Abstract
Objective
To examine racial and ethnic differences in self-care and mobility outcomes for persons with a motor complete, traumatic spinal cord injury (SCI) at discharge and 1-year follow-up.
Design
Retrospective cohort study.
Setting
Sixteen rehabilitation centers contributing to the Spinal Cord Injury Model Systems (SCIMS) database.
Participants
Adults with traumatic, motor complete SCI (N=1766; American Spinal Injury Association Impairment Scale grade A or B) enrolled in the SCIMS between 2000 and 2011. Selected cases had complete self-reported data on race and ethnicity (non-Hispanic white, non-Hispanic black, or Hispanic) and motor FIM scores assessed at inpatient rehabilitation admission, discharge, and 1-year follow-up.
Interventions
Not applicable.
Main Outcome Measures
Functional outcomes were measured by FIM self-care and mobility scores on a 1 to 7 FIM scale, at discharge and 1-year follow-up.
Results
Multiple regression models stratified by neurologic category and adjusted for sociodemographic and injury characteristics assessed racial and ethnic group differences in FIM self-care and mobility change scores at discharge and 1-year follow-up. At discharge, non-Hispanic black participants with tetraplegia and paraplegia had significantly poorer gains in FIM self-care and mobility scores relative to non-Hispanic white and Hispanic participants. At 1-year follow-up, similar FIM self-care and mobility change scores were found across racial and ethnic groups within each neurologic category.
Conclusions
Non-Hispanic white and Hispanic participants had comparatively more improvement in self-care and mobility during inpatient rehabilitation compared with non-Hispanic black participants. At 1-year follow-up, no differences in self-care and mobility outcomes were observed across racial and ethnic groups. Additional research is needed to identify potential modifiable factors that may contribute to racially and ethnically different patterns of functional outcomes observed during inpatient rehabilitation.
Keywords: Activities of daily living, Health status disparities, Motor activity, Rehabilitation, Spinal cord injuries
Spinal cord injury (SCI) is a sudden and debilitating injury that results in paralysis, sensory deficits, and drastically altered function and quality of life.1–3 According to the National Spinal Cord Injury Statistical Center, approximately 275,000 individuals in the United States are living with SCI, with roughly 12,000 new cases of SCI reported annually.4,5 The 3 largest racial and ethnic groups living with a traumatic SCI are non-Hispanic white (64.4%), non-Hispanic black (24.4%), and His-panic (7.9%), respectively.6
As the proportion of racial and ethnic minorities with SCI has increased over the past 3 decades, health disparities research in SCI has begun to reveal important differences in health outcomes among racial and ethnic groups. Racial and ethnic minorities living with an SCI are at increased risk of secondary health complications,7–9 psychological distress,10,11 poorer quality of life,11,12 and having inadequate wheelchair quality.13,14 For example, non-Hispanic black individuals living with SCI have higher rates of severe pressure ulcers requiring invasive treatment than their Hispanic and non-Hispanic white counterparts.8,15,16 Non-Hispanic black and Hispanic women with SCI also report more depressive symptoms in comparison to non-Hispanic black men and non-Hispanic white women and men.17,18 Only a fraction of persons with SCI attain gainful employment postinjury, and this socioeconomic problem is magnified by a significant employment gap observed between non-Hispanic whites and minority groups.19–21 Any combination of these negative outcomes can impose an additional burden on health status, community integration and participation, and readjustment to life after an SCI for minority groups.
Despite the increased focus on the occurrence and implications of health disparities in medical rehabilitation, few SCI studies have examined the association between race and ethnicity on functional outcomes. Functional outcomes are the key predictors of SCI health status, community integration/participation, and quality of life, as well as quality indicators of inpatient rehabilitation facilities.22,23 Self-care and mobility are key domains of SCI rehabilitation used in the classification of therapeutic interventions24–26 as well as constructs of commonly used rehabilitation outcome measures, such as the FIM.27–29
Few published studies have used the Spinal Cord Injury Model Systems (SCIMS) data set to examine the impact of race and ethnicity on functional outcomes. Of these, 3 studied FIM scores from admission to discharge from inpatient rehabilitation,30–32 while only 1 study analyzed changes in functional outcomes after discharge and up to 12 months postinjury.33 While these previous studies observed similar functional outcomes across racial and ethnic groups with SCI, their findings were limited by (1) relatively small sample sizes; (2) limited statistical power to disaggregate racial and ethnic differences (ie, these studies compared only white and black rather than non-Hispanic white, non-Hispanic black, and Hispanic groups), which does not account for the cultural diversity of individuals living with SCI and the potential impact of race and ethnicity on functional outcomes; and (3) broad functional measures that failed to capture clinically important aspects of functional gains over time, such as self-care and mobility.34,35 This cohort study builds on the current literature by examining the effect of race and ethnicity on self-care and mobility outcomes in individuals living with SCI at rehabilitation discharge and 1 year postinjury, after controlling for key sociodemographic and injury characteristics.
Methods
Data source
Secondary data analyses were conducted using data extracted from the SCIMS database (sponsored by the U.S. Department of Education’s National Institute on Disability and Rehabilitation Research). The SCIMS database is a longitudinal repository of clinical, psychosocial, health, and functional data on patients with traumatic SCI.36 In-depth descriptions of the SCIMS database history and methods are described elsewhere.4,36–38 Each center has approval by its local institutional review board, and the primary site for the current study obtained approval from the institutional review board to conduct the current analysis.
Analytic sample
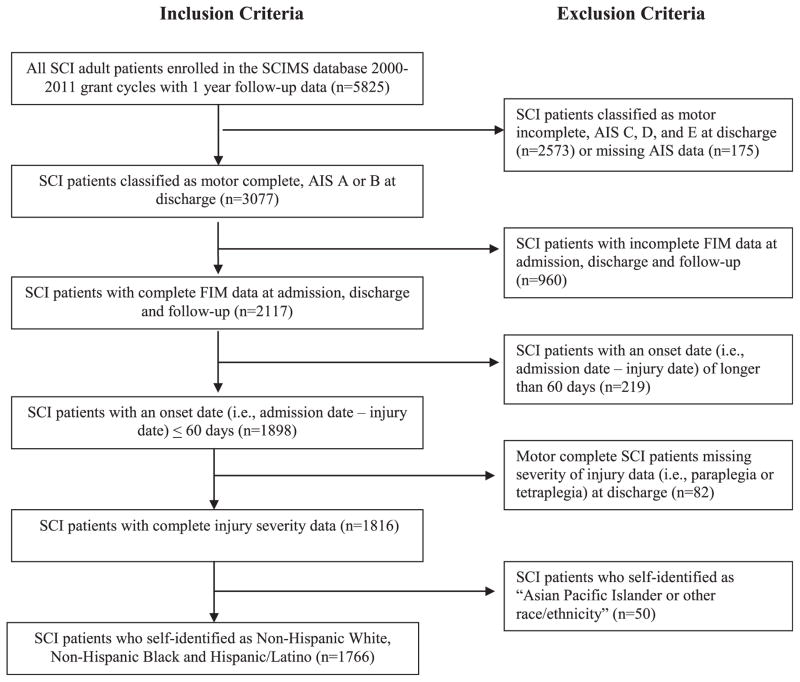
The study sample was derived from acute rehabilitation programs and 1-year follow-up data from persons with traumatic SCI enrolled in the SCIMS database between 2000 and 2011. A total of 16 unique rehabilitation facilities were included in the SCIMS database during the 2000 to 2006 and 2006 to 2011 SCIMS grant cycles. During these grant cycles, 11 rehabilitation facilities were consistently in both grant periods being studied. Inclusion criteria were informed by previous research and the Consortium for Spinal Cord Medicine’s clinical practice guidelines,23,39 to ensure our comparison groups were functionally similar. Sampling targeted (1) individuals from the 3 largest racial and ethnic groups included in the SCIMS database—persons who self-identified as non-Hispanic white, non-Hispanic black, and Hispanic; (2) persons classified with motor complete American Spinal Injury Association Impairment Scale grade A or B at discharge, consistent with the Consortium for Spinal Cord Medicine’s clinical practice guidelines23; (3) complete diagnostic information related to neurologic level of injury obtained at discharge; (4) onset date (ie, the period from injury data to admission date was <60 days), to ensure the similar clinical profiles (ie, minimize risk of major secondary complications associated with an SCI during acute care)40; and (5) complete FIM data at rehabilitation admission, discharge, and 1-year follow-up. Sampling methods are illustrated in figure 1 and yielded a final sample of 1766 participants. The proportions of non-Hispanic white, non-Hispanic black, and Hispanic participants were 62.6%, 25.5%, and 11.9%, respectively. When we compare the motor complete SCI cases missing FIM data with the motor complete cases not missing data, we found the following: (1) a small proportion of non-Hispanic whites were missing FIM data (P<.05); and (2) the group excluded for missing FIM data had significantly lower FIM self-care at admission (P<.05) and mobility scores at discharge (P<.01).
Fig. 1.
Sample derivation. Abbreviation: AIS, American Spinal Injury Association Impairment Scale.
Independent variable
Racial and ethnic group differences in functional independence are the primary focus of the current analysis. The SCIMS collects self-identified data about race (ie, white, black, Native American, Eskimo or Aleut, Asian or Pacific Islander) separately from ethnicity (Hispanic origin). Hispanic origin is not mutually exclusive from racial categories; however, we prioritized Hispanic identity for those individuals who self-identified as being of Hispanic origin. The final race/ethnicity variable used in the analyses distinguished respondents who are non-Hispanic white, non-Hispanic black, and Hispanic.
Stratification criteria and covariates: injury characteristics
The SCIMS centers use standardized methods for the neurologic examination and classification of SCI based on the International Standards for Neurological Classification of Spinal Cord Injury.41 The sample was stratified based on the following neurologic categories: tetraplegia (C1-8) and paraplegia (T1 and below). Based on the 8 levels of injury outlined in the Consortium for Spinal Cord Medicine’s clinical practice guidelines,23 we adjusted for T1-9, T10-L1, and L2-S2 levels of lesions among participants with paraplegia, and adjusted for C1-3, C4, C5, C6, and C7-8 levels of lesions among participants with tetraplegia.42 We controlled for the leading causes of SCI including vehicular collisions, falls, violence, and other (ie, surgical, medical, and pedestrian).
Sociodemographic covariates
Informed by prior studies,21,43–47 the following sociodemographic characteristics were included in our analyses because of their potential association with functional outcomes: (1) age at injury, which was skewed and recoded as a categorical variable—18 to 29 years, 30 to 49 years, and >50 years; (2) sex; (3) marital status, which was coded into 3 categories—single, no longer married including divorced and separated, and married; (4) educational attainment, which was coded into 3 categories—less than high school (up to grade 12), high school diploma (grade 12 or equivalent)/general equivalency diploma, and some college or greater; and (5) self-reported preinjury employment status, which was coded into 2 categories—unemployed (ie, unemployed, homemaker, student, retired, or other) and employed. The regression analyses included only preinjury demographic characteristics.
Outcome variables
Functional outcomes were measured using 11 motor FIM items. FIM items are rated on a scale of 1 (ie, total dependence) to 7 (ie, complete independence). We divided the motor FIM into 2 subdomains for analysis: self-care and mobility. The SCIMS collects FIM scores assessed during rehabilitation by trained clinicians, while follow-up scores are conducted by trained interviewers. Self-care was measured by summing 6 items (ie, eating, grooming, bathing, upper body dressing, lower body dressing, toileting) and dividing by the number of self-care items to maintain a metric (1–7) common with the original FIM rating scale. Similarly, mobility was measured by summing 5 items (ie, bed/wheelchair transfer, toilet transfer, tub/shower transfer, walk/wheelchair, stairs) and dividing by the number of items to enhance the interpretability of the scores in the multivariate analyses. Self-care and mobility scores demonstrated adequate internal consistency and reliability at admission (α=.81 and α=.63, respectively), discharge (α=.95 and α=.85, respectively), and 1-year follow-up (α=.95 and α= .84, respectively).
We assessed 2 sets of functional outcomes: (1) mean FIM self-care and mobility scores at discharge and 1-year follow-up; and (2) change in FIM self-care and mobility scores. We assessed change in FIM self-care and mobility scores at inpatient rehabilitation discharge (ie, discharge FIM score minus admission FIM score) and at 1-year follow-up (ie, 1-year follow-up FIM score minus discharge FIM score).
Statistical analyses
Chi-square and t tests analyses were used to assess racial and ethnic group differences across the covariates. For each neurologic category and at each time point, we compared the unadjusted mean FIM self-care and mobility scores as well as FIM self-care and mobility gains by racial and ethnic group and injury level by using analysis of variance and the Benjamini and Hochberg post hoc method. We calculated effect size to compare the magnitude of the differences in FIM change scores across the 3 racial and ethnic groups between admission, discharge, and 1-year follow-up.48,49 Effect size is defined as the mean change score divided by the pooled SD.48,49 We used Cohen’s general definitions of small (0.2), medium (0.4–0.5) and large (0.8) to interpret the effect size estimates.50
Linear regression models quantified the effect of race and ethnicity on change in FIM self-care and mobility scores. The models adjusted for admission FIM self-care or mobility scores, age at injury, injury etiology, neurologic level at discharge, sex, marital status, education level, and preinjury employment status. The reference categories for injury characteristics were based on the lowest level of lesion at rehabilitation discharge among cervical (eg, C1-3) and thoracic injuries (eg, T1-9). Reference categories for the demographic and socioeconomic covariates were selected based on indicators of socioeconomic advantage (ie, previously employed, more years of education). The Benjamini and Hochberg post hoc method was applied to determine the probability of type 1 errors and to confirm the significance of the regressions models. Data were analyzed using SPSS version 21a software.
Results
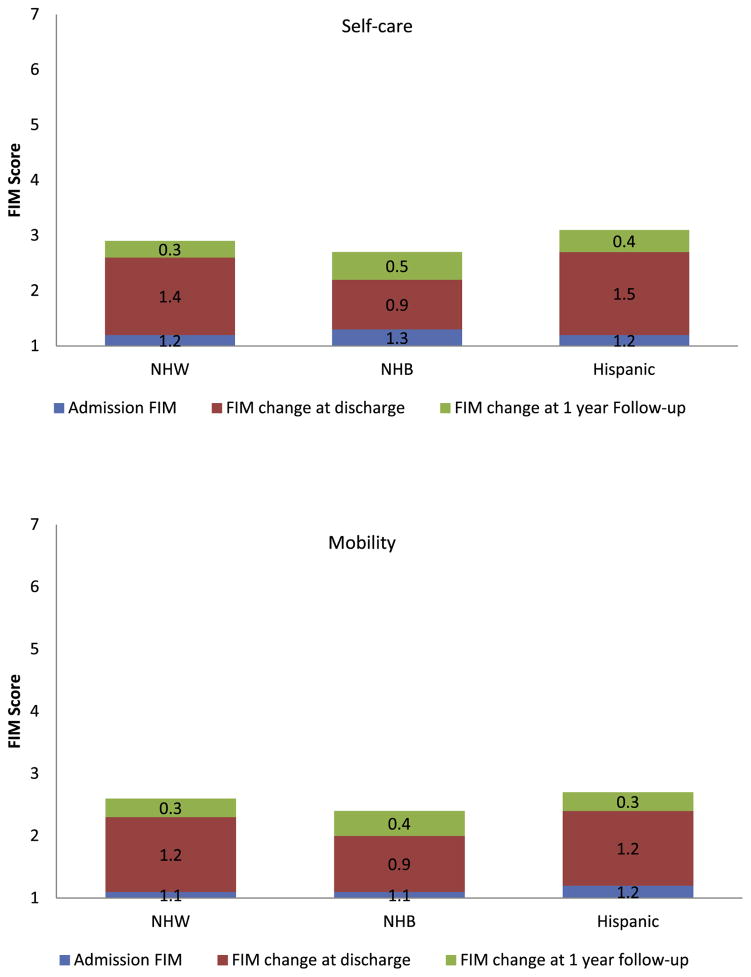
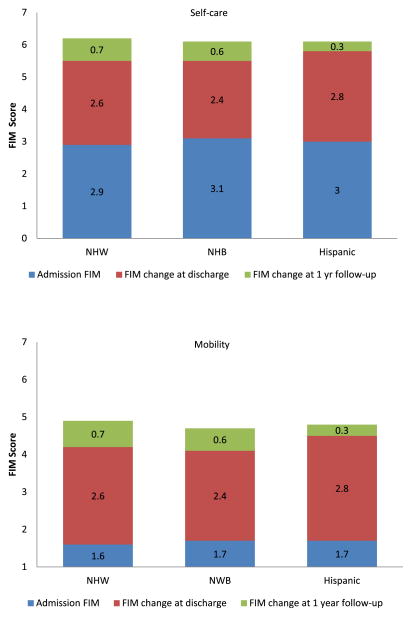
Table 1 compares the sociodemographic and injury characteristics, and FIM self-care and mobility scores across racial and ethnic groups within neurologic categories. Non-Hispanic white participants (mean age=36.4±14.0y) with paraplegia were older at the time of their injury than non-Hispanic black (mean age=29.3±9.7y) and Hispanic (mean age=30.8±10.3y) participants (F=35.5, P=.001). Among participants with tetraplegia and paraplegia, non-Hispanic whites were more likely to report completing some college, in comparison to non-Hispanic black and Hispanic participants (tetraplegia: χ24=84.1, P=.001; paraplegia: χ24=91.2, P=.001). On average, non-Hispanic black participants were more likely to report being unemployed pre-injury relative to non-Hispanic white and Hispanic participants (tetraplegia: χ22=19.0, P=.001; paraplegia: χ22=61.8, P=.001). Non-Hispanic black participants with paraplegia were disproportionately injured from acts of violence in comparison to non-Hispanic white and Hispanic participants (χ24=62.8, P=.001).51,52 The unadjusted mean and change in FIM self-care and mobility scores by race and ethnicity at rehabilitation admission, discharge, and 1-year follow-up are shown in table 2 (including effect sizes) and figures 2 and 3.
Table 1.
Sociodemographic and injury characteristics by neurologic category across racial and ethnic groups
| Characteristics | Tetraplegia
|
Paraplegia
|
||||||
|---|---|---|---|---|---|---|---|---|
| Total Tetraplegia (n=756) |
Non-Hispanic White (n=506) |
Non-Hispanic Black (n=155) |
Hispanic (n=95) |
Total Paraplegia (n=1010) |
Non-Hispanic White (n=600) |
Non-Hispanic Black (n=295) |
Hispanic (n=115) |
|
| Demographics | ||||||||
| Age at injury (y) | 35.3±13.3 | 36.0±14.1 | 34.6±12.0 | 32.5±10.9 | 33.7±13.0 | 36.4±14.0 | 29.3±9.7* | 30.8±10.3* |
| 18–29 | 41.7 | 40.7 | 41.3 | 47.4 | 46.8 | 39.8 | 59.0 | 52.2 |
| 30–49 | 41.9 | 40.3 | 47.1 | 42.1 | 40.0 | 41.5 | 36.6 | 40.9 |
| ≥50 | 16.4 | 19.0 | 11.6 | 10.5 | 13.2 | 18.7 | 4.4* | 7.0* |
| Sex | ||||||||
| Male | 82.3 | 81.2 | 83.9 | 85.3 | 83.4 | 80.3 | 89.5† | 83.5 |
| Marital status | ||||||||
| Single | 47.3 | 44.4 | 55.5* | 49.5 | 52.5 | 41.3 | 74.2* | 54.8 |
| No longer married | 17.1 | 17.7 | 18.1 | 12.6 | 13.6 | 16.0 | 9.2 | 12.2 |
| Married | 35.5 | 37.9 | 26.5 | 37.9 | 34.0 | 42.7 | 16.6 | 33.0 |
| Socioeconomic factors | ||||||||
| Education | ||||||||
| < HS | 14.1 | 7.1* | 27.2 | 31.5 | 20.1 | 10.9* | 31.0 | 38.9 |
| HS/GED | 63.0 | 63.5 | 64.2 | 58.4 | 60.6 | 63.8 | 56.9 | 54.0 |
| Some college + | 22.8 | 29.4* | 8.6 | 10.1 | 19.3 | 25.3* | 12.1 | 7.1 |
| Employment status | ||||||||
| Preinjury employment status | ||||||||
| Unemployed | 18.9 | 15.1 | 31.1* | 19.8 | 21.0 | 14.0 | 36.8* | 17.7 |
| Employed | 81.1 | 84.9 | 68.9* | 80.2 | 79.0 | 86.0 | 63.2* | 82.3 |
| Postinjury employment status | ||||||||
| Unemployed | 92.6 | 90.9 | 98.1‡ | 92.6 | 84.9 | 79.8 | 93.6* | 89.6 |
| Employed | 7.4 | 9.1 | 1.9‡ | 7.4 | 15.1 | 20.2* | 6.4 | 10.4 |
| Injury characteristics | ||||||||
| Injury etiology | ||||||||
| Vehicular | 49.7 | 50.2 | 51.3 | 44.7 | 38.8 | 45.2 | 26.1* | 38.6 |
| Falls | 19.5 | 19.1 | 18.2 | 23.4 | 23.9 | 31.4 | 7.5 | 27.2 |
| Violence | 8.8 | 3.6 | 22.7* | 13.8* | 24.6 | 6.4 | 61.0* | 25.4† |
| Sports | 20.0 | 25.1 | 5.8* | 16.0 | 7.9 | 11.9 | 1.4* | 3.5* |
| Surgical/medical | 0.8 | 0.8 | 0.6 | 1.1 | 3.5 | 4.0 | 2.4 | 3.5 |
| Pedestrian | 1.2 | 1.2 | 1.3 | 1.1 | 1.3 | 1.0 | 1.7 | 1.8 |
| Neurologic level at discharge | ||||||||
| C1-3 (n=68) | 9.0 | 8.7 | 9.7 | 9.5 | NA | NA | NA | NA |
| C4 (n=263) | 34.8 | 33.8 | 38.1 | 34.7 | NA | NA | NA | NA |
| C5 (n=207) | 27.4 | 27.7 | 26.5 | 27.4 | NA | NA | NA | NA |
| C6 (n=148) | 19.6 | 20.6 | 15.5 | 21.1 | NA | NA | NA | NA |
| C7-8 (n=70) | 9.3 | 9.3 | 10.3 | 7.4 | NA | NA | NA | NA |
| T1-9 (n=585) | NA | NA | NA | NA | 57.9 | 57.3 | 58.0 | 60.9 |
| T10-L1 (n=385) | NA | NA | NA | NA | 38.1 | 38.2 | 38.6 | 36.5 |
| L2-S2 (n=40) | NA | NA | NA | NA | 4.0 | 4.5 | 3.4 | 2.6 |
| Length of stay (no. of days from acute rehabilitation to discharge) | ||||||||
| Mean ± SD | 78.8±44.4 | 82.7±45.0 | 68.0±42.1† | 75.6±42.6 | 52.5±33.2 | 54.1±33.6 | 48.2±32.2‡ | 55±33.0 |
| Median | 67.0 | 72.0 | 57.0 | 63.0 | 43.0 | 45.0 | 38.0 | 46.5 |
| Admission rehabilitation motor FIM scores | ||||||||
| Self-care (6 items) | 1.3±0.6 (1.0–5.0) | 1.2±0.5 (1.0–4.0) | 1.3±0.7 (1.0–5.0) | 1.2±0.5 (1.0–3.5) | 3.0±0.8 (1.0–6.5) | 2.9±0.9 (1.0–6.3) | 3.1±0.8‡ (1.0–6.5) | 3.0±0.8 (1.3–5.1) |
| Mobility (5 items) | 1.1±0.3 (1.0–3.6) | 1.1±0.3 (1.0–3.4) | 1.1±0.3 (1.0–3.6) | 1.2±0.3 (1.0–3.0) | 1.7±0.7 (1.0–5.6) | 1.6±0.7 (1.0– 5.4) | 1.7±0.6 (1.0–4.6) | 1.7±0.8 (1.0–5.6) |
| Discharge motor FIM scores | ||||||||
| Self-care (6 items) | 2.6±1.4 (1.0–6.6) | 2.6±1.5 (1.0–6.6) | 2.2±1.2 (1.0–6.5) | 2.8±1.4† (1.0–6.3) | 5.5±1.0 (1.5–7.0) | 5.5±1.0 (1.5–7.0) | 5.5±1.0 (1.5–7.0) | 5.9±0.8‡ (2.67–7.0) |
| Mobility (5 items) | 2.2±0.9 (1.0–6.4) | 2.3±1.0 (1.0–6.2) | 2.0±0.9 (1.0–6.4) | 2.4±0.9† (1.0–5.0) | 4.2±1.0 (1.0–7.0) | 4.2±1.0 (1.0– 7.0) | 4.2±0.9 (1.0–6.0) | 4.4±0.8‡ (2.0–6.0) |
| 1-year follow-up motor FIM scores | ||||||||
| Self-care (6 items) | 3.0±1.8 (1.0–7.0) | 3.0±1.8 (1.0–7.0) | 2.8±1.8 (1.0–7.0) | 3.2±1.8 (1.0–7.0) | 6.2±1.0 (1.5–7.0) | 6.2±1.0 (1.5– 7.0) | 6.1±1.1 (1.6–7.0) | 6.2±0.9 (3.1–7.0) |
| Mobility (5 items) | 2.5±1.4 (1.0–7.0) | 2.6±1.4 (1.0–7.0) | 2.3±1.3 (1.0–6.8) | 2.7±1.3 (1.0–5.8) | 4.8±1.1 (1.0–7.0) | 4.8±1.1 (1.0– 7.0) | 4.7±1.1 (1.0–6.8) | 4.8±1.1 (1.0–7.0) |
NOTE. Values are mean ± SD, %, mean ± SD (range), or as otherwise indicated. FIM self-care ratings were calculated by the sum of 6 items (ie, eating, grooming, bathing, upper body dressing, lower body dressing, toileting) and divided by the number of items. FIM mobility ratings were calculated by the sum of 5 items (ie, bed/wheelchair transfer, toilet transfer, tub/shower transfer, walk/wheelchair, stairs) and divided by the number of items.
Abbreviations: GED, general equivalency diploma; HS, high school; NA, not applicable.
P<.001.
P<.01.
P<.05.
Table 2.
Effect size calculations based on unadjusted mean change in FIM self-care and mobility scores
| FIM Subscale | Racial/Ethnic Group Comparison | Admission to Discharge Change FIM Scores | Effect Size | Discharge to 1-Year Follow-Up Change FIM Scores | Effect Size | Admission to 1-Year Follow-Up Change FIM Scores | Effect Size |
|---|---|---|---|---|---|---|---|
| Tetraplegia (n=756) | |||||||
| Self-care | |||||||
| NHW-NHB | 1.4±1.2 – 0.9±0.9 | .47* | 0.3±1.1 – 0.5±1.2 | −.17 | 1.7±1.6 – 1.5±1.5 | .13 | |
| NHW-Hisp/Latino | 1.4±1.2 – 1.5±1.2 | −.08 | 0.3±1.1 – 0.4±1.4 | −.08 | 1.7±1.6 – 2.0±1.6 | −.18 | |
| NHB-Hisp/Latino | 0.9±0.9 – 1.5±1.2 | −.56* | 0.5±1.2 – 0.4±1.4 | .07 | 1.5±1.5 – 2.0±1.6 | −.32† | |
| Mobility | |||||||
| NHW-NHB | 1.2±0.9 – 0.9±0.8 | .35† | 0.3±1.0 – 0.4±1.1 | −.09 | 1.5±1.3 – 1.2±1.3 | .23* | |
| NHW-Hisp/Latino | 1.2±0.9 – 1.2±0.9 | 0 | 0.3±1.0 – 0.3±1.0 | 0 | 1.5±1.3 – 1.5±1.3 | 0 | |
| NHB-Hisp/Latino | 0.9±0.8 – 1.2±0.9 | −.35† | 0.4±1.1 – 0.9±1.0 | .09 | 1.2±1.3 – 1.5±1.3 | −.23† | |
| Paraplegia (n=1010) | |||||||
| Self-care | |||||||
| NHW-NHB | 2.6±1.1 – 2.4±1.0 | .19 | 0.7±1.1 – 0.6±1.3 | .08 | 3.3±1.2 – 3.0±1.3 | .24† | |
| NHW-Hisp/Latino | 2.6±1.1 – 2.8±1.0 | −.19 | 0.7±1.1 – 0.3±1.1 | .36† | 3.3±1.2 – 3.2±1.1 | .08 | |
| NHB-Hisp/Latino | 2.4±1.0 – 2.8±1.0 | −.39† | 0.6±1.3 – 0.3±1.1 | .25† | 3.0±1.3 – 3.2±1.1 | −.17 | |
| Mobility | |||||||
| NHW-NHB | 2.5±1.1 – 2.5±1.0 | 0 | 0.7±1.0 – 0.5±1.2 | .18 | 3.2±1.2 – 3.0±1.3 | .16 | |
| NHW-Hisp/Latino | 2.5±1.1 – 2.6±1.0 | −.09 | 0.7±1.0 – 0.4±1.0 | .30† | 3.2±1.2 – 3.1±1.2 | .08 | |
| NHB-Hisp/Latino | 2.5±1.1 – 2.5±1.0 | 0 | 0.5±1.2 – 0.4±1.0 | .09 | 3.0±1.3 – 3.1±1.2 | −.08 | |
NOTE. Values are mean ± SD or as otherwise indicated.
Abbreviations: Hisp, Hispanic; NHB, non-Hispanic black; NHW, non-Hispanic white.
Medium effect size: 0.4–0.59.
Small to medium effect size: 0.2–0.39.
Fig. 2.
Unadjusted mean change in FIM self-care and mobility scores by race and ethnicity among SCI patients with tetraplegia. Abbreviations: NHB, non-Hispanic black; NHW, non-Hispanic white.
Fig. 3.
Unadjusted mean change in FIM self-care and mobility scores by race and ethnicity among SCI patients with paraplegia. Abbreviations: NHB, non-Hispanic black; NHW, non-Hispanic white.
In tables 3 and 4, we reported the regression coefficients, stratified by neurologic category, for race and ethnicity associated with the change in FIM self-care and mobility scores during rehabilitation and at 1-year follow-up, adjusting for sociodemographic and injury characteristics. Non-Hispanic black participants with tetraplegia had significantly smaller gains in self-care scores during rehabilitation in comparison to non-Hispanic white participants with tetraplegia (β=−.30; 95% confidence interval [CI], −.48 to −.11; P=.002). Hispanics with tetraplegia had significantly more improvement in self-care change scores (β=.30; 95% CI, .07–.52; P=.01) relative to non-Hispanic whites during rehabilitation. At 1-year follow-up, no racial or ethnic differences in self-care change scores were observed. However, smaller gains in mobility scores were observed for non-Hispanic black participants (β=−.19; 95% CI, −.35 to −.03; P=.02) with tetraplegia during rehabilitation in comparison to non-Hispanic whites. Among Hispanics with tetraplegia, no significant difference in mobility scores was observed in comparison to non-Hispanic whites during rehabilitation and at 1-year follow-up.
Table 3.
Association between race/ethnicity and change in FIM self-care and mobility scores at discharge and 1-year after rehabilitation among persons with tetraplegia (N=756)
| Race/Ethnicity | Self-Care
|
Mobility
|
||
|---|---|---|---|---|
| Discharge | 1-Year Follow-Up | Discharge | 1-Year Follow-Up | |
| Non-Hispanic white | Reference | Reference | Reference | Reference |
| Non-Hispanic black | .30 (−.48 to −.11) P=.002 |
.23 (−.01 to .46) P=.06 |
−.19 (−.35 to −.03) P=.02 |
.07 (−.13 to .28) P=.47 |
| Hispanic | .30 (.07 to .52) P=.01 |
−.02 (−.30 to .26) P=.87 |
.11 (−.08 to .30) P=.27 |
−.10 (−.34 to .15) P=.45 |
NOTE. Values are β (95% CI) or as otherwise indicated. β is an unstandardized coefficient. Adjusted for admission FIM self-care or mobility scores, age at injury, injury etiology, neurologic level at discharge, sex, marital status, education level, and preinjury employment status.
Table 4.
Association between race/ethnicity and change in FIM self-care and mobility scores at discharge and 1-year after rehabilitation among persons with paraplegia (N=1010)
| Race/Ethnicity | Self-Care
|
Mobility
|
||
|---|---|---|---|---|
| Discharge | 1-Year Follow-Up | Discharge | 1-Year Follow-Up | |
| Non-Hispanic white | Reference | Reference | Reference | Reference |
| Non-Hispanic black | −.27 (−.46 to −.08) P=.005 |
.02 (−.19 to .22) P=.86 |
−.21 (−.40 to −.03) P=.02 |
.01 (−.18 to .20) P=.91 |
| Hispanic | .21 (−.01 to .44) P=.06 |
−.33 (−.58 to −.08) P=.009 |
.02 (−.20 to .24) P=.84 |
−.18 (−.42 to .05) P=.12 |
NOTE. Values are β (95% CI) or as otherwise indicated. β is an unstandardized coefficient. Adjusted for admission FIM self-care or mobility scores, age at injury, injury etiology, neurologic level at discharge, sex, marital status, education level, and preinjury employment status.
Among participants with paraplegia (see table 4), the change in FIM self-care scores was significantly different across race and ethnic groups at discharge. Non-Hispanic black participants with paraplegia had significantly smaller self-care gains than non-Hispanic whites during rehabilitation (β=−.27; 95% CI, −.46 to −.08; P=.005). At 1-year follow-up, Hispanic participants with paraplegia demonstrated significantly smaller gains in self-care scores relative to non-Hispanic white participants (β=−.33; 95% CI, −.58 to −.08; P=.009). The mean change in FIM mobility scores at 1-year follow-up was not significantly different across racial or ethnic groups with paraplegia.
Discussion
This study examined the effect of race and ethnicity on self-care and mobility outcomes at discharge and 1-year follow-up among patients with motor complete SCI. Small, significant differences in functional improvements were observed across racial and ethnic groups at discharge. There were no differences observed at 1-year follow-up.
When demographic and injury covariates were taken into account, non-Hispanic black participants with tetraplegia and paraplegia achieved significantly smaller gains in FIM self-care and mobility scores during inpatient rehabilitation in comparison to non-Hispanic white and Hispanic participants. Based on the estimates obtained from this analysis, on average, participants with paraplegia were admitted to rehabilitation with self-care scores of 3.0 (ie, needing moderate assistance) on the 1 to 7 FIM scale. The average gains made over the course of rehabilitation differed by race and ethnicity. Non-Hispanic whites and Hispanics in this sample gained 3.8 and 4.0 FIM units, respectively (adjusting for the covariates), which means that by discharge, the average person with paraplegia of non-Hispanic white or Hispanic descent had an FIM self-care score of 7 and was completely independent in self-care. In comparison, the non-Hispanic blacks gained an average of approximately 3.5 units, which translates to requiring minimal assistance at discharge. Although this is a relatively small difference, this discrepancy implies that non-Hispanic black persons with paraplegia may require more assistance (with devices) in comparison to their non-Hispanic white and Hispanic peers. This places further challenges on persons of non-Hispanic black background in addition to the physical, social, and emotional challenges of SCI, as the need for assistive devices requires resources and advocacy on the part of patients and their families at a time of significant readjustment to life with a disability.
Although not statistically significant, previous studies30,32 using the SCIMS database also observed lower FIM scores at discharge among non-Hispanic black patients with SCI relative to non-Hispanic white patients with SCI. Poorer functional outcomes observed at discharge among non-Hispanic black individuals with tetraplegia and paraplegia may be attributed cultural factors or to reduced access to economic and supportive resources during inpatient rehabilitation. For example, Myaskovsky et al12 found that non-Hispanic black individuals with SCI reported more experiences of discrimination in health care, greater perceived racism, more health care system distrust, and lower health literacy than did non-Hispanic whites.
A key feature of the current study is the ability to elucidate important functional outcome differences between Hispanic patients with SCI and non-Hispanic white and black patients with SCI.4,5,53–55 Hispanics with tetraplegia and paraplegia demonstrated significantly higher self-care and mobility scores at discharge relative to non-Hispanic whites and non-Hispanic blacks. These findings are consistent with the “Hispanic paradox” cited in public health research, which has documented better health outcomes among Hispanics despite being socioeconomically disadvantaged.56,57 Better self-care outcomes at discharge among Hispanic patients with tetraplegia may be related to cultural factors, such as a substantial amount of family involvement and social support during inpatient rehabilitation observed in other SCI studies.43
Consistent with previous studies, our findings show similar mean FIM self-care and mobility scores at 1-year follow-up across racial and ethnic groups.33 Hispanic participants with paraplegia achieved significantly smaller gains in FIM self-care scores at 1-year follow-up in comparison to non-Hispanic whites, which may be due to a “ceiling effect” in their functional gains obtained during inpatient rehabilitation, limited access to assistive devices, lack of transfer of knowledge from inpatient rehabilitation to home environment, and limited access to outpatient therapies or practice of self-care activities.58
The methodological strengths of this study include adjustment for sociodemographic and injury characteristics, using self-care and mobility subscales of the FIM rather than the total FIM score, and stratification of participants with SCI into 3 racial and ethnic groups to compare mean differences and changes in FIM self-care and mobility scores at discharge and 1-year follow-up. Based on the manner in which we operationalized our key outcome variables (ie, change in FIM scores), the best possible comparison study was conducted by Granger et al.59 This study benchmarked functional outcomes using a sample of patients with traumatic SCI from the Uniform Data System Medical Rehabilitation database. The current study’s FIM scores were similar to admission, discharge, and change in FIM scores at discharge reported in Granger’s national sample. The methodological strengths of our study and consistency with prior research give us greater confidence in the accuracy to detect meaningful differences in self-care and mobility outcomes while accounting for the injury complexities across racial and ethnic groups with SCI.
Study limitations
Despite these strengths, the study is limited by the continuity of rehabilitation centers included in the grant cycles of the SCIMS, which could vary the proportion of racial and ethnic groups included in the sample. We attempted to minimize the variability of rehabilitation facilities by focusing on 2 grant cycles that consistently funded 11 SCIMS centers. During 2000 to 2011, trends in health policy and changes in clinical practice could have influenced these results. During this sampling time frame, socioeconomic indicators (eg, health insurance, income) were not assessed in the SCIMS database, making it difficult to ascertain the potential confounding role these socioeconomic factors could contribute to the findings. Although administrative data quality of the SCIMS is highly monitored, admission and discharge FIM scores are gathered by rehabilitation clinical staff, while the follow-up FIM is administered by trained SCIMS interview staff and self-reported by participants, which may also limit the findings. The lack of specificity to the needs of SCI is often demonstrated in the ceiling and floor effects in FIM motor scores.60–62 Since the SCIMS is a database of grantees from the National Institute on Disability and Rehabilitation Research that is not a nationally representative sample of the SCI population across the country, nor are the data weighted, the generalizability of results is limited. Further, the study compared racial and ethnic group changes in FIM scores rather than individual change in FIM trajectories (eg, based on each spinal segment), which could limit findings. While we compared patients with SCI within each stratification group at the lowest level of lesion at discharge, we did not account for potential changes in the American Spinal Injury Association Impairment Scale classification at 1-year follow-up, which could impact functional outcomes. Another potential source of bias may be due to demographic and SCI injury differences observed in the missing and excluded cases, which may have included more disadvantaged and functionally impaired persons than the cases retained for analysis.
Conclusions
Overall, the study suggests that differential patterns of self-care and mobility outcomes among patients with motor complete SCI may emerge across racial and ethnic groups at discharge from inpatient rehabilitation. These differences were not evident at 1-year follow-up. Additional research is needed to confirm these results and determine the underlying mechanisms through which these variations in self-care and mobility outcomes occur across racial and ethnic groups and are associated with successful transition, functional independence, and quality of life in SCI.
Acknowledgments
Supported by the National Institute of Child Health and Human Development (grant no. R24 HD065702); National Institute on Disability and Rehabilitation Research (grant no. H133N110020); the National Institute of Arthritis and Musculoskeletal and Skin Diseases (grant no. U01AR057929-03S1); and the Kessler Foundation.
We thank Rachel Byrne, MA, and Tiara Brown, BA, for their assistance with references, data collection, and preparation.
List of abbreviations
- CI
confidence interval
- SCI
spinal cord injury
- SCIMS
Spinal Cord Injury Model Systems
Footnotes
IBM Corp, 1 New Orchard Rd, Armonk, NY 10504-1722.
Presented in part to the Center for Large Rehabilitation Research Using Large Datasets, October 24–25, 2013, Houston, TX.
Disclosures: none.
References
- 1.Noreau L, Fougeyrollas P, Post M, Asano M. Participation after spinal cord injury: the evolution of conceptualization and measurement. J Neurol Phys Ther. 2005;29:147–56. doi: 10.1097/01.npt.0000282247.15911.dc. [DOI] [PubMed] [Google Scholar]
- 2.Post M, Noreau L. Quality of life after spinal cord injury. J Neurol Phys Ther. 2005;29:139–46. doi: 10.1097/01.npt.0000282246.08288.67. [DOI] [PubMed] [Google Scholar]
- 3.Dijkers MP. Quality of life of individuals with spinal cord injury: a review of conceptualization, measurement, and research findings. J Rehabil Res Dev. 2005;42:87–110. doi: 10.1682/jrrd.2004.08.0100. [DOI] [PubMed] [Google Scholar]
- 4.Devivo MJ. Epidemiology of traumatic spinal cord injury: trends and future implications. Spinal Cord. 2012;50:365–72. doi: 10.1038/sc.2011.178. [DOI] [PubMed] [Google Scholar]
- 5.DeVivo MJ, Chen Y. Trends in new injuries, prevalent cases, and aging with spinal cord injury. Arch Phys Med Rehabil. 2011;92:332–8. doi: 10.1016/j.apmr.2010.08.031. [DOI] [PubMed] [Google Scholar]
- 6.National Spinal Cord Injury Statistical Center. Spinal cord injury facts and figures at a glance. Birmingham: Univ of Alabama at Birmingham; 2013. [Google Scholar]
- 7.Lad SP, Umeano OA, Karikari IO, et al. Racial disparities in outcomes after spinal cord injury. J Neurotrauma. 2013;30:492–7. doi: 10.1089/neu.2012.2540. [DOI] [PubMed] [Google Scholar]
- 8.Saladin LK, Krause JS. Pressure ulcer prevalence and barriers to treatment after spinal cord injury: comparisons of four groups based on race-ethnicity. NeuroRehabilitation. 2009;24:57–66. doi: 10.3233/NRE-2009-0454. [DOI] [PubMed] [Google Scholar]
- 9.Cardenas DD, Bryce TN, Shem K, Richards JS, Elhefni H. Gender and minority differences in the pain experience of people with spinal cord injury. Arch Phys Med Rehabil. 2004;85:1774–81. doi: 10.1016/j.apmr.2004.04.027. [DOI] [PubMed] [Google Scholar]
- 10.Krause JS, Broderick LE, Broyles J, Saladin LK. Racial disparities in health outcomes after spinal cord injury: mediating effects of education and income. J Spinal Cord Med. 2006;29:17–25. doi: 10.1080/10790268.2006.11753852. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Krause JS, Saladin LK, Adkins RH. Disparities in subjective well-being, participation, and health after spinal cord injury: a 6-year longitudinal study. NeuroRehabilitation. 2009;24:47–56. doi: 10.3233/NRE-2009-0453. [DOI] [PubMed] [Google Scholar]
- 12.Myaskovsky L, Burkitt KH, Lichy AM, et al. The association of race, cultural factors, and health-related quality of life in persons with spinal cord injury. Arch Phys Med Rehabil. 2011;92:441–8. doi: 10.1016/j.apmr.2010.10.007. [DOI] [PubMed] [Google Scholar]
- 13.Hunt PC, Boninger ML, Cooper RA, Zafonte RD, Fitzgerald SG, Schmeler MR. Demographic and socioeconomic factors associated with disparity in wheelchair customizability among people with traumatic spinal cord injury. Arch Phys Med Rehabil. 2004;85:1859–64. doi: 10.1016/j.apmr.2004.07.347. [DOI] [PubMed] [Google Scholar]
- 14.Ambrosio F, Boninger ML, Fitzgerald SG, Hubbard SL, Schwid SR, Cooper RA. Comparison of mobility device delivery within Department of Veterans Affairs for individuals with multiple sclerosis versus spinal cord injury. J Rehabil Res Dev. 2007;44:693. doi: 10.1682/jrrd.2006.02.0016. [DOI] [PubMed] [Google Scholar]
- 15.Chen Y, Devivo MJ, Jackson AB. Pressure ulcer prevalence in people with spinal cord injury: age-period-duration effects. Arch Phys Med Rehabil. 2005;86:1208–13. doi: 10.1016/j.apmr.2004.12.023. [DOI] [PubMed] [Google Scholar]
- 16.Fuhrer MJ, Garber SL, Rintala DH, Clearman R, Hart KA. Pressure ulcers in community-resident persons with spinal cord injury: prevalence and risk factors. Arch Phys Med Rehabil. 1993;74:1172–7. [PubMed] [Google Scholar]
- 17.Kemp BJ, Krause JS. Depression and life satisfaction among people ageing with post-polio and spinal cord injury. Disabil Rehabil. 1999;21:241–9. doi: 10.1080/096382899297666. [DOI] [PubMed] [Google Scholar]
- 18.Krause JS, Kemp B, Coker J. Depression after spinal cord injury: relation to gender, ethnicity, aging, and socioeconomic indicators. Arch Phys Med Rehabil. 2000;81:1099–109. doi: 10.1053/apmr.2000.7167. [DOI] [PubMed] [Google Scholar]
- 19.Arango-Lasprilla JC, Ketchum JM, Francis K, et al. Race, ethnicity, and employment outcomes 1, 5, and 10 years after spinal cord injury: a longitudinal analysis. PM R. 2010;2:901–10. doi: 10.1016/j.pmrj.2010.05.009. [DOI] [PubMed] [Google Scholar]
- 20.Krause JS, Terza JV. Injury and demographic factors predictive of disparities in earnings after spinal cord injury. Arch Phys Med Rehabil. 2006;87:1318–26. doi: 10.1016/j.apmr.2006.07.254. [DOI] [PubMed] [Google Scholar]
- 21.Meade MA, Lewis A, Jackson MN, Hess DW. Race, employment, and spinal cord injury. Arch Phys Med Rehabil. 2004;85:1782–92. doi: 10.1016/j.apmr.2004.05.001. [DOI] [PubMed] [Google Scholar]
- 22.Gage B, Ingber MJ, Morley M, et al. [Accessed April 21, 2014];Post-acute care payment reform demonstration project: final report. 2012 Mar; Available at: http://www.cms.gov/Research-Statistics-Data-and-Systems/Statistics-Trends-and-Reports/Reports/Downloads/PAC-PRD_FinalRpt_Vol4of4.pdf.
- 23.Consortium for Spinal Cord Medicine. Outcomes following traumatic spinal cord injury: clinical practice guidelines for health-care professionals. Washington (DC): Paralyzed Veterans of America; 1999. [DOI] [PubMed] [Google Scholar]
- 24.Teeter L, Gassaway J, Taylor S, et al. Relationship of physical therapy inpatient rehabilitation interventions and patient characteristics to outcomes following spinal cord injury: the SCIRehab project. J Spinal Cord Med. 2012;35:503–26. doi: 10.1179/2045772312Y.0000000058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.van Langeveld SA, Post MW, van Asbeck FW, Postma K, Ten Dam D, Pons K. Development of a classification of physical, occupational, and sports therapy interventions to document mobility and self-care in spinal cord injury rehabilitation. J Neurol Phys Ther. 2008;32:2–7. doi: 10.1097/NPT.0b013e3181663533. [DOI] [PubMed] [Google Scholar]
- 26.Ozelie R, Gassaway J, Buchman E, et al. Relationship of occupational therapy inpatient rehabilitation interventions and patient characteristics to outcomes following spinal cord injury: the SCIR-ehab project. J Spinal Cord Med. 2012;35:527–46. doi: 10.1179/2045772312Y.0000000062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Coster WJ, Haley SM, Andres PL, Ludlow LH, Bond TL, Ni PS. Refining the conceptual basis for rehabilitation outcome measurement: personal care and instrumental activities domain. Med Care. 2004;42:I62–72. doi: 10.1097/01.mlr.0000103521.84103.21. [DOI] [PubMed] [Google Scholar]
- 28.Stineman MG, Jette A, Fiedler R, Granger C. Impairment-specific dimensions within the Functional Independence Measure. Arch Phys Med Rehabil. 1997;78:636–43. doi: 10.1016/s0003-9993(97)90430-5. [DOI] [PubMed] [Google Scholar]
- 29.Stineman MG, Shea JA, Jette A, et al. The Functional Independence Measure: tests of scaling assumptions, structure, and reliability across 20 diverse impairment categories. Arch Phys Med Rehabil. 1996;77:1101–8. doi: 10.1016/s0003-9993(96)90130-6. [DOI] [PubMed] [Google Scholar]
- 30.Burnett DM, Kolakowsky-Hayner SA, White JM, Cifu DX. Impact of minority status following traumatic spinal cord injury. NeuroRehabilitation. 2002;17:187–94. [PubMed] [Google Scholar]
- 31.Meade MA, Cifu DX, Seel RT, McKinley WO, Kreutzer JS. Medical procedures, complications, and outcomes for patients with spinal cord injury: a multicenter investigation comparing African Americans and whites. Arch Phys Med Rehabil. 2004;85:368–75. doi: 10.1016/j.apmr.2003.06.008. [DOI] [PubMed] [Google Scholar]
- 32.Putzke JD, Hicken BL, Richards JS. Race: predictor versus proxy variable? Outcomes after spinal cord injury. Arch Phys Med Rehabil. 2002;83:1603–11. doi: 10.1053/apmr.2002.35115. [DOI] [PubMed] [Google Scholar]
- 33.Johnston MV, Wood K, Millis S, Page S, Chen D. Perceived quality of care and outcomes following spinal cord injury: minority status in the context of multiple predictors. J Spinal Cord Med. 2004;27:241–51. doi: 10.1080/10790268.2004.11753755. [DOI] [PubMed] [Google Scholar]
- 34.Kirshblum S, Millis S, McKinley W, Tulsky D. Late neurologic recovery after traumatic spinal cord injury. Arch Phys Med Rehabil. 2004;85:1811–7. doi: 10.1016/j.apmr.2004.03.015. [DOI] [PubMed] [Google Scholar]
- 35.Kirshblum SC, O’Connor KC. Levels of spinal cord injury and predictors of neurologic recovery. Phys Med Rehabil Clin N Am. 2000;11:1–27. [PubMed] [Google Scholar]
- 36.Chen Y, Deutsch A, DeVivo MJ, et al. Current research outcomes from the Spinal Cord Injury Model Systems. Arch Phys Med Rehabil. 2011;92:329–31. doi: 10.1016/j.apmr.2010.12.011. [DOI] [PubMed] [Google Scholar]
- 37.DeVivo MJ, Vogel LC. Epidemiology of spinal cord injury in children and adolescents. J Spinal Cord Med. 2004;27(Suppl 1):S4–10. doi: 10.1080/10790268.2004.11753778. [DOI] [PubMed] [Google Scholar]
- 38.Jackson AB, Dijkers M, Devivo MJ, Poczatek RB. A demographic profile of new traumatic spinal cord injuries: change and stability over 30 years. Arch Phys Med Rehabil. 2004;85:1740–8. doi: 10.1016/j.apmr.2004.04.035. [DOI] [PubMed] [Google Scholar]
- 39.Consortium for Spinal Cord Medicine. Outcomes following traumatic spinal cord injury: clinical practice guidelines for health-care professionals. J Spinal Cord Med. 2000;23:289–316. doi: 10.1080/10790268.2000.11753539. [DOI] [PubMed] [Google Scholar]
- 40.Aito S Gruppo Italiano Studio Epidemiologico Mielolesioni GG. Complications during the acute phase of traumatic spinal cord lesions. Spinal Cord. 2003;41:629–35. doi: 10.1038/sj.sc.3101513. [DOI] [PubMed] [Google Scholar]
- 41.Marino RJ, Barros T, Biering-Sorensen F, et al. International standards for neurological classification of spinal cord injury. J Spinal Cord Med. 2003;26(Suppl 1):S50–6. doi: 10.1080/10790268.2003.11754575. [DOI] [PubMed] [Google Scholar]
- 42.van Hedel HJ, Curt A. Fighting for each segment: estimating the clinical value of cervical and thoracic segments in SCI. J Neurotrauma. 2006;23:1621–31. doi: 10.1089/neu.2006.23.1621. [DOI] [PubMed] [Google Scholar]
- 43.Arango-Lasprilla JC, Ketchum JM, Francis K, Premuda P, Stejskal T, Kreutzer J. Influence of race/ethnicity on divorce/separation 1, 2, and 5 years post spinal cord injury. Arch Phys Med Rehabil. 2009;90:1371–8. doi: 10.1016/j.apmr.2009.02.006. [DOI] [PubMed] [Google Scholar]
- 44.Krause JS, Saunders LL, DeVivo MJ. Income and risk of mortality after spinal cord injury. Arch Phys Med Rehabil. 2011;92:339–45. doi: 10.1016/j.apmr.2010.09.032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Krause JS, Saunders LL, Staten D, Rohe DE. Vocational interests after recent spinal cord injury: comparisons related to sex and race. Arch Phys Med Rehabil. 2011;92:626–31. doi: 10.1016/j.apmr.2010.11.026. [DOI] [PubMed] [Google Scholar]
- 46.Kay E, Deutsch A, Chen D, Semik P, Rowles D. Effects of gender on inpatient rehabilitation outcomes in the elderly with incomplete paraplegia from nontraumatic spinal cord injury. J Spinal Cord Med. 2010;33:379–86. doi: 10.1080/10790268.2010.11689716. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Kozlowski AJ, Heinemann AW. Using individual growth curve models to predict recovery and activities of daily living after spinal cord injury: an SCIRehab project study. Arch Phys Med Rehabil. 2013;94:S154–64. e1–4. doi: 10.1016/j.apmr.2012.11.050. [DOI] [PubMed] [Google Scholar]
- 48.Kazis LE, Anderson JJ, Meenan RF. Effect sizes for interpreting changes in health status. Med Care. 1989;27:S178–89. doi: 10.1097/00005650-198903001-00015. [DOI] [PubMed] [Google Scholar]
- 49.Fitzpatrick R, Davey C, Buxton MJ, Jones DR. Evaluating patient-based outcome measures for use in clinical trials. Health Technol Assess. 1998;2:i–iv. 1–74. [PubMed] [Google Scholar]
- 50.Cohen J. Statistical power analysis for the behavioral sciences. Hillsdale: Lawrence Erlbaum Associates; 1988. [Google Scholar]
- 51.Putzke JD, Richards JS, Devivo MJ. Gunshot versus nongunshot spinal cord injury: acute care and rehabilitation outcomes. Am J Phys Med Rehabil. 2001;80:366–70. doi: 10.1097/00002060-200105000-00008. [DOI] [PubMed] [Google Scholar]
- 52.Putzke JD, Richards JS, DeVivo MJ. Quality of life after spinal cord injury caused by gunshot. Arch Phys Med Rehabil. 2001;82:949–54. doi: 10.1053/apmr.2001.23973. [DOI] [PubMed] [Google Scholar]
- 53.Nelson AR. Unequal treatment: report of the Institute of Medicine on racial and ethnic disparities in healthcare. Ann Thorac Surg. 2003;76:S1377–81. doi: 10.1016/s0003-4975(03)01205-0. [DOI] [PubMed] [Google Scholar]
- 54.Department of Education. Final guidance on maintaining, collecting and reporting racial and ethnic data to the U.S. Department of Education. Federal Register. 2007:72. [Google Scholar]
- 55.Fyffe DC, Botticello AL, Myaskovsky L. Vulnerable groups living with spinal cord injury. Top Spinal Cord Inj Rehabil. 2011;17:1–9. doi: 10.1310/sci1702-01. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Franzini L, Ribble JC, Keddie AM. Understanding the Hispanic paradox. Ethn Dis. 2001;11:496–518. [PubMed] [Google Scholar]
- 57.Palloni A, Morenoff JD. Interpreting the paradoxical in the Hispanic paradox: demographic and epidemiologic approaches. Ann N Y Acad Sci. 2001;954:140–74. doi: 10.1111/j.1749-6632.2001.tb02751.x. [DOI] [PubMed] [Google Scholar]
- 58.Wirth B, van Hedel HJA, Kometer B, Dietz V, Curt A. Changes in activity after a complete spinal cord injury as measured by the Spinal Cord Independence Measure II (SCIM II) Neurorehabil Neural Repair. 2008;22:145–53. doi: 10.1177/1545968307306240. [DOI] [PubMed] [Google Scholar]
- 59.Granger CV, Karmarkar AM, Graham JE, et al. The Uniform Data System for Medical Rehabilitation: report of patients with traumatic spinal cord injury discharged from rehabilitation programs in 2002–2010. Am J Phys Med Rehabil. 2012;91:289–99. doi: 10.1097/PHM.0b013e31824ad2fd. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Anderson K, Aito S, Atkins M, et al. Functional recovery measures for spinal cord injury: an evidence-based review for clinical practice and research. J Spinal Cord Med. 2008;31:133–44. doi: 10.1080/10790268.2008.11760704. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Furlan JC, Noonan V, Singh A, Fehlings MG. Assessment of disability in patients with acute traumatic spinal cord injury: a systematic review of the literature. J Neurotrauma. 2011;28:1413–30. doi: 10.1089/neu.2009.1148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Hall KM, Cohen ME, Wright J, Call M, Werner P. Characteristics of the Functional Independence Measure in traumatic spinal cord injury. Arch Phys Med Rehabil. 1999;80:1471–6. doi: 10.1016/s0003-9993(99)90260-5. [DOI] [PubMed] [Google Scholar]