Abstract
The aim of this review is to present the most recent data regarding the indications of mini percutaneous nephrolithotomy (PCNL), the results and the complications of the method. Medline was searched from 1997 to January 2014, restricted to English language. The Medline search used a strategy including medical subject headings and free-text protocols. PCNL is a well-established treatment option for patients with large and complex renal calculi. In order to decrease morbidity associated with larger instruments like blood loss, postoperative pain and potential renal damage, a modification of the technique of standard PCNL has been developed. This is performed with a miniature endoscope via a small percutaneous tract (11–20 F) and was named as minimally invasive or mini-PCNL. This method was initially described as an alternative percutaneous approach to large renal stones in a pediatric patient population. Furthermore, it has become a treatment option for adults as well, and it is used as a treatment for calculi of various sizes and locations. However, the terminology has not been standardized yet, and the procedure lacks a clear definition. Nevertheless, mini-PCNL can achieve comparable stone-free rates to the conventional method, even for large stones. It is a safe procedure, and no major complications are reported. Although less invasiveness has not been clearly demonstrated so far, mini-PCNL is usually related to less blood loss and shorter hospital stay than the standard method.
Keywords: Complications, mini percutaneous nephrolithotomy, modified Clavien system, stone-free rate, urolithiasis
INTRODUCTION
Urinary stone disease has affected humankind since antiquity. In addition, the incidence of kidney stones has been increased in western societies in the last decades in association with economic development. Nephrolithiasis is a common cause of morbidity in the USA, with a lifetime prevalence of 5-10%.[1] Moreover, kidney stones are a recurrent disorder, with lifetime recurrence risks reported to be as high as 50%.[2] Therefore, urolithiasis is considered to be a disorder with significant socioeconomical parameters, which influences the quality of life. Major technological advances have improved the treatment of kidney stones and minimally invasive techniques, such as extracorporeal shock wave lithotripsy (ESWL), retrograde intrarenal surgery (RIRS), percutaneous nephrolithotomy (PCNL) and laparoscopic ureterolithotomy, have now largely replaced open surgery.[3]
According to the updated European Association of Urology (EAU) guidelines, PCNL is recommended as the therapy of choice for large renal calculi (>20 mm) and also for smaller stones (10–20 mm) of the lower renal pole when unfavorable factors for ESWL exist.[3] Excellent stone-free rates (SFR) following PCNL have been reported, which range from 76% to 98%.[4] However, PCNL is still a challenging surgical technique and can be associated with significant complications, that may compromise its efficacy.
In order to decrease morbidity associated with larger instruments like blood loss, postoperative pain and potential renal damage, a modification of the technique of standard PCNL has been developed. This is performed with a miniature endoscope via a small percutaneous tract (11–20 F) and was named as minimally invasive PCNL or mini-PCNL or mini Perc. Helal et al. were the first to describe a technique for pediatric nephrolithotomy performed on a 2-year-old premature female child with the use of instruments with smaller access diameters.[5] The method involved sequential dilation to 16 F followed by use of a 15 F vascular peel-away sheath. A 10 F pediatric cystoscope and grasper were used to remove the stones. However, mini-PCNL technique was first developed and accomplished by Jackman et al. in the pediatric population with the use of an 11 F access tract.[6] Since then, the method has become a treatment option for adults as well.[7,8,9] Usually, the term mini-PCNL is used for access sheaths below 20 F. However, the terminology has not been standardized yet, and the procedure lacks a clear definition.
The literature was systematically reviewed for the indications, technique, success rates, and complications regarding mini-PCNL.
EVIDENCE ACQUISITION
Medline was searched from 1997 to January 2014, restricted to English language. The Medline search used a strategy including medical subject headings (MeSH) and free-text protocols.
A literature review using the keywords mini-PCNL, minimal invasive PCNL, mini PNL, urolithiasis, indications and contraindications, technique, SFR, efficacy, complications, Clavien, and the MeSH terms nephrostomy, percutaneous/indications, and technique, and efficacy, and adverse effects, and intraoperative complications or postoperative complications was accomplished.
Small (<25 patients) single-center trials, case reports, insufficient methodology, insufficient reporting of indications and contraindications and/or technique and/or success rates and/or complications were excluded.
INDICATIONS AND CONTRAINDICATIONS
Percutaneous nephrolithotomy with the use of appropriate size instruments is recommended by the EAU guidelines as the first-line treatment for renal pelvic or caliceal stones with a diameter larger than 20 mm in children.[3] It is performed as monotherapy in most cases, but it is suggested as an adjunctive procedure as well. However, further indications for mini-PCNL have not been clearly defined. It is true that the use of smaller instruments via smaller access tracts has contributed to a wider use of percutaneous techniques, even for stones smaller than 20 mm.[10,11] Nevertheless, mini-PCNL has not only been used for the removal of small lower caliceal stones, but for the treatment of large impacted proximal ureteral stones and staghorn calculi as well.[12,13,14,15,16]
General indications for mini-PCNL that may also exist for the conventional method include previous failure of ESWL or ureteroscopic lithotripsy, cystine calculi and anatomic abnormalities precluding retrograde access or the distal passage of stones.[8] Mini-PCNL may also be useful in patients with a narrow (<5 mm) or long (>30 mm) infundibulum or as a secondary access for inaccessible or residual fragments resulting from standard PCNL.[8,17]
Anticoagulant therapy must be discontinued before the procedure.[3] Patients receiving aspirin, for example, should discontinue it 7 days before mini-PCNL while those on warfarin need to discontinue the drug 5 days before mini-PCNL. Other important contraindications include untreated urinary tract infections (UTIs), pregnancy, atypical interposition of visceral organs (bowel, spleen or liver), tumor in the probable access tract area and potential malignant renal tumor.[3]
TECHNIQUE
The common denominator of the mini-PCNL technique is the use of small instruments and small diameter sheaths. Access sizes ranging from 11 F to 20 F have been reported in the literature.[18] The use of a great variety of endoscopes has been described by different authors for stone disintegration and removal of fragments. The most common instruments used are an 8/9.8 F rigid or semi-rigid ureteroscope and a specially designed 12 F mini nephroscope with a 6 F working channel and automatic pressure control.[10,15,18] Hydrodynamic effects of a specially designed metallic Amplatz sheath (15 F/16.5 F/18 F/20 F) placed over a one-step metallic dilator were used to evacuate fragmented stones without additional pressure or suction.[10] If the angle of the percutaneous tract precludes a direct approach to stone fragments, a 15.5 F flexible cystonephrocope or 7.5 F flexible ureteroscope may also be utilized.[17]
Traditionally, PCNL has been performed in the prone position, and it is a well-established technique. Valdivia Uría et al. first described the supine position as an alternative, considering anesthesiologic advantages for patients at higher risk for cardiopulmonary complications.[19] Liu et al. performed a systematic review and meta-analysis of standard PCNL for patients in the supine versus prone position and found that both positions appeared to be equivalent with regard to efficacy and safety.[20] The only difference found was a significantly shorter operative time in the supine position, attributed to the time-consuming patient positioning. Additionally, Zhan et al. conducted a randomized trial comparing the effectiveness and safety of the supine lithotomy position for mini-PCNL versus the traditional prone position.[21] In their series, including 109 patients, similar results were reported. The mean operative time was significantly shortened in the supine position, but both positions seemed to be equally effective and safe.[21] Operating in the supine position may also facilitate a combined approach with simultaneous retrograde ureteroscopic and/or intrarenal access.[20,22,23] The traditional prone position, on the other hand, provides access to the posterior calyx with less risk of parenchymal bleeding or perforation and neighboring organ injuries.[22] The position also eases the creation of multiple access tracts and obviates obscured visibility caused by the pelvicaliceal collapse noted in the supine position.[22,23]
In general, percutaneous puncture of the kidney and dilation techniques do not usually differ from standard PCNL. Renal access is usually achieved by the lower posterior calyx or sometimes by the calyx with the largest stone burden.[8,10,17] A posterior middle calyx puncture via the 11th intercostal space between the posterior axillary line and scapula line is usually preferred in the Chinese modification of the method.[15,16,18] For staghorn stones, multiple tracts are usually necessary and are created in the same session.[14,15] Access is gained under the fluoroscopic and/or ultrasonographic control. Intracorporeal lithotripsy devices include ultrasonic, pneumatic and laser lithotriptors.[3] Most stone fragments can be flushed out along with the backflow through the aforementioned specially designed metallic Amplatz seath without increasing intrarenal pressure.[10] Bigger fragments can be extracted with stone forceps or tipless baskets.[12,24] In a series published by Chinese high-volume centers, an endoscopic pulsed perfusion pump is specially designed for retrieval of fragments. Renal pelvic pressure remained lower than the level needed for causing a pyelovenous backflow during these procedures.[15]
The even less invasive character of the mini-PCNL due to smaller access tracts makes the procedure feasible in a tubeless or totally tubeless manner, especially in uncomplicated cases when a stone free status is achieved. Assumed advantages of a tubeless procedure are better patient comfort, less postoperative pain, shorter hospital stay and quicker recovery. A randomized prospective trial evaluated the efficacy and safety of tubeless (JJ stent but no nephrostomy drainage tubes) versus conventional mini-PCNL (JJ stent and drainage tubes).[25] In this series with 32 patients, the tubeless mini-PCNL group had significantly shorter hospital stays and experienced significantly less back pain than the conventional mini-PCNL group. There were no significant differences in operation time, stone clearance and complications.[25] Less postoperative pain and consequently less need for analgesia were also confirmed in the group of patients who underwent tubeless (JJ stent but no nephrostomy tubes) mini-PCNL in a prospective comparative study.[26] The morbidity of JJ-stents, however can be significant. Stent related discomfort is reported in 39% of patients.[27] Totally tubeless mini-PCNL should be performed to achieve the best results in terms of pain but in selected cases.[26] Two meta-analyses of tubeless versus standard PCNL have been published so far.[28,29] A similar meta-analysis regarding mini-PCNL may offer useful conclusions.
The type of care of the nephrostomy tract in order to prevent hemorrhage or persisting urinary leakage is being discussed. The application of different hemostatic agents is mentioned in several studies. The use of gelatin matrix hemostatic sealant, which gains popularity recently, seems to prevent bleeding and urine extravasation.[26,30,31] The necessity for sealant use, however remains controversial and has not been confirmed yet.
EFFICACY
The effectiveness of mini-PCNL is still under debate. Proponents of the method mention limited blood loss, increased maneuverability, decreased postoperative pain and limited hospital stay. Limitations of the procedure include the necessity to disintegrate stones into small enough fragments to fit through a reduced-size sheath which results in longer operative times.
Even in the first series regarding mini-PCNL, the SFR was high enough although the stone burden was relatively low. Jackman et al. reported an SFR of 85% in children and 89% in adults with a stone burden 1.2 cm2 and 1.5 cm2, respectively.[6,7] Similar SFRs between mini-PCNL and PCNL have been reported by most authors except Giusti et al. who reported lower SFRs despite longer operative times.[32]
As the indications for mini-PCNL expanded, newer data were published recently. In Table 1, there is an overview of the recently published SFRs. However, comparison of the data is difficult because of the different definition of SFR with regard to the time of the stone-free state and the real definition of stone-free (true stone-free or clinically insignificant fragments [CIRFs]). CIRFs are usually considered as stone fragments smaller than 3 mm although it is believed that if the CIRFs are left untreated; approximately half of the patients will experience a stone-related event for which more than 50% will also need further intervention.[38] Furthermore, there is wide variation in the imaging used to assess postoperative stone-free status. Most authors use ultrasonography or plain X-ray of kidneys, ureters and bladder. Nephrography and computed tomography (CT) are used less common.[15,26] CT is more accurate although it carries more radiation exposure and is more expensive. Patients, who could not achieve stone-free status will undergo auxiliary procedures such as second look PCNL, RIRS or ESWL.
Table 1.
Data regarding stone free rates of mini-PCNL published in recent series with more than 25 patients
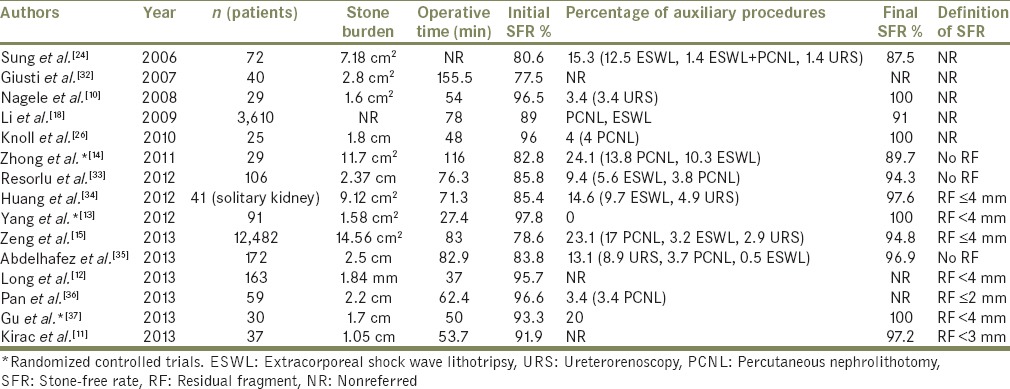
No significant differences in SFR between the mini-PCNL and PCNL has been demonstrated. However, a better stone clearance rate was demonstrated for multiple caliceal stones when mini-PCNL was performed (85.2% vs. 70%).[39] Higher SFR was achieved in the treatment of staghorn stones with mini-PCNL and the creation of multiple access tracts (89.7% vs. 68%).[14] Nevertheless, longer operative times are usually associated with mini-PCNL (155.5 min and 45 min vs. 106.6 min and 31 min respectively).[32,40] Mini-PCNL seems to be more effective when treating smaller (<20 mm) rather than larger (>20 mm) renal stones (SFR 90.8% vs. 76.3%).[35] It also shows better SFR than ESWL especially for stones >10 mm.[41,42] In specific, when the efficacy of ESWL and mini-PCNL in treating renal stones sized 15–25 mm in infants <3 years were compared, significantly higher SFR was observed in the mini-PCNL Group I month postoperatively (84% vs. 31.8%).[42] When mini-PCNL is compared to RIRS for the treatment of large renal calculi (20–30 mm), it seems that mini-PCNL can achieve significantly higher SFR (96.6% vs. 71.4%).[36] Similar effectiveness of the two methods is reported when smaller stones are treated.[11,43] Superiority of mini-PCNL over RIRS was found in the treatment of large impacted proximal ureteral stones (≥15 mm) as well (93.3% vs. 41.4%).[37] Operative times of RIRS seem to be significantly longer in general (66.4 min, 73.1 min and 106 min vs. 53.7 min, 62.4 min and 59 min respectively) with comparable stone burden.[11,36,43] However, combination of RIRS and mini-PCNL is better than monotherapy with mini-PCNL for large calculi (>30 mm), even with shorter operative times (initial SFR 81.7% vs. 38.9%) (120.5 min vs. 181.9 min).[44] The patient is put in prone split-leg position for combined retrograde and antegrade access with the use of 14 Fr ureteral access sheath of length measuring 35 cm in females and 55 cm in males advanced to the ureteropelvic junction to facilitate passage of stone fragments after renal access and stone fragmentation at low intrapelvic pressure.
COMPLICATIONS
The concept behind mini-PCNL was based on the assumption that the use of smaller tracts would decrease morbidity observed in the conventional method. Such an advantage of mini-PCNL has been firstly reported in infants.[45,46,47] Controversy still exists on whether mini-PCNL is less invasive than standard PCNL. Li et al. prospectively evaluated the systemic response to mini-PCNL and PCNL.[48] Based on experimental findings that acute-phase reaction is proportional to surgery-induced tissue damage, they perioperatively measured acute phase markers such as tumor necrosis factor-a, interleukin-6/10, C-reactive protein and serum amyloid A. No significant differences were noted between mini-PCNL and PCNL and their data failed to demonstrate a significant advantage of mini-PCNL in terms of reduced surgical trauma and associated invasiveness compared with standard PCNL.[48] Moreover, Traxer et al. measured and compared the extent of renal parenchyma injury in pigs undergone 11 F and 30 F percutaneous nephrostomy.[49] The difference between the fibrotic scar volumes and the corresponding loss of parenchyma induced by the two tracts was not significant. The authors also concluded that renal parenchyma damage resulting from the creation of a nephrostomy tract is small compared to overall renal volume regardless of the size of the nephrostomy tract.[49] However, the benefit of mini-PCNL remains as the use of smaller access sheaths resulted in reduced intraoperative blood loss, less postoperative pain and shorter hospital stay. An advantage of mini-PCNL over the conventional procedure was noted in terms of a significantly reduced hemoglobin drop (0.53 g/dl and 0.8 g/dL vs. 0.97 g/dL and 1.3 g/dL respectively)[39,40] and the need for blood transfusion (1.4% vs. 10.4%).[39] Analgesic requirement has also been found significantly decreased in mini-PCNL when compared to standard PCNL (55.4 g vs. 70.2 g tramadol).[40] Hospital stay was significantly shorter after mini-PCNL (3.8 days and 3.2 days vs. 6.9 days and 4.8 days respectively).[26,40]
Although, mini-PCNL has not a proven clear advantage over the conventional procedure in terms of lower invasiveness, it remains a safe method. Table 2 shows an overview of the recently published complication rates. Complications can occur during and after the procedure and can be related to renal access and stone removal.[4] Since 2007, the modified Clavien grading system has been used to report perioperative complications of conventional PCNL.[50] In addition, de la Rosette categorization of complications and validation of the Clavien score for PCNL was published.[51] It was demonstrated that the validity of the Clavien grading system is the highest for Grade V and the lowest for Grade I. It had also been proposed that many of the low-grade complications may not be specifically related to PCNL and can be attributed to any surgical procedure or anesthesia.[15] Moreover, it has been shown that the postoperative hospitalization increased with higher Clavien complications.[51] Nevertheless, complication rates are not always recorded according to the Clavien grading system by the authors in recently published literature.
Table 2.
Data regarding complication rates of mini-PCNL according to modified Clavien grading system, published in recent series with more than 25 patients
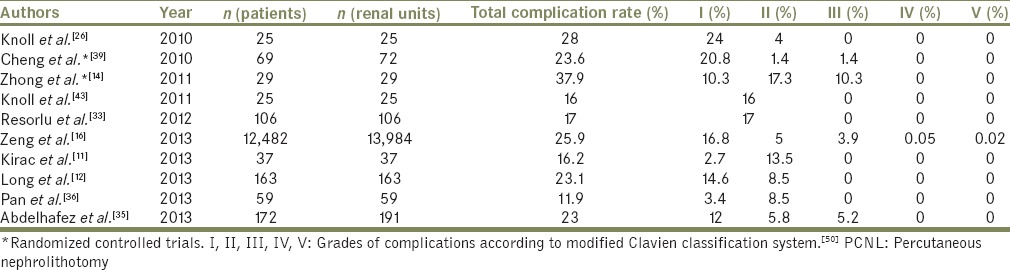
Total complication rates published in a recent series of mini-PCNL according to the Clavien system range from 11.9% to 37.9%. Clavien Grades I, II, III, IV, and V are observed in 2.7–20.8%, 1.4–17.3%, 0–10.3%, 0–0.05% and 0–0.02% of the patients, respectively. In comparison, total complication rates in series of conventional PCNL range from 16.2% to 60.3% and Clavien rates I, II, IIIa, IIIb, IVa, IVb and V are noted in 4–41.2%, 4.5–17.6%, 0–6.6%, 0–2.8%, 0–1.1%, 0–0.5%, 0–0.1%, respectively.[52] It is of interest to mention that the total complication rate has not been found significantly different between patients undergone mini-PCNL for small (<20 mm) or large (>20 mm) renal stones (19.4% vs. 26.9%) and that no Grade IV or V complications occurred.[35] When simple (mean stone burden 10.18 cm2) and complex (mean stone burden 17.63 cm2) were compared, Grade I, II, III, IV and V complications were noted in 17.1% versus 16.6%, 4.29% versus 5.58%, 3.82% versus 4.06%, 0.02% versus 0.07%, and 0% versus 0.04% with regard to stone size, respectively.[15,16] However, blood transfusion (Grade II) (2.2% vs. 3.2%) and arterial embolization (Grade III) (0.28% vs. 0.67%) were observed more often in patients with complex stones. This can be probably attributed to the larger stone burden of these patients and the consequent need for multiple tracts.[15,16] Total complication rate of mini-PCNL was similar even in patients with a solitary kidney and renal calculi.[34] A significant improvement in GFR was detected from the preoperative period to 1-month follow-up. Adequate drainage in patients with a solitary kidney after mini-PCNL was proposed with the placement of both a JJ stent and a nephrostomy tube.[34]
As mentioned before, mini-PCNL is recommended for the treatment of large renal calculi in children. This specific category of patients has usually lower co-morbidities than adults. However, there is always a serious concern about the effect of the chosen treatment option on the growing kidney. The less robust pelvicaliceal system of children and a limited tolerance for blood loss make the procedure more challenging.[53] When mini-PCNL performed in children and adults were compared, there was no significant difference in perioperative total complication rate.[53] However, major complications (Grade IV and V) were not observed in children. On the other hand, intraoperative bleeding was significantly correlated with operative time, stone burden and sheath size in pediatric patients.[46] Higher hemoglobin drop has been reported in children undergone PCNL when nephrostomy tracts used exceeded 22 F (1.6 g/dl vs. 1.1 g/dl).[47] In a large series of 331 mini-PCNL in pediatric population a significant increase in hemoglobin drop and transfusion rate was also noticed in children with multiple nephrostomy tracts (2.7 g/dl vs. 2 g/dl and 18.8% vs. 4.5% respectively).[53] Zeng et al. compared ESWL and mini-PCNL for the treatment of renal stones sized 15–25 mm in infants younger than 3 years old. Total complication rate was significantly higher in the ESWL group (45.5% vs. 16%).[42] Recently mini-PCNL has been compared to RIRS for the treatment of renal calculi of different sizes.[36,37,43,47] No major complications occurred during or after the two procedures. Overall, complication rates were not significantly different between mini-PCNL and RIRS groups (17% and 16% vs. 8.4% and 23.8% respectively).[33,43] In only one study, which included children, blood transfusion rate (Grade II) was significant higher in the mini-PCNL group (6.6% vs. 0%).[33] However, blood transfusions were required when larger access sheaths were utilized (18–20 F), whereas none of the patients in the 12 F access group was transfused.[33] The mean hospital stay for patients undergoing mini-PCNL was found to be significant longer than those in the RIRS group, in most studies (1.7 days vs. 1-day, 4.47 days vs. 1.95 days, 3.1 days vs. 1.7 days and 4.6 days vs. 1.9 days respectively).[33,37,42,43]
Hemodynamic, electrolyte and metabolic changes were assessed and compared prospectively between mini-PCNL and standard PCNL.[54] Electrolyte levels and arterial blood gas analysis during and after both procedures were evaluated. Heart rate and arterial blood pressure were also monitored. A trend toward metabolic acidosis was observed as the irrigation time went by during mini-PCNL compared to the standard method.[54] Liu et al. retrospectively analyzed the data from 834 patients who underwent mini-PCNL, in order to explore the risk factors, prevention and management of the septic shock following the procedure.[55] Twenty out of the 834 patients (2.4%) developed septic shock and 3 (0.3%) expired. Female gender and diabetes mellitus were found to be the risk factors for septic shock following mini-PCNL.[55] Patients with diabetes, large stone burden, UTI and impaired renal function have a higher probability to require longer hospitalization time.[52] There is no extensive analysis in the literature of various risk factors that may influence the occurrence of complications. Body mass index has been studied thoroughly, but it does not seem to correlate with higher complication rates.[11,26,35,36,43] Some believe that more severe complications (Grade III or higher) should be quite rare and are more likely related to surgical techniques and the level of experience.[15] The experience curve is also reported to have a significant impact on the rates of intraoperative bleeding.[47]
CONCLUSION
Mini-PCNL was introduced as an alternative to the standard procedure in order to reduce morbidity associated with larger access tracts. Although less invasiveness has not been clearly demonstrated so far, mini-PCNL is related to less blood loss and shorter hospitalization. It is recommended for treatment of large renal stones in children and can be implemented in adults as well. Mini-PCNL seems to be a reasonable alternative for patients with a small-to-medium-sized stones, especially when a tubeless procedure is considered. Mini-PCNL is safe and is not related to serious complications.
Footnotes
Source of Support: Nil
Conflict of Interest: None.
REFERENCES
- 1.Stamatelou KK, Francis ME, Jones CA, Nyberg LM, Curhan GC. Time trends in reported prevalence of kidney stones in the United States: 1976-1994. Kidney Int. 2003;63:1817–23. doi: 10.1046/j.1523-1755.2003.00917.x. [DOI] [PubMed] [Google Scholar]
- 2.Prezioso D, Di Martino M, Galasso R, Iapicca G. Laboratory assessment. Urol Int. 2007;79(Suppl 1):20–5. doi: 10.1159/000104437. [DOI] [PubMed] [Google Scholar]
- 3.Türk C, Knoll T, Petrik A, Sarica K, Skolarikos A, Straub M, et al. Guidelines on Urolithiasis. Arnhem (The Netherlands): European Association of Urology (EAU) 2013 [Google Scholar]
- 4.Michel MS, Trojan L, Rassweiler JJ. Complications in percutaneous nephrolithotomy. Eur Urol. 2007;51:899–906. doi: 10.1016/j.eururo.2006.10.020. [DOI] [PubMed] [Google Scholar]
- 5.Helal M, Black T, Lockhart J, Figueroa TE. The Hickman peel-away sheath: Alternative for pediatric percutaneous nephrolithotomy. J Endourol. 1997;11:171–2. doi: 10.1089/end.1997.11.171. [DOI] [PubMed] [Google Scholar]
- 6.Jackman SV, Hedican SP, Peters CA, Docimo SG. Percutaneous nephrolithotomy in infants and preschool age children: Experience with a new technique. Urology. 1998;52:697–701. doi: 10.1016/s0090-4295(98)00315-x. [DOI] [PubMed] [Google Scholar]
- 7.Jackman SV, Docimo SG, Cadeddu JA, Bishoff JT, Kavoussi LR, Jarrett TW. The “mini-perc” technique: A less invasive alternative to percutaneous nephrolithotomy. World J Urol. 1998;16:371–4. doi: 10.1007/s003450050083. [DOI] [PubMed] [Google Scholar]
- 8.Chan DY, Jarrett TW. Mini-percutaneous nephrolithotomy. J Endourol. 2000;14:269–72. doi: 10.1089/end.2000.14.269. [DOI] [PubMed] [Google Scholar]
- 9.Lahme S, Bichler KH, Strohmaier WL, Götz T. Minimally invasive PCNL in patients with renal pelvic and calyceal stones. Eur Urol. 2001;40:619–24. doi: 10.1159/000049847. [DOI] [PubMed] [Google Scholar]
- 10.Nagele U, Schilling D, Sievert KD, Stenzl A, Kuczyk M. Management of lower-pole stones of 0.8 to 1.5 cm maximal diameter by the minimally invasive percutaneous approach. J Endourol. 2008;22:1851–3. doi: 10.1089/end.2008.9791. [DOI] [PubMed] [Google Scholar]
- 11.Kirac M, Bozkurt ÖF, Tunc L, Guneri C, Unsal A, Biri H. Comparison of retrograde intrarenal surgery and mini-percutaneous nephrolithotomy in management of lower-pole renal stones with a diameter of smaller than 15 mm. Urolithiasis. 2013;41:241–6. doi: 10.1007/s00240-013-0552-0. [DOI] [PubMed] [Google Scholar]
- 12.Long Q, Guo J, Xu Z, Yang Y, Wang H, Zhu Y, et al. Experience of mini-percutaneous nephrolithotomy in the treatment of large impacted proximal ureteral stones. Urol Int. 2013;90:384–8. doi: 10.1159/000343668. [DOI] [PubMed] [Google Scholar]
- 13.Yang Z, Song L, Xie D, Hu M, Peng Z, Liu T, et al. Comparative study of outcome in treating upper ureteral impacted stones using minimally invasive percutaneous nephrolithotomy with aid of patented system or transurethral ureteroscopy. Urology. 2012;80:1192–7. doi: 10.1016/j.urology.2012.08.045. [DOI] [PubMed] [Google Scholar]
- 14.Zhong W, Zeng G, Wu W, Chen W, Wu K. Minimally invasive percutaneous nephrolithotomy with multiple mini tracts in a single session in treating staghorn calculi. Urol Res. 2011;39:117–22. doi: 10.1007/s00240-010-0308-z. [DOI] [PubMed] [Google Scholar]
- 15.Zeng G, Zhao Z, Wan S, Mai Z, Wu W, Zhong W, et al. Minimally invasive percutaneous nephrolithotomy for simple and complex renal caliceal stones: A comparative analysis of more than 10,000 cases. J Endourol. 2013;27:1203–8. doi: 10.1089/end.2013.0061. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Zeng G, Mai Z, Zhao Z, Li X, Zhong W, Yuan J, et al. Treatment of upper urinary calculi with Chinese minimally invasive percutaneous nephrolithotomy: A single-center experience with 12,482 consecutive patients over 20 years. Urolithiasis. 2013;41:225–9. doi: 10.1007/s00240-013-0561-z. [DOI] [PubMed] [Google Scholar]
- 17.Monga M, Oglevie S. Minipercutaneous nephorlithotomy. J Endourol. 2000;14:419–21. doi: 10.1089/end.2000.14.419. [DOI] [PubMed] [Google Scholar]
- 18.Li X, He Z, Wu K, Li SK, Zeng G, Yuan J, et al. Chinese minimally invasive percutaneous nephrolithotomy: The Guangzhou experience. J Endourol. 2009;23:1693–7. doi: 10.1089/end.2009.1537. [DOI] [PubMed] [Google Scholar]
- 19.Valdivia Uría JG, Valle Gerhold J, López López JA, Villarroya Rodriguez S, Ambroj Navarro C, Ramirez Fabián M, et al. Technique and complications of percutaneous nephroscopy: Experience with 557 patients in the supine position. J Urol. 1998;160:1975–8. doi: 10.1016/s0022-5347(01)62217-1. [DOI] [PubMed] [Google Scholar]
- 20.Liu L, Zheng S, Xu Y, Wei Q. Systematic review and meta-analysis of percutaneous nephrolithotomy for patients in the supine versus prone position. J Endourol. 2010;24:1941–6. doi: 10.1089/end.2010.0292. [DOI] [PubMed] [Google Scholar]
- 21.Zhan HL, Li ZC, Zhou XF, Yang F, Huang JF, Lu MH. Supine lithotomy versus prone position in minimally invasive percutaneous nephrolithotomy for upper urinary tract calculi. Urol Int. 2013;91:320–5. doi: 10.1159/000351337. [DOI] [PubMed] [Google Scholar]
- 22.de la Rosette JJ, Tsakiris P, Ferrandino MN, Elsakka AM, Rioja J, Preminger GM. Beyond prone position in percutaneous nephrolithotomy: A comprehensive review. Eur Urol. 2008;54:1262–9. doi: 10.1016/j.eururo.2008.08.012. [DOI] [PubMed] [Google Scholar]
- 23.De Sio M, Autorino R, Quarto G, Calabrò F, Damiano R, Giugliano F, et al. Modified supine versus prone position in percutaneous nephrolithotomy for renal stones treatable with a single percutaneous access: A prospective randomized trial. Eur Urol. 2008;54:196–202. doi: 10.1016/j.eururo.2008.01.067. [DOI] [PubMed] [Google Scholar]
- 24.Sung YM, Choo SW, Jeon SS, Shin SW, Park KB, Do YS. The “mini-perc” technique of percutaneous nephrolithotomy with a 14-Fr peel-away sheath: 3-year results in 72 patients. Korean J Radiol. 2006;7:50–6. doi: 10.3348/kjr.2006.7.1.50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Lu Y, Ping JG, Zhao XJ, Hu LK, Pu JX. Randomized prospective trial of tubeless versus conventional minimally invasive percutaneous nephrolithotomy. World J Urol. 2013;31:1303–7. doi: 10.1007/s00345-012-0921-2. [DOI] [PubMed] [Google Scholar]
- 26.Knoll T, Wezel F, Michel MS, Honeck P, Wendt-Nordahl G. Do patients benefit from miniaturized tubeless percutaneous nephrolithotomy? A comparative prospective study. J Endourol. 2010;24:1075–9. doi: 10.1089/end.2010.0111. [DOI] [PubMed] [Google Scholar]
- 27.Shah HN, Sodha HS, Khandkar AA, Kharodawala S, Hegde SS, Bansal MB. A randomized trial evaluating type of nephrostomy drainage after percutaneous nephrolithotomy: Small bore v tubeless. J Endourol. 2008;22:1433–9. doi: 10.1089/end.2007.0350. [DOI] [PubMed] [Google Scholar]
- 28.Borges CF, Fregonesi A, Silva DC, Sasse AD. Systematic review and meta-analysis of nephrostomy placement versus tubeless percutaneous nephrolithotomy. J Endourol. 2010 doi: 10.1089/end.2010.0231. [DOI] [PubMed] [Google Scholar]
- 29.Wang J, Zhao C, Zhang C, Fan X, Lin Y, Jiang Q. Tubeless vs standard percutaneous nephrolithotomy: A meta-analysis. BJU Int. 2012;109:918–24. doi: 10.1111/j.1464-410X.2011.10463.x. [DOI] [PubMed] [Google Scholar]
- 30.Nagele U, Anastasiadis AG, Schilling DA, Sievert KD, Kuczyk MA, Stenzl A. Introducing a new sealant applicator for easy, safe, and quick closure of a mini-percutaneous nephrolitholapaxy access tract. J Endourol. 2007;21:393–6. doi: 10.1089/end.2006.0244. [DOI] [PubMed] [Google Scholar]
- 31.Nagele U, Schilling D, Anastasiadis AG, Corvin S, Seibold J, Kuczyk M, et al. Closing the tract of mini-percutaneous nephrolithotomy with gelatine matrix hemostatic sealant can replace nephrostomy tube placement. Urology. 2006;68:489–93. doi: 10.1016/j.urology.2006.03.081. [DOI] [PubMed] [Google Scholar]
- 32.Giusti G, Piccinelli A, Taverna G, Benetti A, Pasini L, Corinti M, et al. Miniperc? No, thank you! Eur Urol. 2007;51:810–4. doi: 10.1016/j.eururo.2006.07.047. [DOI] [PubMed] [Google Scholar]
- 33.Resorlu B, Unsal A, Tepeler A, Atis G, Tokatli Z, Oztuna D, et al. Comparison of retrograde intrarenal surgery and mini-percutaneous nephrolithotomy in children with moderate-size kidney stones: Results of multi-institutional analysis. Urology. 2012;80:519–23. doi: 10.1016/j.urology.2012.04.018. [DOI] [PubMed] [Google Scholar]
- 34.Huang Z, Fu F, Zhong Z, Zhang L, Xu R, Zhao X. Chinese minimally invasive percutaneous nephrolithotomy for intrarenal stones in patients with solitary kidney: A single-center experience. PLoS One. 2012;7:e40577. doi: 10.1371/journal.pone.0040577. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Abdelhafez MF, Amend B, Bedke J, Kruck S, Nagele U, Stenzl A, et al. Minimally invasive percutaneous nephrolithotomy: A comparative study of the management of small and large renal stones. Urology. 2013;81:241–5. doi: 10.1016/j.urology.2012.09.030. [DOI] [PubMed] [Google Scholar]
- 36.Pan J, Chen Q, Xue W, Chen Y, Xia L, Chen H, et al. RIRS versus mPCNL for single renal stone of 2-3 cm: Clinical outcome and cost-effective analysis in Chinese medical setting. Urolithiasis. 2013;41:73–8. doi: 10.1007/s00240-012-0533-8. [DOI] [PubMed] [Google Scholar]
- 37.Gu XJ, Lu JL, Xu Y. Treatment of large impacted proximal ureteral stones: Randomized comparison of minimally invasive percutaneous antegrade ureterolithotripsy versus retrograde ureterolithotripsy. World J Urol. 2013;31:1605–10. doi: 10.1007/s00345-013-1026-2. [DOI] [PubMed] [Google Scholar]
- 38.Skolarikos A, Papatsoris AG. Diagnosis and management of postpercutaneous nephrolithotomy residual stone fragments. J Endourol. 2009;23:1751–5. doi: 10.1089/end.2009.1546. [DOI] [PubMed] [Google Scholar]
- 39.Cheng F, Yu W, Zhang X, Yang S, Xia Y, Ruan Y. Minimally invasive tract in percutaneous nephrolithotomy for renal stones. J Endourol. 2010;24:1579–82. doi: 10.1089/end.2009.0581. [DOI] [PubMed] [Google Scholar]
- 40.Mishra S, Sharma R, Garg C, Kurien A, Sabnis R, Desai M. Prospective comparative study of miniperc and standard PNL for treatment of 1 to 2 cm size renal stone. BJU Int. 2011;108:896–9. doi: 10.1111/j.1464-410X.2010.09936.x. [DOI] [PubMed] [Google Scholar]
- 41.Kruck S, Anastasiadis AG, Herrmann TR, Walcher U, Abdelhafez MF, Nicklas AP, et al. Minimally invasive percutaneous nephrolithotomy: An alternative to retrograde intrarenal surgery and shockwave lithotripsy. World J Urol. 2013;31:1555–61. doi: 10.1007/s00345-012-0962-6. [DOI] [PubMed] [Google Scholar]
- 42.Zeng G, Jia J, Zhao Z, Wu W, Zhao Z, Zhong W. Treatment of renal stones in infants: Comparing extracorporeal shock wave lithotripsy and mini-percutaneous nephrolithotomy. Urol Res. 2012;40:599–603. doi: 10.1007/s00240-012-0478-y. [DOI] [PubMed] [Google Scholar]
- 43.Knoll T, Jessen JP, Honeck P, Wendt-Nordahl G. Flexible ureterorenoscopy versus miniaturized PNL for solitary renal calculi of 10-30 mm size. World J Urol. 2011;29:755–9. doi: 10.1007/s00345-011-0784-y. [DOI] [PubMed] [Google Scholar]
- 44.Hamamoto S, Yasui T, Okada A, Taguchi K, Kawai N, Ando R, et al. Endoscopic combined intrarenal surgery for large calculi: Simultaneous use of flexible ureteroscopy and mini-percutaneous nephrolithotomy overcomes the disadvantageous of percutaneous nephrolithotomy monotherapy. J Endourol. 2014;28:28–33. doi: 10.1089/end.2013.0361. [DOI] [PubMed] [Google Scholar]
- 45.Bilen CY, Koçak B, Kitirci G, Ozkaya O, Sarikaya S. Percutaneous nephrolithotomy in children: Lessons learned in 5 years at a single institution. J Urol. 2007;177:1867–71. doi: 10.1016/j.juro.2007.01.052. [DOI] [PubMed] [Google Scholar]
- 46.Zeren S, Satar N, Bayazit Y, Bayazit AK, Payasli K, Ozkeçeli R. Percutaneous nephrolithotomy in the management of pediatric renal calculi. J Endourol. 2002;16:75–8. doi: 10.1089/089277902753619546. [DOI] [PubMed] [Google Scholar]
- 47.Desai MR, Kukreja RA, Patel SH, Bapat SD. Percutaneous nephrolithotomy for complex pediatric renal calculus disease. J Endourol. 2004;18:23–7. doi: 10.1089/089277904322836613. [DOI] [PubMed] [Google Scholar]
- 48.Li LY, Gao X, Yang M, Li JF, Zhang HB, Xu WF, et al. Does a smaller tract in percutaneous nephrolithotomy contribute to less invasiveness? A prospective comparative study. Urology. 2010;75:56–61. doi: 10.1016/j.urology.2009.06.006. [DOI] [PubMed] [Google Scholar]
- 49.Traxer O, Smith TG, 3rd, Pearle MS, Corwin TS, Saboorian H, Cadeddu JA. Renal parenchymal injury after standard and mini percutaneous nephrostolithotomy. J Urol. 2001;165:1693–5. [PubMed] [Google Scholar]
- 50.Tefekli A, Ali Karadag M, Tepeler K, Sari E, Berberoglu Y, Baykal M, et al. Classification of percutaneous nephrolithotomy complications using the modified clavien grading system: Looking for a standard. Eur Urol. 2008;53:184–90. doi: 10.1016/j.eururo.2007.06.049. [DOI] [PubMed] [Google Scholar]
- 51.de la Rosette JJ, Opondo D, Daels FP, Giusti G, Serrano A, Kandasami SV, et al. Categorisation of complications and validation of the Clavien score for percutaneous nephrolithotomy. Eur Urol. 2012;62:246–55. doi: 10.1016/j.eururo.2012.03.055. [DOI] [PubMed] [Google Scholar]
- 52.Seitz C, Desai M, Häcker A, Hakenberg OW, Liatsikos E, Nagele U, et al. Incidence, prevention, and management of complications following percutaneous nephrolitholapaxy. Eur Urol. 2012;61:146–58. doi: 10.1016/j.eururo.2011.09.016. [DOI] [PubMed] [Google Scholar]
- 53.Zeng G, Zhao Z, Wan S, Zhong W, Wu W. Comparison of children versus adults undergoing mini-percutaneous nephrolithotomy: Large-scale analysis of a single institution. PLoS One. 2013;8:e66850. doi: 10.1371/journal.pone.0066850. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Xu S, Shi H, Zhu J, Wang Y, Cao Y, Li K, et al. A prospective comparative study of haemodynamic, electrolyte, and metabolic changes during percutaneous nephrolithotomy and minimally invasive percutaneous nephrolithotomy. World J Urol. 2014;32:1275–80. doi: 10.1007/s00345-013-1204-2. [DOI] [PubMed] [Google Scholar]
- 55.Liu C, Zhang X, Liu Y, Wang P. Prevention and treatment of septic shock following mini-percutaneous nephrolithotomy: A single-center retrospective study of 834 cases. World J Urol. 2013;31:1593–7. doi: 10.1007/s00345-012-1002-2. [DOI] [PubMed] [Google Scholar]


