Abstract
Objectives:
To evaluate the attitude and perception of the graduates of King Saud University (KSU) College of Medicine regarding the quality of their urology rotation, urology exposure during this rotation, confidence about managing common conditions, and career prospects.
Materials and Methods:
In 2013, a questionnaire regarding the students’ perceptions of urology rotation was developed and E-mailed to all final (5th) year medical students and interns of KSU College of Medicine, Riyadh, Saudi Arabia. Individual responses were recorded, tabulated and compared using descriptive statistics.
Results:
The overall response rate was 67.7%. Respondents included 101 (49.8%) males and 102 (50.2%) females. All the respondents but 18 (8.9%) were enrolled in a urology rotation during undergraduate years. Only 27 (13.3%) were willing to choose urology specialty as a future career. Significant gender differences were found regarding choice of urology as a future career (P = 0.002) and the need for more urology exposure during surgical rotation (P = 0.002).
Conclusions:
Knowledge of medical school graduates is insufficient in many urologic subjects, and there is a need for more urology exposure. Social reasons and lack of knowledge about urology hinder the choice of urology specialty as a future career. Clearance of learning objectives, immediate and prompt feedback on performance and adequate emphasis of common problems and ambulatory care are some aspects that should be taken into account by curriculum planners as they consider improvements to urology rotation program.
Keywords: Medical school, medical students, Saudi Arabia, urology
INTRODUCTION
King Saud University (KSU) College of Medicine, a leading first medical college in Saudi Arabia, accepts graduates of secondary schools after completing a 1-year preparatory course comprising different subjects such as biology, chemistry, physics, medical biostatistics, and English for medical profession. Only students with a grade point average higher than 3 are accepted.[1]
In the 6 years medical program, the preclinical years are represented in the first 2 years where disciplines are integrated with a block/module system. The blocks in these 2 years are: Foundation block, musculoskeletal block, respiratory block, cardiovascular block, renal block, nervous system block, gastrointestinal and hematology block, endocrine block and reproduction block. The next 3 years revolve around various clinical clerkships, and preparation of students to join the medical workforce.[2] In the 5th year, students have 10 weeks rotation in surgery including 1-week in urology. The internship year is the 6th year of medical school when students get more clinical responsibilities under faculty supervision. 6th year graduates have license to practice as general practitioner (GP) all over the country.
With an aging patient population, the frequency with which medical graduates will encounter common urologic problems in the primary care setting will increase.[3,4,5] Thus, the significance of effective urologic education, both didactic and clinical, during medical undergraduate years cannot be overemphasized.
An increasing concern regarding the decline in urological education in medical schools has been recently raised.[6,7] Furthermore, efforts to assess and improve medical student learning in urology are lacking with no comprehensive study assessing urology-specific education in medical schools. Graduates’ perception of the undergraduate medical programs has been an invaluable source for evaluating and improving of these programs.[8,9,10] United States, Graduate Exit Questionnaire is a part of the routine educational process. Data obtained through these surveys are used for quality assurance, finding areas that need curriculum revision, and for tracking changes implemented over a longitudinal period.[8]
We aimed to evaluate the attitude and perception of the graduates of KSU College of Medicine regarding the quality of their urology rotation as well as to assess their urology exposure, confidence about managing common conditions, and career prospects.
MATERIALS AND METHODS
A questionnaire regarding the students’ perceptions of the urology rotation in the final (5th) year of medical school, their competence, overall satisfaction with their training, and career prospects was developed [Appendix 1]. The questionnaire was based largely on a previously used questionnaire[3] and the graduation survey distributed in the United States by the Association of American Medical Colleges.[11] It consisted of Likert scale, binary (yes/no) and multiple choice questions (MCQ). The questions were grouped into 2 major parts to cover students’ perception of urology rotation (part I) and evaluation (part II). The questions in part I were further grouped to cover 3 main issues that included perception of urology rotation, career prospects, and urology knowledge and skills.
After Institution Board approval, questionnaires were E-mailed to all final (5th) year medical students and interns of KSU College of Medicine and the identity of the collected data was kept anonymous to the researchers. Individual responses were recorded and tabulated. Descriptive statistics were presented as the mean, median and percent. For comparative statistics we used Chi-square, Fisher's exact and the nonparametric method of Mann–Whitney tests as appropriate.[12] A P < 0.05 was considered significant for all tests performed using SPSS 18 statistical software (SPSS, Chicago, IL, USA). The study was conducted in 2013 at College of Medicine, KSU, Riyadh, Saudi Arabia.
RESULTS
The overall response rate was 203/300 (67.7%), 101 (49.8%) were males and 102 (50.2%) were females. Respondents included 119 (58.6%) 5th year medical students and 84 (41.1%) medical interns. Missing responses were few 74/7105, (1%).
Part I: Students’ perception
Perception of urology rotation
The majority of respondents had a urology rotation (185, 91.1%), 107 (52.7%) defined urology as a surgical specialty, and 94 (46.3%) considered it as a medico-surgical specialty. Most of the respondents (185, 91.1%) found urology specialty as important or very important, and 157 (77.3%) recommended the inclusion of urology rotation in medical school curriculum. Patient's bedside teaching and attending urology clinics were the best urology learning modalities chosen by the students in 111 (54.7%) and 40 (19.7%) respectively. MCQ examination and objective structured clinical examination were the most common evaluation methods used as part of the final evaluation in 160 (78.8%) respondents [Table 1].
Table 1.
Respondent's perception and differences per gender
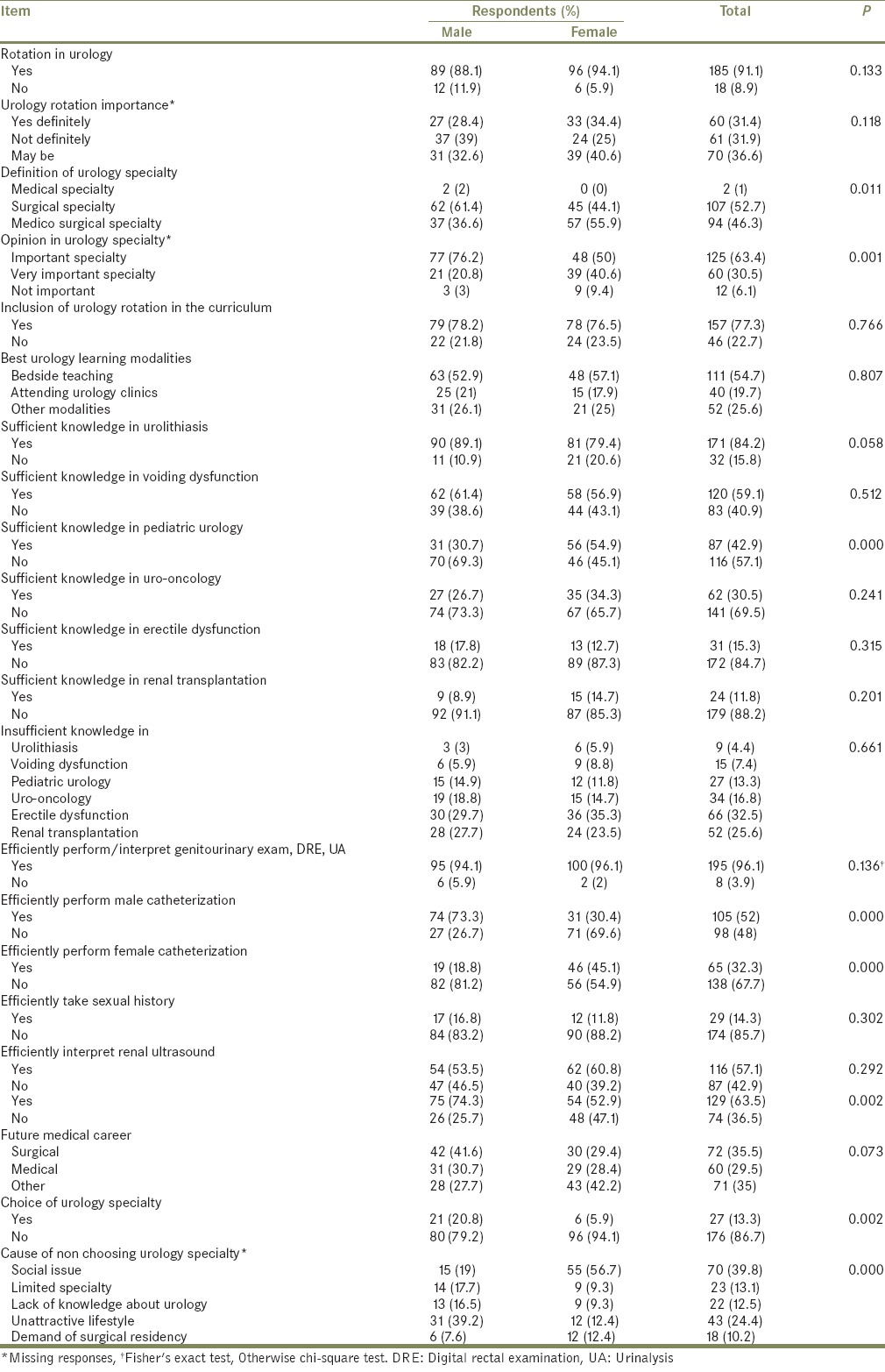
Perception of career prospects
Of the respondents, 27 (13.3%) were willing to choose urology career; 21 (77.8%) males and 6 (22.2%) females. Social barriers (70, 39.8%), unattractive life style (43, 24.4%), and limited specialty (23, 13.1%) were the main reasons behind non choosing urology career. In general, surgery (32, 35.5%), medicine (60, 29.6%), emergency medicine (22, 10.8%), and radiology (15, 7.4%) represented the main specialties chosen by the respondents as future career [Table 1].
Perception of urology knowledge and skills
Most of the respondents (171, 84.2%) reported a sufficient knowledge in urolithiasis. Sufficient knowledge in voiding dysfunction, pediatric urology, and uro-oncology was reported by 120 (59.1%), 87 (42.9%), and 62 (30.5%) of the respondents respectively while 118 (58.1%) reported insufficient knowledge in erectile dysfunction and renal transplantation. However, 129 (63.5%) of the respondents recommended more urology exposure during the 5th year surgical rotation. All the respondents apart from 8 (3.9%) reported that they can efficiently perform genitourinary and digital rectal examination (DRE) as well as they can interpret the results of urinalysis (UA). About one half (105, 51.7%) were comfortable performing male catheterization. Approximately, only one-third (65, 32%) reported the ability to perform female catheterization.
Part II: Students’ evaluation
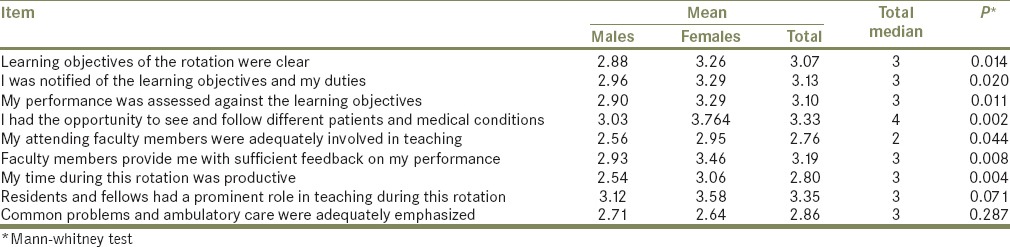
Median scores for each item of the second part of the questionnaire were summarized in Table 2. Most of the responses had a median of 3 which corresponds to uncertain. A value of 4 corresponding to disagree was the median of the responses to the statement “I had the opportunity to see and follow a variety of different patients with different medical conditions on this rotation.” A value of 2 corresponding to agree was the median of the responses to the statement “My attending faculty members were adequately involved in teaching during this rotation.”
Table 2.
Mean and median of total evaluation responses and differences per gender
Gender differences
No statistically significant gender differences were found regarding having a urology rotation, its significance nor its inclusion in medical school curriculum [Table 1]. Also, there was no significant gender differences regarding having sufficient knowledge in urolithiasis, voiding dysfunction, uro-oncology, erectile dysfunction, and renal transplantation nor in the subjects in which they feel having deficient knowledge [Table 1]. Both genders had no differences in performing genitourinary and DRE, taking sexual history and interpreting UA or renal ultrasound [Table 1]. However, male respondents more significantly defined urology as a surgical specialty, appreciated its importance and the need of more urology exposure during surgical rotation, and were more willing to choose urology specialty as a future career [Table 1]. Furthermore, they were significantly more comfortable performing male catheterization (P = 0.001).
Social barriers significantly hindered the choice of urology as a career (P = 0.000), more commonly in female respondents. Female respondents had a significantly more knowledge in pediatrics (P = 0.000) and were more comfortable performing female catheterization (P = 0.000).
Regarding the second part of the questionnaire assessing urology rotation, female respondents were significantly less agreeable than male respondents in the clearance of learning objectives of urology rotation, notification of that objectives, and assessment of their performance against learning objectives [Table 2]. They also were significantly less satisfied than males regarding the performance of their faculty members and the rotation productivity [Table 2]. No significant gender differences were identified regarding teaching role of residents and fellows during the rotation or in emphasis of common problems and ambulatory care [Table 2].
Educational level differences
Both interns and final year medical students had no significant differences in having urology rotation, opinion in urology specialty, importance of urology rotation inclusion in medical school curriculum, the choice of urology/surgery specialty as a future career, the need for more urology exposure during surgical rotation, or the best urology learning modality [Table 3]. Also, no significant differences were found between them regarding knowledge in urolithiasis, voiding dysfunction, pediatrics, erectile dysfunction and renal transplantation subjects [Table 3]. Both groups feel comfortable performing genitourinary examination, DRE, female catheterization, taking sexual history as well as interpreting results of UA and renal ultrasound [Table 3]. However, interns more significantly considered urology as a surgical specialty, appreciate more the significance of urology rotation and were more comfortable performing male catheterization [Table 3].
Table 3.
Respondent's perception per level
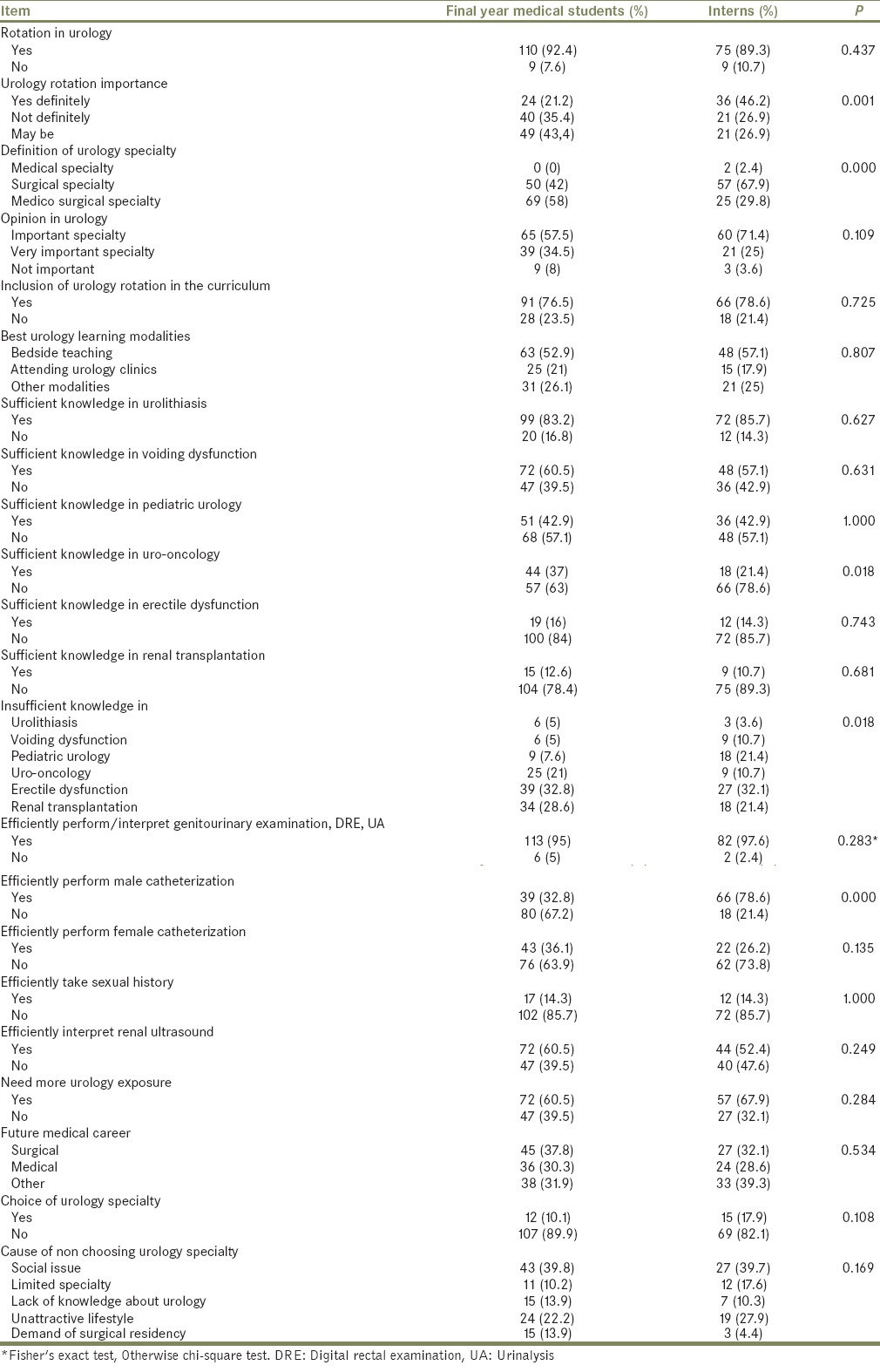
Regarding the second part of the questionnaire, interns more favorably rated variability of medical conditions (P = 0.023), involvement of faculty members in teaching (P = 0.000), and productivity of the course (P = 0.000) than final year medical students, who appreciated better the emphasis of common problems and ambulatory care (P = 0.015).
Effect of having urology rotation
Having urology rotation during the undergraduate clinical years had no statistically significant influence on choosing urology as a future career (P = 0.068), on the appreciation of the significance of urology specialty (P = 0.159), nor on the importance of urology rotation (P = 0.167). No significant differences could be found regarding having sufficient knowledge in urolithiasis (P = 0.186), voiding dysfunction (P = 0.748), pediatric urology (P = 0.392), uro-oncology (P = 0.181), and renal transplantation (P = 0.360) or in performing genitourinary and DRE (P = 0.469), male (P = 0.733) and female (P = 0.144) urethral catheterization as well as taking sexual history (P = 0.055) or interpreting UA (P = 0.469) and renal ultrasound (P = 0.392). Those who were enrolled in urology rotation reported more sufficient knowledge in the subject of erectile dysfunction (P = 0.044).
DISCUSSION
Medical school curricula should be designed to provide students with sufficient knowledge and skills to manage common urologic conditions in the primary care setting.[3] Students perception of undergraduate medical programs is essential for evaluation and improvement of these programs.[8,9,10] We evaluated for the 1st time in Saudi Arabia the urology exposure during medical school years as perceived by interns and final year graduates of KSU College of Medicine.
Although most of respondents (185, 93.9%) found urology specialty as important or very important and 157 (77.3%) recommended inclusion of urology rotation in medical school curriculum, 18 (8.9%) were not enrolled in a urology rotation. Similarly, only 20% of United States medical schools required clinical rotations in urology in the last several years.[7]
Nowadays, primary care physicians provide much of the initial health care to men and women with urological problems.[3,4,5] Thus, effective urologic education during medical undergraduate years became of paramount significance that we believe clinical urology rotations should be mandatory for all medical undergraduate students.
Student feedback on the most effective teaching methods is clearly helpful.[3] Patient's bedside teaching and attending urology clinics were the best urology learning modalities chosen by 151 (74.4%) of the respondents. Both methods allow active students participation, integration of basic and clinical sciences, enhancing clinical competencies and cognitive skills as well as enhancing self-directed learning.[2] Together with formal academic lectures, these are the main learning modalities in KSU medical college undergraduate clinical curriculum.
Traditions and social issues play an important role in all aspects of life in Saudi Arabia. Education and employment are not exempted from the social influences. Urology specialty as a career was more likely to be chosen by male respondents (P = 0.002) as social issues were the most predominant cause of non choosing urology specialty by female respondents (P = 0.000). This also explains why male respondents appreciated more the importance of urology specialty (P = 0.001) and recommended (P = 0.002) more urology exposure during undergraduate medical education [Table 1]. Furthermore, social issues were clearly behind the insufficient knowledge in erectile dysfunction (172, 84.7%) and the inefficiency to take sexual history in 174 (85.7%) respondents. Again, male respondents felt significantly more efficient in performing male catheterization (P = 0.000) while female respondents felt more comfortable performing female catheterization (P = 0.000). We also believe that social reasons are the cause underlying the lower rate of agreement with most of the items evaluating urology rotation in the second part of the questionnaire [Table 2]. Our results showed that only 87 (42.9%), 62 (30.5%) and 24 (11.8%) reported sufficient knowledge in subjects as pediatric urology, uro-oncology, and renal transplantation respectively. Erectile dysfunction and renal transplantation represented the topics of most knowledge deficiency chosen by 118 (58.1%) respondents. Apart from the effect of social issues regarding the subject of erectile dysfunction, it is apparent that bedside teaching and attending urology clinics are not enough to obtain sufficient knowledge in subjects like uro-oncology and renal transplantation. Interactive lectures, small group discussions and E-learning may help in such subjects.[2] Furthermore, final year medical students and interns are not expected to have full knowledge in such subjects that require a higher level of specialization.
Although we attempted to evaluate any relation of having urology rotation on the choice of urology as a future career or gaining sufficient knowledge in common urology subjects interesting for GPs, no effect in all parameters studied could be recognized. This may be explained by the small sample size of those who were not enrolled in an elective urology rotation (18/203, 8.9%). Similar results were reported by Mishail et al.[6]
Medical student exposure to urology is a prerequisite before a student can decide to choose urology as a career.[7,13] Lack of knowledge about urology was the cause of non choosing urology specialty as a future career in 22 (12.5%) responses [Table 1]. Furthermore, none of those who didn’t have urology rotation chose to join urology as a future career although the difference couldn’t attain a statistical significance (P = 0.068). Again this may be attributed to the small size of those who were not enrolled in an elective urology rotation (18/203, 8.9%).
Despite tremendous growth, change and technological advancement in urological care in the last decade as well as graying of society, there has not been a corresponding increase in exposure to urological education.[7] The statement “I had the opportunity to see and follow a variety of different patients with different medical conditions on this rotation” had a median response of 4 corresponding to disagree. This underscores the need for development of effective curriculum and educational strategies to improve the acquisition of knowledge and clinical skills needed for medical school graduates. Clearance of learning objectives, immediate and prompt feedback on performance, and adequate emphasis of common problems and ambulatory care are some aspects that should be taken into account by curriculum planners as they consider improvements to urology rotation programs.
The small sample size of those who were not enrolled in a planned urology rotation during undergraduate medical study and inclusion of only one medical school (although the largest) were the main limitations of the current study. A multicenter study is warranted to evaluate undergraduate urology rotation at other academic institutions and medical schools across the country.
CONCLUSIONS
Knowledge of medical school graduates is insufficient in many urologic subjects. Learning objectives of urology rotation are unclear, and feedback on performance is inadequate. The time of urology rotation is not productive with lack of variability of urology medical conditions and the need for more urology exposure. Social reasons and lack of knowledge about urology hinder the choice of urology specialty as a future career. Patient's bedside teaching and attending urology clinics are the best urology learning modalities reported. There is still an ample room for improving urology teaching for undergraduate medical students.
The findings of this study should assist urology specialty develop a robust curriculum for urology rotation ensuring good knowledge of urology and satisfactory acquisition of necessary urological skills. The study also supports for more research in urologic education in the undergraduate medical education levels and the creation of a validated instrument to evaluate medical student learning in clinical urology.
ACKNOWLEDGMENTS
This study was supported by a grant from the College of Medicine Research Center, Deanship of Scientific Research, King Saud University, Riyadh, Saudi Arabia.
Appendix 1: Attitude and perception of urology by medical students at the end of their medical school: an appraisal from saudi arabia
Dear Medical student/Intern:
We would like to invite you to participate in this short survey, which is looking at medical student's attitude and perception of urology by the end of their final school year.
Learning environments, given the limited time and available resources, may play a crucial role in teaching undergraduate clinical urology.
The main purpose of this study is to evaluate the current learning environment, and hence to improve the knowledge acquisition needed for medical school graduates.
Your time and answers are highly appreciated.
Your time and answers are highly appreciated.
Gender ◻ Male ◻ Female
-
Level ◻ Intern ◻ 5th year medical student
Part I
-
Have you been enrolled/rotated in academic urology unit?
◻ Yes ◻ No
-
If Yes, Do you think working/rotating in a urology unit increased your preparation to become an intern?
◻ Yes definitely ◻ Not definitely ◻ May be
-
How do you define urology?
◻ Medical specialty ◻ Surgical specialty
◻ Medico-surgical specialty
-
In general, do you consider urology as:
◻ Important specialty ◻ Very important
◻ Not important at all
-
Do you think Urology rotation should be part of medical school curriculum?
◻ Yes ◻ No
-
In your opinion what is the best modality to learn urology?
◻ Dealing with in-patient and bed-side teaching
◻ Attending urology clinics
◻ Independent reading ◻ Watching open surgery
◻ Watching endoscopic surgery ◻ Regular lectures
-
Which of the following evaluation methods were used as a part of final evaluation in this rotation? (More than one item may be correct)
◻ Multiple Choice Questions (MCQs) Oral examination
◻ Observation by faculty member.
◻ Objective Structured Clinical Examination (OSCE)
◻ Observation and evaluation by resident physicians
◻ Written essay questions
◻ Other methods; Please specify…
◻ No formal evaluation was performed
-
Which urology subjects do you consider your knowledge sufficient in? (You can mark more than one choice)
◻ Lithiasis/stone disease ◻ Voiding dysfunction
◻ Pediatric urology ◻ Uro-oncology
◻ Erectile dysfunction ◻ Renal transplant
-
Which urology subjects do you consider your knowledge deficient in? (Please mark only one)
◻ Lithiasis/stone disease ◻ Voiding dysfunction
◻ Pediatric urology ◻ Uro-oncology
◻ Erectile dysfunction ◻ Renal transplant
Do you think you need more exposure and knowledge regarding urological disease during your 5th year surgery rotation? ◻ Yes ◻ No
-
Which of the following investigation/procedure you feel comfortable to perform/interpret? (You can mark more than one choice)
◻ Male genitourinary exam ◻ Digital rectal exam
◻ Sexual history ◻ Urinary catheterization (male)
◻ Urinary catheterization (female) ◻ Urinalysis
◻ Renal US
Do you intend to become a urologist? ◻ Yes ◻ No
-
If your answer is No, What caused you NOT to pursue a career in urology?
◻ Limited specialty
◻ Unattractive lifestyle
◻ Demand of surgical residency
◻ Lack of knowledge about urology
◻ Social issue
-
Which area would you like to pursue your medical career in?
◻ Medical specialization ◻ Surgical specialization
◻ Psychiatry ◻ ER ◻ Other, please specify
Part II
Indicate whether you agree or disagree with the statements about your urology rotation:
(Scale: 1 = Strongly Agree to 5 = Strongly Disagree)
1 2 3 4 5
Learning objectives of the rotation were clear. ◻ ◻ ◻ ◻ ◻
I was notified of the learning objectives and my duties during the rotation at the beginning of the course. ◻ ◻ ◻ ◻ ◻
My performance was assessed against the learning objectives ◻ ◻ ◻ ◻ ◻
I had the opportunity to see and follow a variety of different patients (with different medical conditions) on this rotation ◻ ◻ ◻ ◻ ◻
My attending faculty members were adequately involved in teaching during this rotation. ◻ ◻ ◻ ◻ ◻
Faculty members provided me with sufficient feedback on my performance. ◻ ◻ ◻ ◻ ◻
My time during this rotation was productive. ◻ ◻ ◻ ◻ ◻
Residents and fellows had a prominent role in teaching during this rotation. ◻ ◻ ◻ ◻ ◻
Common problems and ambulatory care were adequately emphasized. ◻ ◻ ◻ ◻ ◻
Footnotes
Source of Support: College of Medicine Research Center, Deanship of Scientific Research, King Saud University, Riyadh, Saudi Arabia
Conflict of Interest: None.
REFERENCES
- 1.Al-Rukban MO, Munshi FM, Abdulghani HM, Al-Hoqail I. The ability of the pre-admission criteria to predict performance in a Saudi medical school. Saudi Med J. 2010;31:560–4. [PubMed] [Google Scholar]
- 2.Azer SA, Hasanato R, Al-Nassar S, Somily A, AlSaadi MM. Introducing integrated laboratory classes in a PBL curriculum: Impact on student's learning and satisfaction. BMC Med Educ. 2013;13:71. doi: 10.1186/1472-6920-13-71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Hoag NA, Hamidizadeh R, Macneily AE. Undergraduate exposure to urology: Impact of the distributed model of medical education in British Columbia. Can Urol Assoc J. 2011:1–6. doi: 10.5489/cuaj.10101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Wei JT, Miner MM, Steers WD, Rosen RC, Seftel AD, Pasta DJ, et al. Benign prostatic hyperplasia evaluation and management by urologists and primary care physicians: Practice patterns from the observational BPH registry. J Urol. 2011;186:971–6. doi: 10.1016/j.juro.2011.04.081. [DOI] [PubMed] [Google Scholar]
- 5.Litwin MS, Saigal CS, Beerbohm EM. The burden of urologic diseases in America. J Urol. 2005;173:1065–6. doi: 10.1097/01.ju.0000156555.89385.54. [DOI] [PubMed] [Google Scholar]
- 6.Mishail A, Shahsavari M, Kim J, Welliver RC, Jr, Vemulapalli P, Adler HL. Deficits in urological knowledge among medical students and primary care providers: Potential for impact on urological care. J Urol. 2008;180:2140–7. doi: 10.1016/j.juro.2008.07.043. [DOI] [PubMed] [Google Scholar]
- 7.Loughlin KR. The current status of medical student urological education in the United States. J Urol. 2008;179:1087–90. doi: 10.1016/j.juro.2007.10.068. [DOI] [PubMed] [Google Scholar]
- 8.Jalili M, Mirzazadeh A, Azarpira A. A survey of medical students’ perceptions of the quality of their medical education upon graduation. Ann Acad Med Singapore. 2008;37:1012–8. [PubMed] [Google Scholar]
- 9.Jones A, McArdle PJ, O’Neill PA. How well prepared are graduates for the role of pre-registration house officer? A comparison of the perceptions of new graduates and educational supervisors. Med Educ. 2001;35:578–84. doi: 10.1046/j.1365-2923.2001.00955.x. [DOI] [PubMed] [Google Scholar]
- 10.Hesketh EA, Allan MS, Hsssarden RM, Macpherson SG. New doctors’ perceptions of their educational development during their first year of postgraduate training. Med Teach. 2003;25:67–76. doi: 10.1080/0142159021000061459. [DOI] [PubMed] [Google Scholar]
- 11.Association of American Medical Colleges (2012) Graduation Questionnaire. [Last accessed on 2014 Sep 24]. Available from: https://www.aamc.org/download/300448/data/2012 gqallschoolssummaryreport.pdf .
- 12.Tomkins CC, Hall C. An introduction to non-parametric statistics for health scientists. UAHSJ. 2006;3:20–6. [Google Scholar]
- 13.Kerfoot BP, Nabha KS, Masser BA, McCullough DL. What makes a medical student avoid or enter a career in urology? Results of an international survey. J Urol. 2005;174:1953–7. doi: 10.1097/01.ju.0000177462.61257.4e. [DOI] [PubMed] [Google Scholar]


