Abstract
Primary lymphoma of the urinary bladder is exceedingly rare, representing 0.2% of all extranodal non-Hodgkin's lymphoma. Although Matsuno et al. and others state the most common type is mucosa-associated lymphoid tissue (MALT) lymphoma, 20% of all the primary lymphomas of the urinary bladder are considered to be high grade neoplasms; the majority being diffuse large B-cell lymphoma (DLBCL). This is a case report of a 48-year-old man that presented with hematuria, frequency, nocturia, and flank pain that was found to have high grade DLBCL. Twenty-six other cases of both low and high grade primary bladder lymphomas were selected in order to provide a thorough comparison of different treatment modalities. Of the cases reviewed, bladder lymphoma was more common in females (2:1). The average age at diagnosis was 63.9 years old (low grade: 68.7 years old, high grade: 58.8 years old). The most common low-grade neoplasm was MALT lymphoma (85.7%). For the low-grade malignancies, the most successful treatments were simple therapies (2 transurethral resection of a bladder tumour [TURBT], 1 antibiotics), solitary chemotherapy, and combination TURBT/chemo; all 3 of which achieved 100% clinical remission (CR) in the cases reviewed. The most common high grade neoplasm was DLBCL (76.9%). The most successful therapies used to treat high grade lesions were solitary chemotherapy (cyclophosphamide, duanorubacin, vincristine, prednisolone [CHOP] or ritoximab, CHOP [R-CHOP]) and combination therapies (2 radiation/CHOP, 2 surgery/CHOP). In the agreement with the current literature, this review has shown that simple therapies (TURBT) are equally as effective as aggressive treatments (chemotherapy, radiation) and should therefore be used as first line treatment in low grade tumors. For high grade malignancies, chemotherapy (R-CHOP or CHOP) alone or combination therapy (CHOP/surgery or CHOP/radiation) is recommended.
Keywords: Cyclophosphamide, duanorubacin, vincristine, prednisolone chemotherapy, diffuse large B-cell lymphoma, extranodal non-Hodgkin's lymphoma, hematuria, primary bladder lymphoma
INTRODUCTION
Extranodal lymphomas make up 25-40% of all cases of lymphomas, with the most common sites being the stomach, connective tissue, and the skin.[1,2] Primary lymphomas of the urinary bladder are extremely rare, representing 0.2% of all extranodal lymphomas and <1% of all bladder tumors.[3] As of 2007, a little over 100 cases have been reported since the initial discovery by Eve and Chaffey in 1885.[4,5]
The majority of primary bladder lymphomas are low grade tumors with a good prognosis; the most common type being extranodal marginal zone/mucosa-associated lymphoid tissue (MALT) lymphoma.[3,6,7] High grade tumors are rarer, making up 20% of the reported cases with the most common type being diffuse large B-cell lymphoma (DLBCL).[3,8]
CASE REPORT
A 48-year-old obese (body mass index 39.6) man presented with 1 month history of gross hematuria that had worsened over the last week. The patient also reported nocturia ×8-10, flank pain, and urinary frequency. Prior to this, the patient had no preexisting medical conditions and his review of systems, and physical exams were unremarkable. The patient denied smoking and has a significant family history of leukemia.
In the office, his post void residual volume was 226 mL and urine analysis showed glycosuria (500 mg/dL), ketonuria (15 mg/dL), and hematuria (large amount of red blood cells).
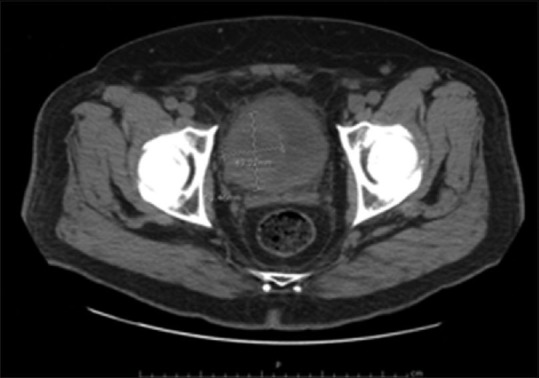
A computed tomography (CT) renay survey with and without contrast showed a 4.9 cm × 6.3 cm bladder mass [Figures 1 and 2] as well as right sided hydrouerteronephrosis and left distal ureter dilation. Transurethral resection was performed, and the initial pathology report showed invasive, poorly-differentiated, malignant tumor extending through the muscularis propria into the perivesicular adipose tissue. Immunohistochemical staining came back positive for CD10 and leukocyte common antigen, and negative for chromagranin. Fluorescence in situ hybridization (FISH) testing was negative for C-MYC, BCL-6, and BCL-2 gene rearrangement. The final diagnosis was DLBCL. Due to the highly invasive nature of the tumor, bone marrow (BM) biopsy was performed and showed no evidence of leukemia or lymphoma. A positron emission tomography (PET) scan showed a large uptake in the bladder (standardized uptake values [SUV]: 23.5, SUVmax: 35.2) and secondary “tree budding” nodules in the left lower lobe of the lung. The PET scan also showed small foci at the inferior pancreatic tail; magnetic resonance imaging is scheduled to further evaluate the pancreatic mass.
Figure 1.

Computed topography scan with contrast of a 48-year-old man presenting with a 1-month history of hematuria, frequency, and flank pain, showing a large anteriolateral bladder mass displacing the contrast dye
Figure 2.
Computed topography scan without contrast of a 48-year-old man presenting with a 1-month history of hematuria, frequency, and flank pain, showing 4.9 cm × 6.3 cm mass on the right anterolateral wall of the bladder
The patient has been receiving ritoximab, cyclophosphamide, duanorubacin, vincristine, prednisolone (R-CHOP) chemotherapy at the University of Virginia Health System. It has been 6 months since his diagnosis and he is on his fifth out of six cycles of chemotherapy. Thus far, PET CT scans have shown no abnormal uptake, indicative of effective treatment. Repeat cystoscopy has also shown no recurrence of the disease.
RESULTS
The epidemiology, clinical characteristics, histology, and treatments of the cases reviewed from the literature are shown in Tables 1 and 2. Table 1 represents all the low grade bladder lymphomas reviewed, while Table 2 shows all the high grade tumors.
Table 1.
Clinicopathologic characteristics, treatment, survival of low grade bladder lymphoma
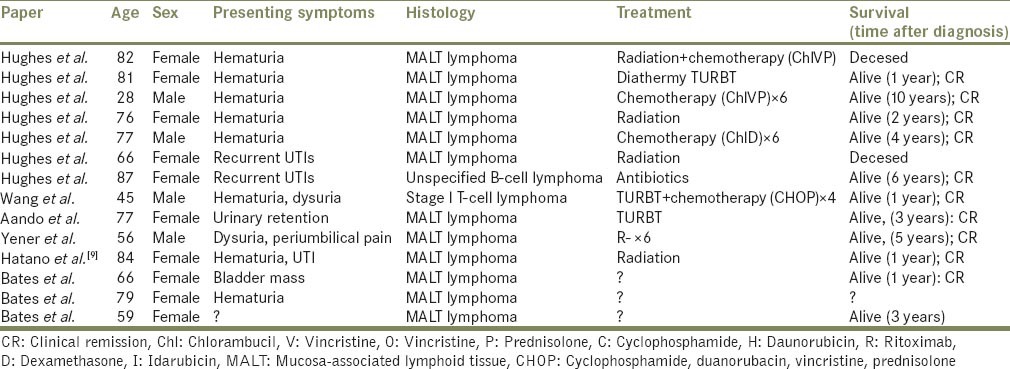
Table 2.
Clinicopathologic characteristics, treatment, survival of high grade bladder lymphoma
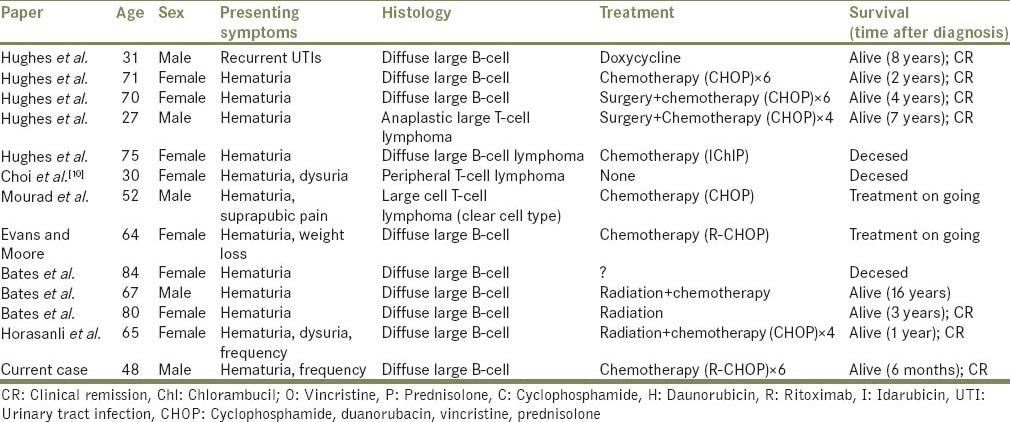
The average age was 63.9 years old; 68.7 years old for low-grade lymphomas and 58.8 years old for high grade lymphomas. Females outnumbered the males 2:1 which is consistent with the current literature.[3,6] Of the 27 cases reviewed, 74.1% presented with hematuria; 92.3% of the 13 high grade cases. According to both Hadway et al. and Bates et al., hematuria is the most common presenting symptom of primary bladder lymphomas.[8,11] Other presenting symptoms of primary bladder lymphomas are frequency, dysuria, nocturia, and suprapubic pain; 14.8% of the cases had a history of recurrent urinary tract infections.
The overall survival rate of the cases with completed treatment was 79.2% with a mean follow up of 4.13 (range: 0.5-16) years. Twelve of the 14 low grade cases were MALT lymphomas [Table 1]. The modalities used to treat these indolent lymphomas varied greatly in the literature. Three received radiation therapy only (2 in clinical remission [CR], 1 deceased). Two received chemotherapy only (1 ChlVP, 1 ChlD), both reaching CR. One received radiation and chemotherapy (ChlVP) and did not survive. Two reached CR with transurethral resection of a bladder tumor (TURBT) diathermy and another with TURBT plus chemotherapy CHOP. Three cases did not list the treatment course. One case of unspecified B-cell lymphoma reached CR with a course of unspecified antibiotics. Ten of the thirteen high grade lymphomas reviewed were DLBCL. Four received chemotherapy (2 R-CHOP, 1 CHOP, 1 IChlP); the patient receiving CHOP reached CR, one reached CR with R-CHOP, and the treatment regimen of IChlP was unsuccessful. Combination therapy of surgery plus CHOP chemotherapy (2 cases) or radiation plus CHOP (2 cases) was successful in four patients (CR in 3). One patient reached CR with a course of doxycycline. One patient died before treatment could be initiated.
DISCUSSION
Diagnosing a lymphoma in the urinary bladder relies on imaging, cystoscopy, and a thorough pathologic evaluation of biopsied tissue. On cystoscopy, these tumors are visualized as well-defined intravesicular masses typically located at the dome or the lateral walls of the bladder.[12] The pathology report should include immunohistochemical staining, FISH testing, and microscopic evaluation of the tumor grade. Immunohistochemical staining for B-cell type lymphomas routinely test positive for CD19, CD20, and CD21. Furthermore, low grade lymphomas routinely test positive for CD20, CD21, and CD43 cell markers, while high grade lymphomas are correlated with CD3, CD20, and CD30 cell markers.[8] FISH testing should be completed due to the propensity of B-cell lymphoid neoplasms to insert specific oncogenes next to immunoglobulin transcription enhancers.[13] The three main types of B-cell derived non-Hodgkin's lymphoma (NHL) with strongly associated FISH test abnormalities are as follows: Burkitt's lymphoma t (8;14) translocation of MYC gene, mantle cell lymphoma t (11;14) translocation of cyclin D1 gene, and follicular lymphoma t (14;18) translocation of BCL-2 gene. Absence of any of these translocations does not exclude these as diagnoses as they are not present in 100% of cases.[13] DLBCL has been associated with concurrent BCL-2 and MYC gene translocations.[14] Johnson et al. conducted a retrospective study from 1991 to 2007 looking at all the cases of NHL in the British Columbia Cancer Agency Lymphoid Cancer and Cytogenetic Database and comparing overall survival with the presence of both MYC and BCL-2 translocations; results showed decreased overall survival in the presence of these translocations due to poor response to chemotherapy. In fact, the presence of the BCL-2 translocation is said to provide lymphomas with an increased resistance to chemotherapy.[15] Once the type of bladder lymphoma has been identified, it is imperative to make the distinction between an indolent, low grade neoplasm versus an aggressive, high grade malignancy in order to initiate the most appropriate treatment regimen for that patient. If determined to be a high grade tumor, it is imperative to exclude systemic involvement; this can be done with a BM biopsy and a PET scan.[3]
The most common type primary lymphoma of the urinary bladder reported is low grade extranodal marginal zone (MALT) lymphoma.[3,6,7] Of the total cases reviewed here, 44.4% of them were MALT lymphomas (accounting for 85.7% of the low grade cases). A wide variety of modalities was reported and most all proved to be successful except for two patients who received radiation and radiation with chemotherapy. Similar to the literature, we recommend that a less systematically toxic therapy like TURBT be attempted first, followed by chemotherapy, radiation, or combination therapy. No recommendations on lesion size have been published for qualifications for TURBT. Therefore following criteria set for other bladder tumors could be used; TURBT has proven effective in urothelial bladder cancer that has yet to invade the musclaris propria (stage Ta, Tis, and T1). Radiation alone proved to be successful in only 66% (2 of 3) cases. As for the type of chemotherapy, all of the regimens (R-CHOP, CHOP, ChlVP, ChlD) were successful in treating low grade bladder lymphomas; R-CHOP was reported by the literature to be used most frequently.[16]
High grade primary bladder lymphoma represents roughly 20% of the 0.2% of extranodal lymphomas residing in the bladder.[7,8] The majority of these cases being DLBCL (76.9%) which is consistent with the most recent literature review on NHL.[17] The average age at diagnosis was 10.4 years younger than that of low grade lymphomas; this was not explained in the literature and should be further explored. DLBCL is an aggressive lymphoma and without treatment, leaves the patient with a prognosis of a matter of months.[17] All of the cases reviewed that utilized combination therapy (radiation/chemotherapy or surgery/chemotherapy) reported CR with an average follow up of 7 years; the majority of these using CHOP therapy. Chemotherapy is currently the preferential treatment due to its ability to treat early systematic disease which has not been detected.[2] The chemotherapy regimen of R-CHOP (ritoximab, cyclophosphamide, duanorubacin, vincristine, prednisolone) has documented success in treating both low and high grade primary bladder lymphomas as either solitary treatment or combination therapy.[16] Solitary treatment with R-CHOP was used in several of the cases reviewed but the only results published were those from this case review in which CR was achieved. Johnson et al. found that DLBCLs positive for the BCL-2 gene translocation may have a better prognosis if rituximab is added to the chemotherapy regimen. Rituximab has been shown to help overcome the chemotherapy resistance seen in patients with BCL-2 over expression by inducing cell apoptosis through the BCL-2 regulated mitochondrial pathway;[15,18] increasing the survival rate of patients with DLBCL on CHOP chemotherapy by 10-15% with very little additional toxicity.[19] Surgical techniques such as a cystectomy are recommended for any invasive transitional cell carcinoma that have spread into the muscular layer, however there are no clear surgical recommendation for bladder lymphomas and surgical modalities have been disputed in the literature due to the morbidity and mortality associated with these procedures.[12] Therefore, with the cases reviewed here, it is recommended that either solitary or combination therapy including the R-CHOP chemotherapy regimen be used to treat high grade urinary bladder lymphomas, particularly for BCL-2 positive DLBCL.
Lymphoma is a very commonly seen cancer, ranking in the top 10 most prevalent malignant neoplasms.[20] However, the diagnosis of primary lymphoma originating in the urinary bladder is exceedingly rare. Kempton et al. conducted a retrograde study of all the bladder lymphomas documented in the Mayo tissue registry from 1940 to 1996 and only found 6 of them to be primary. The rarity of this neoplasm is because there are no germinal follicles or lymphoid tissue developing in the bladder itself and, therefore, the etiology of such malignancies remains unknown. The leading theory in the literature is that these lymphomas develop in the background of a preexisting cystitis; 22-40% of the reported cases were preceded by chronic cystitis[3,8,21] and 4 of the 27 cases reviewed in this paper presented with active or recurrent cystitis. This could help explain why some primary bladder lymphomas have been successfully treated with antibiotics. No matter the cause, a focused effort should be made to identify and treat these lymphomas as the overwhelming consensus from the literature is a good prognosis if appropriate treatment is received[2,6,8] due to the tumors confinement to a solitary organ.[8]
Footnotes
Source of Support: Nil
Conflict of Interest: None.
REFERENCES
- 1.Mourad WA, Khalil S, Radwi A, Peracha A, Ezzat A. Primary T-cell lymphoma of the urinary bladder. Am J Surg Pathol. 1998;22:373–7. doi: 10.1097/00000478-199803000-00014. [DOI] [PubMed] [Google Scholar]
- 2.Wang L, Cao ZZ, Qi L. Primary T-cell lymphoma of the urinary bladder presenting with haematuria and hydroureteronephrosis. J Int Med Res. 2011;39:2027–32. doi: 10.1177/147323001103900550. [DOI] [PubMed] [Google Scholar]
- 3.Maninderpal KG, Amir FH, Azad HA, Mun KS. Imaging findings of a primary bladder maltoma. Br J Radiol. 2011;84:e186–90. doi: 10.1259/bjr/66130737. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Evans DA, Moore AT. The first case of vesico-vaginal fistula in a patient with primary lymphoma of the bladder-a case report. J Med Case Rep. 2007;1:105. doi: 10.1186/1752-1947-1-105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Jacobs A, Symington T. Primary lymphosarcoma of urinary bladder. Br J Urol. 1953;25:119–26. doi: 10.1111/j.1464-410x.1953.tb09253.x. [DOI] [PubMed] [Google Scholar]
- 6.Hughes M, Morrison A, Jackson R. Primary bladder lymphoma: Management and outcome of 12 patients with a review of the literature. Leuk Lymphoma. 2005;46:873–7. doi: 10.1080/10428190500079829. [DOI] [PubMed] [Google Scholar]
- 7.Kempton CL, Kurtin PJ, Inwards DJ, Wollan P, Bostwick DG. Malignant lymphoma of the bladder: Evidence from 36 cases that low-grade lymphoma of the MALT-type is the most common primary bladder lymphoma. Am J Surg Pathol. 1997;21:1324–33. doi: 10.1097/00000478-199711000-00007. [DOI] [PubMed] [Google Scholar]
- 8.Bates AW, Norton AJ, Baithun SI. Malignant lymphoma of the urinary bladder: A clinicopathological study of 11 cases. J Clin Pathol. 2000;53:458–61. doi: 10.1136/jcp.53.6.458. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Hatano K, Sato M, Tsujimoto Y, Takada T, Honda M, Matsumiya K, et al. Primary mucosa-associated lymphoid tissue (MALT) lymphoma of the urinary bladder associated with left renal pelvic carcinoma: A case report. Hinyokika Kiyo. 2007;53:57–60. [PubMed] [Google Scholar]
- 10.Choi JH, Jeong YY, Shin SS, Lim HS, Kang HK. Primary calcified T-cell lymphoma of the urinary bladder: A case report. Korean J Radiol. 2003;4:252–4. doi: 10.3348/kjr.2003.4.4.252. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Hadway P, Riaz AA, Lotzof KL, Gelister JS. Renal colic: An unusual presentation of non-Hodgkin's lymphoma of the urinary bladder. Grand Rounds. 2004;4:7–9. [Google Scholar]
- 12.Yener NA, Sinanoglu O, Sezgin G, Midi A, Ekici S. Primary muscosa-associated lymphoid tissue (MALT) lymphoma of the urinary bladder: A rare case report. Istanbul Med J. 2013;14:212–4. [Google Scholar]
- 13.Ventura RA, Martin-Subero JI, Jones M, McParland J, Gesk S, Mason DY, et al. FISH analysis for the detection of lymphoma-associated chromosomal abnormalities in routine paraffin-embedded tissue. J Mol Diagn. 2006;8:141–51. doi: 10.2353/jmoldx.2006.050083. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Johnson NA, Savage KJ, Ludkovski O, Ben-Neriah S, Woods R, Steidl C, et al. Lymphomas with concurrent BCL2 and MYC translocations: The critical factors associated with survival. Blood. 2009;114:2273–9. doi: 10.1182/blood-2009-03-212191. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Mounier N, Briere J, Gisselbrecht C, Emile JF, Lederlin P, Sebban C, et al. Rituximab plus CHOP (R-CHOP) overcomes bcl-2– Associated resistance to chemotherapy in elderly patients with diffuse large B-cell lymphoma (DLBCL) Blood. 2003;101:4279–84. doi: 10.1182/blood-2002-11-3442. [DOI] [PubMed] [Google Scholar]
- 16.Horasanli K, Kadihasanoglu M, Aksakal OT, Ozagari A, Miroglu C. A case of primary lymphoma of the bladder managed with multimodal therapy. Nat Clin Pract Urol. 2008;5:167–70. doi: 10.1038/ncpuro1035. [DOI] [PubMed] [Google Scholar]
- 17.Freedman AS, Friedberg JW, Lister A, Connor RF. Initial treatment of advanced stage diffuse large B cell lymphoma. [Uptodate 2013]; [Google Scholar]
- 18.Stolz C, Hess G, Hähnel PS, Grabellus F, Hoffarth S, Schmid KW, et al. Targeting Bcl-2 family proteins modulates the sensitivity of B-cell lymphoma to rituximab-induced apoptosis. Blood. 2008;112:3312–21. doi: 10.1182/blood-2007-11-124487. [DOI] [PubMed] [Google Scholar]
- 19.Sehn LH, Donaldson J, Chhanabhai M, Fitzgerald C, Gill K, Klasa R, et al. Introduction of combined CHOP plus rituximab therapy dramatically improved outcome of diffuse large B-cell lymphoma in British Columbia. J Clin Oncol. 2005;23:5027–33. doi: 10.1200/JCO.2005.09.137. [DOI] [PubMed] [Google Scholar]
- 20.Jemal A, Siegel R, Xu J, Ward E. Cancer statistics, 2010. CA Cancer J Clin. 2010;60:277–300. doi: 10.3322/caac.20073. [DOI] [PubMed] [Google Scholar]
- 21.Coskun U, Günel N, Eroglu A, Biri H, Poyraz A, Gurocak S, et al. Primary high grade malignant lymphoma of bladder. Urol Oncol. 2002;7:181–3. doi: 10.1016/s1078-1439(02)00186-2. [DOI] [PubMed] [Google Scholar]


