Abstract
Objective
Despite guidelines recommending cervical cancer screening intervals be extended beyond one year, clinical practice has been slow to change. Patient preferences are a potential barrier. In the Centers for Disease Control's Cervical Cancer (Cx3) Study at Federally Qualified Health Centers (FQHCs) across Illinois, we surveyed patients about screening practices, and assessed beliefs regarding lengthening screening intervals.
Method
We analyzed data from 984 low income women in the Cx3 Study (2009–2011). Participants completed a survey assessing health history, knowledge about Pap testing, beliefs and intentions about extending screening intervals, and demographics.
Results
The majority reported annual Pap testing (61%), while only 24% reported a 2–3 year screening interval (recommendation at time of survey). Misunderstandings about the Pap test were prevalent, with over half believing it screened for vaginal, yeast, and sexually transmitted infections (58%–72%). Unfavorable beliefs about extending screening intervals were common. The majority (57%) indicated that they would not wait 3 years to be screened if their physician recommended it, and intentions were associated with knowledge about Pap testing.
Conclusion
Most women reported annual cervical cancer screening, and intended to resist longer screening intervals. Patients' lack of knowledge and unfavorable beliefs may serve as barriers to extending screening intervals. Published by Elsevier Inc.
Keywords: Cervical cancer screening, Early detection of cancer, Patient acceptance of health care, Patient compliance, Healthcare disparities
Introduction
Current guidelines from U.S. professional medical organizations recommend that women who have a cervix and are at average risk of cervical cancer forego an annual Pap testing schedule in favor of extending the interval between routine screening tests. Specifically, the American College of Obstetricians and Gynecologists (ACOG), the United States Preventive Services Task Force (USPSTF), and the American Cancer Society (ACS) recommend that average risk women 30 to 65 years old be screened for cervical cancer via co-testing (i.e., Pap and HPV testing) every 5 years, or with Pap alone every 3 years (ACOG, 2012; Moyer, 2012; Saslow et al., 2012). The current guidelines updated those issued in 2002/2003, which recommended extending intervals to 2–3 years for women 30 years and older with 3 consecutive normal Pap test results (ACOG, 2003; USPSTF, 2003; Saslow et al., 2002). Despite the length of time passed since extended intervals were recommended and evidence supporting the safety of recommendations, clinical practice has been slow to change (Meissner et al., 2010; Roland et al., 2011; Saint et al., 2005; Saraiya et al., 2010; Sirovich and Welch, 2004; Yabroff et al., 2009). Five or more years after extended intervals were recommended, many medical providers continued to recommend annual screening (Benard et al., 2011; Meissner et al., 2010; Roland et al., 2011; Saraiya et al., 2010) and a recent survey of women confirmed the predominance of annual testing (Chen et al., 2012).
Patients' unfavorable attitudes about lengthening intervals have been recognized as a potential barrier to implementing current guidelines (MacLaughlin et al., 2011; Meissner et al., 2010; Sirovich and Welch, 2004; Sirovich et al., 2005). While some have found that patients are suspicious of motivations behind the guidelines (Sirovich et al., 2005), the wider variety of reasons behind patient resistance have not been fully explored.
As part of the Centers for Disease Control's Cervical Cancer (Cx3) Study, we surveyed a sample of women being screened for cervical cancer at Federally Qualified Health Centers (FQHC) on their knowledge about the Pap test, beliefs about extending screening intervals, and intentions to extend screening intervals.
Methods
Participants
Data were obtained from baseline surveys conducted October 2009 to May 2011 as part of Cx3, a study to identify barriers to appropriate cervical cancer screening practices and to implement an educational intervention to promote evidence-based screening practices. The study was conducted in 15 clinics associated with six FQHCs serving low income women in Illinois. FQHCs provide comprehensive primary health care services to medically underserved communities and vulnerable populations in high-need areas across the United States. A baseline survey was completed by a convenience sample of 984 women 30 to 60 years old who were undergoing a regular screening Pap test (i.e., no: abnormal Pap test in the last year, cervical cancer, HIV, hysterectomy, or other known risk factors). Eligible patients were identified through medical chart review by clinic staff and were invited to participate when they arrived at the clinic for their visit. No records were kept on those who refused participation; thus, we could not calculate a response rate. Women were offered a $5 cash incentive for participation. Baseline questionnaires were self-administered in the clinic waiting room prior to the woman's exam and were available in English and Spanish. They elicited information on demographic characteristics, cervical cancer screening history, risk factors, knowledge and beliefs about cervical cancer screening, and cost of health care services. The questionnaire was pilot tested with nine women at a FQHC clinic in Atlanta, Georgia. This study was approved by CDC's Institutional Review Board and informed consent was obtained from study participants.
Measures
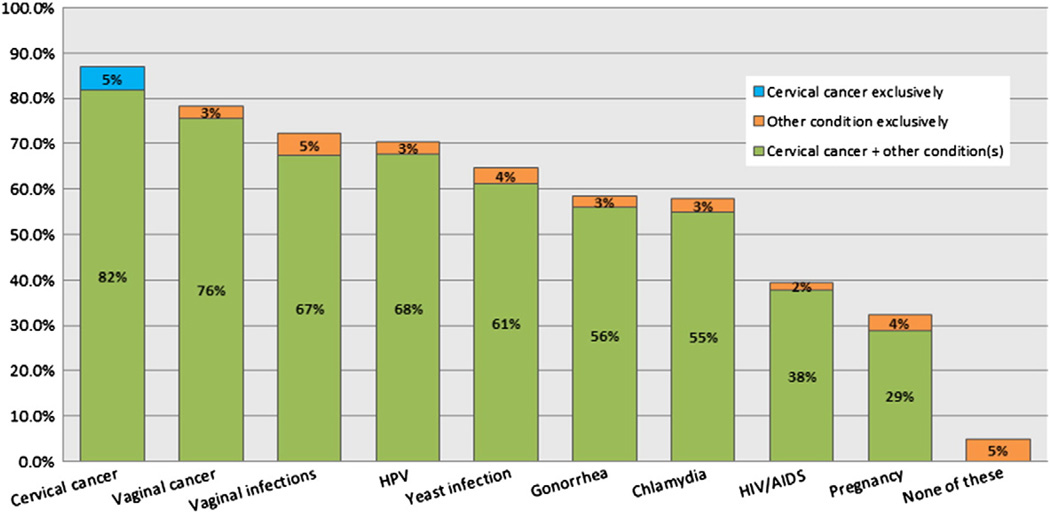
Knowledge about the purpose of the Pap test was assessed by questions modified from previously published research (Hawkins et al., 2011). Questions asked, “Do you agree or disagree that the Pap test is used to check for…” Nine conditions were listed with the following response options: “Agree,” “Disagree,” and “Not Sure” (see Fig. 1 for the conditions). Women (n = 26) who did not answer any of the nine items but answered other questions on the same and subsequent pages of the survey were categorized as answering “Not Sure” to all conditions. Those who did not answer any items nor adjacent questions (n = 22) were categorized as having missing responses.
Fig. 1.
Knowledge about the purpose of the Pap test in screening for cancer and othzer conditions (n = 962). (Study was conducted in 15 Federally Qualified Health Center clinics in Illinois, USA, 2009–2011.)
Knowledge about the purpose of the Pap test was summarized in two ways. First, as shown in Fig. 1, participants were categorized by believing the Pap test screens for: (a) cervical cancer exclusively, (b) other conditions exclusively, or (c) cervical cancer plus other conditions. Second, a score was created to represent participants' "general Pap understanding," which prioritized knowing that the Pap test screens for cervical cancer and ignored beliefs about the Pap test's link with two conditions: HPV and vaginal cancer. Beliefs about HPV and vaginal cancer were excluded from this score because of HPV's close connection with cervical cancer and because in rare circumstances it is clinically advisable to use a Pap test to detect vaginal cancer. Participants who did not check cervical cancer were categorized as having poor general Pap understanding. Participants who checked cervical cancer but also checked pregnancy, HIV, gonorrhea, chlamydia, yeast infections and/or vaginal infections were also categorized as having poor general Pap understanding. Participants who checked cervical cancer and no additional conditions (excluding HPV and vaginal cancer) were considered to have good general Pap understanding.
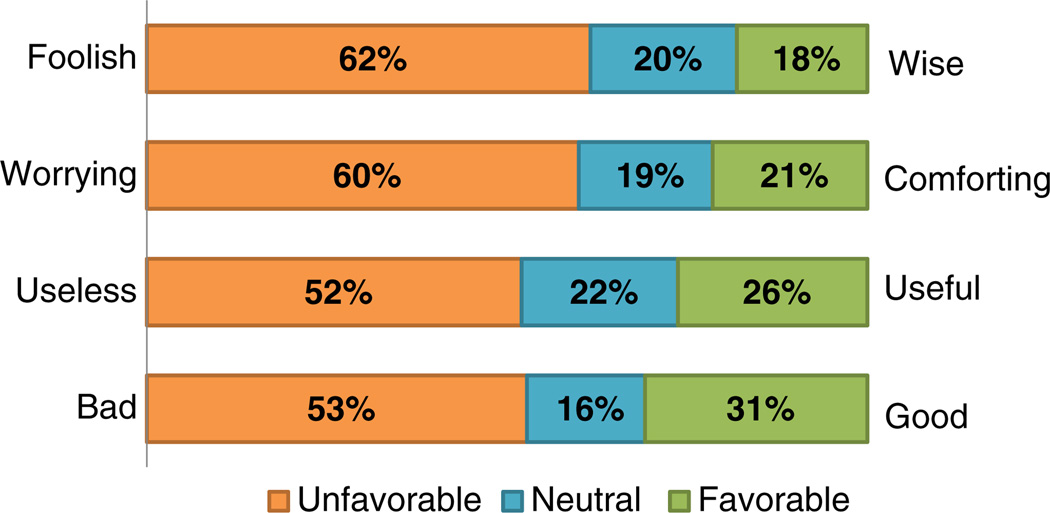
Seven items developed for this study elicited participants' beliefs about waiting three years between Pap tests. This series of questions began with the introductory language, “Waiting three years for my next Pap test …” and followed with seven beliefs (displayed in Fig. 2). The specific beliefs assessed by these items were based on previous research (e.g., Sirovich et al., 2005). Participants were instructed to indicate whether they agreed, disagreed or neither agreed nor disagreed with each statement.
Fig. 2.
Beliefs about waiting three years between Pap tests (n = 600–618). (Study was conducted in 15 Federally Qualified Health Center clinics in Illinois, USA, 2009–2011.)
Intention to wait three years between Pap tests was assessed by a question developed for this study: “If your health care provider recommends that you have your next Pap test in 3 years, how likely are you to wait that long?” Five response options from“Very unlikely” to “Very likely” with a “Neither”/“Not sure” midpoint were offered.
Statistical analysis
We present descriptive statistics for all measures. Analyses of beliefs and intentions to wait three years between Pap screenings were conducted on a subset of respondents (n = 663), as skip patterns in the survey necessitated excluding those who had never heard of HPV (n = 194) and who were above average risk for cervical cancer based on the following: they were told to return in less than a year based on their last Pap test results (n = 61); they had tested positive for HPV (n = 8); or, they had an abnormal Pap test result in the previous three years (n = 51).
Ordered logit regression was conducted to examine the association between general Pap understanding and intentions to follow a three-year screening interval (outcome variable). The ordered logit model assumes the proportionality of the odds-ratio. The proportionality assumption was tested with the Brant test; no violation was found (chi-square = 1.37 with d.f. = 3, p = .7412). Stata release 12.1 was used to fit the ordered logit models using maximum likelihood estimation. Estimation of standard errors accounted for the clinic-based clustered sampling design using the Stata survey (svyset) option. The significance level was set as two-sided p = 0.05.
Results
Demographic characteristics for the whole sample and subsample are presented in Table 1. Study participants were females between the ages of 30 and 60 (mean 45 years; standard deviation [SD] 7.5), 32% Hispanic, 39% non-Hispanic white, and 26% non-Hispanic black. Educational attainment was varied, with 32% not having completed a high school diploma, 23% with a high school diploma, and 45% having attempted or completed degrees in higher education. Only 21% held private insurance while 45% had no insurance, and 40% had public or another type of coverage (percentages add to >100% because respondents could check more than one category of insurance).
Table 1.
Participant demographic characteristics, pap testing history, and gynecologic health history. Full study sample and subsample included in analyses of beliefs and intentions to wait 3 years. (Study was conducted in 15 Federally Qualified Health Center clinics in Illinois, USA, 2009–2011.)
| Full study sample N = 984 |
Subsample N = 663a |
|||
|---|---|---|---|---|
| N | % | N | % | |
| Age | ||||
| Age at baseline, years (Mean ± SD) | 45.0 ± 7.5 | 45.1± 7.6 | ||
| Race — ethnicity | ||||
| Hispanic | 312 | 32 | 200 | 30 |
| Non-Hispanic White | 384 | 39 | 278 | 42 |
| Non-Hispanic Black, African American | 254 | 26 | 162 | 25 |
| Non-Hispanic other/multiple races | 26 | 3 | 17 | 3 |
| Marital status | ||||
| Never married | 176 | 18 | 121 | 18 |
| Unmarried, living with partner | 80 | 8 | 56 | 9 |
| Married | 430 | 44 | 286 | 44 |
| Separated/divorced | 250 | 26 | 169 | 26 |
| Widowed | 37 | 4 | 25 | 4 |
| Highest level of schooling completed | ||||
| <High school diploma | 300 | 32 | 189 | 29 |
| High school diploma or GED | 217 | 23 | 133 | 21 |
| Some college or AA | 296 | 31 | 215 | 34 |
| Bachelor's degree or higher | 133 | 14 | 104 | 16 |
| Type of insurance coverage (respondent could check all that apply) | ||||
| Private insurance | 200 | 21 | 151 | 24 |
| Medicare | 89 | 10 | 65 | 10 |
| Medicaid/medical coupons | 159 | 17 | 105 | 16 |
| Military or veterans administration | 5 | 1 | 3 | <1 |
| Illinois BCCP | 87 | 9 | 56 | 9 |
| No insurance | 416 | 45 | 276 | 43 |
| Other insurance | 30 | 3 | 20 | 3 |
| Current employment status | ||||
| Employed or self-employed full- or part-time | 472 | 54 | 329 | 55 |
| Unemployed | 182 | 21 | 124 | 21 |
| Unable to work | 60 | 7 | 39 | 7 |
| Homemaker | 152 | 17 | 99 | 17 |
| Student/retired | 11 | 1 | 6 | 1 |
| Pap test history | ||||
| How many Pap tests in lifetime? | ||||
| Never | 6 | 1 | 3 | <1 |
| 1 time | 14 | 2 | 6 | 1 |
| 2–4 times | 125 | 13 | 81 | 13 |
| 5–10 times | 279 | 29 | 187 | 29 |
| >10 times | 527 | 55 | 370 | 57 |
| How often get Pap tests? | ||||
| More often than once a year | 22 | 2 | 8 | 1 |
| Once a year | 561 | 61 | 387 | 62 |
| Once every 2–3 years | 223 | 24 | 156 | 25 |
| Less often than once every 3 years | 114 | 12 | 74 | 12 |
| Today is first | 6 | 1 | 3 | <1 |
| After last Pap test, when told to return for next one? | ||||
| As soon as possible | 19 | 2 | 0 | 0 |
| 6 months | 55 | 6 | 0 | 0 |
| 1 year | 600 | 66 | 442 | 71 |
| 2 years | 82 | 9 | 63 | 10 |
| 3 years | 14 | 2 | 12 | 2 |
| No one said/not sure | 145 | 16 | 102 | 16 |
| Abnormal Pap test results, everb | ||||
| Yes | 266 | 28 | 145 | 23 |
| No | 639 | 69 | 466 | 74 |
| Not sure | 29 | 3 | 18 | 3 |
| Gynecologic health history | ||||
| HPV infection, everc | ||||
| Yes | 47 | 5 | 26 | 4 |
| No | 825 | 92 | 566 | 92 |
| Not sure | 23 | 3 | 20 | 3 |
| Sexually transmitted infection(s), ever | ||||
| Yes | 198 | 21 | 128 | 20 |
| No | 714 | 77 | 487 | 77 |
| Not sure | 22 | 2 | 14 | 2 |
| Genital warts, ever | ||||
| Yes | 82 | 9 | 57 | 9 |
| No | 848 | 90 | 572 | 90 |
| Not sure | 14 | 1 | 8 | 1 |
The subsample used in analyses of beliefs and intention to wait three years between Pap screenings excluded women who had never heard of HPV (as necessitated by a skip pattern) or who were considered above average risk for cervical cancer.
Respondents who were having their first Pap test were recoded as never having an abnormal Pap result.
Respondents who had never heard of HPV were recoded as never having been diagnosed with an HPV infection.
As Table 1 shows, the majority reported receiving annual Pap tests (61%) and were advised to return annually (66%) after their last Pap test. While 28% reported ever having an abnormal Pap test result, the average time since most recent abnormal test was 9.8 (SD 7.8) years (not in table).
When asked about conditions for which the Pap test checks, respondents selected “agree” to a mean of 5.6 (SD 2.9) conditions out of nine. As Fig. 1 shows, cervical cancer was most commonly selected (87%). Only 5% indicated that cervical cancer was the only condition detected by the Pap, while 82% believed the Pap test screened for cervical cancer in conjunction with one or more conditions on the list. Over half believed that the Pap test screened for chlamydia (58%), gonorrhea (59%), yeast infections (65%), HPV virus (71%), vaginal infections (72%) and vaginal cancer (79%). A sizable minority believed that it checked for HIV/AIDS (40%) and pregnancy (33%).
Categorizing participants by their “general Pap understanding” using the definition above, revealed that 15% had a good general understanding of the Pap test's purpose (i.e., knew it checked for cervical cancer and did not believe it checked for chlamydia, gonorrhea, yeast or vaginal infections), while 85% had a poor general understanding. Of those with a poor general understanding, 15% did not recognize that it checked for cervical cancer while 85% knew that it checked for cervical cancer but also believed it checked for one or more of the other conditions (data not shown).
Beliefs about lengthening screening intervals to 3 years can be seen in Fig. 2. The majority believed longer intervals would cause them to worry about getting cancer (68%), and half (50%) believed they would increase their chances of getting cancer. While 38% agreed with the statement that waiting 3 years “is something your doctor thinks you should do,” 34% disagreed. Just over one third (36%) believed that waiting 3 years would prevent them from getting other needed health care, and one-third or fewer agreed that waiting longer between Pap tests would save time (33%), money (31%), or give peace of mind (30%).
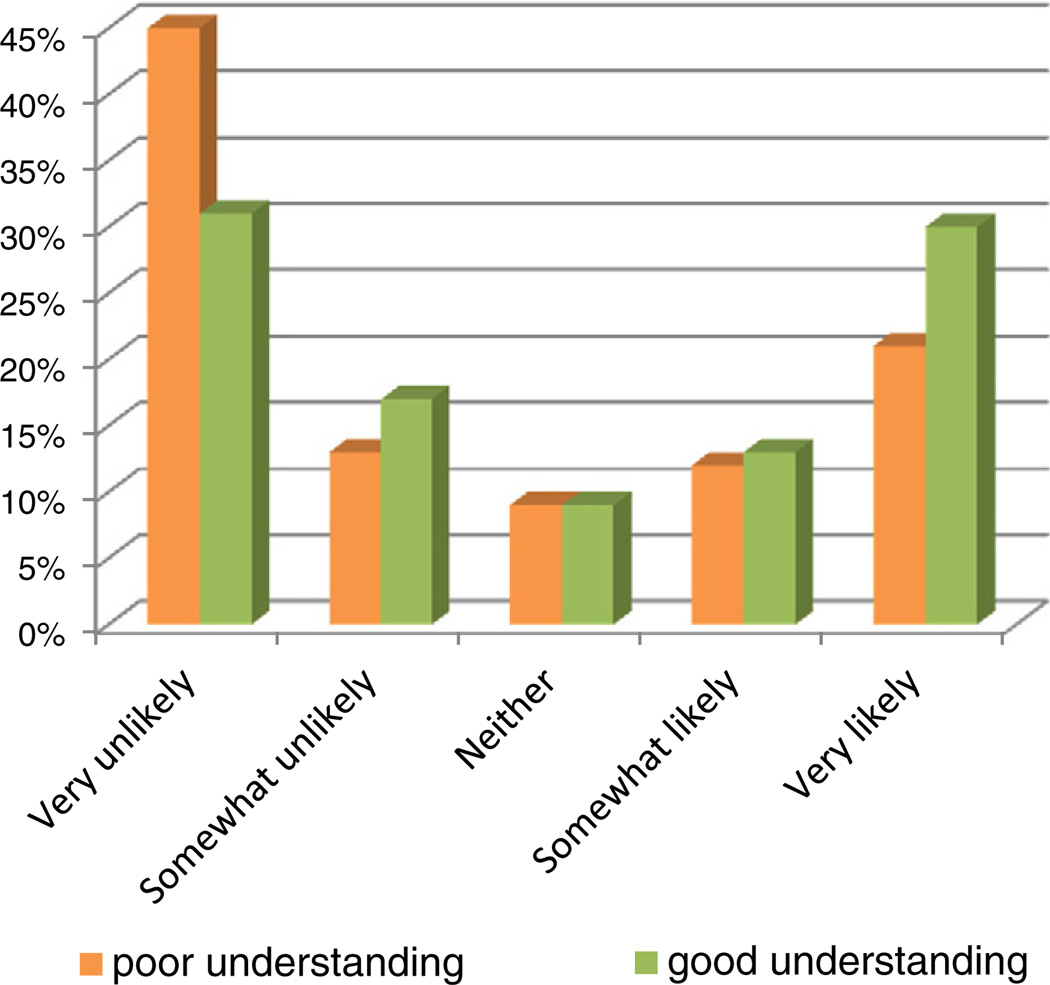
When asked how likely they would be to follow a health care provider's recommendation to wait 3 years until their next Pap test, 22% said “very likely,” 13% said “somewhat likely,” 8% said “neither unlikely nor likely/not sure,” 14% said “somewhat unlikely,” and 43% said “very unlikely” (data not shown).
Fig. 3 shows intentions to wait 3 years between Pap tests by general Pap understanding. Of women with poor general understanding, 45% reported that they were very unlikely to wait 3 years compared to 31% of women with a good general understanding. When tested with ordinal regression, women with a good general understanding of the Pap test were more likely to report a more favorable intention to wait 3 years for their next Pap test than women with poor understanding (O.R. = 1.66, 95% confidence interval 1.11–2.51).
Fig. 3.
Intentions to wait three years before the next Pap test by general understanding of the Pap test's purpose (n = 608). (Study was conducted in 15 Federally Qualified Health Center clinics in Illinois, USA, 2009–2011.)
Discussion
In this sample of low-income women at Federally Qualified Health Centers across Illinois, annual Pap testing was the norm and very few reported screening intervals consistent with newer recommendations for women at average risk of cervical cancer. Only 11% reported previously receiving guidance from their providers to return for a routine Pap test in two or three years, as had been the recommendation in place for over five years. This finding is similar to other recent accounts (Meissner et al., 2010; Roland et al., 2011; Saraiya et al., 2010) and suggests that over-screening persists, even among the under- and un-insured.
Given that the majority reported being told after their last Pap test to return for their next test in 1 year, perhaps it is not surprising that over half said they would be unlikely to wait 3 years between Pap tests if their physician recommended it. Physician recommendation is an important influence on patient behavior and the recommendation actually received by most of the women in our study had been to undergo annual Pap testing. Without widespread change in the intervals physicians recommend to their patients, significant change in Pap testing practices will be unlikely. For this reason, multi-pronged approaches to educate both providers and patients about evidence-based guidelines for screening and to encourage guideline-consistent practices at the provider level are essential.
In our search for patient-related barriers to recommended screening practices, we looked to knowledge, beliefs and intentions regarding Pap testing and found that many women displayed poor understanding of the purpose of the Pap test. While the vast majority recognized that Pap tests are used to screen for cervical cancer, substantial proportions also believed that they are used to check for many other conditions, including pregnancy, HIV/AIDS, and chlamydia. These findings are consistent with previous work showing misconceptions about Pap testing among the general population (Hawkins et al., 2011), and suggest that patient education is needed to improve understanding of this widely used screening test. Misunderstandings about the purpose of Pap tests could indicate inadequate patient–provider communication about this test and about the bundling of tests that sometimes occurs with the Pap test. For example, providers may choose to test for sexually transmitted infections at the same time they administer a Pap test. If patients are not told that multiple tests are being conducted from the sample taken at the time of the Pap test, any subsequent diagnoses may be misunderstood by the patient to have been detected by the Pap test, thus leading to misunderstandings about the purpose of the Pap test.
We found that misunderstandings could also present a barrier to extending Pap test screening intervals. While over half of the women said they would be unlikely to follow a doctor's recommendation to wait 3 years between Pap tests, intentions were associated with the general understanding about the Pap test's purpose. Women with the poorest understanding were significantly more likely than those with better understanding to indicate that they would not wait 3 years between tests. Although we did not directly ask women why they would not favor interval extension, it is possible that the more conditions a woman believes are revealed by a Pap test, the more essential she may believe the test to be in terms of gauging overall gynecological health. Thus, women who believe the Pap test screens only for cervical cancer may be more comfortable with waiting longer between tests than women who believe the Pap test screens for multiple gynecological cancers, sexually transmitted infections, and pregnancy. As efforts are made to encourage guideline-consistent cervical cancer screening practices, it may be useful to develop educational materials that present information about the safety of less frequent screening, while explaining the purpose of Pap testing as it differs from other types of testing that may or may not be offered in conjunction with it.
We identified a number of beliefs that may serve as barriers to extending Pap testing intervals. Among the most common was that waiting longer between tests would put women at higher risk of cervical cancer, and increase worry about getting cervical cancer. Beliefs of this nature indicate a need for patient education on the rationale behind extending the screening interval beyond one year. Educational efforts should explain the potential harms involved in screening more often than clinically advised (Moyer, 2012) and directly address the common misconception that the decision to extend screening intervals is primarily financially driven (Sirovich et al., 2005). The majority of women in our study did not believe waiting longer between Pap tests would present benefits such as saving time, cost, and promoting peace of mind. Interestingly, only a minority of women believed waiting longer between tests would prevent them from getting other needed healthcare, a concern that is commonly expressed by medical care providers (Roland et al., 2013).
Study limitations
Despite the strengths of this study in examining the knowledge, beliefs and intentions of medically underserved patients, several limitations should be noted. We did not include questions on all aspects of medical history (i.e., high-grade precancerous cervical lesions, in utero exposure to diethylstilbestrol, immunocompromised health status), which are known to contribute to cervical cancer risk and may indicate the need for more frequent screening. Instead, we relied upon clinic staff to review medical records in determining initial eligibility and specified that the study include only women seeking routine cervical screening. We excluded women who reported recent abnormal Pap tests, positive HPV test results and other screening-related problems.
Another limitation given the nature of the study methodology (i.e., self-administered survey) is that it was not possible to fully explore women's understanding of the Pap test. Response bias could have led women to answer affirmatively to the conditions presented, and inflate the number of conditions believed to be associated with the Pap test.
Conclusions
In summary, our findings suggest widespread misunderstandings among medically underserved women about the purpose of the Pap test and shed light on potential barriers to guideline-consistent screening behavior. As the Cx3 Study continues, it will be possible to determine whether efforts to educate both women and medical care providers on cervical cancer screening will result in changes to attitudes and actual screening behavior.
Footnotes
Funding: Centers for Disease Control & Prevention, Contract 200-2002-00573, Task Order No. 0006.
Disclaimers: This manuscript was written in the course of employment by the United States Government and it is not subject to copyright in the United States. The findings and conclusions in this report are those of the authors and do not necessarily represent the official position of the Centers for Disease Control and Prevention.
Conflict of interest statement
There are no conflicts of interest reported by any of the authors.
References
- ACOG Committee on Practice Bulletins-Gynecology. ACOG practice bulletin no. 131: screening for cervical caner. Obstet. Gynecol. 2012;120:1222–1238. doi: 10.1097/aog.0b013e318277c92a. [DOI] [PubMed] [Google Scholar]
- American College of Obstetricians and Gynecologists. ACOG practice bulletin no. 45: cervical cytology screening. Int. J. Gynaecol. Obstet. 2003;83:237–247. doi: 10.1016/s0020-7292(03)00412-0. [DOI] [PubMed] [Google Scholar]
- Benard VB, Saraiya MS, Soman A, Roland KB, Yabroff KR, Miller J. Cancer screening practices among physicians in the National Breast and Cervical Cancer Early Detection Program. J. Womens Health (Larchmt) 2011;20:1479–1484. doi: 10.1089/jwh.2010.2530. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen HY, Kessler CL, Mori N, Chauhan SP. Cervical cancer screening in the United States, 1993–2010: characteristics of women who are never screened. J. Womens Health (Larchmt) 2012;21:1132–1138. doi: 10.1089/jwh.2011.3418. [DOI] [PubMed] [Google Scholar]
- Hawkins NA, Cooper CP, Saraiya M, Gelb CA, Polonec L. Why the Pap test? Awareness and use of the Pap test among women in the United States. J. Womens Health (Larchmt) 2011;20:511–515. doi: 10.1089/jwh.2011.2730. [DOI] [PubMed] [Google Scholar]
- MacLaughlin KL, Angstman KB, Flynn PM, Schmitt JR, Weaver AL, Shuster LT. Predictors of patient comfort and adherence with less frequent cervical cancer screening. Qual. Prim. Care. 2011;19:355–363. [PubMed] [Google Scholar]
- Meissner HI, Tiro JA, Yabroff KR, Haggstrom DA, Coughlin SS. Too much of a good thing? Physician practices and patient willingness for less frequent pap test screening intervals. Med. Care. 2010;48:249–259. doi: 10.1097/MLR.0b013e3181ca4015. [DOI] [PubMed] [Google Scholar]
- Moyer VA. Screening for cervical cancer: U.S. Preventive Services Task Force recommendation statement. Ann. Intern. Med. 2012;156:880–891. doi: 10.7326/0003-4819-156-12-201206190-00424. [DOI] [PubMed] [Google Scholar]
- Roland KB, Soman A, Benard VB, Saraiya M. Human papillomavirus and Papanicolaou tests screening interval recommendations in the United States. Am. J. Obstet. Gynecol. 2011;205(447):e1–e8. doi: 10.1016/j.ajog.2011.06.001. [DOI] [PubMed] [Google Scholar]
- Roland KB, Benard VB, Greek A, Hawkins NA, Manninen D, Saraiya M. Primary care provider practices and beliefs related to cervical cancer screening with the HPV test in Federally Qualified Health Centers. Prev. Med. 2013 doi: 10.1016/j.ypmed.2013.04.012. http://dx.doi.org/10.1016/j.ypmed.2013.04.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Saint M, Gildengorin G, Sawaya GF. Current cervical neoplasia screening practices of obstetrician/gynecologists in the US. Am. J. Obstet. Gynecol. 2005;192:414–421. doi: 10.1016/j.ajog.2004.09.026. [DOI] [PubMed] [Google Scholar]
- Saraiya M, Berkowitz Z, Yabroff KR, Wideroff L, Kobrin S, Benard V. Cervical cancer screening with both human papillomavirus and Papanicolaou testing vs Papanicolaou testing alone: what screening intervals are physicians recommending? Arch. Intern. Med. 2010;170:977–985. doi: 10.1001/archinternmed.2010.134. [DOI] [PubMed] [Google Scholar]
- Saslow D, Runowicz CD, Solomon D, Moscick AB, Smith RA, Eyre HJ, Cohen C. American Cancer Society guideline for the early detection of cervical neoplasia and cancer. CA Cancer J Clin. 2002;52:342–362. doi: 10.3322/canjclin.52.6.342. [DOI] [PubMed] [Google Scholar]
- Saslow D, Solomon D, Lawson HW, Killackey M, Kulasingam SL, Cain JM, Garcia FA, Moriarty AT, Waxman AG, et al. American Cancer Society, American Society for Colposcopy and Cervical Pathology, and American Society for Clinical Pathology screening guidelines for the prevention and early detection of cervical cancer. Am. J. Clin. Pathol. 2012;137:516–542. doi: 10.1309/AJCPTGD94EVRSJCG. [DOI] [PubMed] [Google Scholar]
- Sirovich BE, Welch HG. The frequency of Pap smear screening in the United States. J. Gen. Intern. Med. 2004;19:243–250. doi: 10.1111/j.1525-1497.2004.21107.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sirovich BE, Woloshin S, Schwartz LM. Screening for cervical cancer: will women accept less? Am. J. Med. 2005;118:151–158. doi: 10.1016/j.amjmed.2004.08.021. [DOI] [PubMed] [Google Scholar]
- USPSTF. Screening for Cervical Cancer. 2003 Available at: http://www.uspreventiveservicetaskforce.org/3rduspstf/cervcan/cervcanrr.pdf. [Google Scholar]
- Yabroff KR, Saraiya M, Meissner HI, Haggstrom DA, Wideroff L, Yuan G, Berkowitz Z, Davis WW, Benard VB, et al. Specialty differences in primary care physician reports of Papanicolaou test screening practices: a national survey, 2006 to 2007. Ann. Intern. Med. 2009;151:602–611. doi: 10.7326/0003-4819-151-9-200911030-00005. [DOI] [PubMed] [Google Scholar]