that the low dose of 7.5 mg of hyperbaric (0.5%) bupivacaine combined with 25 μg of fentanyl produce better analgesia and stable hemodynamics than the conventional dose of 10 mg of (0.5%) hyperbaric bupivcaine.
MATERIALS AND METHODS
This study was conducted from 2008 to 2011 as a prospective randomized double-blinded, controlled study at a single tertiary academic hospital on 50 singleton patients between the age of 18 and 30 years of American Society of Anesthesiologists (ASA) physical status[9] I and II scheduled for elective caesarean section. The study design was approved by the institutional ethics committee prior to data collection and written informed consent was taken from all the patients. Patients with preexisting hypertension or pregnancy induced hypertension requiring treatment, those with cardiac/renal or other end-organ disease, patients in active labor, placenta previa and those with contraindication to neuraxial block were excluded from the study. Obese patients and patients with extreme height (<140 cm or >180 cm) were also excluded from the study.
Before proceeding with the spinal anesthesia fasting status of patients was confirmed, and antacid prophylaxis was given. The Boyle anesthesia machine was checked, appropriate sized endotracheal tubes, two working laryngoscopes, a working suction apparatus and emergency drugs along with mephentermine and naloxone were kept ready. Intravenous access was secured with a large bore catheter and ringers lactate infusion was started. Standard monitors such as electrocardiography, Pulse oximetry and noninvasive blood pressure cuff were applied.
Baseline systolic, diastolic blood pressure (DBP) and heart rate readings were taken in the supine position with a wedge under the right buttock. A two operator technique was employed to maintain blinding. Patients were allocated into two groups of 25 patients each by computer-generated random allocation into a study group (group S) and a control group (group C). Study group received a total volume of 2 ml with a combination of 25 μg fentanyl and 7.5 mg of (0.5%) hyperbaric bupivacaine, whereas group-C also received 2 ml but with 10 mg of (0.5%) hyperbaric bupivacaine. The enrolling investigator prepared the intrathecal solution and subsequently had no role in patient's assessment.
Under aseptic conditions, lumbar puncture was performed with 25 gauge spinal needle at the level of the L3-4 interspace. After the free flow of cerebro-spinal fluid the specified drug in each group was injected slowly over 20 s, with the orifice of the spinal needle pointing cephalad. Patients were positioned immediately in supine position. The wedge was placed under patient's right buttock to avoid the supine hypotension syndrome. Oxygen was supplemented by Hudson's mask. An independent investigator blinded to anesthetic technique evaluated the effects.
Systolic and DBP and maternal heart rate were recorded every 2 min for the first 30 min and thereafter for every 5 min intraoperatively. A decrease of systolic blood pressure <95 mmHg or decrease >25% from baseline was considered as hypotension and treated with 3 mg-5 mg of mephenteramine. Vasopressor requirements were noted. Sensory level of the block was assessed by loss of cold sensation bilaterally at 2 min intervals and confirmed by a pinprick method. All patients were evaluated for quality of sensory block on a descriptive scale (good, satisfactory, poor).
Degree of motor block was assessed by modified Bromage scale as:
Free movement of legs and feet;
Just able to flex knees with free movement of feet;
Unable to flex knees, but with free movement of feet;
unable to move legs and feet.
An intraoperative pain assessment was done using visual analog scale (VAS) (0-10 cm where 0 = no pain and 10 = worst pain ever felt). Postoperative pain was also assessed using a VAS scale. Duration of effective analgesia was taken from the time of intrathecal injection to a VAS score ≥4. Side-effects such as nausea, vomiting, pruritus and shivering were noted. Duration for two segment regressions of the sensory blockade was noted, Apgar score of newborn was recorded at 1 min and 5 min.
The statistical power analysis suggested that a sample size of 25patients/group was required to achieve a power of 80% and a level significance of 0.001 to be able to detect a difference of analgesia of 50 min between the groups. Interpretation of the data was carried out, and analyzed using Microsoft excel and by the software Statistical Package for Social Sciences SPSS Inc. Released 2006, (SPSS for Windows, Version 15.0. Chicago).
Data is represented as mean ± standard deviation for continuous data. The two groups were compared using analysis of variance to compare the demographic data and hemodynamic parameters. The proportion of adverse effects was compared using Chi-square test and level of analgesia was compared with the help of VAS with 0 = no pain and 10 = worst pain ever. P value was assessed by paired t-test and P < 0.001 was considered as statistically significant.
RESULTS
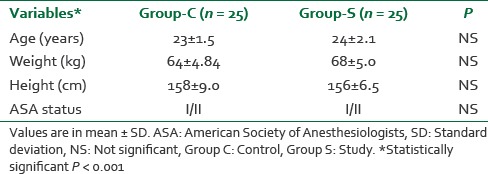
The age, weight, height, ASA physical status were comparable in both the groups and statistically insignificant as shown in Table 1.
Table 1.
Demographic characteristics of two groups
There were no significant changes in the blood pressure in both the groups till 3 min after spinal block. However, there was a fall in blood pressure in both the groups at 3 min and 5 min, but the fall in the blood pressure in the control group was >25% from the baseline which was statistically significant with P < 0.001 [Figures 1 and 2]. The heart rate also decreased from baseline in both the groups after 3 min and 5 min of giving spinal anesthesia, but the difference between the groups was not statistically significant with P > 0.001 [Table 2].
Figure 1.
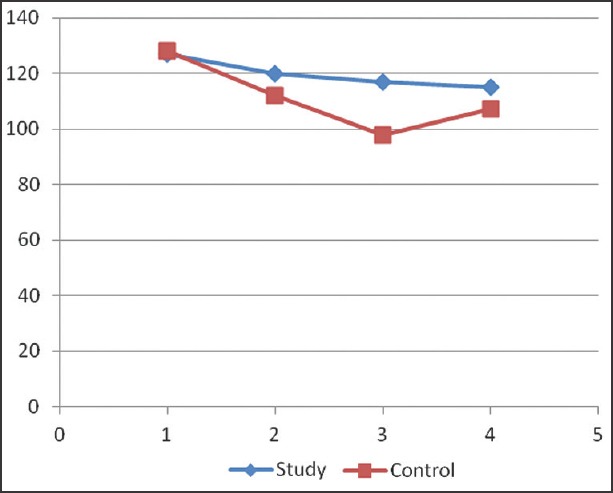
Systolic blood pressure (mmHg) at different time intervals. SBP: Systolic blood pressure
Figure 2.
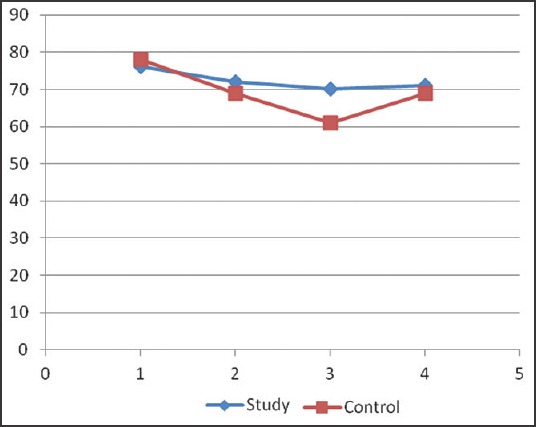
Diastolic blood pressure changes at different time intervals. DBP: Diastolic blood pressure
Table 2.
Hemodynamic and analgesic characteristics
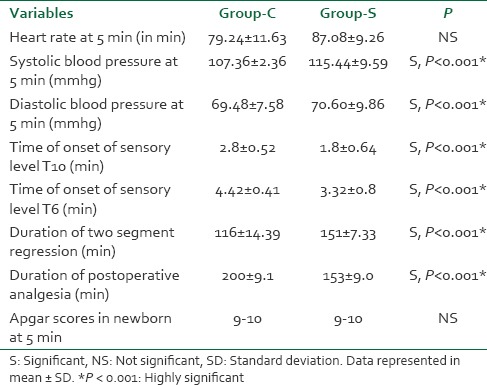
The time required for the onset of sensory block till T10 dermatome and the target sensory block of T6 dermatome was significantly faster in group S (3.32 min ± 0.8 min) than in group C (4.42 min ± 0.41 min) with (P < 0.001) [Figure 3]. However, there was no significant difference between both the groups in the quality of surgical anesthesia.
Figure 3.
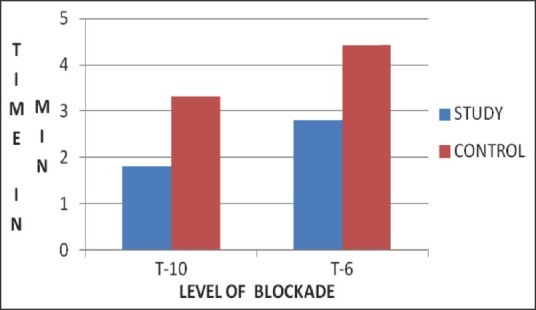
Time of onset of sensory block in minutes
The duration of postoperative analgesia was significantly prolonged in the study group (200 ± 9.1) than in the control group (153 ± 9.0) with P < 0.001. The time for first rescue analgesic dose was prolonged in the study group and was statistically significant [Table 2].
Quality of sensory blockade was good referring to no requirement of any analgesic support intraoperatively in both the groups. Quality of motor blockade assessed by bromage scale showed adequate muscle relaxation in both the groups. The proportion of adverse effects in intraoperative and early postoperative period, including nausea, vomiting, fetal bradycardia and shivering were not significant (NS) in both the groups. However, one patient from the study group complained of mild pruritus later in the postoperative period with no significant increase in the next 24 h. There was no difference in neonatal Apgar scores in both the groups at 1 min and 5 min after birth.
DISCUSSION
Spinal anesthesia is the preferred method for elective caesarean section as being simple to perform, economical and producing rapid onset of anesthesia with complete muscle relaxation. It carries high efficiency, involves less drug doses, minimal neonatal depression and lesser incidences of aspiration pneumonitis. However, it also produces a fixed duration of anesthesia, lesser control of block height, postdural puncture headache and hypotension.[10,11] Subsequently, hypotension is known to result in maternal morbidity, nausea, vomiting, dizziness and can also directly influence the neonate well-being by reducing uteroplacental blood flow.[12] The link between the extent of sympathetic block and the incidence of hypotension has led to numerous attempts at reducing the dose of local anesthetic and also the addition of opioids due to their synergistic action with local anesthetics on the sensory block without increasing sympathetic block for cesarean section.[13]
Various authors have used different dosages of local anesthetics and the volume required for spinal anesthesia in caesarean delivery. Nagata et al.,[14] have reported that 8 mg hyperbaric bupivacaine is preferable to 10 mg in spinal anesthesia for cesarean section to obtain adequate analgesia and avoid maternal hypotension. In Ben David study, they used 5 mg of isobaric bupivacaine intrathecally with 25 μg of fentanyl, but there were a number of patients who expressed brief and moderate intraoperative pain which was unacceptable. Subedi et al.,[15] observed that the relatively low dose of bupivacaine use restricted spinal block segments and thus the extent of sympathetic block, thus improving the safety margin of hemodynamic effects seen after spinal anesthesia. Hence, in our study, we were interested to assess the efficacy of the combination of low-dose (7.5 mg) of (0.5%) hyperbaric bupivacaine and 25 μg of fentanyl in spinal anesthesia. Patients scheduled for caesarean section were chosen for the study because it is well known that they show visceral discomfort and pain under spinal anesthesia.[16]
The aim of our study was to assess the hemodynamics, duration of effective analgesia with the combination of fentanyl and low dose hyperbaric bupivacaine. We observed that the systolic and DBPs were decreased significantly (P < 0.001) after 3 min and 5 min of spinal anesthesia in the control group when compared to the study group, mostly due to more sympathetic blockade by higher doses of bupivacaine in the control group. Similar findings were observed by Bogra et al.,[17] and also by Seyedhejazi and Madarek[18] wherein they studied by using 8 mg of bupivacaine and 10 μg of fentanyl for spinal anesthesia in caesarean section.
In our study, we observed that the time required for the onset of sensory blockade up to T6 was faster in the group-S than in the group-C and is statistically significant with P < 0.001, which corroborate with the study of Singh et al., However, it differs from the observations of Randall's et al.,[19] which states that the onset of sensory block to T6 gets faster with increasing bupivacaine dose. The complete motor block was achieved in 90-100% of patients in our study, this is in accordance with the results of Pedersen et al.,[20] and Choi et al.[21]
Quality of sensory blockade was good as there was no analgesic supplementation required in study group even when the uterus was exteriorized and to the pulling of fallopian tubes, this may be due to the addition of opioid like fentanyl which blocks the visceral pain, but the difference between the groups was NS.
The quality of analgesia which was assessed by VAS was excellent in the study group, similar observations were made by Choi et al., Biswas. The duration of effective analgesia was significantly prolonged with P < 0.001 in the study group, which also correlates with the study done by Ngiam and Chong[22] who observed that the duration of effective analgesia was significantly prolonged with the addition of fentanyl to hyperbaric bupivacaine. The time of the first request for analgesics was significantly delayed, which strongly suggest a synergism of action between intrathecal fentanyl and local anesthetics. The duration of two segment regression of sensory blockade was prolonged in the study group than in the control group, which was statically significant (P < 0.001) and concurs with the study made by Idowu et al.[23]
Further, in the group-S, one patient complained of mild pruritus, maybe because of side effect of fentanyl, but the etiology of it was not ascertained. Similar findings were observed by Cowan et al.,[24] but the study by Jashri et al., observed no incidence of pruritus. No patients complained of nausea and vomiting may be due to reduction of dose of bupivacaine from 10 mg to 7.5 mg causing less hypotension in the study group. Negligible incidences of shivering or respiratory depression was observed in both the groups, which were similar to the findings of Kang et al.[25]
In our study, none of the newborn babies had 5 min Apgar score <7. Similar observations were made by Belzarena,[26] Biswas, indicating that the dose of fentanyl used may not have a significant effect on the newborn. By reducing the doses of bupivacaine from 10 mg to 7.5 mg and the addition of fentanyl, we have been able to decrease the incidence of episodes of low blood pressure and subsequently poor neonatal outcome.
CONCLUSION
Based on the present clinical comparative study, we conclude that the addition of 25 μg of fentanyl to 7.5 mg of hyperbaric bupivacaine in spinal anesthesia for elective cesarean section shows faster onset of sensory block with better hemodynamic stability and significantly prolong postoperative analgesia than hyperbaric bupivacaine alone.
ACKNOWLEDGMENT
We are thankful to the Department of Obstetrics and Gynecology of Gandhi Hospital for their support. To the patients and their family members of Gandhi Hospital for consenting to the study.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Sachan P, Kumar N, Sharma J. Intrathecal clonidine with hyperbaric bupivacaine administered as a mixture and sequentially in caesarean section: A randomised controlled study. Indian J Anaesth. 2014;58:287–92. doi: 10.4103/0019-5049.135039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.McCrae AF, Wildsmith JA. Prevention and treatment of hypotension during central neural block. Br J Anaesth. 1993;70:672–80. doi: 10.1093/bja/70.6.672. [DOI] [PubMed] [Google Scholar]
- 3.Hug CC Jr, Murphy MR. Tissue redistribution of fentanyl and termination of its effects in rats. Anesthesiology. 1981;55:369–75. doi: 10.1097/00000542-198110000-00006. [DOI] [PubMed] [Google Scholar]
- 4.Jadon A. Complications of regional and general anesthesia in obstetric practice. Indian J Anaesth. 2010;54:415–20. doi: 10.4103/0019-5049.71039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Moller RA, Covino BG. Effect of progesterone on the cardiac electrophysiologic alterations produced by ropivacaine and bupivacaine. Anesthesiology. 1992;77:735–41. doi: 10.1097/00000542-199210000-00018. [DOI] [PubMed] [Google Scholar]
- 6.Akkamahadevi P, Srinivas H, Siddesh A, Kadli N. Comparision of efficacy of sufentanil and fentanyl with low-concentration bupivacaine for combined spinal epidural labour analgesia. Indian J Anaesth. 2012;56:365–9. doi: 10.4103/0019-5049.100819. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Ben-David B, Solomon E, Levin H, Admoni H, Goldik Z. Intrathecal fentanyl with small-dose dilute bupivacaine: Better anesthesia without prolonging recovery. Anesth Analg. 1997;85:560–5. doi: 10.1097/00000539-199709000-00014. [DOI] [PubMed] [Google Scholar]
- 8.Biswas BN, Rudra A, Bose BK. Intrathecal fentanyl with hyperbaric bupivacaine improves analgesia during caesarean delivery and in early postoperative period. Indian J Anaesth. 2002;46:469. [Google Scholar]
- 9.Daabiss M. American society of anaesthesiologists physical status classification. Indian J Anaesth. 2011;55:111–5. doi: 10.4103/0019-5049.79879. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Rout CC, Rocke DA, Levin J, Gouws E, Reddy D. A reevaluation of the role of crystalloid preload in the prevention of hypotension associated with spinal anesthesia for elective cesarean section. Anesthesiology. 1993;79:262–9. doi: 10.1097/00000542-199308000-00011. [DOI] [PubMed] [Google Scholar]
- 11.Caplan RA, Ward RJ, Posner K, Cheney FW. Unexpected cardiac arrest during spinal anesthesia: A closed claims analysis of predisposing factors. Anesthesiology. 1988;68:5–11. doi: 10.1097/00000542-198801000-00003. [DOI] [PubMed] [Google Scholar]
- 12.De Santiago J. The effects of the pregnant uterus on the extradural venous plexus in the supine and lateral positions, as determined by magnetic resonance imaging. Br J Anaesth. 1997;78:317. doi: 10.1093/bja/78.3.317. [DOI] [PubMed] [Google Scholar]
- 13.Kaur M, Katyal S, Kathuria S, Singh P. A comparative evaluation of intrathecal bupivacaine alone, sufentanil or butorphanol in combination with bupivacaine for endoscopic urological surgery. Saudi J Anaesth. 2011;5:202–7. doi: 10.4103/1658-354X.82804. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Nagata E, Yoshimine K, Minoda Y, Kawaguchi Y, Sakamoto M, Takehara A. Comparison of 8 mg and 10 mg hyperbaric bupivacaine during spinal anesthesia for cesarean section in Japanese parturients. Masui. 2004;53:131–6. [PubMed] [Google Scholar]
- 15.Subedi A, Tripathi M, Bhattarai BK, Gupta PK, Pokharel K, Regmi MC. The effect of height and weight adjusted dose of intrathecal hyperbaric bupivacaine for elective caesarean section. JNMA J Nepal Med Assoc. 2011;51:1–6. [PubMed] [Google Scholar]
- 16.Zahir J, Syed S, Jabeen N, Anjum Q, Rehman SU. Maternal and neonatal outcome after spinal versus general anesthesia for caesarean delivery. Ann Pak Inst Med Sci. 2011;7:115–8. [Google Scholar]
- 17.Bogra J, Arora N, Srivastava P. Synergistic effect of intrathecal fentanyl and bupivacaine in spinal anesthesia for cesarean section. BMC Anesthesiol. 2005;5:5. doi: 10.1186/1471-2253-5-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Seyedhejazi M, Madarek E. Effect of small dose bupivaciane-fentanyl in spinal anesthesia on hemodynamic nausea and vomiting in caesarean section. Pak J Med Sci. 2007;23:747–50. [Google Scholar]
- 19.Randalls B, Broadway JW, Browne DA, Morgan BM. Comparison of four subarachnoid solutions in a needle-through-needle technique for elective caesarean section. Br J Anaesth. 1991;66:314–8. doi: 10.1093/bja/66.3.314. [DOI] [PubMed] [Google Scholar]
- 20.Pedersen H, Santos AC, Steinberg ES, Schapiro HM, Harmon TW, Finster M. Incidence of visceral pain during cesarean section: The effect of varying doses of spinal bupivacaine. Anesth Analg. 1989;69:46–9. [PubMed] [Google Scholar]
- 21.Choi DH, Ahn HJ, Kim MH. Bupivacaine-sparing effect of fentanyl in spinal anesthesia for cesarean delivery. Reg Anesth Pain Med. 2000;25:240–5. doi: 10.1016/s1098-7339(00)90005-1. [DOI] [PubMed] [Google Scholar]
- 22.Ngiam SK, Chong JL. The addition of intrathecal sufentanil and fentanyl to bupivacaine for caesarean section. Singapore Med J. 1998;39:290–4. [PubMed] [Google Scholar]
- 23.Idowu OA, Sanusi AA, Eyelade OR. Effects of intrathecally administered fentanyl on duration of analgesia in patients undergoing spinal anesthesia for elective caesarean section. Afr J Med Med Sci. 2011;40:213–9. [PubMed] [Google Scholar]
- 24.Cowan CM, Kendall JB, Barclay PM, Wilkes RG. Comparison of intrathecal fentanyl and diamorphine in addition to bupivacaine for caesarean section under spinal anesthesia. Br J Anaesth. 2002;89:452–8. [PubMed] [Google Scholar]
- 25.Kang FC, Tsai YC, Chang PJ, Chen TY. Subarachnoid fentanyl with diluted small-dose bupivacaine for cesarean section delivery. Acta Anaesthesiol Sin. 1998;36:207–14. [PubMed] [Google Scholar]
- 26.Belzarena SD. Clinical effects of intrathecally administered fentanyl in patients undergoing cesarean section. Anesth Analg. 1992;74:653–7. doi: 10.1213/00000539-199205000-00006. [DOI] [PubMed] [Google Scholar]


