Abstract
The TLR7/8 agonist, Resiquimod has been used as an immune adjuvant in cancer vaccines. We evaluated the safety and immunogenicity of the cancer testis antigen NY-ESO-1 given in combination with Montanide with or without Resiquimod in high-risk melanoma patients. In Part I of the study, patients received 100ug full length NY-ESO-1 protein emulsified in 1.25mL Montanide (day 1) followed by topical application of 1000mg of 0.2% Resiquimod gel on days 1 and 3 (Cohort 1) versus days 1, 3, and 5 (Cohort 2) of a 21 day cycle. In Part II, patients were randomized to receive 100ug NY-ESO-1 protein plus Montanide (day 1) followed by topical application of placebo gel (Arm-A; N=8) or 1000mg of 0.2% Resiquimod gel (Arm-B; N=12) using the dosing regimen established in Part I. The vaccine regimens were generally well-tolerated. NY-ESO-1-specific humoral responses were induced or boosted in all patients, many of whom had high titer antibodies. In Part II, 16 of 20 patients in both arms had NY-ESO-1-specific CD4+ T-cell responses. CD8+ T-cell responses were only seen in 3 of 12 patients in Arm B. Patients with TLR7 SNP rs179008 had a greater likelihood of developing NY-ESO-1-specific CD8+ responses. In conclusion, NY-ESO-1 protein in combination with Montanide with or without topical Resiquimod is safe and induces both antibody and CD4+ T-cell responses in the majority of patients; the small proportion of CD8+ T-cell responses suggests that the addition of topical Resiquimod to Montanide is not sufficient to induce consistent NY-ESO-1-specific CD8+ T-cell responses.
INTRODUCTION
NY-ESO-1 is considered widely a suitable tumor antigen for vaccination due to its presence in many tumor types, its highly restricted expression in normal tissues, and the ability to induce strong spontaneous humoral and cellular immune responses (1). In vitro and in vivo studies have shown that NY-ESO-1 is immunogenic with particular regions of the protein specifically targeted by antibodies as well as CD4+ and CD8+ T cells. Although clinical trials have demonstrated that patients have immunity to NY-ESO-1, only a small number of clinical tumor responses have been observed in patients with advanced disease. Induction of integrated immune responses to NY-ESO-1 consisting of humoral and CD4+ and CD8+ T-cell responses correlated with clinical benefit in melanoma patients who received anti-CTLA4-inhibitors (2). Therefore, to achieve effective CD4+ and CD8+ T-cell priming we vaccinated individuals with the full-length recombinant NY-ESO-1 protein and evaluated the addition of toll-like receptor adjuvants to the vaccine.
Toll-like receptors (TLR) are a family of highly conserved transmembrane receptors which recognize specific molecular patterns in microbial components (3). Stimulation of different TLRs induces distinct patterns of gene expression, not only activating innate immunity but also directing adaptive immunity, such as the induction of a T helper 1 (Th1) cell response that is necessary for antitumor immune responses (4). TLR agonists control antigen-presenting cells (APC), in particular dendritic cells (DC), by triggering their maturation program, including up-regulation of the expression of human leukocyte antigen (HLA) and co-stimulatory molecules and secretion of cytokines such as TNFα, IL6, IL12 and IFNα (5). Additionally, animal models have shown that TLR agonists can improve the efficacy of vaccines targeting self antigens by activation of innate immune cells and production of inflammatory cytokines (6) and alter the immunosuppressive function of regulatory T cells (Treg) (7). Consequently, TLR agonists have been recognized as promising vaccine adjuvants and have been developed for use as adjuvants for cancer vaccines in clinical trials (8-10). However, there is a paucity of controlled studies assessing the potency of adding TLR agonists to standard adjuvants such as Montanide.
Previously, we examined the safety and immunogenicity of the topical TLR7 agonist Imiquimod (Aldara®) as an adjuvant to NY-ESO-1 protein vaccination in melanoma patients. Although the vaccine, which was given without Montanide, induced NY-ESO-1-specific antibodies and CD4+ T-cell responses, no detectable CD8+ T-cell responses were observed (11). Therefore, we sought to improve upon the results of the study using another TLR agonist. Resiquimod is a TLR7/8 agonist that is chemically related to Imiquimod but has been shown to stimulate a more potent immune response than Imiquimod (12). In vitro studies using Resiquimod have shown that it can activate DC maturation by increasing costimulatory molecule expression and cytokine production, and skew a Th1 cytokine profile, consequently enhancing humoral and cellular immune responses (13,14). More recently, Resiquimod has been shown to promote cross-presentation of exogenous antigens resulting in the efficient induction of antigen-specific CD8+ T-cell responses (15). Results from animal study have confirmed the ability of Resiquimod to activate DCs (16), bias immune responses towards a predominance of Th1 cells (17), and enhance antigen-specific CD8+ T-cell responses that can inhibit tumor growth (18,19). Therefore, the capacity of Resiquimod to induce local activation of immune cells, stimulate production of proinflammatory cytokines, and enhance antigen-presentation by DCs leading to activation of effective cellular responses are features supporting its potential as a cancer vaccine adjuvant (20).
In this randomized study, we evaluated the safety and immunogenicity of vaccination with NY-ESO-1 protein emulsified in Montanide ISA-51 VG when given with or without Resiquimod in patients with resected stage IIB-IV melanoma. We observed that NY-ESO-1 protein and Montanide when given with or without Resiquimod induced both humoral and cellular immune responses specific for NY-ESO-1 in the majority of vaccinated patients although the induction of statistically significant CD8+ T-cell responses was only observed in a small subset of patients who received Resiquimod.
MATERIALS AND METHODS
Study Design, Patients and Treatment Plan
This is a two-part study with Resiquimod dose-escalation in Part I and randomization to Resiquimod versus placebo in Part II. The primary objectives of the study were safety of the vaccine regimen and assessment of humoral and cellular responses to NY-ESO-1. Patients with histologically confirmed, resected malignant melanoma (American Joint Committee on Cancer (AJCC) stages IIB, IIC, III, and IV) were eligible. Tumor NY-ESO-1 expression was assessed by immunohistochemistry as previously described (21), but was not required for study entry. The study (NCT00821652) was approved by the New York University School of Medicine Institutional Review Board and written informed consent was obtained from all patients prior to enrollment.
In Part I of the study, the safety of 2 different dosing regimens of Resiquimod was assessed in 2 cohorts of 3 patients each. Subjects received four 3-week cycles of subcutaneous (s.c.) injections with 100ug of recombinant human NY-ESO-1 protein (Ludwig Institute for Cancer Research) emulsified in 1.25mL Montanide (Seppic) (day 1) followed by topical application of 1000mg of Resiquimod (3M Pharmaceuticals, 0.2%) gel to the vaccination site on days 1 and 3 (cohort 1) and days 1, 3, and 5 (cohort 2), respectively (Figure 1). In Part II of the study, patients were randomized in a blinded fashion to receive 100ug NY-ESO-1 protein emulsified in 1.25mL Montanide (day1) s.c. followed by topical application of placebo gel (Arm-A; N=8) or 1000mg of 0.2% Resiquimod gel (Arm-B; N=12) on days 1, 3, and 5 as established in Part I (Figure 1). Study arm assignments were unblinded after completion of study and immune monitoring.
Figure 1. Study design.
In Part I of the study, the safety of two different dosing regimens of Resiquimod in two cohorts of three patients each was assessed. Subjects received four 3-week cycles of intradermal (i.d.) injections of 100ug of recombinant human NY-ESO-1 protein emulsified in 1.25mL Montanide (day 1) followed by topical application of 1000mg of Resiquimod (0.2%) gel on days 1 and 3 (cohort 1) and days 1, 3, and 5 (cohort 2), respectively. In Part II of the study, patients were randomized in a blinded fashion to receive an intradermal injection of 100ug NY-ESO-1 protein emulsified in 1.25mL Montanide (day1) followed by topical application of placebo gel (Arm-A; N=8) or 1000mg of 0.2% Resiquimod gel (Arm-B; N=12) as determined in Part I.
Blood Samples
Blood samples were collected at baseline and day 8 of each cycle (Weeks 1, 4, 7, and 10), and during the first follow-up visit at week 12-14. Peripheral blood mononuclear cells (PBMC) were isolated from heparinized blood by Ficoll centrifugation and frozen in aliquots using pooled human serum (90%) and DMSO (10%). Plasma from each time point was also frozen.
Humoral Responses
Patient plasma samples were analyzed by ELISA for seroreactivity against recombinant NY-ESO-1 protein (1 μg/ml) as well as 3 individual overlapping long peptides (68-mers, 1 μM each) covering the NY-ESO-1 sequences as previously described (22). Synthetic long peptides were used to confirm specificity for NY-ESO-1 plasma antibodies and for approximate epitope mapping. A reciprocal titer was calculated for each plasma sample as the maximal dilution still significantly reacting to a specific antigen. This value was extrapolated by determining the intersection of a linear trend regression with a cutoff value. The cutoff was defined as 10 × the average of OD values from the first four dilutions of a negative control pool comprising five healthy donor sera. In each assay, sera of patients with known presence or absence of specific reactivity were used as controls.
Titers >100 were considered reactive, and specificity was determined by comparing reactivity to control antigens and to the NY-ESO-1 peptides.
T-cell Assays
T-cell responses to NY-ESO-1 were evaluated after in vitro stimulations (IVS) with overlapping pools of NY-ESO-1 peptides. T cells were restimulated with the overlapping pools of NY-ESO-1 peptides and then stained for IFNγ, TNFα, and IL2 and analyzed by flow cytometry. IVS were performed with some modifications as described previously (11). PBMCs were thawed and cultured overnight in 5% PHS (Valley Biomedicals) in RPMI (Gibco), then separated into CD4+, CD8+, and CD4−CD8− (APC) fractions using Dynal Beads (Invitrogen). For the CD25-depletion experiments, CD25+ cells were initially depleted from PBMCs prior to positive selection of CD4+ and CD8+ fractions. Each fraction was then washed and resuspended in 5% PHS/RPMI containing 10 U/ml IL2 (R&D Systems) and 10 ng/ml IL7 (R&D Systems). CD4+ and CD8+ cells (500,000 to 1 million cells per well) were co-cultured separately for 14-20 days with APCs stimulated with pooled NY-ESO-1 overlapping peptides covering the NY-ESO-1 protein (1 μg/ml each) in a 96-well round-bottom plate. Medium and cytokines were replenished every 2–3 days.
IVS CD8+ T-cell cultures were tested on day 14 and CD4+ T-cell cultures on day 21 for reactivity to NY-ESO-1 by intracellular cytokine staining (ICS). T-cell cultures were harvested, washed, and re-plated in 5% PHS/RPMI medium in a 96-well V-bottom plate. A pool of all 17 NY-ESO-1 peptides (1 μg/ml each) was added to one of the wells. Control wells containing DMSO, MOG, CMV, and PMA/Ionomycin were included. Epitope mapping was done using individual NY-ESO-1 peptides. For all ICS cultures, plates were incubated for 1 h at 37°C, after which BD GolgiPlug and GolgiStop was added to each well and the cultures incubated for an additional 5 h. Cells were then stained for CD4 and CD8, fixed and permeabilized with BD Cytofix/Cytoperm solution, then washed with 1× BD Perm/Wash buffer and stained for CD3, CD4, CD8, IL2, TNF, IFNγ and Live/Dead Violet. Cells were analyzed on a BD LSR II and BD LSRFortessa flow cytometers using FACSDiva software. Data were analyzed using FlowJo software (TreeStar).
Phenotyping of T cells was performed by staining PBMCs with antibodies to CTLA-4, PD-1, CD25 (all from BD Biosciences), Tim3 (R&D Systems), and FoxP3 (eBioscience) in addition to antibodies to CD3. CD4, CD8 (all from BD Biosciences), and Live/Dead (Invitrogen). Cells were analyzed on BD LSRFortessa flow cytometer using FACSDiva software. Data were analyzed using FlowJo software (TreeStar).
TLR Polymorphisms
Coding sequences were obtained from PBMCs using PCR and Sanger sequencing on genomic DNA. Primers were designed to cover the coding sequences plus at least 10 nucleotides in the intron region on both ends. Primer extension sequencing was performed by GENEWIZ, Inc. (South Plainfield, NJ) using Applied Biosystems BigDye version 3.1. Both forward and reverse strands were sequenced. The reactions were then run on Applied Biosystem's 3730xl DNA Analyzer. The sequencing data were analyzed with Lasergene SeqMan software (DNASTAR, Madison, WI) to detect any mutations compared to the genomic DNA reference sequence.
Statistical Analyses
Linear mixed effects model analyses of repeated measures were used to compare the T-cell responses over time on the placebo (Arm A) and Resiquimod (Arm B). Repeat measurements were obtained from blood drawn on the day of the first vaccine injection, eight days after the first, second, third, and fourth (final) vaccine injection, and 2-4 weeks after the final injection. A first-order autoregressive structure with heterogeneous variances was used for the covariance structure of the residuals. A Mann-Whitney test was used to compare plasma antibody titers at various time points between Arms A and B. An exact logistic regression model was used for comparing the odds of developing NY-ESO-1-specific CD8+ T-cell responses between patients positive for the TLR7 SNP rs179008 and patients who tested negative for this SNP.
RESULTS
Patient characteristics
A total of 6 patients were sequentially enrolled in Part I of the study, 3 patients in each cohort (Figure 1). All patients had resected cutaneous melanoma except for one patient who had resected ocular melanoma. A total of 20 patients were enrolled in Part II of the study. Patients were randomized into two arms – Arm A (Placebo) and Arm B (Resiquimod). All patients had resected malignant melanoma (Table 1). Expression of NY-ESO-1 in the resected tumor was not required for study entry and specimens for immunohistochemical (IHC) analysis were available in only 4 of 6 patients in Part I and 10 of 20 patients in Part II. Consistent with the reported frequencies, one patient in Part I and three in Part II (Arm A (Placebo) = 1, Arm B (Resiquimod) = 3) had tumors that expressed NY-ESO-1 (23).
TABLE 1.
Pretreatment Patient Characteristics
| Phase I | Phase II | |
|---|---|---|
| Sex | ||
| Male | 3 | 12 |
| Female | 3 | 8 |
| Age (years), median (range) | 72 (29-81) | 58 (37-67) |
| AJCC Staging | ||
| IIB | 1 | |
| IIC | ||
| IIIA | 5 | |
| IIIB | 1 | 5 |
| IIIC | 2 | 3 |
| IV | 2 | 6 |
| NY-ESO-1 expression in tumors | 1 | 4 |
Safety
All 26 patients enrolled on study were evaluable for safety. The vaccine combinations were generally well-tolerated. Dose escalation in Part I of the study proceeded as planned with no reported dose-limiting toxicity (DLT). 6 of 6 patients completed all four vaccine injections and gel applications. The dose of Resiquimod used in Cohort 2 (3 × weekly) was chosen for Part II of the study, which proceeded as planned. 19 of the 20 patients completed all four vaccine injections and gel applications. One patient from Part II was removed from the study prior to receiving the fourth and final vaccine injection and gel application due to injection site necrosis (CTAE Grade 3) possibly related to the study drugs. There were no grade 4 or 5 adverse events. The most commonly reported adverse clinical responses were influenza-like symptoms (chills, myalgia, arthralgia, fatigue) and injection site reactions (rash/erythema, granuloma, skin induration) (Table 2).
Table 2.
Toxicity profile
| Toxicity grade |
||||
|---|---|---|---|---|
| Grade 1 and 2 | Grade 3 and 4 | |||
| n | % | n | % | |
| Constitutional | ||||
| Chills | 2 | 8 | 0 | |
| Fatigue | 16 | 62 | 0 | |
| Musculosceletal | ||||
| Arthralgia | 10 | 38 | 0 | |
| Myalgia | 4 | 16 | 0 | |
| Gastrointestinal | ||||
| Emesis | 2 | 8 | 0 | |
| Injection site reactions | ||||
| Injection Site Necrosis | 1 | 4 | ||
| Erythema | 24 | 92 | 0 | |
| Granuloma | 26 | 100 | 0 | |
| Skin Induration | 23 | 89 | 0 | |
| Rash (pruritic) | 24 | 92 | 0 | |
| Rash (non-pruritic) | 6 | 23 | 0 | |
| Urticaria | 18 | 69 | ||
| Neurological | ||||
| Headache | 4 | 15 | 0 | |
| Dizziness | 4 | 15 | 0 | |
NY-ESO-1-Specific Humoral Responses
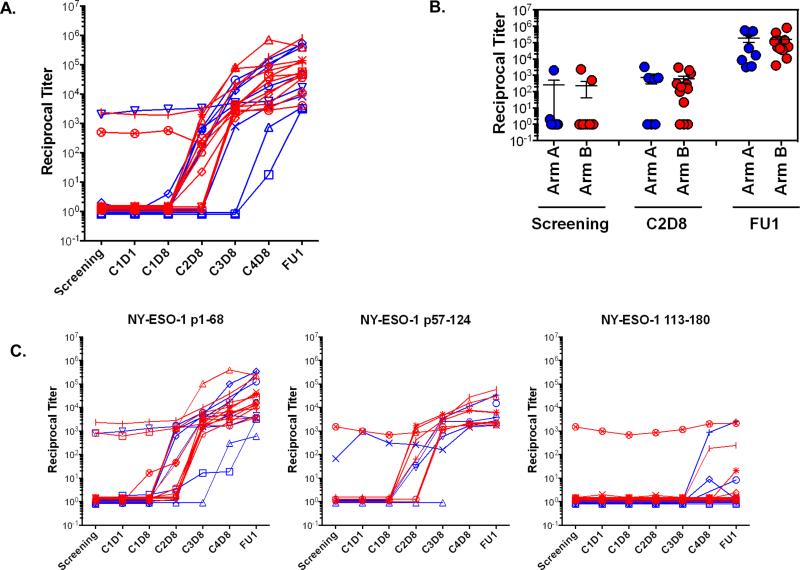
Antibody responses to NY-ESO-1 were induced in all patients who were seronegative prior to vaccination regardless of the presence or dose of Resiquimod (Figure 2A). The majority of patients seroconverted after receiving the second or third vaccine. Antibody titers were not significantly different between patients in Arm A and Arm B at screening, C2D8, and follow up visits (Figure 2B). Pre-treatment antibody responses to NY-ESO-1 were detected in 3 of 20 (15%) patients; and all 3 patients (Arm-A = 1, Arm-B =2) demonstrated substantial increases in antibody titers after vaccination. Only one (Arm B) of 4 patients whose tumors were NY-ESO-1+ had pre-treatment anti-NY-ESO-1 antibodies. This patient had the highest anti-NY-ESO-1 titers after vaccination compared to that of all study patients (Table 3).
Figure 2. NY-ESO-1—Specific Humoral Responses.
A. Plasma collected from patients pre- and post-treatment was analyzed by ELISA for seroreactivity against recombinant NY-ESO-1 protein. Graph shows reactivity for Arm A (blue) and Arm B (red). B. Reciprocal titer comparisons for NY-ESO-1 at screening, C2D8, and follow-up time points for patients in Arm A (blue) and in Arm B (red) showing no statistically significant difference between cohorts by Mann-Whitney unpaired t-test analysis. C. Seroreactivity to specific regions of NY-ESO-1 were mapped using three overlapping peptides covering the entire NY-ESO-1 protein--peptide 1: 1-68, peptide 2: 57-124, and peptide 3: 113-180.
Table 3.
Summary of NY-ESO-1 Antibody Titers, T cell Responses, SNPs, NY-ESO-1 Expression, and Clinical Outcome
| Humoral Response | T cell Responses | TLR SNP Analysis | NY-ESO-1 Expression in Tumor | Clinical Outcome | ||||
|---|---|---|---|---|---|---|---|---|
| Study Arm | PID | Antibody Titer | CD4 | CD8 | TLR 7 rs179008 | TLR 8 rs3764880 | ||
| A | 008 | + | + | - | - | - | ND | AWD |
| A | 009 | ++++ | + | - | - | - | - | deceased |
| A | 012 | + | + | - | - | + | ND | NED |
| A | 016 | ++ | + | - | - | - | ND | deceased |
| A | 018 | ++ | - | - | + | - | ND | Resected-NED |
| A | 020 | ++ | + | - | - | - | + | Lost to Follow Up |
| A | 022 | + | - | - | - | + | ND | NED |
| A | 025 | ++++ | + | - | - | - | ND | deceased |
| B | 007 | ++ | - | - | - | - | ND | deceased |
| B | 010 | + | + | - | - | + | - | NED |
| B | 011 | ++++ | + | + | + | - | + | deceased |
| B | 013 | ++++ | + | + | + | - | - | Resected-NED |
| B | 014 | ++ | + | - | - | + | - | NED |
| B | 015 | ++ | - | - | - | - | - | NED |
| B | 017 | +++ | + | - | - | + | + | Resected-NED |
| B | 019* | +++ | + | - | - | + | - | NED |
| B | 021 | +++ | + | - | - | - | ND | Resected-NED |
| B | 023* | ++++ | + | + | + | - | + | deceased |
| B | 024 | ++ | + | - | - | + | ND | Resected-NED |
| B | 026* | ++ | + | - | - | - | ND | Resected-NED |
NY-ESO-1 Antibody Titers: 1-9,999: +; 10,000-99,999: ++; 100,000-249,000: +++; ≥ 250,000: ++++
pre-vaccine antibody response NY-ESO-1 expression in tumor: ND - not done due to insufficient tumor tissue ; PID: patient identification number
Latest Clinical Outcome: AWD - alive with disease; NED - No Evidence of Disease
Mapping of epitopes recognized by vaccine-induced NY-ESO-1 antibodies was performed by ELISA using 3 overlapping long peptides covering the NY-ESO-1 protein (Peptide 1: 1-68; Peptide 2: 57-124, and Peptide 3: 113-180). As shown in Figure 2C, specific antibody responses induced by the vaccine were detected in all three regions covered by the long peptides in both Arm A and B. Consistent with previous studies, most of these antibody responses mapped to peptides 1 and 2 corresponding to the N-terminal end and central regions of NY-ESO-1 (22).
NY-ESO-1-Specific Cellular Responses
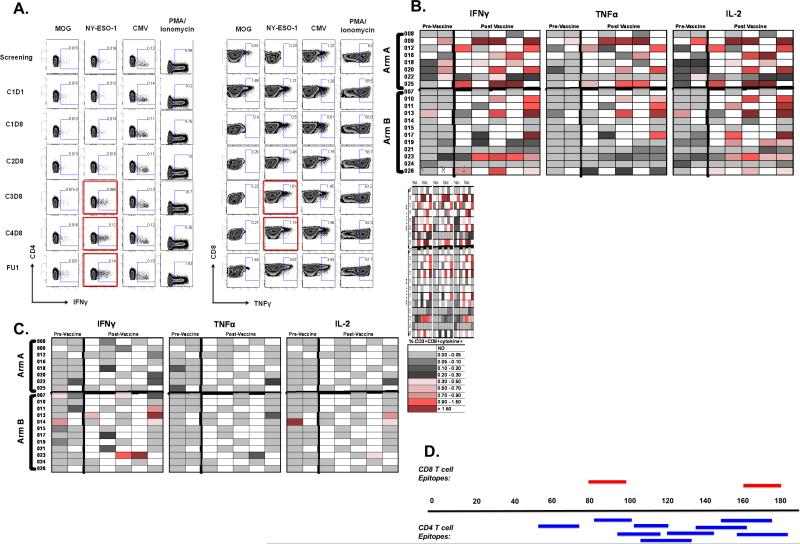
Figure 3A shows representative flow cytometry results after IVS. NY-ESO-1-specific CD4+ T-cell responses were induced in 6 of 8 (75%) patients in Arm A and 10 of 12 (83%) patients in Arm B (Figure 3B). Pre-treatment NY-ESO-1—specific CD4+ T-cell responses were detected in 4 of 8 (50%) patients in Arm A and 2 out of 12 (17%) patients in Arm B; vaccination increased the frequencies of these CD4+ T-cell responses in all patients. In responders, NY-ESO-1—specific CD4+ T cells were detectable after the second and third cycle of vaccination. NY-ESO-1—specific CD8+ T-cell responses were detected in 3 of 12 (25%) patients in Arm B (Figure 3C). Of note, 2 of the patients with NY-ESO-1—specific CD8+ T-cell responses also had tumors with documented NY-ESO-1 expression (Table 3). The majority of NY-ESO-1—specific CD4+ and CD8+ T cells were polyfunctional as they secreted both IFNγ and TNFα with a small proportion also secreting IL2. Results of the mixed model analyses showed that there was no significant difference between study arms for mean changes from baseline to post-treatment evaluations for NY-ESO-1—specific CD4+ and CD8+ T-cell responses.
Figure 3. NY-ESO-1—Specific Cellular Responses.
A. PBMCs were separated into CD4 and CD8 T-cell fractions and in vitro stimulated with NY-ESO-1 overlapping peptides. Responses to NY-ESO-1 were evaluated by intracellular cytokine staining for IFNγ, IL2, and TNF after 14 days for CD8+ T-cell fractions and 21 days for CD4+ T-cell fractions. Patients with NY-ESO-1—specific CD4+ (left) and CD8+ (right) T-cell responses pre- and post-treatment are shown. B, C. Summary of NY-ESO-1—specific CD4+ (B) and CD8+ (C) T-cell responses in study Part II patients pre- and post-vaccination. Top panel shows responses by patients in Arm A and bottom panel shows responses by patients in Arm B. D. NY-ESO-1—specific T-cell responses were mapped using individual overlapping peptides covering the entire NY-ESO-1 protein sequence.
Mapping of reactivity to vaccine-induced T-cell responses using individual peptides showed induction of NY-ESO-1—specific T-cell responses to several peptide epitopes (Figure 3D). Vaccine-induced CD4+ T-cell responses mapped mostly to the central and C-terminal regions of NY-ESO-1 protein, consistent with results from previous studies (11,24). CD4+ T-cell responses to peptides 81-100, 101-120, and 119-143 were detected in several patients (Arm A: 4 of 8 and Arm B: 10 of 12). Although not feasible in all cases due to limited cell quantities, NY-ESO-1—specific CD8+ T-cell responses were mapped to the central and C-terminal region of the protein. More specifically, CD8+ T-cell responses were mapped to peptides 81-100 and 161-180, which is consistent with results from previous studies (24,25).
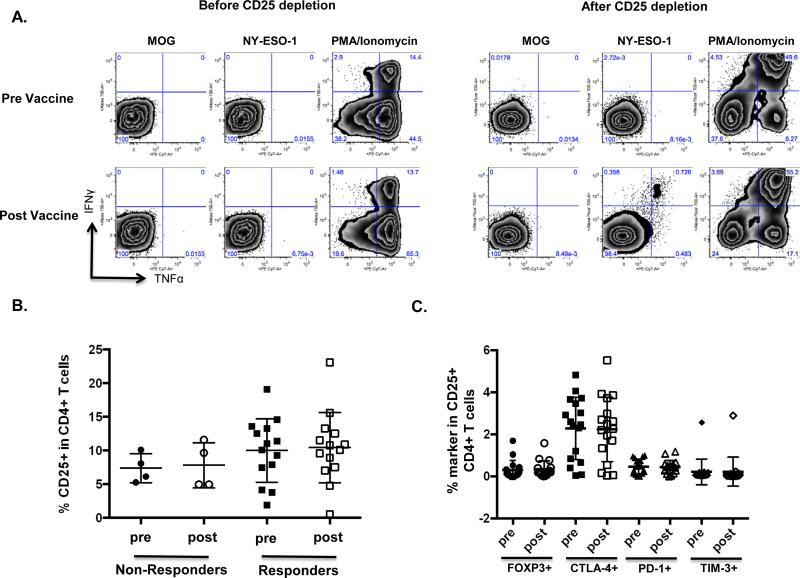
Effect of CD25 Depletion on NY-ESO-1—Specific Cellular Responses
Although designed to induce antigen-specific T-cell responses with effector function, vaccines have also been reported to induce Tregs (26,27). We also considered that circulating Tregs might compromise the induction of antigen-specific T-cell responses as a result of vaccination. To assess these possibilities, we depleted CD25+ cells from bulk PBMCs prior to positive selection of CD4+ and CD8+ T cells and IVS. CD8+ T-cell responses were unmasked in an additional 2 patients (1 of 8 patients in Arm A and 1 of 9 patients in Arm B). CD4+ T-cell responses were unmasked in an additional 4 patients (2 of 2 patients in Arm A and 2 of 2 patients in Arm B). Figure 4A shows a representative example of NY-ESO-1—specific CD4+ T-cell responses in a patient before and after CD25 depletion. The effect of CD25 depletion was not consistent in all patients as some patients had no effect or only slightly amplified responses after CD25 depletion. Interestingly, we also detected NY-ESO-1—specific CD4+ T-cell responses in pre-vaccine samples in 3 of 4 patients in Arm B whose responses became detectable after CD25 depletion.
Figure 4. Effect of CD25 Depletion on NY-ESO-1—Specific Cellular Responses.
A. NY-ESO-1 CD4+ T-cell response in a patient becomes detectable after in vitro CD25 depletion. B. Comparison of % CD25 expression in CD4+ T cells pre- and post-treatment in patients who had detectable NY-ESO-1—specific CD4+ T-cell responses (Responders) vs patients who did not have detectable NY-ESO-1—specific CD4+ T-cell responses (Non-Responders). C. Analysis of potential co-expression of CD25 with CTLA-4, PD-1, Tim-3, and FoxP3 in CD4+ T cells pre- and post-treatment in all patients.
Although CD25 depletion resulted in the ability to detect T-cell responses in a subset of patients, CD25 expression in CD4+ T cells was similarly elevated pre- and post-treatment in patients with detectable NY-ESO-1—specific CD4+ T-cell response as compared to patients with no detectable NY-ESO-1—specific CD4+ T-cell response (Figure 4B). Examination of the CD25-expressing cells revealed that CD25 was co-expressed with CTLA-4 but not with PD-1, TIM-3, and FoxP3 in CD4+ T cells possibly indicative of the specific presence of inhibitory or “exhausted” cells (Figure 4C).
Role of TLR Polymorphisms in Response to Vaccination
Accumulating evidence suggests an important role for single nucleotide polymorphisms (SNP) within TLR genes as determinants of disease susceptibility and severity (28). Furthermore, SNPs may influence response and outcome to vaccination with TLR ligands (29). We investigated the role of TLR7 and TLR8 SNPs in the ability of a patient to respond to the vaccine regimen. Two SNPs in TLR7 (rs179008 and rs864058) and 6 SNPs in TLR 8 (rs3764880, rs2159377, rs5744080, rs2407992, rs3747414, and rs2109135) were detected. Of these 8 SNPs, TLR8 SNP rs3764880 and TLR7 SNP rs179008 were non-synonymous.
The non-synonymous TLR8 SNP rs3764880 was detected in 7 of the 20 (35%) patients in Arm A and B (Table 3). This SNP has been shown to affect the coding region of TLR8, leading to differential activation of NF-κB (30); in addition, it was found to be associated with protection against tuberculosis (31) and increased risk for systemic lupus erythematosus (32). In our study, no association was observed between vaccine-induced immune responses and the presence of SNP rs3764880. The TLR7 SNP rs179008 has been associated with accelerated HIV-1 disease progression (33) and decreased risk for Hodgkin's disease (34). SNP rs179008 was detected in the 3 patients in Arm B who had detectable NY-ESO-1—specific CD8+ T-cell responses and in 1 patient in Arm A who did not have a detectable NY-ESO-1—specific CD8+ T-cell response (Table 3). When adjusted for cohort, the estimated frequency of a CD8+ T-cell response for patients carrying SNP rs179008 were almost 20 times that of patients who did not have this SNP (OR: 19.7, 95% CI 1.11 to 999, p=0.04).
Clinical Outcome
The last clinical follow-up for this study was performed in January 2014. In study Part I, 1 patient has died, 1 patient is alive with disease, 1 patient has undergone further resection and has remained without evidence of disease, and 3 patients have remained without evidence of disease. In Part II of the study, 1 patient was lost to follow-up (Arm A), 5 patients have died (Arm-A = 2, Arm-B = 3), 1 patient is alive with disease (Arm A), 6 patients have undergone further resection and have remained without evidence of disease (Arm-A = 1, Arm-B = 5), and 7 patients have remained without evidence of disease (Arm-A = 3, Arm-B = 4) (Table 3). Analysis of time to progression at the end of the study and at the last follow-up did not reveal any significant differences between study arms.
DISCUSSION
NY-ESO-1 is a commonly expressed tumor-specific antigen that can induce both humoral and cellular immune responses in cancer patients. Studies have evaluated the immunogenicity of NY-ESO-1 antigens in melanoma and other solid tumors in combination with Montanide or/and TLR agonists. Montanide is considered an effective immune adjuvant because of its ability to create a depot effect, which results in slow release of antigens and recruitment of APCs to the injection site. TLR agonists such as Resiquimod (TLR7/8), CpG (TLR9), and poly-ICLC (TLR3) have strong immune adjuvant properties because of their ability to trigger signaling pathways and transcription programs resulting in the activation of key molecules associated with inflammation and immunity (in particular NF-κB and type 1 interferons). Both Montanide and a number of TLR agonists have been shown to induce humoral and cellular immune responses; addition of the TLR3 agonist poly-ICLC to Montanide in an NY-ESO-1 peptide vaccine was shown to induce stronger, more frequent and earlier-onset T-cell and humoral responses in advanced ovarian cancer patients (24,35). However, randomized studies comparing the adjuvant effect of Montanide alone with a combination with TLR agonists have not been performed. To our knowledge, our study is the first to compare Montanide with and without the addition of a TLR agonist as adjuvant in an NY-ESO-1 protein vaccine in a randomized trial.
We show that NY-ESO-1 protein in combination with Montanide alone or Montanide plus Resiquimod is both safe and immunogenic in patients with resected high-risk melanoma. All patients developed anti-NY-ESO-1 IgG antibody titers. The magnitude of antibody titers was notable: 6 of 12 (50%) patients vaccinated with NY-ESO-1 protein in Montanide plus Resiquimod exhibited very high (≥100,000) IgG titers, whereas 2 of 8 patients (25%) had similarly high titers in the Montanide-only cohort. No difference in the kinetics of antibody responses was seen when Resiquimod was added to Montanide, in contrast to an earlier onset of IgG antibodies observed in patients immunized with NY-ESO-1 peptides with Montanide plus poly-ICLC compared to that with only Montanide (24).
Using short-term in vitro restimulation assays, CD4+ T-cell responses were induced in the majority of patients; no differences in the rates or magnitude of the responses were seen with the addition of Resiquimod. In contrast, CD8+ T-cell responses in addition to humoral and CD4+ T-cell responses (integrated responses), were induced albeit in a relatively small subset of patients (3 of 12, 25%) who were vaccinated with NY-ESO-1 plus both Montanide and Resiquimod. Of note, all 3 patients with integrated antibody, CD4+, and CD8+ T-cell responses had substantially higher IgG antibody titers (at least three times higher than non-CD8+ T-cell responders). We have previously shown a trend for correlation of NY-ESO-1 protein-specific CD8+ T-cell responses with higher NY-ESO-1—specific antibody titers (36). In that study, efficient cross-presentation of recombinant NY-ESO-1 protein by autologous DC (as measured by IFNγ secretion of vaccine-induced CD8+ T cells) was only seen when the protein was pre-incubated either with murine NY-ESO-1-specific monoclonal Ab (ES121) or with post vaccine serum. The strikingly higher anti-NY-ESO-1 IgG antibody titers observed in the three CD8+ T-cell responders and the observation that none of the CD8+ T-cell responses were seen prior to development of vaccine-induced antibodies suggest that these antibodies promoted cross-presentation through the formation of immune complexes (37,38).
In a previous study we demonstrated that NY-ESO-1 protein, given intradermally along with topical Imiquimod and without Montanide, induced both humoral and CD4+, but not CD8+ T-cell responses in high-risk melanoma patients (11). Acknowledging the limitations of cross-trial comparisons and the additional TLR8 agonistic activity of Resiquimod, it appears that the more controlled antigen release mediated by Montanide may have resulted in the substantially higher NY-ESO-1—specific antibody titers and, either independently or as a result of cross-presentation facilitated by antibodies, in the CD8+ T-cell responses seen in a proportion of patients. Furthermore, the higher CD8+ T-cell response rate observed with NY-ESO-1 protein in combination with CpG and Montanide injected subcutaneously suggests that topical application of the TLR agonist may be inferior to application into deeper skin layers since only epidermal DC such as Langerhans Cells (LC) may be directly exposed to the inflammatory stimulus. This is demonstrated in the lack of statistically significant difference when comparing recruitment of immune cells at injection biopsies taken from patients in Arm A vs in Arm B (data not shown). DC trafficking from the skin to the draining lymph nodes is a complex process involving the need to detach from structural tissue elements, migration through the basement membrane and extracellular matrix, and traversing the afferent lymphatic endothelium (39,40). Furthermore, diverse DC populations reside in different layers of the skin. It is therefore conceivable that s.c. deposit of a TLR agonist may reach DC populations, such as the CD141+ DC subset, which plays a key role in cross-presentation of protein antigens (41), and which may be more easily mobilized and migrate more promptly to draining lymph nodes leading to more efficient encounter with T cells.
Vaccination with NY-ESO-1 full length protein genetically fused to a fully human anti–DEC-205 monoclonal antibody given with topical Resiquimod generated T-cell responses (as measured by IFNγ ELISPOTS after IVS of PBMCs) in 10 of 19 (53%) patients with advanced malignancies. Acknowledging the limitations of a cross-trial comparison, the higher rate of T-cell responses in the current study indicates that soluble NY-ESO-1 antigen given with Montanide alone or Montanide plus Resiquimod may not be inferior to antigen delivery through a DEC-205 targeted approach (38).
Epitope mapping studies with three long peptides revealed a predominance of antibody reactivity directed against the N-terminal and central portions of NY-ESO-1, consistent with results from previous reports of both spontaneous and vaccine-induced NY-ESO-1 antibody titers in cancer patients (1,11,36). Determinant mapping using a library of overlapping 20- to 22–mers showed CD4+ and CD8+ T-cell responses directed against epitopes essentially spanning the entire central and C-terminal regions of the NY-ESO-1 protein. This broad and dense pattern of immunogenicity is expected from previous reports assessing both spontaneous and vaccine-induced T-cell responses to NY-ESO-1 (1,11,24,36,42).
Cancer vaccines can lead to expansion of Tregs, potentially impeding the effector function of vaccine-induced Th1 responses (26,27). Likewise, the presence of significant numbers of antigen-specific Tregs may prevent the detection of desirable antigen-specific T-cell responses. Depletion of CD25+ cells from whole T-cell populations can promote the induction of NY-ESO-1—specific T cells in vitro (43,44). Removal of CD25+ cells from PBMCs prior to CD4+ and CD8+ selection in our study resulted in detection of NY-ESO-1—specific T-cell responses in several patients; however this effect was not consistent in all patients. Several observations therefore argue against a general effect of NY-ESO-1—specific Treg expansion by the vaccine: the heterogeneity of “unmasking” T-cell responses with CD25+ cell depletion across patients; the lack of statistically significant differences in CD25 expression between patients in whom NY-ESO-1—specific responses were unmasked by CD25+ depletion and those in whom they were not; the absence of an increase in CD25 expression after vaccination, and the fact that both NY-ESO-1—specific CD4+ and CD8+ T-cell responses were observed without CD25 depletion.
Using SNP analysis, we examined possible associations of TLR7 and TLR8 polymorphisms with immune response to the NY-ESO-1 vaccine. In the current study, 4 of 20 (20%) patients in Part II of the study were carriers of the non-synonymous TLR7 SNP rs179008, which is consistent with the prevalence of this SNP in a large (n>500) control group of predominantly male, Caucasian individuals in an HIV study (33). Notably, this SNP was detected in all 3 patients who developed CD8+ T-cell responses after vaccination with NY-ESO-1 and Montanide plus Resiquimod. The other patient who also had this particular SNP did not develop CD8+ T-cell responses after vaccination with NY-ESO-1 and Montanide plus placebo. The observed statistically significant correlation between the TLR7 SNP rs179008 and CD8+ T-cell response induced by a vaccine containing the respective TLR agonist raises the possibility that SNP analysis may be useful to select appropriate vaccine adjuvants based on TLR polymorphisms in cancer patients. The SNP rs179008 results in alteration of a Gln to a Leu residue in the signal peptide sequence of TLR7. In silico analysis using SignalP previously predicted that the amino acid change to Leu at position 11 extends the hydrophobic region of the signal sequence, possibly affecting the processing of TLR7 (45). It is conceivable that altered TLR7 processing could lead to enhanced sensitivity of TLR7, potentially affecting the production of mediators for inflammation and immunity.
In conclusion, vaccination with NY-ESO-1 protein given in combination with Montanide with or without topical Resiquimod induces NY-ESO-1-specific humoral and CD4+ T-cell responses. CD8+ T-cell responses were only induced in a subset of patients vaccinated with NY-ESO-1 combined with Montanide and Resiquimod. These immune responses were targeted at multiple epitopes of NY-ESO-1 primarily in the N-terminal portion for the antibody responses and central/C-terminal portions for the cellular responses. Recent observations of NY-ESO-1 immune responses as a predictor of objective tumor responses to CTLA-4 blockade and the finding that CTLA-4 blockade can induce or enhance polyfunctional CD4+ and CD8+ T-cell responses (2,46) provide the rationale for concurrent therapy using NY-ESO-1 vaccines in combination with immune checkpoint blockade or other agents mediating relief from immune suppression in patients with melanoma and other cancers. An ongoing study using NY-ESO-1 vaccine and CTLA-4 blockade in melanoma (NCT01810016) is testing this hypothesis.
ACKNOWLEDGEMENTS
We would like to thank Christine Sedrak for excellent technical assistance.
Grant Support: This study was sponsored and funded by the Ludwig Institute for Cancer Research with a supplemental grant from the Cancer Research Institute as part of the Cancer Vaccine Collaborative. SG was supported by a grant from the Cancer Vaccine Collaborative for Immunological Monitoring.
REFERENCES
- 1.Nagata Y, Ono S, Matsuo M, et al. Differential presentation of a soluble exogenous tumor antigen, NY-ESO-1, by distinct human dendritic cell populations. Proc Natl Acad Sci U S A. 2002;99:10629–34. doi: 10.1073/pnas.112331099. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Yuan J, Gnjatic S, Li H, et al. CTLA-4 blockade enhances polyfunctional NY-ESO-1 specific T cell responses in metastatic melanoma patients with clinical benefit. Proc Natl Acad Sci U S A. 2008;105:20410–5. doi: 10.1073/pnas.0810114105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Akira S, Takeda K. Toll-like receptor signalling. Nat Rev Immunol. 2004;4:499–511. doi: 10.1038/nri1391. [DOI] [PubMed] [Google Scholar]
- 4.Iwasaki A, Medzhitov R. Toll-like receptor control of the adaptive immune responses. Nat Immunol. 2004;5:987–95. doi: 10.1038/ni1112. [DOI] [PubMed] [Google Scholar]
- 5.Kopp E, Medzhitov R. Recogntion of microbial infection by Toll-like receptors. Current Opinion in Immunology. 2003;15:396–401. doi: 10.1016/s0952-7915(03)00080-3. [DOI] [PubMed] [Google Scholar]
- 6.Yang Y, Huang CT, Huang X, Pardoll DM. Persistent Toll-like receptor signals are required for reversal of regulatory T cell-mediated CD8 tolerance. Nat Immunol. 2004;5:508–15. doi: 10.1038/ni1059. [DOI] [PubMed] [Google Scholar]
- 7.Wang RF. Regulatory T cells and innate immune regulation in tumor immunity. Springer seminars in immunopathology. 2006;28:17–23. doi: 10.1007/s00281-006-0022-7. [DOI] [PubMed] [Google Scholar]
- 8.Gnjatic S, Sawhney NB, Bhardwaj N. Toll-like receptor agonists: are they good adjuvants? Cancer J. 2010;16:382–91. doi: 10.1097/PPO.0b013e3181eaca65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Adams S. Toll-like receptor agonists in cancer therapy. Immunotherapy. 2009;1:949–64. doi: 10.2217/imt.09.70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Vacchelli E, Eggermont A, Sautes-Fridman C, et al. Trial Watch: Toll-like receptor agonists for cancer therapy. Oncoimmunology. 2013;2:e25238. doi: 10.4161/onci.25238. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Adams S, O'Neill DW, Nonaka D, et al. Immunization of malignant melanoma patients with full-length NY-ESO-1 protein using TLR7 agonist imiquimod as vaccine adjuvant. J Immunol. 2008;181:776–84. doi: 10.4049/jimmunol.181.1.776. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Vasilakos JP, Tomai MA. The use of Toll-like receptor 7/8 agonists as vaccine adjuvants. Expert Rev Vaccines. 2013;12:809–19. doi: 10.1586/14760584.2013.811208. [DOI] [PubMed] [Google Scholar]
- 13.Ahonen CL, Gibson SJ, Smith RM, et al. Dendritic cell maturation and subsequent enhanced T-cell stimulation induced with the novel synthetic immune response modifier R-848. Cellular immunology. 1999;197:62–72. doi: 10.1006/cimm.1999.1555. [DOI] [PubMed] [Google Scholar]
- 14.Wagner TL, Ahonen CL, Couture AM, et al. Modulation of TH1 and TH2 cytokine production with the immune response modifiers, R-848 and imiquimod. Cellular immunology. 1999;191:10–9. doi: 10.1006/cimm.1998.1406. [DOI] [PubMed] [Google Scholar]
- 15.Tel J, Sittig SP, Blom RA, et al. Targeting uptake receptors on human plasmacytoid dendritic cells triggers antigen cross-presentation and robust type I IFN secretion. J Immunol. 2013;191:5005–12. doi: 10.4049/jimmunol.1300787. [DOI] [PubMed] [Google Scholar]
- 16.Kwissa M, Nakaya HI, Oluoch H, Pulendran B. Distinct TLR adjuvants differentially stimulate systemic and local innate immune responses in nonhuman primates. Blood. 2012;119:2044–55. doi: 10.1182/blood-2011-10-388579. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Thomsen LL, Topley P, Daly MG, Brett SJ, Tite JP. Imiquimod and resiquimod in a mouse model: adjuvants for DNA vaccination by particle-mediated immunotherapeutic delivery. Vaccine. 2004;22:1799–809. doi: 10.1016/j.vaccine.2003.09.052. [DOI] [PubMed] [Google Scholar]
- 18.Chang BA, Cross JL, Najar HM, Dutz JP. Topical resiquimod promotes priming of CTL to parenteral antigens. Vaccine. 2009;27:5791–9. doi: 10.1016/j.vaccine.2009.07.062. [DOI] [PubMed] [Google Scholar]
- 19.Dovedi SJ, Melis MH, Wilkinson RW, et al. Systemic delivery of a TLR7 agonist in combination with radiation primes durable antitumor immune responses in mouse models of lymphoma. Blood. 2013;121:251–9. doi: 10.1182/blood-2012-05-432393. [DOI] [PubMed] [Google Scholar]
- 20.Meyer T, Surber C, French LE, Stockfleth E. Resiquimod, a topical drug for viral skin lesions and skin cancer. Expert Opin Investig Drugs. 2013;22:149–59. doi: 10.1517/13543784.2013.749236. [DOI] [PubMed] [Google Scholar]
- 21.Vaughan HA, Svobodova S, Macgregor D, et al. Immunohistochemical and molecular analysis of human melanomas for expression of the human cancer-testis antigens NY-ESO-1 and LAGE-1. Clin Cancer Res. 2004;10:8396–404. doi: 10.1158/1078-0432.CCR-04-0809. [DOI] [PubMed] [Google Scholar]
- 22.Gnjatic S, Ritter E, Buchler MW, et al. Seromic profiling of ovarian and pancreatic cancer. Proc Natl Acad Sci U S A. 2010;107:5088–93. doi: 10.1073/pnas.0914213107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Velazquez EF, Jungbluth AA, Yancovitz M, et al. Expression of the cancer/testis antigen NY-ESO-1 in primary and metastatic malignant melanoma (MM)--correlation with prognostic factors. Cancer Immun. 2007;7:11. [PMC free article] [PubMed] [Google Scholar]
- 24.Sabbatini P, Tsuji T, Ferran L, et al. Phase I Trial of Overlapping Long Peptides from a Tumor Self-Antigen and Poly-ICLC Shows Rapid Induction of Integrated Immune Response in Ovarian Cancer Patients. Clinical cancer research : an official journal of the American Association for Cancer Research. 2012;18:6497–508. doi: 10.1158/1078-0432.CCR-12-2189. [DOI] [PubMed] [Google Scholar]
- 25.Dutoit V, Taub RN, Papadopoulos KP, et al. Multiepitope CD8(+) T cell response to a NY-ESO-1 peptide vaccine results in imprecise tumor targeting. J Clin Invest. 2002;110:1813–22. doi: 10.1172/JCI200216428. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Ebert LM, MacRaild SE, Zanker D, Davis ID, Cebon J, Chen W. A cancer vaccine induces expansion of NY-ESO-1-specific regulatory T cells in patients with advanced melanoma. PLoS One. 2012;7:e48424. doi: 10.1371/journal.pone.0048424. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Francois V, Ottaviani S, Renkvist N, et al. The CD4(+) T-cell response of melanoma patients to a MAGE-A3 peptide vaccine involves potential regulatory T cells. Cancer Res. 2009;69:4335–45. doi: 10.1158/0008-5472.CAN-08-3726. [DOI] [PubMed] [Google Scholar]
- 28.Kutikhin AG. Association of polymorphisms in TLR genes and in genes of the Toll-like receptor signaling pathway with cancer risk. Hum Immunol. 2011;72:1095–116. doi: 10.1016/j.humimm.2011.07.307. [DOI] [PubMed] [Google Scholar]
- 29.Trejo-de la OA, Hernandez-Sancen P, Maldonado-Bernal C. Relevance of single-nucleotide polymorphisms in human TLR genes to infectious and inflammatory diseases and cancer. Genes and immunity. 2014;15:199–209. doi: 10.1038/gene.2014.10. [DOI] [PubMed] [Google Scholar]
- 30.Cervantes JL, Weinerman B, Basole C, Salazar JC. TLR8: the forgotten relative revindicated. Cellular & molecular immunology. 2012;9:434–8. doi: 10.1038/cmi.2012.38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Davila S, Hibberd ML, Hari Dass R, et al. Genetic association and expression studies indicate a role of toll-like receptor 8 in pulmonary tuberculosis. PLoS genetics. 2008;4:e1000218. doi: 10.1371/journal.pgen.1000218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Wang CM, Chang SW, Wu YJ, et al. Genetic variations in Toll-like receptors (TLRs 3/7/8) are associated with systemic lupus erythematosus in a Taiwanese population. Scientific reports. 2014;4:3792. doi: 10.1038/srep03792. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Oh DY, Baumann K, Hamouda O, et al. A frequent functional toll-like receptor 7 polymorphism is associated with accelerated HIV-1 disease progression. Aids. 2009;23:297–307. doi: 10.1097/QAD.0b013e32831fb540. [DOI] [PubMed] [Google Scholar]
- 34.Monroy CM, Cortes AC, Lopez MS, et al. Hodgkin disease risk: role of genetic polymorphisms and gene-gene interactions in inflammation pathway genes. Molecular carcinogenesis. 2011;50:36–46. doi: 10.1002/mc.20688. [DOI] [PubMed] [Google Scholar]
- 35.Tsuji T, Sabbatini P, Jungbluth AA, et al. Effect of Montanide and poly-ICLC adjuvant on human self/tumor antigen-specific CD4+ T cells in phase I overlapping long peptide vaccine trial. Cancer Immunol Res. 2013;1:340–50. doi: 10.1158/2326-6066.CIR-13-0089. [DOI] [PubMed] [Google Scholar]
- 36.Valmori D, Souleimanian NE, Tosello V, et al. Vaccination with NY-ESO-1 protein and CpG in Montanide induces integrated antibody/Th1 responses and CD8 T cells through cross-priming. Proc Natl Acad Sci U S A. 2007;104:8947–52. doi: 10.1073/pnas.0703395104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Regnault A, Lankar D, Lacabanne V, et al. Fcgamma receptor-mediated induction of dendritic cell maturation and major histocompatibility complex class I-restricted antigen presentation after immune complex internalization. The Journal of experimental medicine. 1999;189:371–80. doi: 10.1084/jem.189.2.371. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Dhodapkar MV, Sznol M, Zhao B, et al. Induction of antigen-specific immunity with a vaccine targeting NY-ESO-1 to the dendritic cell receptor DEC-205. Science translational medicine. 2014;6:232ra51. doi: 10.1126/scitranslmed.3008068. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Randolph GJ, Angeli V, Swartz MA. Dendritic-cell trafficking to lymph nodes through lymphatic vessels. Nature reviews Immunology. 2005;5:617–28. doi: 10.1038/nri1670. [DOI] [PubMed] [Google Scholar]
- 40.Alvarez D, Vollmann EH, von Andrian UH. Mechanisms and consequences of dendritic cell migration. Immunity. 2008;29:325–42. doi: 10.1016/j.immuni.2008.08.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Haniffa M, Shin A, Bigley V, et al. Human tissues contain CD141hi cross-presenting dendritic cells with functional homology to mouse CD103+ nonlymphoid dendritic cells. Immunity. 2012;37:60–73. doi: 10.1016/j.immuni.2012.04.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Davis ID, Chen W, Jackson H, et al. Recombinant NY-ESO-1 protein with ISCOMATRIX adjuvant induces broad integrated antibody and CD4(+) and CD8(+) T cell responses in humans. Proc Natl Acad Sci U S A. 2004;101:10697–702. doi: 10.1073/pnas.0403572101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Nishikawa H, Jager E, Ritter G, Old LJ, Gnjatic S. CD4+ CD25+ regulatory T cells control the induction of antigen-specific CD4+ helper T cell responses in cancer patients. Blood. 2005;106:1008–11. doi: 10.1182/blood-2005-02-0607. [DOI] [PubMed] [Google Scholar]
- 44.Nishikawa H, Qian F, Tsuji T, et al. Influence of CD4+CD25+ regulatory T cells on low/high-avidity CD4+ T cells following peptide vaccination. J Immunol. 2006;176:6340–6. doi: 10.4049/jimmunol.176.10.6340. [DOI] [PubMed] [Google Scholar]
- 45.Moller-Larsen S, Nyegaard M, Haagerup A, Vestbo J, Kruse TA, Borglum AD. Association analysis identifies TLR7 and TLR8 as novel risk genes in asthma and related disorders. Thorax. 2008;63:1064–9. doi: 10.1136/thx.2007.094128. [DOI] [PubMed] [Google Scholar]
- 46.Yuan J, Adamow M, Ginsberg BA, et al. Integrated NY-ESO-1 antibody and CD8+ T-cell responses correlate with clinical benefit in advanced melanoma patients treated with ipilimumab. Proc Natl Acad Sci U S A. 2011;108:16723–8. doi: 10.1073/pnas.1110814108. [DOI] [PMC free article] [PubMed] [Google Scholar]