Abstract
In the United States, race and ethnicity are considered key social determinants of health because of their enduring association with social and economic opportunities and resources. An important policy and research concern is whether the U.S. is making progress toward reducing racial/ethnic inequalities in health. While race/ethnic disparities in infant and adult outcomes are well documented, less is known about patterns and trends by race/ethnicity among children. Our objective was to determine the patterns of and progress toward reducing racial/ethnic disparities in child health. Using nationally representative data from 1998 to 2009, we assessed 17 indicators of child health, including overall health status, disability, measures of specific illnesses, and indicators of the social and economic consequences of illnesses. We examined disparities across five race/ethnic groups (non-Hispanic white, non-Hispanic black, Hispanic, non-Hispanic Asian, and non-Hispanic other). We found important racial/ethnic disparities across nearly all of the indicators of health we examined, adjusting for socioeconomic status, nativity, and access to health care. Importantly, we found little evidence that racial/ethnic disparities in child health have changed over time. In fact, for certain illnesses such as asthma, black–white disparities grew significantly larger over time. In general, black children had the highest reported prevalence across the health indicators and Asian children had the lowest reported prevalence. Hispanic children tended to be more similar to whites compared to the other race/ethnic groups, but there was considerable variability in their relative standing.
Keywords: Race, Ethnicity, Inequality, Disparities, Child health, Asthma, Autism, Trends, United States
Introduction
Nowhere is the changing race and ethnic profile of the U.S. more evident than among children. While approximately 80% of U.S. adults over age 65 are non-Hispanic white, only 55% of individuals under age 18 fall into this category (U.S. Census Bureau 2010: Author calculations). These young cohorts of today indicate what the racial/ethnic demographic makeup of the U.S. adult population will be in the future. Some projections suggest that the U.S. will become a “majority minority” population by 2050 (i.e., non-Hispanic whites will comprise less than half of the U.S. population) (Ortman & Guarneri, 2009). These demographic trends have brought renewed policy and research attention to racial/ethnic minorities and their social and economic wellbeing, including understanding racial/ethnic differences in population health (Dentzer, 2011).
In the U.S., race is considered a key social determinant of health because of its long-standing association with poverty, discrimination, residential segregation, and unequal access to health care (Link & Phelan,1995; Williams & Jackson, 2005). Numerous studies indicate that race/ethnicity is also an important social category that has strong associations with many health outcomes, even after adjusting for traditional measures of socioeconomic status (SES) such as education and income. These findings are believed to highlight differences in a complex set of social, economic, and biological assets available to different race/ethnic groups (Link & Phelan, 1995; Williams & Jackson, 2005; Williams, Mohammed, Leavell, & Collins, 2010) that are often unable to be fully accounted for or inadequately measured in empirical work (Krieger, Williams, & Moss, 1997; Krieger, Chen, Waterman, Rehkopf, & Subramanian, 2005; LaVeist, 2005). Indeed, from a social determinants of health perspective, race/ethnicity can be considered a “fundamental cause” of disease in the U.S. due to both historical (e.g., slavery and Jim Crow) and current (e.g., redlining and employment discrimination) forms of institutionalized discrimination. Race/ethnicity determines access to crucial resources, such as knowledge, money, prestige, power, as well as interpersonal resources, which assist people in avoiding diseases and their negative consequences.
Although accurate population-wide health data on racial/ethnic groups have only been available since the mid-20th century, racial/ethnic differences in health have become one of the most widely studied topics in U.S. health disparities research (Jones, LaVeist, & Lillie-Blanton, 1991; Williams, 1994). on differences between non-Hispanic blacks and whites, but there has been increasing attention given to Hispanics and Asian-origin populations, groups that have both grown rapidly as a result of changes in U.S. immigration policy in the mid-1960s.
An important policy concern is whether the U.S. is making progress toward reducing racial/ethnic inequalities in health (Agency for Healthcare Research and Quality, 2011; U.S. Department of Health and Human Services, 2010). However, with the exception of infant outcomes, the majority of the research examining U.S. racial/ethnic health differentials has focused on adults. Changes over time in race/ethnic differences among adults have been well characterized. For example, the black–white gap in life expectancy at age 50 has been relatively stable for males and declined steadily for females since the mid-1990s, although large disparities persist for both sexes. A number of recent studies have also examined trends in adult inequalities with respect to disability, major adult chronic diseases, and their risk factors (e.g., Burt et al., 1995; Crimmins & Saito, 2001; Egan, Zhao, & Axon, 2010; Lee, Brancati, & Yeh, 2011; Moss & Mannino, 2002; Williams & Collins, 1995).
Similarly, changes over time in infant mortality have also been well characterized, at least between blacks and whites. Throughout most of the twentieth century, the black–white ratio of the infant mortality rate (IMR) has increased (although the absolute black–white difference has declined over much of this period) (Singh & van Dyck, 2010). In 2000, the IMR among black infants was more than 2.5 times that of white infants, a relative disparity which decreased only slightly between 2000 and 2007 (Singh & van Dyck, 2010). In contrast, we know comparatively less about changes over time in race/ethnic inequalities in child health. With respect to race/ethnic differences, perhaps the best studied child health indicator is asthma (e.g., Akinbami, Moorman, Garbe, & Sondik, 2009; Akinbami & Schoendorf, 2002). One nationally representative study indicated that black–white differences in asthma prevalence increased between 1997 and 2003 (in that blacks were increasingly more likely to have asthma compared to whites) (McDaniel, Paxson, & Waldfogel, 2006). More recent changes in the black–white disparity have not been assessed to our knowledge. In addition, recent nationally representative evidence suggests that increases in the prevalence of autism have been more pronounced in whites compared to blacks and Hispanics between 1997 and 2008 (Boyle et al., 2011). A recent technical report by the American Academy of Pediatrics (AAP), which reviewed the existing evidence on race/ethnic disparities, concluded that “[r]acial/ethnic disparities in child health and health care are extensive, pervasive, and persistent, and occur across the spectrum of health and health care” (Flores & Committee On Pediatric Research, 2010; Flores & Tomany-Korman, 2008). The AAP report also indicated that few studies have examined trends in child health disparities.
Our objective is to examine whether racial/ethnic differences in child health have been widening or narrowing over time. We focus on the recent 1998–2009 period and compare trends occurring across multiple indicators of child health. This comparative perspective enables researchers to understand how the overall health of children is changing over time and whether there are variations in race/ethnic disparities across different dimensions of child health. In addition, this approach allows for the differentiation between improvements in child population health overall versus improvements in reducing racial/ethnic disparities in child health, both important but distinct national health policy goals (Koh, Graham, & Glied, 2011; National Research Council, 2004; U.S. Department of Health and Human Services, 2010). We utilize large-scale nationally representative data and include Asian-origin children, a group that has been traditionally excluded from the race/ethnic disparities literature.
Data and methods
We used the 1998–2009 waves of the National Health Interview Survey (NHIS), which is an annual and ongoing cross-sectional survey of the U.S. non-institutionalized population. We did not include earlier data because information on many child health indicators was not available or not comparable with data from more recent survey waves. Since 1998, the NHIS has consisted of a core component that collects a limited set of data from all members in a family including children and a “Sample Child” interview, which collects more detailed information from a randomly selected child (ages 0–17) in each family. Information in the Sample Child interview is obtained from a knowledgeable adult (usually the parent) in the household (National Center for Health Statistics, 2012). Most of the health indicators we used are contained in the Sample Child interview, although some indicators are contained in the core interview and therefore are available for a larger number of children. In order to obtain the most stable estimates, we used all available data for each of the health indicators. The study did not require ethics review, since this is a secondary analysis of deidentified publicly available data.
The 1998–2009 NHIS waves contain a total of 286,232 children ages 0–16, of which 133,647 were part of the Sample Child file. We limited the analysis to children under the age of 17 because of the possibility that some 17 year olds are selected out of the household due to college attendance. We omitted respondents with missing data on at least one covariate, which resulted in a small attrition from the sample (1–2%). The health indicators were also reported for the vast majority of the samples with missing information well under 1% of respondents for each of the indicators. The exception was missing school days, which was unusable for approximately 2.5% of the school-aged sample (ages 5+). This proportion of missing data was partly because 0.9% of the school-age sample (ages 5–16) was reported as not attending school. All analyses were based on public-use NHIS data files provided by the University of Minnesota's Integrated Health Interview Series (IHIS). The IHIS contains a harmonized set of NHIS variables for multiple NHIS years and is therefore ideally situated to investigate trends (Minnesota Population Center and State Health Access Data Assistance Center, 2012).
Child health indicators
We examined 17 indicators of child health. For purposes of presentation, we categorized the 17 indicators into four broad groupings: (1) Overall health status; (2) Disability; (3) Consequences of illness; and (4) Specific conditions. All indicators were measured dichotomously. Overall health status elicited responses based on the standard 5-point Likert scale (Excellent, Very Good, Good, Poor, Fair). We created a 0/1 dummy variable indicating Poor/Fair health (alternative models treating this variable linearly resulted in similar substantive conclusions). We examined two measures of disability: limitations in play and activities of daily living (ADL) limitations. Limitations in play is restricted to children ages 0–4. Consequences of illness indicators highlight the potential social and economic costs of poor child health. We examined number of missed school days in the prior year due to illness or injury, analyzed dichotomously as ≥18 days vs. <18 days, which is a threshold based on missing 10% of school days based on a 180 day school year. Such a threshold has been used previously (Chang & Romero, 2008). We also assessed whether the child stayed in the hospital overnight in the prior year. Respondents were asked to exclude overnight stays in the emergency room. These first three categories represent indicators that can arise from a variety of child health illnesses. We also assessed eleven specific child health illnesses. Table 1 presents a description of all health indicators and the corresponding age ranges examined.
Table 1.
Child health indicators in the National Health Interview Survey (1998–2009).
| Characteristic | Ages (years) | Description |
|---|---|---|
| Overall health | ||
| Overall health status | 0–16 | Fair/Poor (vs. Excellent/Very Good/Good) |
| Disability | ||
| Limited in kind or amount of play | 0–4 | Limited in the amount of play activities child could do because of a physical, mental, or emotional problem (Yes/No) |
| Activities of Daily Living (ADL) limitation | 3–16 | Help with eating/bathing, dressing, or getting around inside the home because of physical, mental, or emotional problem (Yes/No) |
| Consequences of illness | ||
| Missed School Days | 5–16 | School days lost due to illness or injury, prior 12 months (≥18 days vs. <18 days) |
| Overnight at hospital | 1–16 | Overnight stay in hospital (excluding ER visits), prior 12 months (Yes/No) |
| Specific conditions | ||
| Allergies Respiratory | 0–16 | Respiratory allergy or hay fever, prior 12 months (Yes/No) |
| Skin | 0–16 | Skin allergy, prior 12 months (Yes/No) |
| Frequent headaches | 3–16 | Frequent headaches/migraines, prior 12 months (Yes/No) |
| Asthma Ever diagnosed | 0–16 | Ever diagnosed as having asthma (Yes/No) |
| ER visit due to asthmaa | 0–16 | Emergency room visit for asthma, prior 12 months (Yes/No) |
| Frequent Diarrhea | 0–16 | Frequent or repeated diarrhea, prior 12 months (Yes/No) |
| Ear Infection | 0–16 | 3 + ear infections, prior 12 months (Yes/No) |
| ADHDb | 2e16 | Ever diagnosed as having ADHD/ADD (Yes/No) |
| Vision Problems | 0–16 | Trouble seeing even when wearing glasses or contact lenses (Yes/No) |
| Stutter and Stammer | 3–16 | Stutter/stammer, prior 12 months |
| Anemia | 0–16 | Had anemia, prior 12 months (Yes/No) |
| Autism | 2–16 | Ever diagnosed with autism (Yes/No) |
Among those who reported being diagnosed with asthma and reported as having had an asthma attack/episode in the prior 12 months.
ADHD, Attention Deficit Hyperactivity Disorder; ADD, Attention Deficit Disorder.
Race/ethnic groups
We examined differences across five mutually exclusive race/ethnic groups: (1) Non-Hispanic white, (2) Non-Hispanic black, (3) Hispanic (of any race), (4) Non-Hispanic Asian (including Asian Indian and other South Asian), and (5) Non-Hispanic other. Hispanic ethnicity was ascertained from a question asking whether the child had any Hispanic or Latino ancestry. Due to sample size constraints, we did not examine differences across Hispanic subgroups. The non-Hispanic other category includes Aleut, Alaskan Native, American Indians, and those who reported “other” or multiple races. Pacific Islanders (e.g., Hawaiian, Samoans) were categorized under the Non-Hispanic Asian group. While we present results for the Other category, we do not focus our discussion on findings for this group. For purposes of description and discussion, we use the term “minority” to refer to the latter four groups and omit the term “non-Hispanic.”
Statistical analysis
We estimated the unadjusted prevalence of each health indicator using the pooled 1998–2009 data. The prevalence of each indicator was calculated for all race/ethnic groups combined and for each race/ethnic group independently. We tested for statistically significant differences in the prevalence of each indicator across the pairwise combinations of the race/ethnic groups using a set of χ2 tests (e.g., black vs. white, Hispanic vs. black, etc.).
We used a model-based approach to estimate overall trends and race/ethnic differences in trends. Given that many child health indicators are rare, estimates based on a single year of data may produce large uncertainties and thus we pooled all years of data and estimated a series of logit models with a continuous measure of survey year as a predictor variable. We use logit models because all outcomes are binary and these models have more favorable properties compared to linear probability models (Allison, 1999). Estimates from the logit models can be most straightforwardly interpreted as relative differences in the odds. First, we examined the trend for all race/ethnic groups combined adjusting for age. Positive coefficients (odds ratios [OR] > 1.0) for the year variable indicate increasing odds over time and negative coefficients (OR < 1.0) indicate declining odds. The annual percentage change in the odds was calculated by subtracting one from the odds ratio and multiplying by 100. Second, we examined changes over time in race/ethnic disparities focusing on differences between each minority group and whites. We included interaction terms between each race/ethnic category and the survey year variable (whites were the reference category). The magnitude of the odds ratios for the interaction terms indicates the proportionate difference in the trend for each minority group compared to the trend for white (and thus whether the relative disparity is changing over time). The p-values for these interaction terms indicate whether the trend for the minority group was statistically different (p < .05) from that of whites.
For each outcome, we initially tested whether the trend for whites, the reference category, exhibited any nonlinearities in the log-odds scale by estimating models excluding the other race/ethnic groups and including a term for year and year-squared. In all cases, the year-squared term did not significantly (p > .05) contribute to the explanatory power of the model (based on F-tests for nested models). We therefore held the trend for whites to be linear in the log-odds. As indicated, changes over time in race/ethnic disparities were estimated on a pooled sample with interactions between each race/ethnic minority category and year. For each of these race/ethnic groups, we tested whether a race × year-squared term contributed significantly (p > .05) to the model after including the linear interaction. If so, these terms were retained, otherwise they were dropped from the final model. Using the estimates from the logit models, we present a series of figures showing predicted probabilities (expressed as percentages) by race/ethnicity at the beginning (1998) and at the end (2009) of the observation period. These figures highlight absolute differences in risk across groups and absolute changes in disparities over time. Predicted probabilities were estimated by holding the other covariates at their overall mean. We excluded the Other race/ethnic category from the figures.
Fully adjusted models wereadjusted for age (in single years), sex, highest educational attainment in the family (<HS/GED, HS/GED, some college, college degree+), place of birth (U.S. vs. outside of the U.S.), and access to health care (whether the child had health insurance). Educational attainment is strongly associated with health behaviors and is less subject to reverse causation than income (Cutler & Lleras-Muney, 2008). Interactions between race/ethnicity and age were explored in preliminary analyses, but in most cases these interactions were either not statistically significant or did not change the substantive results so they were excluded from the final models for parsimony.
All analyses were weighted and conducted using STATA 12.0 with the svy: prefix. We adjusted the NHIS-supplied sampling weights according to recommended guidelines for pooling multiple years of data and we utilized psu and strata codes provided by the IHIS, which are appropriate for pooled analyses (Minnesota Population Centerand State Health Access Data Assistance Center, 2012). We additionally tested the sensitivity of results to corrections for potential biases arising from the use of logistic regression models to predict rare outcomes (King & Zeng, 2001) and found that our presented results were highly similar to the corrected results.
Results
Descriptive characteristics
Table 2 provides descriptive characteristics of all children in the core interview. Reflective of the demographic changes of U.S. children, nearly 40% of all children belonged to one of the minority race/ethnic groups. Hispanics represented the largest minority group (19%) followed by blacks (15%), Asians (4%), and Others (2%). The mean age of the sample was 8.20 years with some variation across race/ethnicity (Hispanic children were slightly younger at 7.55 years on average). WhiteandAsian children were considerably more likely to come from families in which at least one adult had a college degree (42% and 60%, respectively). In contrast, approximately one-third of Hispanic children came from families in which no adult had completed high school. Few white and black children were foreign born (2% each). Approximately 12% and 21% of Hispanic and Asian children, respectively, were foreign born. The distribution of these characteristics among children interviewed as part of the Sample Child interview was highly similar (results not shown).
Table 2.
Descriptive characteristics.
| Characteristic | NH whites (N=132,710) | NH blacks (N=45,704) | Hispanics (N=85,766) | NH Asians (N=10,073) | NH Other (N=4177) |
|---|---|---|---|---|---|
| Sample Proportion | 0.61 | 0.15 | 0.19 | 0.04 | 0.02 |
| Mean age, years | 8.20 (8.16,8.24) | 8.13 (8.07,8.19) | 7.55 (7.51,7.60) | 7.96 (7.81,8.10) | 7.70 (7.50,7.89) |
| Female | 0.04(0.04,0.05) | 0.14(0.13,0.14) | 0.33(0.32,0.34) | 0.07(0.06,0.08) | 0.08(0.06,0.09) |
| Highest educational level in family | |||||
| <HS | 0.04 (0.04,0.05) | 0.14 (0.13,0.14) | 0.33 (0.32,0.34) | 0.07 (0.06,0.08) | 0.08 (0.06,0.09) |
| HS/GED | 0.21 (0.20,0.21) | 0.30 (0.29,0.31) | 0.26 (0.26,0.27) | 0.13 (0.12,0.14) | 0.29 (0.26,0.32) |
| Some College | 0.33 (0.33,0.34) | 0.38 (0.37,0.38) | 0.27 (0.27,0.28) | 0.20 (0.18,0.21) | 0.39 (0.37,0.42) |
| College Degree+ | 0.42 (0.41,0.42) | 0.18 (0.18,0.19) | 0.13 (0.13,0.14) | 0.60 (0.58,0.62) | 0.24 (0.21,0.27) |
| Foreign born | 0.02 (0.02,0.02) | 0.02 (0.02,0.02) | 0.12 (0.11,0.12) | 0.21 (0.20,0.23) | 0.03 (0.02,0.04) |
| Health Insurance | 0.93 (0.93,0.93) | 0.91 (0.91,0.92) | 0.80 (0.80,0.81) | 0.91 (0.90,0.91) | 0.83 (0.79,0.86) |
Note: NH = Non-Hispanic. N = 278,430 children ages 0–16 in the NHIS core file. 95% CI shown in parenthesis.
Source: National Health Interview Survey, 1998–2009.
Overall prevalence and trends
Table 3 shows the unadjusted prevalence of the health indicators overall and by race/ethnicity. The prevalence of the overall health indicators (fair/poor health) was low. Approximately 1.75% of all children were reported to be in fair or poor health. Similarly, approximately 1.94% of children (ages 0–4) were reported to be limited in the kind or amount of play. The prevalence of an ADL limitation, a relatively severe measure of disability, was 0.56%. About 2.41% of children were reported to have missed 18 or more days of school and a similar percentage were reporting as spending a night in the hospital. The lower portion of Table 3 lists the specific conditions. Among the specific conditions, the most prevalent were respiratory allergies (17.67%) and asthma (12.52%). Approximately 2% or less of children was reported to have vision problems, stutter/stammer, anemia, and autism.
Table 3.
Prevalence (%) and percent annual change in child health indicators; 1998–2009.
| Characteristic | All | NH whites | NH blacks | Hispanics | NH Asians | NH Other | % Annual Change1 (95% CI) | |
|---|---|---|---|---|---|---|---|---|
| Overall health | ||||||||
| Fair/poor overall health status | 1.75 | 1.13b,c,d,e | 3.37a,c,d | 2.67a,b,d | 0.75a,b,c,e | 2.67a,d | −0.06 | (−1.43, 1.34) |
| Disability | ||||||||
| Limited in kind/amount of play | 1.94 | 2.11b,c,d | 3.04a,c,d | 1.63a,b,d,e | 0.78a,b,c,e | 3.71c,d | 2.35 | (−0.55, 5.33) |
| ADL3 limitation | 0.56 | 0.55 | 0.74 | 0.60 | 0.52 | 1.16 | 3.22* | (0.22, 6.31) |
| Consequences of illness | ||||||||
| Missed school days (≥18 days) | 2.41 | 2.37b,c,d,e | 2.02a,d,e | 2.06a,d,e | 0.81a,b,c,e | 4.15a,b,c,d | −2.98*** | (−4.49, −1.44) |
| Over night at hospital | 2.48 | 2.51d | 2.73d | 2.62d | 1.68a,b,c,e | 2.92d | −1.38* | (−2.68, −0.06) |
| Specific conditions | ||||||||
| Allergies | ||||||||
| Respiratory | 17.67 | 19.07b,c,d | 15.45a,c,d,e | 12.27a,b,e | 12.47a,b,e | 18.62b,c,d | −0.65* | (−1.22, −0.09) |
| Skin | 9.46 | 9.26b,c,e | 12.13a,c,d | 7.25a,b,d,e | 8.78b,c,e | 13.37a,c,d | 5.06*** | (4.27, 5.86) |
| Frequent Headaches | 5.89 | 5.82b,c,d | 6.56a,c,d | 4.94a,b,d | 2.40a,b,c,e | 6.34d | −1.47** | (−2.44, −0.48) |
| Asthma | ||||||||
| Ever diagnosed | 12.52 | 11.66b,d,e | 17.54a,c,d | 11.33b,d,e | 9.65a,b,c,e | 17.02a,c,d | 1.81*** | (1.17, 2.47) |
| ER visit due to asthma2 | 33.28 | 24.98b,c,e | 51.74a,c,d | 41.30a,b,d | 27.49a,b,c,e | 42.69a,d | 0.37 | (−2.20, −1.49) |
| Frequent Diarrhea | 1.53 | 1.52d | 1.54d | 1.68d | 0.98a,b,c | 1.60 | 0.17 | (−1.58, 1.94) |
| Ear Infection | 6.67 | 6.87b,c,d | 4.74a,c,d,e | 6.31a,b,d | 3.20a,b,c,e | 7.57b,d | −2.91*** | (−3.80, −2.01) |
| ADHD3 | 6.68 | 7.50b,c,d | 6.55a,c,d | 3.72a,b,d,e | 1.50a,b,c,e | 6.23c,d | 3.02*** | (2.10, 3.94) |
| Vision Problems | 2.23 | 2.13b,d | 2.97a,c,d | 2.35b,d | 1.58a,b,c,e | 2.98d | 0.42 | (−0.92, 1.78) |
| Stutter and Stammer | 1.57 | 1.34b,c,d,e | 2.65a,c,d | 2.00a,b,d | 0.41a,b,c,e | 2.94a,d | 1.88* | (0.22, 3.56) |
| Anemia | 1.02 | 0.80b,c | 1.90a,c,d | 1.38a,b,d | 0.69b,c | 1.30 | 0.28 | (−1.60, 2.21) |
| Autism | 0.59 | 0.61c,d | 0.50 | 0.37a,e | 0.32a,e | 1.24c,d | 13.59*** | (10.28, 17.00) |
Note: NH is non-Hispanic. Letter super-scripts indicate significant differences for each pairwise comparison (p < .05)
from NH whites
from NH blacks
from Hispanics
from NH Asians
from NH other
Annual percentage change in the odds estimated from a logistic model adjusting for age
p < .001
p < .01
p < .05
Among those who reported being diagnosed with asthma and reported as having had an asthma attack/episode in the prior 12 months.
ADL: Activities of Daily Living; ADHD: Attention Deficit Hyperactivity Disorder.
Source: National Health Interview Survey, 1998–2009.
The final column of Table 3 shows age-adjusted trends for each health indicator expressed as the percentage annual change in the odds of having the indicator. Six of the seventeen indicators demonstrated a significantly (p < .05) increasing trend: ADL limitations, skin allergies, asthma, Attention Deficit Hyperactivity Disorder (ADHD), and stutter/stammer, and autism. The increase in autism was most striking, with an average annual increase in the odds of approximately 14%. Missed school days, hospital stays, respiratory allergies, frequent headaches, and ear infections all showed statistically significant declines in prevalence. The largest proportionate declines were observed for ear infections (−2.91%) and missed school days (−2.98%).
Race/ethnic disparities and trends
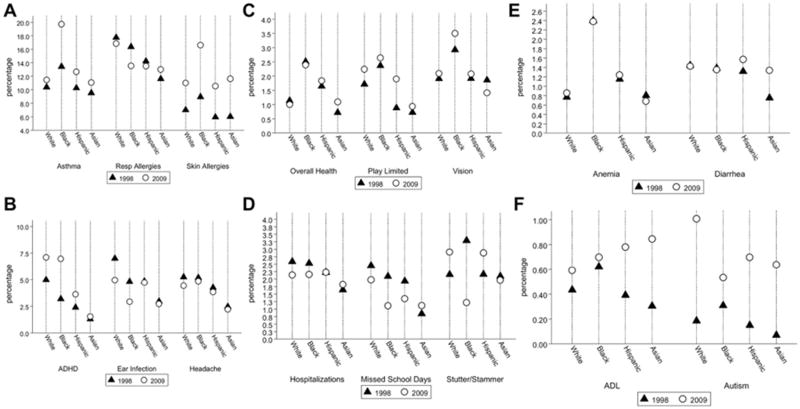
We next turn to race/ethnic disparities in child health and trends therein. Table 4 shows results from the multivariate logistic regression models examining race/ethnic differences in the trends. Fig. 1 shows the predicted probabilities from the regression models shown in Table 4. Below, we discuss specific findings for each minority group separately in reference to whites. However, some broad patterns are worth noting. First, as indicated by the pair-wise comparisons in Table 3, there is considerable variation in the prevalence of the health indicators across race/ethnicity. Second, Asian children had a significantly lower prevalence of nearly all health indicators compared to the other groups. In contrast, with some exceptions, black children had the highest prevalence of the indicators among the groups, although many comparisons did not reach statistical significance. The results for Hispanic children were more variable, although they were generally better off than white children.
Table 4.
Odds ratios (95% CI) from logistic regression models for all race/ethnic groups combined.
| Characteristic | Overall health |
Play limitation |
ADL limitation | Missed school days (≥18 days) |
Overnight hospitalization |
Respiratory allergies |
Skin allergies |
Frequent headaches |
|
|---|---|---|---|---|---|---|---|---|---|
| Trend (Whites) | |||||||||
| Year | 1.001 (0.983,1.019) | 1.017 (0.991,1.043) | 1.029 (0.998,1.061) | 0.980* (0.962,0.998) | 0.997 (0.985,1.009) | 0.995 (0.989,1.002) | 1.042*** (1.032,1.052) | 0.985* (0.972,0.999) | |
| Race/ethnic (Ref: White) | |||||||||
| Black | 2.338*** (1.992,2.743) | 1.590*** (1.208,2.093) | 1.376 (0.997,1.897) | 0.734** (0.582,0.925) | 1.186* (1.041,1.351) | 0.915* (0.841,0.995) | 1.304*** (1.157,1.470) | 0.989 (0.836,1.171) | |
| Black × year | 0.991 (0.965,1.017) | 0.975 (0.932,1.020) | 0.977 (0.926,1.032) | 0.985 (0.946,1.026) | 0.978* (0.958,0.999) | 0.989 (0.975,1.003) | 1.018 (0.999,1.037) | 1.009 (0.983,1.035) | |
| Black × year2 | – | – | – | – | – | – | – | – | |
| Hispanic | 1.523*** (1.309,1.772) | 0.76 (0.561,1.030) | 0.916 (0.671,1.249) | 0.749** (0.613,0.915) | 0.874* (0.775,0.985) | 0.785*** (0.726,0.850) | 0.840* (0.735,0.959) | 0.805** (0.684,0.947) | |
| Hispanic × year | 1.007 (0.983,1.031) | 1.012 (0.964,1.063) | 1.014 (0.966,1.064) | 0.988 (0.957,1.021) | 1.002 (0.982,1.023) | 0.998 (0.986,1.011) | 1.011 (0.992,1.030) | 1.006 (0.981,1.032) | |
| Hispanic year2 | – | – | – | – | – | – | – | – | |
| Asian | 0.779 (0.465,1.304) | 0.554 (0.222,1.383) | 1.473 (0.729,2.977) | 0.360** (0.171,0.760) | 0.697* (0.488,0.996) | 0.585*** (0.470,0.729) | 0.85 (0.653,1.107) | 0.457*** (0.307,0.679) | |
| Asian × year | 1.037 (0.965,1.113) | 0.949 (0.820,1.097) | 0.95 (0.856,1.055) | 1.048 (0.942,1.165) | 0.996 (0.945,1.050) | 1.018 (0.986,1.050) | 1.019 (0.982,1.057) | 1.005 (0.938,1.077) | |
| Asian × year2 | – | – | – | – | – | – | – | – | |
| Other | 1.712** (1.197,2.447) | 2.351* (1.179,4.690) | 2.378* (1.025,5.516) | 1.6 (0.937,2.731) | 0.982 (0.650,1.483) | 1.153 (0.886,1.502) | 1.153 (0.785,1.695) | 0.948 (0.603,1.491) | |
| Other × year | 1.032 (0.966,1.104) | 0.934 (0.841,1.037) | 0.979 (0.894,1.072) | 1.003 (0.916,1.098) | 1.003 (0.940,1.071) | 1.004 (0.965,1.044) | 1.047 (0.983,1.116) | 1.029 (0.960,1.104) | |
| Other × year2 | – | – | – | – | – | – | – | – | |
|
| |||||||||
| Characteristic | Asthma | ER visit due to asthma | Frequent Diarrhea | Ear infection | ADHD | Vision problems | Stutter/Stammer | Anemia | Autism |
|
| |||||||||
| Trend (Whites) | |||||||||
| Year | 1.009* (1.001,1.018) | 0.991 (0.963,1.020) | 0.999 (0.975,1.024) | 0.970*** (0.959,0.981) | 1.032*** (1.020,1.044) | 1.008 (0.988,1.028) | 1.013 (0.987,1.040) | 1.009 (0.977,1.042) | 1.153*** (1.113,1.194) |
| Race/ethnic (Ref: White) | |||||||||
| Black | 1.338*** (1.203,1.488) | 2.862*** (2.220,3.688) | 0.957 (0.719,1.273) | 0.671*** (0.578,0.780) | 0.629*** (0.537,0.736) | 1.547*** (1.223,1.955) | 1.757*** (1.371,2.251) | 3.166*** (2.290,4.378) | 1.671 (0.919,3.036) |
| Black × year | 1.030*** (1.012,1.047) | 0.997 (0.951,1.046) | 0.999 (0.952,1.049) | 0.988 (0.961,1.015) | 1.038** (1.013,1.063) | 0.896* (0.810,0.990) | 0.999 (0.958,1.043) | 0.838* (0.731,0.962) | 0.908* (0.832,0.991) |
| Black × year2 | – | – | – | – | – | 1.010* (1.001,1.019) | 1.014* (1.002,1.026) | – | |
| Hispanic | 0.986 (0.887,1.096) | 1.613** (1.205,2.160) | 0.91 (0.699,1.185) | 0.676*** (0.596,0.767) | 0.469*** (0.390,0.565) | 1.003 (0.815,1.235) | 0.999 (0.767,1.303) | 1.503** (1.115,2.027) | 0.809 (0.453,1.446) |
| Hispanic × year | 1.011 (0.995,1.027) | 1.01 (0.961,1.061) | 1.016 (0.976,1.058) | 1.029** (1.009,1.049) | 1.004 (0.979,1.030) | 0.999 (0.966,1.033) | 1.026 (0.986,1.067) | 0.997 (0.952,1.045) | 0.987 (0.920,1.059) |
| Hispanic × year2 | – | – | – | – | – | – | – | – | – |
| Asian | 0.909 (0.708,1.167) | 1.27 (0.636,2.539) | 0.516* (0.270,0.986) | 0.406*** (0.291,0.565) | 0.254*** (0.149,0.432) | 0.973 (0.593,1.596) | 0.330* (0.121,0.906) | 1.047 (0.490,2.235) | 0.375 (0.075,1.889) |
| Asian × year | 1.005 (0.969,1.042) | 0.974 (0.881,1.078) | 1.051 (0.961,1.150) | 1.024 (0.970,1.081) | 0.982 (0.910,1.060) | 0.969 (0.903,1.041) | 0.999 (0.872,1.144) | 0.977 (0.881,1.084) | 1.044 (0.855,1.274) |
| Asian × year2 | – | – | – | – | – | – | – | – | – |
| Other | 1.583** (1.164,2.153) | 1.874 (0.811,4.330) | 1.21 (0.593,2.469) | 1.284 (0.775,2.129) | 0.776 (0.471,1.277) | 1.584 (0.842,2.979) | 1.602 (0.743,3.457) | 1.700 (0.702,4.120) | 2.915 (0.811,10.483) |
| Other × year | 1.003 (0.955,1.054) | 1.001 (0.878,1.142) | 0.963 (0.849,1.092) | 0.963 (0.889,1.043) | 1.007 (0.936,1.082) | 0.975 (0.880,1.080) | 1.034 (0.927,1.153) | 0.981 (0.848,1.134) | 0.950 (0.783,1.153) |
| Other × year2 | – | – | – | – | – | – | – | – | – |
Note: Year indicates survey year. Models are adjusted for age, sex, highest education in family, foreign born status, and health insurance status. Race by year-squared interactions are included only if significant (p < .05).
p < .001;
p < .01;
p < .05.
Source: National Health Interview Survey, 1998–2009.
Fig. 1.
Predicted prevalence (%) estimated from logistic regression models by health indicator and race/ethnicity in 1998 and 2009.
Blacks
Compared to whites, black children had a higher reported prevalence of overall fair/poor health and both measures of disability (limited in play, ADL limitation) (Table 3). Comparisons for ADL limitations were not statistically significant. In contrast, black children were less likely to be reported as missing 18 or more days of school (2.02% vs. 2.37%; p < .05). Among the specific conditions, black children were reported to have a higher prevalence of asthma (17.54% vs. 11.66%; p < .05) and were more than twice as likely to have a reported ER visit due to asthma conditional on having an asthma attack in the prior 12 months (51.74% vs. 24.98%; p < .05). Black children also had significantly higher reports of skin allergies, vision problems, stutter and stammer, and anemia, although a significantly lower reported prevalence of respiratory allergies, ear infections, and ADHD.
For 11 of the 17 health indicators, we found no significant trend in the black–white odds ratios from the multivariate regression models (Table 4). We found that disparities in asthma increased considerably. For example, the predicted black–white odds ratio for asthma was 1.338 (95% CI: 1.203,1.488) in 1998 and it increased to 1.844 (95% CI: 1.651, 2.060) in 2009 (p < .001 for annual trend). Fig. 1A highlights how the absolute black–white disparity in asthma grew over the observation period. Interestingly, black children appeared less likely (OR = 0.629; 95% CI: 0.537, 0.736) to have been diagnosed with ADHD at the beginning of the period compared to white children. However, over time this advantage diminished and by the end of the period black children were about equally as likely to have been diagnosed with ADHD (OR = 0.945; 95% CI: 0.809, 1.103) compared to white children. Fig. 1B further highlights the diminishing absolute advantage of black children over time.
The results for autism are noteworthy. We found that reported autism significantly increased for both whites and blacks. For whites, the odds of autism increased by approximately 15% annually (Table 4). For blacks, the proportionate annual increases were significantly (p < .05) different and smaller than that of whites at approximately 5% (e.g., 1.153 × 0.908 = 1.047). In 1998, the predicted black–white odds ratio was 1.671 (95% CI: 0.919, 3.036). By 2009 it was approximately 0.579 (95% CI: 0.341, 0.983). Thus, the direction of the disparity appears to have reversed. As indicated, blacks had a significantly lower overall prevalence of missed school days compared to whites.
We performed additional analyses including a three-way interaction among sex, black, and year to examine whether the trends noted above for asthma, ADHD, and, autism differed by sex. While these models have reduced power, we found no indication that the initial relative disparity or the trend differed by sex. The p-values for the two-way (black × sex) and three-way interaction (black × year × sex) terms were highly insignificant in all cases (p > .45).
Hispanics
The results for Hispanics showed considerable variability with respect to their comparison with whites (Table 3). Hispanic children were reported to be more than twice as likely to be in fair/poor health compared to whites (2.67% vs. 1.13%; p < .05 for the comparison). However, they were less likely to have a reported play limitation (1.63% vs. 2.11%; p < .05 for the comparison) and about equally likely to be reported as having an ADL limitation. Hispanic children were also less likely to have been reported to miss 18 or more days of school compared to white children (2.06% vs. 2.37%; p < .05 for the comparison). Among the specific conditions, Hispanic children had lower reported levels of respiratory and skin allergies and frequent headaches compared to whites. They had similar levels of reported asthma diagnosis (11–12%), but had a much higher risk of an ER visit due to asthma if diagnosed with asthma (41.30% vs. 24.98%; p < .05 for the comparison). Hispanic children also had a lower prevalence of ear infections, ADHD, and autism, but a higher prevalence of stutter and stammer and anemia.
With respect to trends, we only detected significant changes in the Hispanic-white odds ratio for ear infections (Table 4). Hispanic children appeared to be better off in 1998 (OR = 0.676; 95% CI: 0.596, 0.767), but that advantage disappeared over time (OR = 0.924 in 2009; 95% CI: 0.804,1.061). There was virtually no difference in the trend for Hispanics and whites on the other health indicators (ORs ≈ 1.00 for the Hispanic × year interaction term). Thus, there is little indication that Hispanic-white relative disparities have changed appreciably over time.
Asians
As indicated, Asian children had a lower prevalence of the health indicators compared to all other groups. In fact, for 11 of the 17 indicators they had a significantly lower prevalence compared to all the other race/ethnic groups based on results from the pairwise comparisons (Table 3). We did not detect significant changes over time in the odds ratios for Asian-white disparities for any of the health indicators (Table 4). As shown in Fig. 1A, Asian children experienced slight increases in the prevalence of reported asthma, similar to white children. They appear to not have experienced any change in ADHD unlike the other race/ethnic groups, however, they did experience increases in prevalence of autism similar to the other race/ethnic groups.
Discussion
Our objective was to examine changes over time in race/ethnic disparities in child health. Unlike prior work, the strength of these analyses is the assessment of a comprehensive set of child health indicators and the implementation of a model-based approach to examine statistically significant changes in disparities over time. We examined both relative and absolute disparities. Our findings confirm prior reports of race/ethnic disparities across multiple child health indicators (Flores & Committee On Pediatric Research, 2010). Specifically, we found that black children generally had the highest prevalence of the global health indicators (overall health, disability) and most specific illnesses examined compared to the other race/ethnic groups. Nonetheless, they were less likely to miss more than 10% of the school year compared to white children. In contrast, Asian children appeared better off compared to all other race/ethnic groups. The results for Hispanics were more variable. Importantly, we found little evidence that race/ethnic disparities in child health have changed over time in a consistent way. For certain conditions such as asthma, black–white disparities grew significantly larger over the period of observation. For ADHD, black children appeared to have a lower prevalence in 1998 compared to white children, but that advantage disappeared by 2009. We detected large increases in the prevalence of autism over time, with proportionate and absolute increases being larger for whites compared to blacks and Hispanics.
Among the specific illnesses we examined, respiratory and skin allergies and asthma were the most highly prevalent indicators. Aggregate trends indicated significant increases in the prevalence of skin allergies with virtually no variation in the relative trend across the four main race/ethnic groups. In addition, the prevalence of asthma also significantly increased over time with apparently faster increases among black children compared to the other race/ethnic groups.
Prior research has also highlighted race/ethnic disparities in asthma and asthma-related care (Akinbami et al., 2009; Akinbami & Schoendorf, 2002; McDaniel et al., 2006; Piper, Glover, Elder, Baek, & Wilkinson, 2010; Stewart et al., 2010). Causes of the high burden of allergies and asthma in childhood have been the topic of recent debate. The “hygiene hypothesis” suggests that reductions in exposure to infectious agents and microbial contamination have increased risks of asthma for children in developed nations (Fishbein & Fuleihan, 2012; Greenwood, 2011; Liu & Murphy, 2003; Schaub, Lauener, & von Mutius, 2006). It is not clear how this hypothesis could explain growing black–white disparities in asthma. Other explanations that may be pertinent to the increasing disparity include differential exposure to substandard housing with high levels of asthma triggers (e.g., dust mites, cockroaches) (Bashir, 2002; Rauh, Chew, & Garfinkel, 2002) indoor and outdoor air pollutants (Gold & Wright, 2005; Gorman & Chu, 2009; Institute of Medicine, 2000; Rosenbaum, 2008), and childhood obesity (Gilliland et al., 2003). The contribution of these various factors to the growing disparity is not fully examined or understood.
We observed an increasing reported prevalence of developmental disabilities such as autism and ADHD over time, which is consistent with a prior investigation (Boyle et al., 2011). For autism, increased parental awareness and pediatrician diagnosis as well as decreased stigma associated with the condition are likely contributing factors (Boyle et al., 2011; Keyes et al., 2011). Changes in awareness, therefore, may mask the true underlying secular trend and an increasing trend may be largely due to the diagnosis of less severe cases that were undiagnosed previously (King & Bearman, 2009, 2011). Environmental risk factors, both social and physical have also been postulated as a contributor to changing risks, but their role has been debated (Grandjean & Landrigan, 2006; Keyes et al., 2011; King & Bearman, 2011; Palmer, Blanchard, Jean, & Mandell, 2005; Windham, Zhang, Gunier, Croen, & Grether, 2006).
One of the most noteworthy findings of our study is that black children appeared more likely to be diagnosed with autism in 1998 compared to white children, but were less likely to be diagnosed by 2009. It is not clear what may have prompted such a pattern. King and Bearman (2011) found that there was a strong positive association between SES and less severe cases of autism, while there was little association between SES and more severe cases. This finding supports the idea that more advantaged families (and those residing in affluent areas) are in a better position to seek and obtain a diagnosis of autism compared to others, particularly in the early stages of the disease and with less severe forms (King & Bearman, 2011). Such a phenomenon could also shed light on the black–white pattern observed here. Although we adjusted for family-level education, residual differences in socioeconomic resources between black and white children likely exist, contributing to the differential changes over time. Previous research has noted under-diagnoses of mental illnesses such as autism for black and other minority children compared to white children (Gourdine, Baffour, & Teasley, 2011). There has also been speculation that minority children are under-screened for autism spectrum disorders (ASD) by health professionals, which is possibly the result of statistical discrimination (Balsa & McGuire, 2001; Gibson, 2007; Mandell, Listerud, Levy, & Pinto-Martin, 2002; Mandell, Listerud, Levy, & Pinto-Martin, 2009).
In order to assess disparities in the potential consequences of childhood illnesses, we also examined disparities in missed school days due to illness. We found that black and Hispanic children were less likely to miss more than one week of school compared to white children, an advantage that grew over time (though differences in trends were not statistically significant). The missed school days variable is distinct from the other health indicators examined because it captures both the severity of childhood illness and the ability of families to provide childcare away from school. It is yet unclear why black children, who appear disadvantaged on most of the health indicators, would be advantaged on this indicator. One clue may lie with changing welfare policies, which resulted in increasing employment among single mothers and which may have disproportionately affected minority families. The Personal Responsibility and Work Opportunity Act instituted under the Clinton administration in 1996 created Temporary Assistance for Needy Families (TANF). This policy change resulted in large decreases in welfare caseloads and increases in the employment levels of single women with children, which rose from 56.9 percent in March 1994 to 73.9 percent in March 2000 (Grogger, Karoly, & Klerman, 2002; Hotz, Mullin, & Scholz, 2002). As a consequence, single mothers may have less ability to stay at home with ill children and fewer resources and support to find alternative forms of care for children. A recent report discusses the fact that parents without paid sick leave, which is more common in low paying jobs, are more likely to send their sick children to school (Gould, Filion, & Green, 2011). In addition, a review of research on the consequences of welfare reform found some evidence of negative effects on the health of children (Grogger et al., 2002).
Due to sample size constraints, we were unable to examine specific subgroups of Hispanic and Asian children. These groups are heterogeneous with respect to origin country, English proficiency, and citizenship; thus, there are considerable variations in health among these subgroups that are masked by the average levels we report. For example, infant mortality rates are higher among infants of mothers who are from Puerto Rico compared to that of those from Mexico and Cuba (Singh & van Dyck, 2010). Similarly, certain subgroups of Asian-origin children including those from Southeast Asia and Native Hawaiians may be at higher risk for poor physical health than that observed for other Asian-origin subgroups (Huang, Calzada, Cheng, & Brotman, 2012; National Center for Health Statistics, 2006). In addition, non-citizen Hispanics with limited English proficiency are more likely to be without health insurance, underutilize health care services, and be in poorer health than their English-speaking and U.S. citizen counterparts (Kaiser Family Foundation, 2003). This would lead to a relative underestimation of health burdens for this population. We found that Hispanic children with asthma were far more likely to visit the emergency room compared to white children with asthma despite these groups having a similar prevalence of asthma. This finding could partly reflect lower access to a regular source of primary care for Hispanic children, as these individuals more often resort to the ER for care (Self, Chrisman, Mason, & Rumbak, 2005).
We did not examine childhood obesity because disparities have been well described using measured height and weight data, which is unavailable in the NHIS. In a study using the National Health and Nutrition Examination Survey (NHANES), data from 2009 to 2010 indicate that approximately 17% of U.S. children aged 2–19 year of age were obese with non-Hispanic black and Hispanic children having a higher odds of being obese compared to non-Hispanic white children (Ogden, Carroll, Kit, & Flegal, 2012). This pattern was observed for both sexes. With respect to trends, the same study found that obesity significantly increased only among non-Hispanic black children during the 2000s (Ogden et al., 2012). Less research has been conducted on Asians, but existing work indicates that Asian children have considerably lower levels of obesity compared to the other race/ethnic groups (Singh & Kogan, 2011). Childhood obesity has been associated with multiple health and social outcomes among children, such as asthma, poor mental health and overall health (Daniels, 2006; Holguin et al., 2011; Williams & Jackson, 2005). It is possible that disparities in obesity could contribute to race/ethnic differences in other health outcomes as well. Further research is needed to fully disentangle these patterns. In addition, although we examine 17 health conditions, we do not include all possible health conditions that impact children. We may have missed relevant health indicators that assess child health. In fact, there continues to be much debate about the appropriate measures that should be used to evaluate child health status (Starfield, 2004; Stein, Stanton, & Starfield, 2005).
Our findings are subject to other limitations. A barrier to estimating race/ethnic differences in child health is that many childhood illnesses are rare. Large samples of children are required to obtain reliable estimates, particularly for race/ethnic minority subgroups. We did not detect many significant changes in race/ethnic trends in child health over time. Although our sample size was large, the power to detect these trends is limited. A recent systematic review of literature on racial/ethnic disparities in children's health identified multiple methodological flaws in how child health disparities were documented and analyzed (Flores & Committee on Pediatric Research, 2010). We improve upon prior literature by using nationally representative data and adjust for parental education and nativity status, which has been noted as a weakness in existing studies. Nonetheless, unmeasured confounding is possible and there may be interactive effects between race/ethnicity and SES (Chen, Martin, & Matthews, 2006). Finally, the NHIS utilizes parental/caretaker reports of specific child illnesses. It is possible that illnesses may be over- or under-reported by the respondent.
Child health disparities remain an understudied but critical area to health inequality research. The nature of race/ethnic health disparities among recent cohorts of children provides an important barometer of national well-being, and serves as a predictor of future patterns in adult disparities. Poor health during childhood likely contributes to poorer health and socioeconomic outcomes in adulthood (Ben-Shlomo & Kuh, 2002; Case, Fertig, & Paxson, 2005) and thus race/ethnic disparities in child health may contribute to future race/ethnic disparities in SES and health later in the life course. Our results document important race/ethnic disparities in child health and also suggest persistent and growing disparities for some health indicators over the 1998 to 2009 period, which warrants particular concern and research attention. The mechanisms that serve to explain the causes of these disparities likely differ across outcomes and over time. Future research should continue to investigate these mechanisms.
Our results also highlight the complexities in studying disparities and the need to consider the health and wellbeing of children of all racial/ethnic groups in the U.S. Indeed, research has shown that U.S. children are in generally worse health, by all standard indicators, than children in comparable industrialized countries (Duderstadt, 2007; Starfield, 2004; Stein et al., 2005). Therefore, policy goals to reduce racial/ethnic health disparities will not be as simple as aiming to give all racial/ethnic minority groups the health of white children, the general population, or even using U.S. racial/ethnic subpopulations with the “best” rate as the benchmark (Carter-Pokras & Baquet, 2002). Concerted efforts will be necessary to continue to identify, measure, and monitor appropriate indicators of child health for all population subgroups, improve overall child health across multiple indicators for the entire population, and reduce social disparities in these health indicators where they exist.
Acknowledgments
The authors would like to thank the Robert Wood Johnson Foundation Health and Society Scholars program for its financial support. Neil K. Mehta was additionally supported by the National Institute on Minority Health and Health Disparities' Loan Repayment Program. An earlier version of this paper was presented at the Population Association of America 2012 Annual Conference (San Francisco, CA). We thank Enrico A. Marcelli and three anonymous reviewers for their helpful comments. The content in this article is solely the responsibility of the authors and does not necessarily represent the official views of any agency.
References
- Agency for Healthcare Research and Quality. 2010 Healthcare disparities report. AHRQ; 2011. Publication No. 11-0005. [Google Scholar]
- Akinbami LJ, Moorman JE, Garbe PL, Sondik EJ. Status of childhood asthma in the United States, 1980–2007. Pediatrics. 2009;123(S3):S131–S145. doi: 10.1542/peds.2008-2233C. [DOI] [PubMed] [Google Scholar]
- Akinbami LJ, Schoendorf KC. Trends in childhood asthma: prevalence, health care utilization, and mortality. Pediatrics. 2002;110(2):315–322. doi: 10.1542/peds.110.2.315. [DOI] [PubMed] [Google Scholar]
- Allison P. Logistic regression using the SAS system. Cary, NC: SAS Institute, Inc; 1999. [Google Scholar]
- Balsa AI, McGuire TG. Statistical discrimination in health care. Journal of Health Economics. 2001;20:881–907. doi: 10.1016/s0167-6296(01)00101-1. [DOI] [PubMed] [Google Scholar]
- Bashir SA. Home is where the harm is: inadequate housing as a public health crisis. American Journal of Public Health. 2002;92(5):733–738. doi: 10.2105/ajph.92.5.733. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ben-Shlomo Y, Kuh D. A life course approach to chronic disease epidemiology: conceptual models, empirical challenges and interdisciplinary perspectives. International Journal of Epidemiology. 2002;31(2):285–293. [PubMed] [Google Scholar]
- Boyle CA, Boulet S, Schieve LA, Cohen RA, Blumberg SJ, Yeargin-Allsopp M, et al. Trends in the prevalence of developmental disabilities in US children, 1997–2008. Pediatrics. 2011;127:1034–1042. doi: 10.1542/peds.2010-2989. [DOI] [PubMed] [Google Scholar]
- Burt VL, Cutler JA, Higgins M, Horan MJ, Labarthe D, Whelton P, et al. Trends in the prevalence, awareness, treatment, and control of hypertension in the adult US population. Data from the health examination surveys, 1960 to 1991. Hypertension. 1995;26(1):60–69. doi: 10.1161/01.hyp.26.1.60. [DOI] [PubMed] [Google Scholar]
- Carter-Pokras O, Baquet C. What is a “health disparity”? Public Health Reports. 2002;117(5):426–434. doi: 10.1093/phr/117.5.426. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Case A, Fertig A, Paxson C. The lasting impact of childhood health and circumstance. Journal of Health Economics. 2005;24(2):365–389. doi: 10.1016/j.jhealeco.2004.09.008. [DOI] [PubMed] [Google Scholar]
- Chang HN, Romero M. Present, engaged, and accounted for: The critical importance of addressing chronic absence in the early grades. New York: National Center for Children in Poverty; 2008. [Accessed 09.07.12]. http://www.nccp.org/publications/pub_837.html. [Google Scholar]
- Chen E, Martin A, Matthews K. Understanding health disparities: the role of race and socioeconomic status in children's health. American Journal of Public Health. 2006;96(4):702–708. doi: 10.2105/AJPH.2004.048124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Crimmins EM, Saito Y. Trends in healthy life expectancy in the United States, 1970–1990: gender, racial, and educational differences. Social Science & Medicine. 2001;52(11):1629–1641. doi: 10.1016/s0277-9536(00)00273-2. [DOI] [PubMed] [Google Scholar]
- Cutler DM, Lleras-Muney A. Education and health: evaluating theories and evidence. In: Schoeni RF, House JS, Kaplan G, Pollack H, editors. Making Americans healthier: Social and economics policy as health policy. New York, NY: Russell Sage Foundation; 2008. [Google Scholar]
- Daniels SR. The consequences of childhood overweight and obesity. Future Child. 2006;16(1):47–67. doi: 10.1353/foc.2006.0004. [DOI] [PubMed] [Google Scholar]
- Dentzer S. A nation at risk for wider health disparities. Health Affairs. 2011;30(10):1818. doi: 10.1377/hlthaff.2011.1091. [DOI] [PubMed] [Google Scholar]
- Duderstadt KG. Health of U.S. children from the global view. Journal of Pediatric Health Care. 2007;21(6):403–406. doi: 10.1016/j.pedhc.2007.08.012. [DOI] [PubMed] [Google Scholar]
- Egan BM, Zhao Y, Axon RN. U.S. trends in prevalence, awareness, treatment, and control of hypertension, 1988–2008. Journal of the American Medical Association. 2010;303(20):2043–2050. doi: 10.1001/jama.2010.650. [DOI] [PubMed] [Google Scholar]
- Fishbein AB, Fuleihan RL. The hygiene hypothesis revisited: does exposure to infectious agents protect us from allergy? Current Opinion in Pediatrics. 2012;24(1):98–102. doi: 10.1097/MOP.0b013e32834ee57c. [DOI] [PubMed] [Google Scholar]
- Flores G Committee On Pediatric Research. Technical report–racial and ethnic disparities in the health and health care of children. Pediatrics. 2010;125(4):e979–e1020. doi: 10.1542/peds.2010-0188. [DOI] [PubMed] [Google Scholar]
- Flores G, Tomany-Korman S. Racial and ethnic disparities in medical and dental health, access to care, and use of services in US children. Pediatrics. 2008;121:e286–e298. doi: 10.1542/peds.2007-1243. [DOI] [PubMed] [Google Scholar]
- Gibson DD. Racial disparities in the age of diagnosis of autism spectrum disorder: examining factors that may contribute to delayed diagnosis in African–American children. PRAXIS. 2007;7:34–38. [Google Scholar]
- Gilliland FD, Berhane K, Islam T, McConnell R, Gauderman WJ, Gilliland SS, et al. Obesity and the risk of newly diagnosed asthma in school-age children. American Journal of Epidemiology. 2003;158(5):406–415. doi: 10.1093/aje/kwg175. [DOI] [PubMed] [Google Scholar]
- Gold D, Wright R. Population disparities in asthma. Annual Review of Public Health. 2005;26:89–113. doi: 10.1146/annurev.publhealth.26.021304.144528. [DOI] [PubMed] [Google Scholar]
- Gorman BK, Chu M. Racial and ethnic differences in adult asthma prevalence, problems, and medical care. Ethnicity & Health. 2009;14(5):527–552. doi: 10.1080/13557850902954195. [DOI] [PubMed] [Google Scholar]
- Gould E, Filion K, Green A. The need for paid sick days. Washington D.C: Economic Policy Institute; 2011. [Accessed 09.07.12]. http://www.epi.org/publication/the_need_for_paid_sick_days/ [Google Scholar]
- Gourdine RM, Baffour TD, Teasley M. Autism and the African American community. Social Work in Public Health. 2011;26(4):454–470. doi: 10.1080/19371918.2011.579499. [DOI] [PubMed] [Google Scholar]
- Grandjean P, Landrigan P. Developmental neurotoxicity of industrial chemicals. Lancet. 2006;368:2167–2178. doi: 10.1016/S0140-6736(06)69665-7. [DOI] [PubMed] [Google Scholar]
- Greenwood V. Why are asthma rates soaring? [Accessed 23.02.12];Scientific American. 2011 doi: 10.1038/scientificamerican0411-32. http://www.scientificamerican.com/article.cfm?id=why-are-asthma-rates-soaring. [DOI] [PubMed]
- Grogger J, Karoly LA, Klerman JA. Consequences of welfare reform: A research synthesis. RAND; 2002. [Accessed 27.02.12]. http://www.rand.org/pubs/drafts/DRU2676.html#src=mobile. [Google Scholar]
- Holguin FR, Bleecker E, Busse WW, Calhoun WJ, Castro M, Erzurum SC, et al. Obesity and asthma: an association modified by age of asthma onset. Journal of Allergy and Clinical Immunology. 2011;127(6):1486–1493.e2. doi: 10.1016/j.jaci.2011.03.036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hotz VJ, Mullin CH, Scholz JK. The effects of welfare reform on employment and income: Evidence from California. [Accessed 27.02.12];2002 http://ww.ssc.wisc.edu/˜scholz/Research/CWPDP_paper_version6.pdf.
- Huang KY, Calzada E, Cheng S, Brotman LM. Physical and mental health disparities among young children of Asian immigrants. Journal of Pediatrics. 2012;160(2):331–336. doi: 10.1016/j.jpeds.2011.08.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Institute of Medicine. Clearing the air: Asthma and indoor air exposures. Washington, DC: National Academies Press; 2000. [PubMed] [Google Scholar]
- Jones CP, LaVeist TA, Lillie-Blanton M. “Race” in the epidemiologic literature: an examination of the American Journal of Epidemiology, 1921–1990. American Journal of Epidemiology. 1991;134(10):1079–1084. doi: 10.1093/oxfordjournals.aje.a116011. [DOI] [PubMed] [Google Scholar]
- Kaiser Family Foundation. [Accessed 09.03.12];How race/ethnicity, immigration status, and language affect health insurance coverage, access to and quality of care among the low-income population. 2003 http://www.kff.org/uninsured/kcmu4132report.cfm.
- Keyes KM, Susser E, Cheslack-Postava K, Fountain C, Liu K, Bearman PS. Cohort effects explain the increase in autism diagnosis among children born in 1992 to 2003 in California. International Journal of Epidemiology. 2011:1–9. doi: 10.1093/ije/dyr193. [DOI] [PMC free article] [PubMed] [Google Scholar]
- King M, Bearman P. Diagnostic change and the increased prevalence of autism. International Journal of Epidemiology. 2009;38:1224–1234. doi: 10.1093/ije/dyp261. [DOI] [PMC free article] [PubMed] [Google Scholar]
- King MD, Bearman PS. Socioeconomic status and the increased prevalence of autism in California. American Sociological Review. 2011;76(2):320–346. doi: 10.1177/0003122411399389. [DOI] [PMC free article] [PubMed] [Google Scholar]
- King G, Zeng L. Logistic regression in rare events data. Political Analysis. 2001;9:137–163. [Google Scholar]
- Koh HK, Graham G, Glied SA. Reducing racial and ethnic disparities: the action plan from the Department of Health and Human Services. Health Affairs. 2011;30:1822–1829. doi: 10.1377/hlthaff.2011.0673. [DOI] [PubMed] [Google Scholar]
- Krieger N, Chen JT, Waterman PD, Rehkopf DH, Subramanian SV. Painting a truer picture of US socioeconomic and racial/ethnic health inequalities: the Public Health Disparities Geocoding Project. American Journal of Public Health. 2005;95:312–323. doi: 10.2105/AJPH.2003.032482. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Krieger N, Williams D, Moss N. Measuring social class in US public health research: concepts, methodologies, and guidelines. Annual Review Public Health. 1997;18:341–378. doi: 10.1146/annurev.publhealth.18.1.341. [DOI] [PubMed] [Google Scholar]
- LaVeist T. Disentangling race and socioeconomic status: a key to understanding health inequalities. Journal of Urban Health. 2005;82(2):iii26–iii34. doi: 10.1093/jurban/jti061. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee JW, Brancati FL, Yeh HC. Trends in the prevalence of type 2 diabetes in Asians versus whites: results from the United States National Health Interview Survey, 1997–2008. Diabetes Care. 2011;34(2):353–357. doi: 10.2337/dc10-0746. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Link BG, Phelan J. Social conditions as fundamental causes of disease. Journal of Health and Social Behavior. 1995:80–94. Spec No. [PubMed] [Google Scholar]
- Liu AH, Murphy JR. Hygiene hypothesis: fact or fiction? Journal of Allergy and Clinical Immunology. 2003;111(3):471–478. doi: 10.1067/mai.2003.172. [DOI] [PubMed] [Google Scholar]
- McDaniel M, Paxson C, Waldfogel J. Racial disparities in childhood asthma in the United States: evidence from the National Health Interview Survey, 1997 to 2003. Pediatrics. 2006;117(5):e868–e877. doi: 10.1542/peds.2005-1721. [DOI] [PubMed] [Google Scholar]
- Mandell DS, Listerud J, Levy SE, Pinto-Martin JA. Race differences in the age at diagnosis among medicaid-eligible children with autism. Journal of the American Academy of Child and Adolescent Psychiatry. 2002;41(12):1447–1453. doi: 10.1097/00004583-200212000-00016. [DOI] [PubMed] [Google Scholar]
- Mandell DS, Wiggins LD, Carpenter LA, Daniels J, DiGuiseppi C, Durkin MS, et al. Racial/ethnic disparities in the identification of children with autism spectrum disorders. American Journal of Public Health. 2009;99(3):493–498. doi: 10.2105/AJPH.2007.131243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Minnesota Population Center and State Health Access Data Assistance Center. Integrated health interview series: Version 5.0. Minneapolis: University of Minnesota; 2012. Available at http://www.ihis.us. [Google Scholar]
- Moss M, Mannino DM. Race gender differences in acute respiratory distress syndrome deaths in the United States: an analysis of multiple-cause mortality data (1979–1996) Critical Care Medicine. 2002;30(8):1679–1685. doi: 10.1097/00003246-200208000-00001. [DOI] [PubMed] [Google Scholar]
- National Center for Health Statistics. Health, United States, 2006: With chartbook on trends in the health of Americans. Hyattsville, MD: 2006. [PubMed] [Google Scholar]
- National Center for Health Statistics. Centers for Disease Control and Prevention. [Accessed 09.03.12];About the National Health Interview Survey. 2012 http://www.cdc.gov/nchs/nhis/about_nhis.htm.
- National Research Council (2004) Children's health, the nation's wealth: Assessing and improving child health. Washington, DC: The National Academies Press; [Google Scholar]
- Ogden CL, Carroll MD, Kit BK, Flegal KM. Prevalence of obesity and trends in body mass index among US children and adolescents, 1999–2010. Journal of the American Medical Association. 2012;307(5):483–490. doi: 10.1001/jama.2012.40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ortman JM, Guarneri CE. [Accessed 27.02.12];United States population projections: 2000 to 2050. 2009 http://www.census.gov/population/www/projections/analytical-document09.pdf.
- Palmer RF, Blanchard S, Jean CR, Mandell DS. School district resources and identification of children with autistic disorder. American Journal of Public Health. 2005;95:125–130. doi: 10.2105/AJPH.2003.023077. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Piper CN, Glover S, Elder K, Baek JD, Wilkinson L. Disparities in access to care among asthmatic children in relation to race and socioeconomic status. Journal of Child Health Care. 2010;14(3):271–279. doi: 10.1177/1367493510371629. [DOI] [PubMed] [Google Scholar]
- Rauh V, Chew G, Garfinkel R. Deteriorated housing contributed to high cockroach allergen levels in inner-city households. Environmental Health Perspectives. 2002;110(Supplement 2):323–327. doi: 10.1289/ehp.02110s2323. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rosenbaum E. Racial/ethnic differences in asthma prevalence: the role of housing and neighborhood environments. Journal of Health and Social Behavior. 2008;49:131–145. doi: 10.1177/002214650804900202. [DOI] [PubMed] [Google Scholar]
- Schaub B, Lauener R, von Mutius E. The many faces of the hygiene hypothesis. Journal of Allergy and Clinical Immunology. 2006;117(5):969–977. doi: 10.1016/j.jaci.2006.03.003. [DOI] [PubMed] [Google Scholar]
- Self TH, Chrisman CR, Mason DL, Rumbak MJ. Reducing emergency department visits and hospitalizations in African American and Hispanic patients with asthma: a 15-year review. Journal of Asthma. 2005;42:807–812. doi: 10.1080/02770900500369835. [DOI] [PubMed] [Google Scholar]
- Singh GK, Kogan MD. Contemporary racial/ethnic and socioeconomic patterns in U.S. childhood obesity. In: Bagchi D, editor. Global perspectives on childhood obesity: Current status, consequences, and prevention. London: Academic Press; 2011. pp. 71–85. [Google Scholar]
- Singh GK, van Dyck PC. Infant mortality in the United States, 1935–2007: Over Seven Decades of progress and disparities; A 75th Anniversary Publication Health Resources and Services Administration, Maternal and Child Health Bureau; Rockville, Maryland. U.S. Department of Health and Human Services; 2010. [Accessed 06.03.12]. http://www.mchb.hrsa.gov/ [Google Scholar]
- Starfield B. U.S. child health: what's amiss, and what should be done about it? Health Affairs. 2004;23(5):165–170. doi: 10.1377/hlthaff.23.5.165. [DOI] [PubMed] [Google Scholar]
- Stein REK, Stanton B, Starfield B. How healthy are U.S. children? Journal of the American Medical Association. 2005;293(14):1781–1783. doi: 10.1001/jama.293.14.1781. [DOI] [PubMed] [Google Scholar]
- Stewart KA, Higgins PC, McLaughlin CG, Williams TV, Granger E, Croghan TW. Differences in prevalence, treatment, and outcomes of asthma among a diverse population of children with equal access to care: findings from a study in the military health system. Archives of Pediatrics & Adolescent Medicine. 2010;164(8):720–726. doi: 10.1001/archpediatrics.2010.100. [DOI] [PubMed] [Google Scholar]
- U.S. Census Bureau, Current Population Survey. Annual Social and Economic Supplement. [Accessed 27.02.12];Age and sex in the United States: 2010. 2010 http://www.census.gov/population/www/socdemo/age/age_sex_2010.html.
- U.S Department of Health and Human Services. Healthy People 2020. [Accessed 27.02.12];Foundation health measures: Disparities. 2010 http://www.healthypeople.gov/2020/about/DisparitiesAbout.aspx.
- Williams DR. The concept of race in health services research: 1966 to 1990. Health Services Research. 1994;29(3):261–274. [PMC free article] [PubMed] [Google Scholar]
- Williams DR, Collins C. US socioeconomic and racial differences in health: patterns and explanations. Annual Review of Sociology. 1995;21:349–386. [Google Scholar]
- Williams DR, Jackson PB. Social sources of racial disparities in health. Health Affairs. 2005;24(2):325–334. doi: 10.1377/hlthaff.24.2.325. [DOI] [PubMed] [Google Scholar]
- Williams DR, Mohammed SA, Leavell J, Collins C. Race, socioeconomic status and health: complexities, ongoing challenges and research opportunities. Annals of the New York Academy of Sciences. 2010;1186:69–101. doi: 10.1111/j.1749-6632.2009.05339.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Windham GC, Zhang L, Gunier R, Croen LA, Grether JK. Autism spectrum disorders in relation to the distribution of hazardous air pollutants in the San Francisco bay area. Environmental Health Perspectives. 2006;114:1438–1444. doi: 10.1289/ehp.9120. [DOI] [PMC free article] [PubMed] [Google Scholar]