Abstract
Background
The quality of patient-physician discussions about chronic kidney disease (CKD) in primary care has not been studied previously.
Study Design
Cross-sectional study.
Settings & Participants
We audiotaped encounters between 236 patients with hypertension and their primary care physicians (n = 40).
Predictors
Patient, physician, and encounter characteristics.
Outcomes & Measurements
We described the occurrence and characteristics (content, use of technical terms, and physician assessment of patient comprehension of new concepts) of CKD discussions. We assessed patient and physician characteristics associated with CKD discussion occurrence.
Results
Many patients (mean age, 59 years) had uncontrolled hypertension (51%), diabetes (44%), and/or 3 or more comorbid conditions (51%). Most primary care physicians practiced (52%) fewer than 10 years. CKD discussions occurred in few (26%; n = 61) encounters, with content focused on laboratory assessment (89%), risk-factor treatment (28%), and causes (26%) of CKD. In encounters that included a CKD discussion, physicians used technical terms (28%; n = 17) and rarely assessed patients’ comprehension (2%; n = 1). CKD discussions were statistically significantly less common in visits of patients with some (vs no) college education (OR, 0.23; 95% CI, 0.09–0.56), with 3 or more (vs fewer) comorbid conditions (OR, 0.49; 95% CI, 0.25–0.96), and who saw physicians with more (vs fewer) than 10 years of practice experience (OR, 0.41; 95% CI, 0.21–0.80). CKD discussions were more common during longer encounters (OR, 1.31; 95% CI, 1.04–1.65) and encounters in which diabetes was (vs was not) discussed (OR, 2.87; 95% CI, 1.22–6.77).
Limitations
Generalizability of our findings may be limited.
Conclusions
Patient-physician discussions about CKD in high-risk primary care patients were infrequent. Physicians used technical terms and infrequently assessed patients’ understanding of new CKD concepts. Efforts to improve the frequency and content of patient-physician CKD discussions in primary care could improve patients’ clinical outcomes.
INDEX WORDS: Chronic kidney disease, primary care, patient-physician communication, patient awareness
A significant majority of patients at risk of the development or progression of chronic kidney disease (CKD) have poor knowledge and inaccurate perceptions of their CKD risk.1–5 Patient-physician discussions about CKD have been widely advocated as an important means through which patients’ knowledge and awareness of CKD risk could be improved. Patients’ enhanced knowledge and awareness of CKD risk are postulated to encourage their enhanced engagement in self-management behaviors (ie, adherence to prescribed medications for CKD risk factors and avoidance of nephrotoxins) that are associated with improved clinical outcomes.5–8 Because primary care physicians care for most patients with risk factors for CKD incidence or progression, patient-physician discussions during primary care clinical encounters represent an important venue through which effective communication about patients’ CKD risks could occur.
Recently, programs such as the National Institutes of Health’s National Kidney Disease Education Program have sought to enhance patients’ awareness and knowledge regarding ways to mitigate their CKD risks in part by providing primary care physicians with tools to enhance their discussions with patients about CKD.9,10 However, very little is known about the occurrence of CKD discussions in primary care or the adequacy of discussions with regard to enhancing patients’ knowledge and awareness of their CKD risks. Characterization of patient-physician discussions occurring in primary care in patients at risk of CKD incidence or progression could greatly inform efforts to improve patients’ knowledge and awareness of their CKD risks and, in turn, contribute to improving their clinical outcomes.
In a study of patients at risk of CKD incidence or progression, we assessed the prevalence, characteristics, and determinants of patient-physician discussions about CKD during routine primary care visits.
METHODS
Study Design and Population
As part of a randomized controlled trial of patient and physician behavioral interventions to improve blood pressure management in primary care, we assessed the prevalence, characteristics, and determinants of CKD discussions occurring between patients at risk of CKD incidence or progression and their primary care physicians. We hypothesized that the prevalence of CKD discussions in primary care would be low and would vary based on patient, physician, and visit characteristics. The Patient-Physician Partnership (Triple P) Study was a randomized controlled trial with a 2 × 2 factorial design to evaluate the effectiveness of a patient and physician behavioral intervention, both separately and in combination, in improving patients’ adherence to appointments, medication, and lifestyle recommendations compared with minimal intervention groups. The detailed eligibility criteria, recruitment methods, and interventions have been published previously.11
Briefly, study participants included 50 primary care physicians (family physicians or internists enrolled between January 2002 and January 2003) recruited from 15 primary care practices in the Baltimore, MD, metropolitan area and 279 of their patients (enrolled between September 2003 and August 2005). Eligible primary care physicians had to engage in patient care at least 20 hours weekly. Eligibility criteria for patients were defined as aged 18 years or older and an International Classification of Diseases, Ninth Revision, Clinical Modification diagnosis of hypertension (401.00–401.9) in the preceding year.
Baseline patient assessment in Triple P included audiotaping of a single clinical encounter between each patient with hypertension and his or her primary care physician. Because of technical and logistical issues, 43 patients did not obtain an audiotaped encounter. Our analysis of the prevalence, determinants, and quality of CKD discussions during these encounters is limited to 236 enrolled patients (85%) for whom audiotaped data were available. The study was approved by the Johns Hopkins Institutional Review Board.
Data Collection
At baseline, patient participants completed an in-depth interview to assess demographics, self-reported medical history, and health literacy, as well as a brief physical examination to assess blood pressure. As part of an ancillary study within Triple P, estimated glomerular filtration rate and urine albumin-creatinine ratio were assessed at the 3- and/or 12-month visit. Because the ancillary study began when data collection for the 3-month visit was underway, blood or urine studies were obtained for only a subsample of participants (n = 119) included in this analysis. Physician participants completed a questionnaire to assess demographics and practice experience at baseline.
Concurrent with study enrollment for each patient, a single routine clinical encounter (index visit) with the primary care provider was audiotaped. All other medical care was continued during the visit per routine. The audiotaped encounter occurred after delivery of the physician intervention and after the first stage of the patient intervention. The physician intervention was a 2-hour continuing medical education training program designed to improve physicians’ communication skills. The patient intervention included a 20-minute previsit coaching session by a community health worker (to improve patient-provider communication and patient engagement in care) immediately before the patients’ index visit with his or her physician, as well as five 15-minute telephone calls with the community health worker during 12 months of study follow-up. Patients also received printed materials discussing challenges in hypertension self-management during study follow-up.
Assessment of Patient and Physician Characteristics
We assessed patients’ demographic characteristics, health literacy (measured using the Rapid Estimate of Adult Literacy in Medicine),12 self-reported medical history, and burden of comorbid medical conditions (defined as number of medical conditions participants reported in addition to hypertension). To assess patients’ awareness of their CKD status, we asked patients, “Do you currently have kidney failure?” We ascertained blood pressure by using the average of 3 measurements obtained using an automatic oscillometric monitor programmed for a 5-minute delay before activation with a 30-second delay between the triplicate measurements. We defined blood pressure as controlled if the average of the 3 measurements at baseline was systolic/diastolic blood pressure <130/80 mm Hg for patients with diabetes or <140/90 mm Hg for patients without diabetes. For participants from whom blood and urine were obtained, we defined CKD as estimated glomerular filtration rate <60 mL/min/1.73 m2 (<1.0 mL/s/1.73 m2), estimated using the Modification of Diet in Renal Disease (MDRD) Study equation,13 or the presence of microalbuminuria, assessed using a modified Jaffé method (urine albumin-creatinine ratio >30 mg albumin/g creatinine) at the 3- or 12-month visit. We also assessed physicians’ sex and years in practice.
Assessment of Patient-Physician Communication Patterns
We assessed patterns of patient-physician communication throughout each audiotaped encounter and characterized the content of discussions focusing on CKD. To assess patient-physician communication, we transcribed and analyzed audiotapes using the Roter Interaction Analysis System, an extensively used coding system with established reliability and predictive validity in characterizing patient-physician communication.14,15 Each complete thought expressed by a physician or patient was coded by 2 trained raters (who were blinded to the study hypothesis) into 1 of 37 mutually exclusive and exhaustive categories of communication. These categories can be used individually or combined in a variety of ways to summarize the communication that occurs during an encounter, including categories such as data gathering (open and closed-ended biomedical and psychosocial questions), patient education and counseling (biomedical and psychosocial information giving and counseling), and relationship building through emotionally responsive exchange (empathy, concern, approval, and reassurance). In addition, other features of the physician and patient communication can be calculated, such as number of times a topic is discussed and total amount of patient or physician talk during the encounter.
In this study, we categorized the content of patient-physician discussions pertaining to diabetes, hypertension, medication adherence, or CKD during visits. Categories were not mutually exclusive. For example, a patient-physician discussion about the risk of CKD due to diabetes would be categorized as both a visit with a patient-physician discussion about diabetes and about CKD. We also assessed clinical encounters’ duration, time dedicated to patient education and counseling, patient-centeredness of encounters, and physician verbal dominance. We determined patient-centeredness of encounters by dividing the sum of codes that promoted the socioemotional and psychosocial agenda of patients during encounters, including patient questions of any topic, by the sum of codes related to the biomedical agenda of the physicians (eg, all biomedical and procedural statements made by patients and physicians). Scores >1 indicate a more patient-centered encounter.16 Because most encounters had a patient-centeredness score <1, we classified encounters as having greater versus less patient-centeredness (dichotomized at the median score for patient-centeredness across all encounters). We calculated physician verbal dominance during encounters by dividing the total amount of physician statements by the total amount of patient statements.16 Scores >1 indicate more physician statements and scores <1 indicate more patient statements. Because most encounters had verbal dominance scores >1, we classified encounters as having greater versus less physician verbal dominance (dichotomized at the median score for verbal dominance across all encounters).
We identified all patient-physician communication related to CKD (ie, included terms such as kidney, creatinine, or proteinuria) and characterized both the content and intensiveness of discussions. We categorized content of CKD discussions as pertaining to: (1) laboratory tests assessing kidney function or damage; (2) the presence of risk factors for CKD incidence or progression, such as diabetes or hypertension; (3) treatment to ameliorate kidney damage, such as angiotensin-converting enzyme inhibitors or treatment of risk factors for CKD; and (4) clinical complications of CKD, such as anemia or bone disease. We also ascertained the frequency of physicians’ assessment of patients’ needs regarding CKD education (eg, questions assessing patients’ existing knowledge about CKD during encounters; eg, “What do you know about kidney disease?”). Using the framework of the interactive communication loop described by Schillinger et al,17 we quantified the frequency of physicians’ assessments of patients’ recall and/or understanding of new concepts related to CKD introduced during encounters (eg, asking patients to repeat concepts or asking, “Do you have any questions?”). We assessed physicians’ use of unclarified technical terms during CKD discussions (defined as clinical or technical terms that the physician did not define for the patient). We considered CKD discussions consisting of more than 2 sentences uttered by the physician to be ”more (vs less) intensive.” We also assessed patients’ participation in CKD discussions (ie, patients’ initiation of discussions or asking questions related to CKD).
Statistical Analysis
We described the occurrence and content of CKD discussions during encounters and assessed associations between the presence of CKD discussions and patient, physician, encounter, and communication characteristics. In the subsample of patients with blood and urine samples, we performed bivariate (χ2 and t test) analyses to assess differences in patient, physician, and encounter characteristics and the presence of CKD discussions between patients with and without clinical evidence of CKD. In sequential multivariable logistic regression models, we assessed independent patient, physician, encounter, and communication characteristics associated with the occurrence (vs absence) of CKD discussions during encounters in participants with complete data for all variables. Multivariable analysis controlled for the intervention status of patients and physicians and accounted for clustering of patients within physicians using a generalized estimating equation.18 Our models included variables statistically significant in unadjusted analyses and variables hypothesized to be directly related to the occurrence of CKD discussion during visits (physician experience and encounter patient-centeredness). We also performed random-effects multivariable logistic regression incorporating the same variables to assess and account for variability in physicians’ propensity for CKD discussion (random effects assumed to follow a normal distribution with variance G).19 We performed all statistical analyses using Stata, version 11 (StataCorp, www.stata.com).
RESULTS
Participant Characteristics
Of 236 patients with hypertension who had an audiotaped encounter, most (mean age, 59 years) were African American, were women, had a high school reading level, and did not have a college education (Table 1). More than half the patients had uncontrolled blood pressure and were obese. Nearly half the patients had diabetes and 3 or more comorbid conditions. Of 40 primary care physicians, most were women and practiced fewer than 10 years. Each physician saw an average of 6 patients included in this analysis. In patients in whom CKD status was assessed, the presence of diabetes and greater than 2 comorbid conditions were more common in those with (vs without) CKD (P = 0.03 and P = 0.04, respectively). Patients with CKD also were older than patients without CKD (P = 0.001). There were no statistically significant differences in patient demographics (including age, sex, race, and education level), health literacy, or health status (including the presence of diabetes, number of comorbid illnesses, and blood pressure control) between patients with versus without an audiotaped encounter.
Table 1.
Patient and Physician Characteristics
| All (N = 236) | Without Laboratory Results (n = 117) | With Laboratory Results (n = 119)
|
||
|---|---|---|---|---|
| CKD (n = 45) | No CKD (n = 74) | |||
| Patient Characteristics | ||||
| Mean age (y)a | 59 ± 13 | 57 ± 14 | 66 ± 12 | 58 ± 12 |
| Sex | ||||
| Female | 156 (66) | 80 (68) | 29 (64) | 47 (64) |
| Male | 80 (34) | 37 (32) | 16 (36) | 27 (36) |
| Race | ||||
| White | 90 (38) | 51 (44) | 17 (38) | 22 (30) |
| African American | 141 (60) | 63 (54) | 28 (62) | 50 (68) |
| Other | 5 (2) | 3 (3) | 0 (0) | 2 (3) |
| Education | ||||
| No college | 172 (73) | 86 (74) | 34 (76) | 52 (70) |
| Some college | 64 (27) | 31 (26) | 11 (34) | 22 (30) |
| Health literacy | ||||
| REALM ≥9th grade | 147 (63) | 71 (61) | 27 (61) | 49 (67) |
| REALM <9th grade | 86 (37) | 45 (39) | 17 (39) | 24 (33) |
| Income | ||||
| ≥$35,000 | 65 (32) | 29 (28) | 15 (39) | 21 (32) |
| <$35,000 | 141 (68) | 73 (72) | 23 (61) | 45 (68) |
| BP statusb | ||||
| Controlled | 113 (49) | 52 (46) | 20 (45) | 41 (55) |
| Uncontrolled | 117 (51) | 60 (54) | 24 (55) | 33 (45) |
| Diabetesa | ||||
| Present | 102 (44) | 43 (37) | 28 (64) | 31 (42) |
| Absent | 131 (56) | 73 (63) | 16 (36) | 42 (58) |
| Comorbid illnessesa | ||||
| ≥3 | 117 (51) | 57 (50) | 28 (64) | 32 (44) |
| <3 | 114 (49) | 58 (50) | 16 (36) | 40 (56) |
| Median eGFR (mL/min/1.73 m2) | 60 (49,90) | 90 (76,106) | ||
| Median UACR (mg/g) | 58 (15,140) | 6 (3,10) | ||
| Physician Characteristics (n = 40) | ||||
| Sex | ||||
| Female | 21 (52) | |||
| Male | 19 (48) | |||
| Time in practice (y) | ||||
| <10 | 21 (52) | |||
| ≥10 | 19 (48) | |||
Note: Unless otherwise indicated, values are shown as number (percentage), mean ± standard deviation, or median (25th, 75th percentile). Because of missing values, categorical frequencies may not equal column total. Conversion factors for units: eGFR in mL/min/1.73 m2 to mL/s/1.73 m2, ×0.01667. No conversion necessary for UACR.
Abbreviations: BP, blood pressure; CKD, chronic kidney disease; eGFR, estimated glomerular filtration rate; REALM, Rapid Assessment of Adult Literacy in Medicine; UACR, urine albumin-creatinine ratio.
P < 0.05 between the CKD versus no-CKD group.
Blood pressure defined as controlled if <130/80 mm Hg for patients with diabetes and <140/90 mm Hg for patients without diabetes.
Occurrence and Characteristics of Patient-Physician Discussions About CKD
In the 236 patient-physician encounters, mean encounter length was 16.4 ± 8.9 (standard deviation) minutes, and mean proportion of the visit dedicated to education and counseling was 44% ± 12%. For most encounters, physicians spoke most of the time (median verbal dominance ratio, 1.37; 25th–75th percentile, 1.08–1.99), and communication was not patient centered (median score, 0.54; 25th–75th percentile, 0.38–0.74).
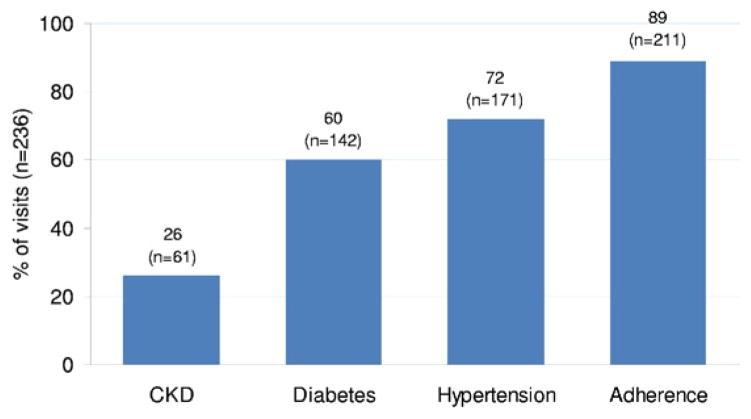
CKD discussions occurred during few (n = 61; 26%) encounters and less frequently than discussions related to diabetes, hypertension, or medication adherence (Fig 1). Content of CKD discussions varied, with most discussions focusing on the laboratory assessment of CKD (89%), followed by treatment of CKD risk factors or prevention of CKD (28%), presence of CKD risk factors (26%), and complications of CKD (5%). Examples of the content of CKD discussions are listed in Table 2. In more than one-quarter (28%) of encounters in which CKD discussion occurred, physicians used technical terms, including “target-organ damage” or “creatinine,” without explanation of their meaning. Moreover, none of the encounters with CKD discussions included an assessment of patients’ educational needs by physicians before CKD discussions and only 2% of encounters included an assessment of patients’ recall and/or understanding of new concepts after CKD discussions. Most CKD discussions (62%) were not intensive (≤2 sentences). In the 61 encounters in which CKD was discussed, few (15%) patients actively participated in CKD discussions.
Figure 1.
Topics of patient-physician discussions. We categorized the content of patient-physician discussions as pertaining to diabetes, hypertension, medication adherence, or chronic kidney disease (CKD) during visits. Categories were not mutually exclusive.
Table 2.
Examples of Content of CKD Discussions
| Category | Comment |
|---|---|
| Content of Physician Statements in CKD Discussions | |
| Laboratory assessmenta | “We are going to check a chemistry level, make sure your kidney function is okay.” |
| “We got some lab work back from last time. We checked your blood count and your blood count was okay and your kidney function tests were okay also. We did another test called the microalbumin. It checks for small proteins that may leak in your urine. It usually gives us an early sign of your body leaking proteins or having problems with your kidneys. And that was a tad high, but not too bad. But you are on medication anyway to try to help that.” | |
| “Your blood work done in April shows that you are not spilling any proteins in the urine. There [are] no proteins being passed in the urine in an abnormal way. So your kidney functions are intact as far as we can say through your blood work and your urine test.” | |
| Treatmentb | “It [losartan] is the kind of medication that protects the kidney” |
| “Your kidney function is abnormal, but it is stable. It hasn’t gotten worse. Your creatinine is 2 and it has been that way for 2–3 years. So you definitely have some damage and the best thing we can do for that is to keep your diabetes and hypertension under good control.” | |
| “You do have chronic kidney disease …. We have you on a thiazide diuretic and an ACE—angiotensin-converting enzyme—inhibitor which has been shown to thwart the progression or slow the progression of kidney decline … to prevent … [you] ever going on dialysis.” | |
| “Looking at your labs, your kidney function, your serum creatinine [is] 1.1 and probably fairly normal for you. It’s 1.1 and how old are you … 68. Your GFR is like 64. Chronic kidney disease stage 2. There is a mild decrease in your kidney function and [the] goal of this is to prevent progression by treating blood pressure …. Hypertension affects your kidney and looking at your kidney function we want to get you at the goal of less than 130/80. Ok? We know that you have hypertension and chronic kidney disease which means … we have to go for a more aggressive goal.” | |
| Risksc | “Diabetes also affects your kidneys” |
| “Remember I told you that your kidney wasn’t functioning so well. It is what we call renal insufficiency. We see this a lot with people who are diabetics and also have high blood pressure. The number is not very high …. We will follow your renal function and see how you do.” | |
| “We know you have essential hypertension. You’ve had it for years. We’ve worked it up. We’ve identified the cause. And we’ll follow you to assess for target organ damage like kidney disease. You already have that. I already said that and we documented that before. We followed your urine in the past. We are trying to get [your blood sugar] better controlled. Hypertension and diabetes are the biggest determinants of keeping your kidneys in good shape to prevent you from going on dialysis.” | |
| “Every time it [your glucose] goes up it damages some part of your body. Either your kidneys are getting damaged or blood vessels all over the body and [it] gets to a point where it is irreversible.” | |
| Complicationsd | “The blood count is a little bit low …. It may well be related to the kidney function. When the kidneys aren’t functioning completely normally. One of the things they do … actually the kidneys create hormone to stimulate your bone marrow to make blood cells. So when the kidneys are not working as well they don’t make that hormone and the bone marrow doesn’t make the blood cell. We can give you that hormone. There is an injection that you give once a week to stimulate it. But if your blood counts is where it is, we’re just gonna to watch it.” |
| Example of Active Patient Participation in CKD Discussion | |
| Active patient participation | Patient: For my blood, what all are you going to check for? |
| Physician: Cholesterol, liver, kidneys, sugar, the muscle enzyme test, the prostate blood test. | |
| Patient: How about a urine test. What is that? Is that for the sugar? | |
| Physician: The urine? | |
| Patient: I haven’t one of those for a while. | |
| Physician: If you haven’t had that we can do that too. | |
Abbreviations: ACE, angiotensin-converting enzyme; CKD, chronic kidney disease; GFR, glomerular filtration rate.
Laboratory assessment: discussion of laboratory tests assessing kidney function or damage.
Treatment: discussion of treatment to ameliorate kidney damage or treatment of risk factors for CKD incidence or progression.
Risks: discussions of presence of risk factors for CKD incidence or progression.
Complications: discussions of clinical complications of CKD.
Determinants of Patient-Physician Discussion of CKD
After adjustment for patient, provider, and visit characteristics, the presence of CKD discussions was less common during encounters with patients who had some (vs no) college education, patients who had 3 or more (vs <3) comorbid conditions, and with physicians practicing 10 years or more (vs <10 years). CKD discussions were more common during longer encounters, encounters in which diabetes was (vs was not) discussed, encounters with greater (vs less) physician verbally dominant communication, and encounters with more (vs less) time dedicated to education and counseling (Table 3). There was no association between blood pressure control and the presence of CKD discussion during visits. Multivariable models accounting for random effects yielded similar estimates. For all 3 models, correlation between patient visits within physician was near zero. Therefore, most of the variation was explained by patient visit–level measures.
Table 3.
Patient, Physician, and Encounter Characteristics Associated With the Presence of CKD Discussions
| Unadjusted
|
Model 1a (patient factors)
|
Model 2b+ Physician Factors
|
Model 3c+ Visit Factors
|
|||||
|---|---|---|---|---|---|---|---|---|
| OR (95% CI) | P | OR (95% CI) | P | OR (95% CI) | P | OR (95% CI) | P | |
| Patient Characteristics | ||||||||
| Age (/y) | 1.03 (1.01–1.05) | 0.01 | 1.03 (1.00–1.05) | 0.03 | 1.04 (1.01–1.06) | 0.01 | 1.03 (1.00–1.06) | 0.05 |
| Education | ||||||||
| Some college | 0.27 (0.12–0.60) | 0.001 | 0.25 (0.11–0.60) | 0.002 | 0.29 (0.12–0.68) | 0.005 | 0.23 (0.09–0.56) | 0.001 |
| No college | Reference | Reference | Reference | Reference | ||||
| Comorbid illness | ||||||||
| ≥3 | 0.61 (0.39–0.98) | 0.04 | 0.55 (0.33–0.91) | 0.02 | 0.60 (0.34–1.04) | 0.07 | 0.49 (0.25–0.96) | 0.04 |
| <3 | Reference | Reference | Reference | Reference | ||||
| Physician Characteristics | ||||||||
| Years in practice | ||||||||
| ≥10 | 0.56 (0.30–1.07) | 0.08 | 0.50 (0.23–1.09) | 0.08 | 0.41 (0.21–0.80) | 0.009 | ||
| <10 | Reference | Reference | Reference | |||||
| Visit Characteristics | ||||||||
| Length (/5 min) | 1.28 (1.04–1.59) | 0.02 | 1.31 (1.04–1.65) | 0.02 | ||||
| Counseling and education time (/10% of visit) | 1.37 (1.03–1.82) | 0.03 | 1.48 (1.17–1.87) | 0.001 | ||||
| Diabetes discussion | ||||||||
| Present | 2.52 (1.33–4.77) | 0.004 | 2.87 (1.22–6.77) | 0.02 | ||||
| Absent | Reference | Reference | ||||||
| Communication Characteristics | ||||||||
| Physician verbal dominance | ||||||||
| High | 1.96 (1.13–3.41) | 0.02 | 1.86 (1.03–3.33) | 0.04 | ||||
| Low | Reference | Reference | ||||||
| Patient centered | ||||||||
| High | 1.36 (0.73–2.54) | 0.3 | 2.37 (0.98–5.72) | 0.06 | ||||
| Low | Reference | Reference | ||||||
Note: Values shown are for a CKD discussion in a primary care visit. A total of 220 participants with complete data were included in the models. All models were adjusted for the intervention status of patients and physicians. Patients’ sex, race, income, health literacy, blood pressure control, and diabetes status and physicians’ sex were not associated with the presence of CKD discussions during visits in unadjusted analyses.
Abbreviations: CI, confidence interval; CKD, chronic kidney disease; OR, odds ratio.
Model 1 adjusted for patient factors (age, education, and comorbid illness).
Model 2 adjusted for all variables in model 1 and physicians’ years in practice.
Model 3 adjusted for all variables in models 1 and 2 and visit (length, proportion dedicated to education and counseling, and presence of diabetes discussion) and communication (physician verbal dominance and patient-centeredness) characteristics.
Of patients with assessment of CKD using blood and urine tests (n = 119), 38% had CKD. At baseline, only 4 of these patients self-reported kidney failure. CKD discussions were not more common during encounters of patients with versus without CKD (33% vs 24%; P = 0.3). Characteristics of CKD discussions in this subgroup were similar to those for the entire study population.
DISCUSSION
In this population of patients at risk of CKD incidence or progression and cared for by primary care physicians, patient-physician discussions were infrequent and focused primarily on laboratory assessment of CKD, rather than enhancing patients’ knowledge and awareness of their risks of CKD. Most discussions were not intensive and frequently consisted of technical terms (ie, medical jargon). No physician assessed patients’ educational needs during encounters and few assessed patients’ understanding of new concepts related to CKD. Patient-physician discussions about CKD were more common during encounters that were longer, included a discussion about diabetes, and primarily were dedicated to education and counseling.
To our knowledge, this is the first study to assess the occurrence and quality of CKD discussions in primary care. These findings emphasize the need to improve the quality of patient-physician discussions about CKD during routine primary care encounters to enhance patients’ knowledge and awareness about their CKD risks. Previous studies showing low CKD awareness and knowledge in patients at risk of CKD incidence or progression have not identified the potential contribution of patient-physician communication to awareness or knowledge.2–5 By identifying deficiencies in patient-physician CKD discussions, our findings may aid ongoing efforts seeking to improve patient awareness and knowledge regarding CKD.
Although CKD discussions occurred infrequently, discussions of the most common CKD risk factors, hypertension and diabetes, occurred much more frequently. Campaigns seeking to increase rates of patient-physician CKD discussions might be most effective if they emphasize the pairing of discussions about CKD with discussions about these highly prevalent risk factors. For example, while discussing the benefits of adherence to antihypertension medication therapy with patients, physicians also might mention the benefits of adherence on decreasing the risk of CKD or slowing CKD progression. To help encourage patient involvement in discussions about CKD, our findings suggest that emphasis should be placed on physicians’ more frequent ascertainment of patients’ knowledge of CKD before discussions and their more frequent assessment of patients’ understanding of new concepts introduced during CKD discussions. Efforts to provide physicians with tools to aid CKD discussions, for example, tools providing physicians with model terms, could help them avoid using confusing technical terms during discussions.
Both physician- and system-level barriers may contribute to poor-quality discussions about CKD in primary care. Previous research has shown that primary care physicians frequently lack knowledge regarding CKD.20–23 Although we did not assess physicians’ knowledge of CKD in this study, our finding that physicians who were closer to their training years were more likely to discuss CKD suggests recent efforts to enhance primary care physician education about CKD may have been effective in enhancing physicians’ willingness and competence to engage in discussions about CKD. As shown in other studies, system constraints, such as the amount of time allotted for visits, also are likely to have a role in the frequency and quality of patient-physician discussions.24,25 Because of limited time, physicians must prioritize education topics and may focus on active issues, such as improving blood pressure and diabetes control rather than CKD. Although our findings did not show a relation between control of CKD risk factors and discussion of CKD, our findings showed more frequent CKD discussions in encounters with longer length and more time dedicated to education and counseling. Efforts to align system factors (eg, payment incentives) that influence physicians’ time spent engaging in education and counseling could help primary care physicians better accommodate patients’ educational needs.
Our study has limitations. First, a single audiotaped clinical encounter may not reflect prior patient-physician discussions of CKD or physicians’ future plans for CKD discussions. However, our findings are consistent with other research, which describes low awareness and knowledge of CKD in patients with hypertension or diabetes and physician barriers to CKD management in primary care (ie, low knowledge).3,4,21,26 We did not assess whether some patients were already seeing nephrologists. It is possible that primary care physicians caring for patients seen by nephrologists deferred CKD discussions to specialty care. Second, the generalizability of our findings, derived from a regional randomized controlled trial of primarily low income and African American patients and conducted in 2003–2005, may be limited. Physicians’ initiation of CKD discussions could vary based not only on the prevalence of CKD risk factors in patients seen in their practices, but also on their recent exposure to campaigns emphasizing the importance of CKD education. Although we controlled for intervention assignments in our analysis, our findings may not reflect rates of patient-physician discussion of CKD in standard practice. In addition, it is possible that patients’ and physicians’ awareness of being tape recorded during encounters biased their communication. However, a prior study of performance bias showed that recordings of clinical encounters have limited systematic effect on communication behaviors of physicians.27 Finally, the low frequency of CKD discussions observed in this study might limit our ability to generalize observations regarding the content of CKD discussions. However, we believe that our observation of more than 200 patient-physician encounters provided a reasonable opportunity to assess the frequency of CKD discussions relative to discussions of other clinical conditions. Our findings also provide insight into potential areas of discussions that can be targeted for improvement. Specifically, our findings highlight the potential importance of encouraging more patient-physician discussions regarding patients’ risk and prevention of CKD incidence or progression.
In conclusion, patient-physician discussions of CKD occurred infrequently in patients at risk of CKD incidence or progression seen in primary care practices. Efforts to improve patients’ CKD awareness and knowledge might be most helpful if focused on integrating the discussion of CKD with that of common CKD risk factors, such as hypertension and diabetes. Efforts to improve physicians’ communication skills (ie, assessing patients’ understanding of new concepts discussed), tools helping physicians minimize their use of technical terms, and provision of time for CKD discussions during clinical encounters also may enhance the quality of CKD discussions.
Acknowledgments
We thank Gayane Yenokyan for statistical support.
Support: Dr Cooper was supported by grants R01HL069403 and K24HL083113 from the National Heart Lung and Blood Institute and Contract 200609197 from Amgen; Dr Greer, by a National Research Service Award (5 T32 HL007180) and Research Supplement to Promote Diversity in Health-Related Research (grant R01DK079682) from the National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK); Dr Crews, by Amos Medical Faculty Development Award of the Robert Wood Johnson Foundation; Dr Boulware, by grant K23DK070757 from the National Center for Minority Health and Health Disparities and the NIDDK and contract 200609197 from Amgen; Dr Powe, by grant K240502643 from NIDDK and Foundation for Informed Medical Decision Making.
Footnotes
Financial Disclosure: The authors declare that they have no relevant financial interests.
References
- 1.Boulware LE, Carson KA, Troll MU, Powe NR, Cooper LA. Perceived susceptibility to chronic kidney disease among high-risk patients seen in primary care practices. J Gen Intern Med. 2009;24(10):1123–1129. doi: 10.1007/s11606-009-1086-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Finkelstein FO, Story K, Firanek C, et al. Perceived knowledge among patients cared for by nephrologists about chronic kidney disease and end-stage renal disease therapies. Kidney Int. 2008;74(9):1178–1184. doi: 10.1038/ki.2008.376. [DOI] [PubMed] [Google Scholar]
- 3.Waterman AD, Browne T, Waterman BM, Gladstone EH, Hostetter T. Attitudes and behaviors of African Americans regarding early detection of kidney disease. Am J Kidney Dis. 2008;51(4):554–562. doi: 10.1053/j.ajkd.2007.12.020. [DOI] [PubMed] [Google Scholar]
- 4.Plantinga LC, Boulware LE, Coresh J, et al. Patient awareness of chronic kidney disease: trends and predictors. Arch Intern Med. 2008;168(20):2268–2275. doi: 10.1001/archinte.168.20.2268. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Plantinga LC, Tuot DS, Powe NR. Awareness of chronic kidney disease among patients and providers. Adv Chronic Kidney Dis. 2010;17:225–236. doi: 10.1053/j.ackd.2010.03.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Curtin RB, Becker B, Kimmel PL, Schatell D. An integrated approach to care for patients with chronic kidney disease. Semin Dial. 2003;16(5):399–402. doi: 10.1046/j.1525-139x.2003.16082.x. [DOI] [PubMed] [Google Scholar]
- 7.Bakris GL, Ritz E World Kidney Day Steering Committee. The message for World Kidney Day 2009: hypertension and kidney disease: a marriage that should be prevented. J Clin Hypertens (Greenwich) 2009;11(3):144–147. doi: 10.1111/j.1751-7176.2009.00092.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Beaulieu M, Levin A. Analysis of multidisciplinary care models and interface with primary care in management of chronic kidney disease. Semin Nephrol. 2009;29(5):467–474. doi: 10.1016/j.semnephrol.2009.06.003. [DOI] [PubMed] [Google Scholar]
- 9.Narva AS, Briggs M. The National Kidney Disease Education Program: improving understanding, detection, and management of CKD. Am J Kidney Dis. 2009;53(3 suppl 3):S115–S120. doi: 10.1053/j.ajkd.2008.05.038. [DOI] [PubMed] [Google Scholar]
- 10.McGill JB, Brown WW, Chen SC, Collins AJ, Gannon MR Kidney Early Evaluation Program (KEEP) Findings from a community screening program. Diabetes Educ. 2004;30(2):196–198. 200–202, 206. doi: 10.1177/014572170403000209. [DOI] [PubMed] [Google Scholar]
- 11.Cooper LA, Roter DL, Bone LR, et al. A randomized controlled trial of interventions to enhance patient-physician partnership, patient adherence and high blood pressure control among ethnic minorities and poor persons: study protocol NCT00123045. Implement Sci. 2009;4:7. doi: 10.1186/1748-5908-4-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Davis TC, Crouch MA, Long SW, et al. Rapid assessment of literacy levels of adult primary care patients. Fam Med. 1991;23(6):433–435. [PubMed] [Google Scholar]
- 13.Levey AS, Bosch JP, Lewis JB, Greene T, Rogers N, Roth D. A more accurate method to estimate glomerular filtration rate from serum creatinine: a new prediction equation. Modification of Diet in Renal Disease Study Group. Ann Intern Med. 1999;130(6):461–470. doi: 10.7326/0003-4819-130-6-199903160-00002. [DOI] [PubMed] [Google Scholar]
- 14.Roter D, Larson S. The Roter Interaction Analysis System (RIAS): utility and flexibility for analysis of medical interactions. Patient Educ Couns. 2002;46(4):243–251. doi: 10.1016/s0738-3991(02)00012-5. [DOI] [PubMed] [Google Scholar]
- 15.Roter DL, Larson S. The relationship between residents’ and attending physicians’ communication during primary care visits: an illustrative use of the Roter Interaction Analysis System. Health Commun. 2001;13(1):33–48. doi: 10.1207/S15327027HC1301_04. [DOI] [PubMed] [Google Scholar]
- 16.Cooper LA, Roter DL, Johnson RL, Ford DE, Steinwachs DM, Powe NR. Patient-centered communication, ratings of care, and concordance of patient and physician race. Ann Intern Med. 2003;139(11):907–915. doi: 10.7326/0003-4819-139-11-200312020-00009. [DOI] [PubMed] [Google Scholar]
- 17.Schillinger D, Piette J, Grumbach K, et al. Closing the loop: physician communication with diabetic patients who have low health literacy. Arch Intern Med. 2003;163(1):83–90. doi: 10.1001/archinte.163.1.83. [DOI] [PubMed] [Google Scholar]
- 18.Liang KY, Zeger SL. Regression analysis for correlated data. Annu Rev Public Health. 1993;14:43–68. doi: 10.1146/annurev.pu.14.050193.000355. [DOI] [PubMed] [Google Scholar]
- 19.Skrondal A, Rabe-Hesketh S. Generalized Latent Variable Modeling: Multilevel, Longitudinal, and Structural Equation Models. Washington, DC: Chapman & Hall/CRC; 2004. [Google Scholar]
- 20.Charles RF, Powe NR, Jaar BG, Troll MU, Parekh RS, Boulware LE. Clinical testing patterns and cost implications of variation in the evaluation of CKD among US physicians. Am J Kidney Dis. 2009;54(2):227–237. doi: 10.1053/j.ajkd.2008.12.044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Israni RK, Shea JA, Joffe MM, Feldman HI. Physician characteristics and knowledge of CKD management. Am J Kidney Dis. 2009;54(2):238–247. doi: 10.1053/j.ajkd.2009.01.258. [DOI] [PubMed] [Google Scholar]
- 22.Fox CH, Brooks A, Zayas LE, McClellan W, Murray B. Primary care physicians’ knowledge and practice patterns in the treatment of chronic kidney disease: an Upstate New York Practice-Based Research Network (UNYNET) Study. J Am Board Fam Med. 2006;19(1):54–61. doi: 10.3122/jabfm.19.1.54. [DOI] [PubMed] [Google Scholar]
- 23.Agrawal V, Ghosh AK, Barnes MA, McCullough PA. Awareness and knowledge of clinical practice guidelines for CKD among internal medicine residents: a national online survey. Am J Kidney Dis. 2008;52(6):1061–1069. doi: 10.1053/j.ajkd.2008.06.022. [DOI] [PubMed] [Google Scholar]
- 24.Chen LM, Farwell WR, Jha AK. Primary care visit duration and quality: does good care take longer? Arch Intern Med. 2009;169(20):1866–1872. doi: 10.1001/archinternmed.2009.341. [DOI] [PubMed] [Google Scholar]
- 25.Wilson IB, Kaplan S. Physician-patient communication in HIV disease: the importance of patient, physician, and visit characteristics. J Acquir Immune Defic Syndr. 2000;25(5):417–425. doi: 10.1097/00042560-200012150-00006. [DOI] [PubMed] [Google Scholar]
- 26.Crews DC, Plantinga LC, Miller ER, III, et al. Prevalence of chronic kidney disease in persons with undiagnosed or prehypertension in the United States. Hypertension. 2010;55(5):1102–1109. doi: 10.1161/HYPERTENSIONAHA.110.150722. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Pringle M, Stewart-Evans C. Does awareness of being video recorded affect doctors’ consultation behaviour? Br J Gen Pract. 1990;40(340):455–458. [PMC free article] [PubMed] [Google Scholar]