Abstract
Objectives:
Partial nephrectomy is a standard intervention for the treatment of small renal tumors. Our study compares the outcomes of three different partial nephrectomy methods (open, laparoscopic and robotic assisted) in obese (≥30 Kg/m2) patients with renal tumors.
Materials and Methods:
Between 2005-2011, 66 obese patients had partial nephrectomy. Patients were divided into three groups according to intervention received: Open (n = 21), laparoscopic (n = 31) and robotic (n = 14). The outcome variables of blood loss, length of hospital stay, and complications were assessed.
Results:
Mean blood loss in the laparoscopic group (100 mls) was significantly less than open group (300 mls) and no difference between laparoscopic and robotic groups (150 mls). We observed a shorter median hospital stay in the laparoscopic group (two days) than open group (four days) and no difference between laparoscopic and robotic groups (three days). Three patients in the laparoscopic group had complications: Two grade II and one with grade III (based on Clavien-Dindo classification). Tumor location, pathology, grade, stage, patient gender, age, preoperative creatinine and postoperative creatinine were not different among the groups (P > 0.05). The mean tumor size in the laparoscopic group (2.70 cms) was significantly smaller than that of the open group (4.22 cm) (P < 0.05), but not statistically different from that of the robotic group (2.99 cm).
Conclusions:
Our study demonstrates that in obese patients, both laparoscopic and robotic partial nephrectomy are associated with less blood loss than open partial nephrectomy. Second, the length of the hospital stay was not related to the type of utilized intervention.
Keywords: Kidney neoplasms, minimally invasive, nephrectomy, obesity, surgical procedures
INTRODUCTION
According to the American Cancer Society, 65,150 new cases of kidney cancer will occur in the United States in the year 2013.[1] Due to numerous advancements in imaging modalities, renal cell carcinomas may be detected in their early stages. Partial nephrectomy emerged as a viable treatment option that will eradicate cancer while maintaining overall renal function.[2]
Age, general health, and obesity are three major factors that are associated with the risk of developing renal cancer.[3] In the United States, more than one-third of its citizens are considered to be obese.[4] A recent study determined that for robotic partial nephrectomy, body mass index (BMI) was strongly associated with estimated blood loss, length of stay, and operative time.[5] Currently, there are no reports to determine, which method of partial nephrectomy has a better outcome overall for obese patients.
This study compares the outcomes of three different partial nephrectomy methods (open, laparoscopic and robotic assisted) in obese patients at our institution, with obesity being defined as having a BMI ≥30 kg/m2.
MATERIALS AND METHODS
We first obtained Internal Review Board approval before starting any study activities.
Patient selection
A retrospective analysis was performed on a total of 66 obese patients who received partial nephrectomy by fellowship-trained urologic oncologists at our institution between 2005 and 2011.
Surgical approach
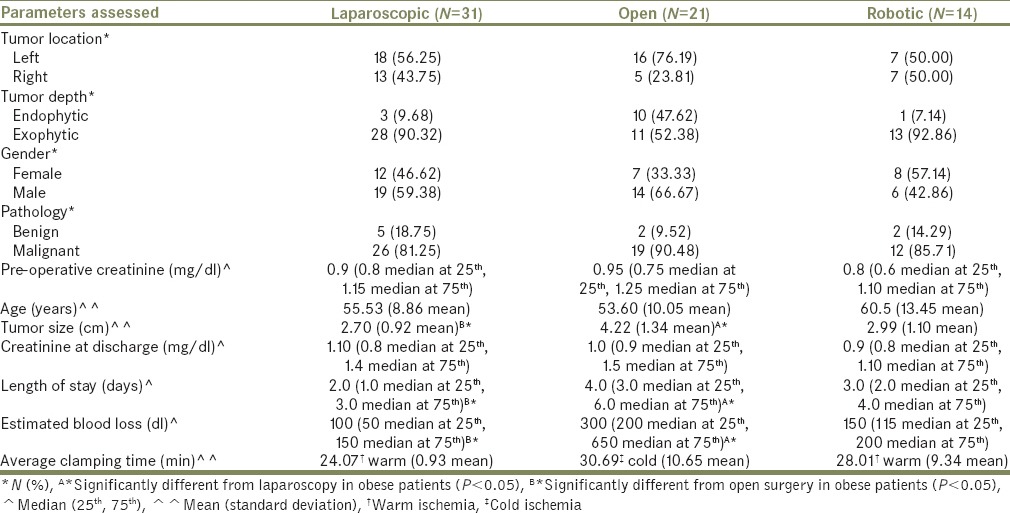
Surgical approach was based on patient and surgeon preferences as well as tumor characteristics (i.e., size, exophytic or endophytic location). These patients were divided into three groups based on the type of partial nephrectomy they received: Open (n = 21), laparoscopic (n = 31) and robotic (n = 14). Patient demographics are illustrated in Table 1. Outcome variables of blood loss, length of stay, morbidity, and mortality were assessed among the groups.
Table 1.
Patient demographics (total=66)
Statistical analysis
All analyses were performed using SAS 9.2 software. This program provides data access, transformation and reporting with data manipulation and descriptive statistics. Non-parametric tests were utilized because continuous variables such as the pre-operative and post-operative creatinine and the hospital length of stay were not normally distributed. P values were corrected for multiple group comparisons using Bonferroni's test. A comparison of the categorical variables such as tumor location and pathology across the intervention groups was made by the Chi-square test.
A quantile regression analysis was conducted to calculate the conditional medians of the blood loss and hospital stay due to different interventions. The intervention type and tumor size were included in the model as covariates for blood loss. As for length of hospital stay, intervention type and American Society of Anesthesiologists (ASA) score were utilized as covariates.
RESULTS
A total of 66 obese patients were identified and divided into three groups based on procedure type: Laparoscopic (n = 31), open (n = 21) and robotic partial nephrectomy (n = 14).
All except nine patients (four laparoscopic, four open and one robotic) had clamping of the renal vascular pedicle prior to the partial nephrectomy, with an average clamping time of 26.6 min and a range of 10-50 min. The average ischemia time for laparoscopic, open and robotic groups was 24, 30 and 28 min, respectively. Although, it appears from our data that the robotic approach had longer ischemia time, these numbers were not statistically significant. On univariate analysis, laparoscopic group had a median blood loss of 100 ml that was significantly less than the open group's median loss of 300 ml (P < 0.05). Though the robotic group blood loss was greater than laparoscopic (150 ml), statistically, there was no significant difference (P > 0.05). On multivariate analysis, however, both laparoscopic and robotic interventions were significant predictors of less blood loss in the obese population. Furthermore, tumor size was not a predictor of blood loss.
With regards to the hospital stay, univariate analysis determined that the laparoscopic group had significantly shorter median hospital stay of 2 days compared with the open group value of 4 days (P < 0.05). Robotic group had a median stay of 3 days, but this was not significantly greater than the laparoscopic group (P > 0.05). On multivariate analysis, none of the methods of partial nephrectomy were a predictor of shorter hospital stay in obese patients.
Univariate analysis revealed no difference among the groups in terms of tumor pathology, location, grade and stage. There was also no difference in gender, pre-operative and post-operative creatinine, and age. The mean creatinine at discharge was within the normal range (0.8-1.2), which leads us to use absolute numbers for creatinine in our table. Tumor size for open partial nephrectomy was statistically greater than that of the laparoscopic intervention (P < 0.05), but not for robotic. Furthermore, there was a tendency to perform open partial nephrectomy for endophytic tumors (P < 0.05) [Table 1]. Of the 66 obese patients, 64 had their margin status commented on. Of these 64, 5 had positive margins: 3 in the laparoscopic category, 1 robotic and 1 open.
We had three patients with complications, and all three of those patients with complications were in the laparoscopic group. We classified complications using the Clavien-Dindo classification of surgical complications. Two patients had grade II complications: Blood transfusion on the post-operative day 1, and pneumonia post-operative day 3. One patient had grade III complication: Urine leak on the post-operative day 3 treated with JJ stent. Mortality occurred in two patients: One patient had renal cell carcinoma metastasis to the lungs 3 years after laparoscopic partial nephrectomy and another patient had retro-peritoneal sarcoma with metastasis to the lungs 4 years after open partial nephrectomy.
There were a total of four patients who underwent conversion of surgical modality. In the laparoscopic group, a total of two patients were converted to open because of failure to progress/bleeding. In the robotic group, two patients were converted to laparoscopic intervention because of failure to progress.
DISCUSSION
Not only does obesity enhance one's risk of developing renal cancer,[6] but also increased BMI is associated with greater morbidity and mortality, a phenomenon explained by the notion that obesity is a “multisystem chronic pro-inflammatory disorder.”[7] Obese patients therefore bear a different set of comorbidities than non-obese, which may affect their peri-operative outcomes and path of recovery. One study that sought to determine the effect of BMI on partial nephrectomy peri-operative outcomes concluded that greater BMI is an independent risk factor for increased blood loss, length of stay and operative time.[5]
Partial nephrectomy can be safely achieved through multiple modalities. However, each method possesses its own set of advantages. For instance, one institution compared open to laparoscopic partial nephrectomy, stratified the results into different BMI categories, and found that for every category, laparoscopic partial nephrectomy was favored in terms of blood loss, hospital stay and operative time.[8] Our study focused on obese patients and expanded the comparison of partial nephrectomy techniques to not only include open and laparoscopic, but also robotic modality. We determined that the laparoscopic and robotic partial nephrectomy patients have predictably less blood loss than open partial nephrectomy. Though patients who received the open procedure also had larger tumor sizes, our multivariate analyses determined that tumor size was not a predictor of blood loss. Our multivariate analysis also indicated that the partial nephrectomy technique is not a predictor for shortened hospital stay. Overall we encountered three complications in the study, of which two were surgical complications. There are multiple factors that may explain both these findings. One possibility is that robotic surgery was recently introduced to our department, and the learning curve for robotic surgery takes time. Another is that the majority of patients in each group had ASA scores of two or three, so preexisting comorbidities may contribute to their hospital stay. We also acknowledge that the sample size of this study may not have provided enough power to detect a significant difference among the three modalities.
We only had one patient that had a urine leak that was successfully managed by a double J stent. We don’t feel that obesity increases the risk of urine leak after partial nephrectomy in our cohort. Similarly, we only had one patient that needed a blood transfusion post-operatively for a drop in his hematocrit/hemoglobin count. This patient responded well to the blood transfusion, and no further intervention was needed.
In an era of changing medical reimbursement and health cut backs, we should always think about modalities that will be minimally invasive and cost-effective, that we may achieve improved quality of life without compromising the patient's disease outcomes. A recent study compared overall costs among open, laparoscopic and robotic partial nephrectomies in both obese and non-obese patients. The authors concluded that laparoscopic partial nephrectomy was less costly than open technique because of shorter length of stay, and though laparoscopic length of stay was longer than robotic, the cost of instrumentation made robotic more expensive than laparoscopic.[9] We acknowledge that this study was a retrospective analysis and our patient population was non-randomized.
We concluded that in obese patients, the laparoscopic and robotic partial nephrectomy patients have less blood loss than open partial nephrectomy. Furthermore, length of stay was not related to the type of utilized surgical procedure.
Footnotes
Source of Support: Nil
Conflict of Interest: None.
REFERENCES
- 1.Cancer Research UK. 2012. [Last cited on 2013 Jun 01]. Available from: http://www.cancerresearchuk.org/cancer info/cancerstats/types/kidney/riskfactors/kidney-cancer-risk-factors .
- 2.Institute NC. National Cancer Institute at the National Institutes of Health. 2012. [Last cited on 2013 June 01]. Available from: http://www.cancer.gov/cancertopics/factsheet/Risk/obesity .
- 3.American Cancer Society. American Cancer Society. 2013. [Last cited on 2013 Apr 22]. Available from: http://www.cancer.org/cancer/kidneycancer/detailedguide/kidney-cancer-adult-key-statistics .
- 4.American Urological Association. American Urological Association. 2013. [Last cited on 2013 May 01]. Available from: http://www.auanet.org/content/press/press_releases/article.cfm?articleNo=127 .
- 5.Centers for Disease Control and Prevention. Centers for Disease Control and Prevention. 2013. [Last cited on 2013 Apr 22]. Available from: http://www.cdc.gov/obesity/data/adult.html .
- 6.Feder MT, Patel MB, Melman A, Ghavamian R, Hoenig DM. Comparison of open and laparoscopic nephrectomy in obese and nonobese patients: Outcomes stratified by body mass index. J Urol. 2008;180:79–83. doi: 10.1016/j.juro.2008.03.023. [DOI] [PubMed] [Google Scholar]
- 7.Mir SA, Cadeddu JA, Sleeper JP, Lotan Y. Cost comparison of robotic, laparoscopic, and open partial nephrectomy. J Endourol. 2011;25:447–53. doi: 10.1089/end.2010.0510. [DOI] [PubMed] [Google Scholar]
- 8.Kiziloz H, Dorin R, Finnegan KT, Shichman S, Meraney A. The impact of body mass index on perioperative outcomes in robot-assisted laparoscopic partial nephrectomy. J Endourol. 2013;27:1000–7. doi: 10.1089/end.2012.0665. [DOI] [PubMed] [Google Scholar]
- 9.Cullen A, Ferguson A. Perioperative management of the severely obese patient: A selective pathophysiological review. Can J Anaesth. 2012;59:974–96. doi: 10.1007/s12630-012-9760-2. [DOI] [PubMed] [Google Scholar]


