Abstract
Purpose
In adult Chinese men, smoking prevalence is high, but little is known about its association with chronic respiratory disease, which is still poorly diagnosed and managed.
Methods
A nationwide study recruited 0.5 million men and women aged 30–79 years during 2004–2008 from ten geographically diverse areas across the Mainland China. Information was collected from each participant regarding smoking and self-reported physician diagnosis of chronic bronchitis/emphysema (CB/E), along with measurement of lung function indices. Logistic regression was used to yield sex-specific odds ratios (ORs) relating smoking to airflow obstruction (AFO), defined as forced expiratory volume in 1 second (FEV1)/forced vital capacity (FVC) <0.7 and CB/E, adjusting for age, areas, education, and income.
Results
Overall 74% of men were ever regular smokers; among them, 7.2% had AFO compared with 5.4% in never-smokers, yielding an OR of 1.42 (95% confidence interval [CI]: 1.34–1.50). The risk was strongly associated with amount smoked and starting to smoke at a younger age. Among ex-smokers, the OR was more extreme for those who had quit due to illness (OR: 1.86, 95% CI: 1.77–1.96) than those who had quit by choice (OR:1.08, 95% CI: 1.01–1.16). CB/E prevalence was also significantly elevated in ex-smokers who had quit because of ill health (OR:2.79, 95% CI: 2.64–2.95), but not in regular smokers (OR:1.04, 95% CI: 0.96–1.11). Female smokers was rare (3%), but carried an excess risk for AFO (OR:1.53, 95% CI: 1.43–1.65) and, to a lesser extent, for CB/E (OR:1.28, 95% CI: 1.15–1.42).
Conclusion
In Mainland China, adult smokers, particularly ex-smokers who had quit because of illness, had significantly higher prevalence of chronic respiratory disease. AFO appeared to be more strongly associated with smoking than self-reported chronic respiratory disease.
Keywords: China Kadoorie Biobank, smoking cessation, airflow obstruction, chronic respiratory diseases, Mainland China
Introduction
Chronic obstructive pulmonary disease (COPD) is characterized by persistent airflow limitation that is usually progressive and often accompanied by a range of comorbidities.1 The burden of the disease is particularly high in some low- and middle-income countries, including the Mainland China where it was the third leading cause of years of life lost in 2010.2 Despite this high burden of COPD, it is still poorly diagnosed and managed in the Mainland China, particularly in some rural areas.3
Tobacco smoking is the primary cause of COPD.1 Several large prospective studies have reported that tobacco-attributed mortality is currently much lower in the Mainland China than in Western countries with, for example, relative risk for respiratory mortality in the Mainland China being more than tenfold lower compared to Western countries (<2 versus >20).4–10 These differences may reflect the older age of initiation and lower smoking intensity in Chinese smokers compared to their Western counterparts,7–9 and/or potential high background rates of disease in never-smokers.7 However, previous prospective studies of smoking in the Mainland China have generally involved relatively small numbers of COPD cases, particularly in women where only a low proportion smoked.9,10 Moreover, most of these studies in the Mainland China have failed to find any beneficial effect of voluntary smoking cessation on COPD risk.9–13 This could be attributed to smokers in the Mainland China not quitting until they are critically ill, but no large studies have specifically investigated the associations of recent changes in the amount smoked or the reason for quitting in relation to COPD risk.
Given the known large geographical variation in background rate of COPD across the Mainland China, studies involving multiple and diverse localities will be more informative than those conducted only in a single region. To our knowledge, there has only been one large multicenter study of COPD prevalence in the Mainland China, but that study did not consider associations with smoking in any detail.13 We report data from an even larger and more detailed study – the China Kadoorie Biobank (CKB) – that includes spirometric data, self-reported physician-diagnosed chronic bronchitis/emphysema (CB/E), and smoking habits in over 0.5 million men and women from ten diverse regions of the Mainland China.14–17 The main objectives of the study were 1) to describe cross-sectional associations of tobacco smoking with prevalent spirometrically-defined airway flow obstruction (AFO) in men and women separately; and 2) to investigate the associations of AFO with specific smoking habits, particularly smoking cessation, and in specific strata of the population. In addition, similar analyses were also done for self-reported physician-diagnosed CB/E.
Methods
Baseline survey
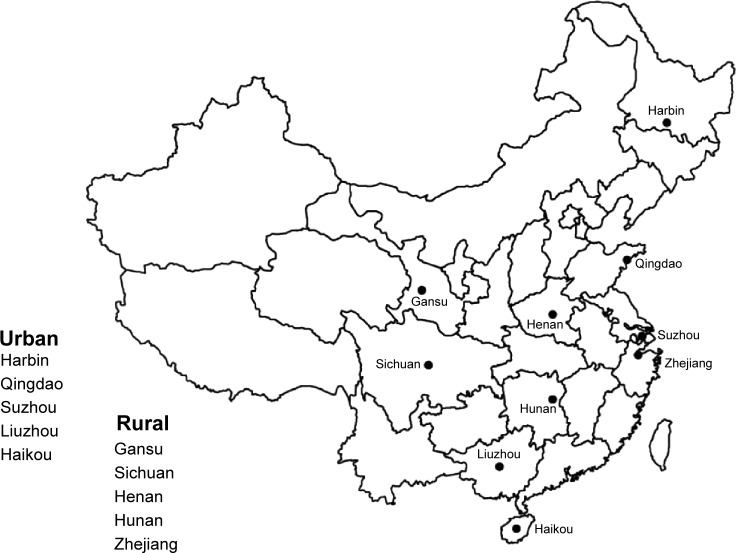
The detailed CKB design and procedures have been described previously.18 The baseline survey took place during 2004–2008 in ten geographically defined diverse localities (Figure 1) chosen to include a range of incidence of major chronic diseases (including COPD) and of behavioral and environmental risk factors.19 In each area, temporary assessment clinics were set up, and all nondisabled residents aged 35–74 years were invited to participate and ~30% responded. Overall, a total of 512,891 adults were recruited including a few slightly outside the target 35–74 age range group. All participants provided written informed consent and local, national, and international ethical approvals were obtained.
Figure 1.
Locations of the ten China Kadoorie Biobank survey sites across Mainland China.
At the study assessment clinics, trained health workers administered laptop-based questionnaires on sociodemographic factors, smoking, alcohol drinking, diet, physical activities, and medical history; measured each participant’s lung function, exhaled carbon monoxide, and blood pressure; and also collected blood for long-term storage.15
Smoking history
Participants were asked about their current and past smoking habits. For the present study, never-smokers were defined as those who had not smoked more than 100 cigarettes during their lifetime. Ever regular smokers were defined as those who had smoked one cigarette or equivalent daily for at least 6 months. Those who had never smoked regularly but had smoked ≥100 cigarettes in their lifetime were classified as occasional smokers. Regular smokers who had quit completely for at least 6 months at baseline were classified as ex-smokers.
For ever regular smokers, additional information was also collected, including age started to smoke regularly, amount and types of tobacco smoked when last smoking, depth of inhalation, and recent changes in amount smoked, and for ex-smokers the main reason for quitting (ill health, concerns about effect on future health, money worries, pressure from family, and other unspecified reasons) was recorded. The amount of tobacco smoked (g/day) by each smoker was calculated, assuming 1 g of tobacco per factory cigarette and 2 g per cigar, with quantities smoked in pipes and hand-rolled cigarettes given as liang/month (1 liang equivalent to 50 g) by the respondents. To help validate smoking exposure, exhaled carbon monoxide (CO) was measured in all participants, using the MicroCO meter (CareFusion Corp, San Diego, CA, USA).20
Spirometry and COPD
Forced expiratory volume in 1 second (FEV1) and forced vital capacity (FVC) were measured using a hand held Micro (MS01) Spirometer (CareFusion Corp) by trained technicians following recommended procedures.21 Participants made some practice blows, then the results of two successful blows were recorded. Participants were classified to their AFO status using modified Global Initiative for Chronic Obstructive Lung Disease (GOLD) spirometric criteria (prebronchodilator FEV1/FVC <0.7).1 The presence of AFO includes both asthma and COPD, as no bronchodilator was used, although the self-reported physician-diagnosed prevalence of asthma in the CKB participants was extremely low (~0.5%). During the survey, participants were also asked if they had ever had a diagnosis of CB/E (ie, COPD) by a physician.
Of the 512,891 (210,259 men, 302,632 women) participants enrolled, 396 (202 men, 194 women) with a recorded FEV1/FVC >1 were excluded, leaving 210,057 men and 302,438 women for the main analyses. The highest FEV1 and FVC values, not necessarily always from the same blow, were used in the analyses.22
Statistical analysis
Given the large difference in smoking prevalence, all analyses were conducted separately for men and women. The prevalence of AFO and CB/E was calculated for the different categories of smoking, directly standardized to the age group structure (30–39 years, 40–44 years, 45–49 years, 50–54 years, 55–59 years, 60–64 years, 65–69 years, and 70–79 years) and region structure of the male or female population.
Logistic regression was used to estimate the odds ratios (OR) of AFO or CB/E associated with smoking, adjusting for the 5-year age group, region, annual household income (<5, 5–9, 10–19, 20–34, ≥35 thousand yuan/year), highest education level (no formal, primary, secondary, tertiary), and the region by age group interaction. For variables with more than two groups, the ORs and their 95% confidence intervals (CI) were floated so that comparisons could be made between any chosen groups rather than just with the baseline category.23 Heterogeneity or trends of ORs between different smoking categories were assessed with chi-square tests.
Effect modification was assessed by logistic regression analysis within subgroups of urban/rural region, baseline age, and category of household income. All analyses used SAS 9.3 (SAS Institute Inc., Cary, NC, USA).
Results
Smoking prevalence differed considerably between men and women. In men, 74.3% were ever regular smokers compared to only 3.2% in women. In both sexes, smokers were less well educated and had a lower household income (Table 1). Compared with female regular smokers, male smokers had, on average, started smoking ~5 years earlier (22.5 years versus 27.1 years, for men and women, respectively), smoked twice as much (18.3 g versus 9.6 g tobacco/day, respectively) and were more likely to inhale to the lung (35.9% versus 25.3%, respectively) (Tables 2 and 3).
Table 1.
Baseline characteristics of the study participants by smoking category
| Variable* | Men (n=210,057)
|
Women (n=302,438)
|
||||
|---|---|---|---|---|---|---|
| Never | Occasional | All regular | Never | Occasional | All regular | |
| All (N) | 30,282 | 23,610 | 156,165 | 287,117 | 5,522 | 9,799 |
| Study area | ||||||
| Urban | 55.5 | 44.4 | 40.9 | 44.8 | 38.6 | 39.4 |
| Rural | 44.5 | 55.6 | 59.1 | 55.2 | 61.4 | 60.6 |
| Age at baseline (years) | 54.4±11.9 | 51.1±11.1 | 52.8±10.6 | 51.1±10.4 | 53.1±10.9 | 60.1±9.9 |
| 30–39 | 15.2 | 19.9 | 13.0 | 16.4 | 13.3 | 3.6 |
| 40–49 | 23.2 | 29.7 | 28.9 | 31.5 | 28.3 | 13.4 |
| 50–59 | 25.8 | 26.9 | 31.7 | 31.2 | 29.3 | 27.3 |
| 60–69 | 23.8 | 16.8 | 19.3 | 15.8 | 21.3 | 38.5 |
| 70–79 | 12.1 | 6.7 | 7.1 | 5.1 | 7.8 | 17.2 |
| Annual household income (yuan; in thousands) | ||||||
| <5 | 8.4 | 8.6 | 9.5 | 9.4 | 20.2 | 25.6 |
| 5–9 | 14.9 | 16.6 | 17.2 | 19.4 | 23.4 | 25.0 |
| 10–19 | 28.4 | 28.9 | 28.2 | 29.6 | 29.6 | 28.8 |
| 20–34 | 26.7 | 24.6 | 25.3 | 24.7 | 16.8 | 13.4 |
| ≥35 | 21.6 | 21.2 | 19.8 | 16.9 | 10.1 | 7.3 |
| Highest education completed | ||||||
| No formal school | 7.3 | 5.8 | 9.6 | 25.0 | 21.2 | 34.9 |
| Primary school | 26.6 | 28.0 | 35.5 | 31.0 | 35.3 | 41.1 |
| Middle/high school | 50.0 | 54.4 | 49.2 | 39.4 | 38.6 | 22.6 |
| College/university | 16.1 | 11.8 | 5.7 | 4.5 | 4.9 | 1.4 |
| Standing height (m) | 1.65±0.07 | 1.65±0.06 | 1.65±0.06 | 1.54±0.06 | 1.53±0.07 | 1.52±0.06 |
| FEV1 (L) | 2.61±0.68 | 2.77±0.66 | 2.65±0.70 | 2.00±0.48 | 1.92±0.57 | 1.64±0.54 |
| FVC (L) | 3.06±0.75 | 3.27±0.74 | 3.16±0.77 | 2.36±0.54 | 2.31±0.60 | 2.03±0.57 |
| FEV1/FVC (%) | 85.5±8.9 | 84.6±8.1 | 83.6±9.3 | 85.0±7.8 | 82.7±9.1 | 80.2±10.2 |
Note:
Data are % or mean ± SD.
Abbreviations: n, number; N, total number; FEV1, forced expiratory volume in 1 second; FVC, forced vital capacity; SD, standard deviation.
Table 2.
Associations of smoking with prevalent AFO and self-reported chronic bronchitis/emphysema among men
| Smoking habit (%) | AFO
|
Bronchitis/emphysema
|
|||
|---|---|---|---|---|---|
| %‡ | OR (95% CI)† | %‡ | OR (95% CI)† | ||
| Smoking category | |||||
| Never | 14.4 | 5.4 | 1.00 (0.95–1.06) | 3.3 | 1.00 (0.94–1.07) |
| Occasional | 11.2 | 5.2 | 0.93 (0.88–1.00) | 3.1 | 0.98 (0.90–1.06) |
| Exregular | 13.3 | 7.4 | 1.50 (1.44–1.57) | 5.6 | 1.85 (1.77–1.95) |
| Current regular | 61.1 | 7.1 | 1.37 (1.34–1.41) | 2.5 | 0.77 (0.74–0.80) |
| P heterogeneity | <0.0001 | <0.0001 | |||
| All regular | 74.4 | 7.2 | 1.42 (1.34–1.50) | 3.1 | 1.04 (0.96–1.11) |
| Amount smoked (g tobacco/day) in regular smokers | |||||
| Mean (SD), 18.3 (10.8) | |||||
| <5 | 6.1 | 6.6 | 1.34 (1.24–1.44) | 3.3 | 0.99 (0.87–1.11) |
| 5–14 | 28.9 | 6.9 | 1.36 (1.31–1.41) | 2.9 | 0.95 (0.90–1.01) |
| 15–24 | 46.2 | 7.4 | 1.46 (1.42–1.51) | 3.2 | 1.03 (0.99–1.08) |
| 25–34 | 10.4 | 7.6 | 1.47 (1.39–1.56) | 3.4 | 1.11 (1.02–1.21) |
| ≥35 | 8.4 | 7.4 | 1.42 (1.32–1.52) | 4.3 | 1.32 (1.21–1.45) |
| P trend | 0.014 | <0.0001 | |||
| Age started to smoke regularly (years) in regular smokers | |||||
| Mean (SD), 22.5 (7.0) | |||||
| ≥28 | 6.3 | 5.9 | 1.15 (1.10–1.21) | 4.2 | 0.76 (0.70–0.81) |
| 24–27 | 27.7 | 6.5 | 1.27 (1.21–1.34) | 3.7 | 0.92 (0.85–0.99) |
| 20–23 | 32.9 | 7.4 | 1.48 (1.43–1.54) | 3.4 | 1.12 (1.07–1.18) |
| 16–19 | 16.1 | 8.1 | 1.60 (1.54–1.67) | 2.8 | 1.24 (1.17–1.31) |
| <16 | 16.9 | 9.6 | 1.79 (1.68–1.92) | 2.4 | 1.35 (1.22–1.49) |
| P trend | <0.0001 | <0.0001 | |||
| Depth of inhalation in regular smokers | |||||
| Mouth/throat | 51.8 | 7.0 | 1.35 (1.31–1.39) | 2.9 | 0.94 (0.90–0.98) |
| Lung now | 12.3 | 6.4 | 1.27 (1.19–1.35) | 3.2 | 1.06 (0.97–1.15) |
| Lung always | 35.9 | 7.7 | 1.58 (1.52–1.64) | 3.6 | 1.19 (1.13–1.25) |
| P trend | <0.0001 | <0.0001 | |||
| Recent changes in amount smoked in current regular smokers§ | |||||
| No change | 66.5 | 6.8 | 1.28 (1.24–1.32) | 2.1 | 0.62 (0.59–0.65) |
| Increased a lot | 15.3 | 6.9 | 1.33 (1.25–1.42) | 2.4 | 0.72 (0.64–0.80) |
| Decreased a lot | 12.7 | 9.0 | 1.77 (1.68–1.87) | 4.3 | 1.20 (1.10–1.30) |
| P heterogeneity | <0.0001 | <0.0001 | |||
| Reason for stopping smoking in exregular smokers | |||||
| Ill health | 49.6 | 8.8 | 1.86 (1.77–1.96) | 8.4 | 2.79 (2.64–2.95) |
| Other reason | 50.4 | 5.6 | 1.08 (1.01–1.16) | 2.7 | 0.90 (0.81–0.99) |
| P heterogeneity | <0.0001 | <0.0001 | |||
Notes:
Adjusted for region, 5-year age group, age group × region interaction, education, and income, with the never-smoker category as the reference group. With the exception of the comparison of all regular versus never-smokers, the CIs are floated, so that comparisons can be made between any pair of categories.
Prevalences of disease are directly standardized to the age and area structure of the study’s male population.
The variable was missing in 5.4% of male current smokers (N=6,963 men).
Abbreviations: AFO, airflow obstruction; OR, odds ratio; CI, confidence interval; SD, standard deviation; N, total number.
Table 3.
Associations of smoking with prevalent AFO and self-reported chronic bronchitis/emphysema among women
| Smoking habit (%) | AFO
|
Bronchitis/emphysema
|
|||
|---|---|---|---|---|---|
| %‡ | OR (95% CI)† | %‡ | OR (95% CI)† | ||
| Smoking category | |||||
| Never | 94.9 | 4.3 | 1.00 (0.96–1.04) | 2.2 | 1.00 (0.95–1.05) |
| Occasional | 1.8 | 4.4 | 1.11 (1.00–1.22) | 1.9 | 0.99 (0.84–1.15) |
| Exregular | 0.9 | 5.0 | 1.67 (1.50–1.86) | 4.0 | 2.31 (2.02–2.63) |
| Current regular | 2.4 | 6.5 | 1.46 (1.36–1.57) | 2.0 | 0.87 (0.77–0.99) |
| P heterogeneity | <0.0001 | <0.0001 | |||
| All regular | 3.3 | 6.4 | 1.53 (1.43–1.65) | 2.4 | 1.28 (1.15–1.42) |
| Amount smoked (g tobacco/day) in regular smokers | |||||
| Mean (SD), 9.6 (7.5) | |||||
| <5 | 27.4 | 6.3 | 1.38 (1.23–1.55) | 2.2 | 1.14 (0.96–1.36) |
| 5–14 | 48.9 | 5.6 | 1.64 (1.51–1.79) | 2.6 | 1.32 (1.16–1.50) |
| 15–24 | 20.5 | 7.1 | 1.48 (1.30–1.69) | 2.3 | 1.37 (1.13–1.67) |
| 25–34 | 2.0 | 9.2 | 1.58 (1.07–2.34) | 2.3 | 1.49 (0.84–2.63) |
| ≥35 | 1.2 | 9.8 | 1.79 (1.03–3.10) | 5.9 | 1.10 (0.44–2.70) |
| P trend | 0.269 | 0.1966 | |||
| Age started to smoke regularly (years) in regular smokers | |||||
| Mean (SD), 27.1 (11.9) | |||||
| ≥28 | 11.3 | 5.5 | 1.36 (1.23–1.52) | 1.4 | 1.00 (0.85–1.18) |
| 24–27 | 18.5 | 6.7 | 1.57 (1.33–1.86) | 2.5 | 1.27 (0.98–1.66) |
| 20–23 | 16.8 | 7.6 | 1.69 (1.47–1.93) | 3.8 | 1.56 (1.28–1.90) |
| 16–19 | 12.2 | 7.9 | 1.50 (1.32–1.70) | 3.1 | 1.52 (1.26–1.84) |
| <16 | 41.1 | 9.4 | 1.82 (1.56–2.11) | 1.9 | 1.45 (1.15–1.84) |
| P trend | 0.0063 | 0.0005 | |||
| Depth of inhalation in regular smokers | |||||
| Mouth/throat | 62.0 | 6.4 | 1.49 (1.39–1.61) | 2.2 | 1.14 (1.02–1.29) |
| Lung now | 12.6 | 7.0 | 1.68 (1.41–1.99) | 2.2 | 1.28 (0.99–1.66) |
| Lung always | 25.3 | 6.9 | 1.58 (1.39–1.78) | 3.4 | 1.65 (1.40–1.95) |
| P trend | 0.3214 | 0.0004 | |||
| Recent changes in amount smoked in current regular smokers§ | |||||
| No change | 62.5 | 6.3 | 1.37 (1.25–1.51) | 1.8 | 0.69 (0.58–0.83) |
| Increased a lot | 16.7 | 8.2 | 1.55 (1.30–1.86) | 3.4 | 1.04 (0.77–1.41) |
| Decreased a lot | 14.1 | 11.0 | 1.90 (1.61–2.24) | 2.9 | 1.26 (0.96–1.65) |
| P heterogeneity | 0.0056 | 0.0003 | |||
| Reason for stopping smoking in ex regular smokers | |||||
| Ill health | 54.6 | 6.5 | 2.03 (1.78–2.31) | 9.3 | 3.24 (2.78–3.78) |
| Other reason | 45.4 | 5.2 | 1.20 (0.99–1.45) | 2.0 | 1.22 (0.95–1.58) |
| P heterogeneity | <0.0001 | <0.0001 | |||
Notes:
Adjusted for region, 5-year age group, age group × region interaction, education, and income, with the never-smoker category as the reference group. With the exception of the comparison of all regular versus never-smokers, CIs are floated, so that comparisons can be made between any pair of categories.
Prevalences of disease are directly standardized to the age and area structure of the study female population.
The variable was missing in 6.8% of female current smokers (N=485 women).
Abbreviations: AFO, airflow obstruction; OR, odds ratio; CI, confidence interval; SD, standard deviation; N, total number.
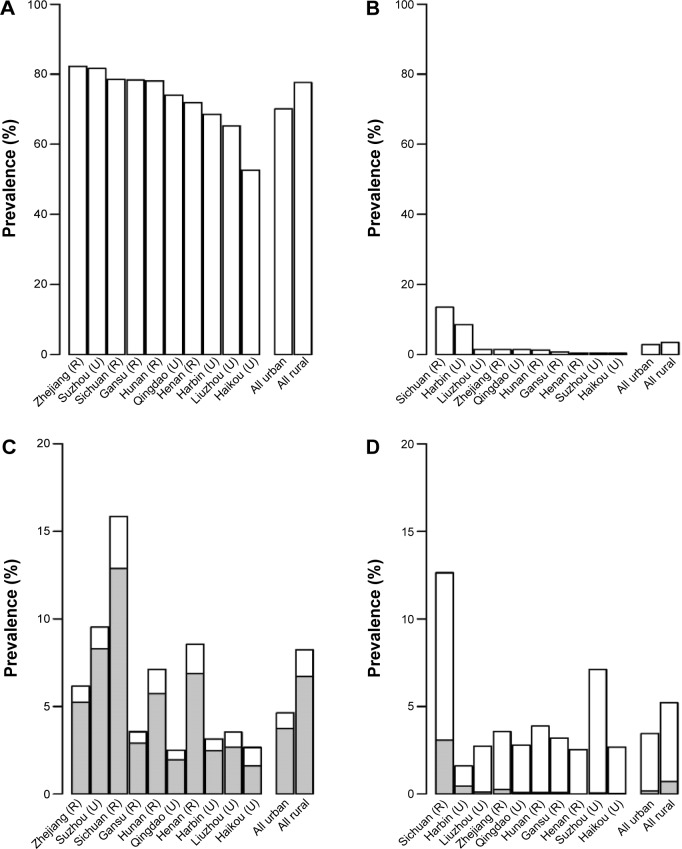
The overall prevalence of AFO was 6.7% (number [n]=14,024) in men and 4.4% (n=13,387) in women, and varied considerably across ten areas, with the crude prevalence ranging from 2.5%–15.9% in men and 1.4%–13.1% in women (Figure 2). The prevalence of CB/E was about half that of AFO in both men (3.1%; n=6,538) and women (2.2%; n=6,741). Only 15% of the men and 12% of the women with AFO also had a diagnosis of CB/E, whereas 33% of men and 23% of women with CB/E also had AFO. Regular smokers had a higher prevalence of AFO (Tables 2 and 3). In men, 7.2% of regular smokers had AFO versus 5.4% in never-smokers, yielding an adjusted OR of 1.42 (95% CI: 1.34–1.50). Similarly, in women, these were 6.4% versus 4.3%, yielding an adjusted OR of 1.53 (95% CI: 1.43–1.65). In both sexes, the OR was more extreme in those who started to smoke at a younger age (P-trend <0.0001 in men and 0.0063 in women). The association with the amount smoked was positive but weak in men and statistically significant in women. CB/E was not associated with regular smoking in men (OR: 1.04; 95% CI: 0.96–1.11), but there was a weak positive association in women (OR: 1.28; 95% CI: 1.15–1.42) (Tables 2 and 3).
Figure 2.
Prevalence of smoking and airflow obstruction in regular smokers in the ten areas.
Notes: (A and B) Prevalence of regular smoking in men and women, respectively. (C and D) Prevalence of airflow obstruction in men and women, respectively. The percentage of each shaded bar represents the percent of airflow obstruction cases in that region for smokers. Bars for all plots are order by the regional prevalence of regular smoking in men or women.
Abbreviations: R, rural; U, urban.
At baseline, 17.9% of male regular smokers and 26.9% of female regular smokers were ex-smokers, with about half reporting that they had quit because of ill health. Compared with current smokers, ex-smokers were older in both men (57.8 years versus 51.7 years for ex-smokers and current smokers, respectively) and women (63.4 versus 58.9 years, respectively), and overall ORs of AFO were only slightly elevated in ex-smokers (Tables 2 and 3). However, among those who had quit because of ill health, the ORs were considerably elevated in both men (OR: 1.86; 95% CI: 1.77–1.96) and women (OR: 2.03; 95% CI: 1.78–2.31). Similar findings were also seen for CB/E (men, OR: 2.79, 95% CI: 2.64–2.95; women, OR: 3.24; 95% CI: 2.78–3.78). There was little or no excess risk of either AFO or CB/E among those who had quit by choice, but regular smokers who had recently decreased the amount of smoking had comparable excess risk to those who quit because of ill health: in men the OR for AFO was 1.77 (95% CI: 1.68–1.87) and in women it was 1.90 (95% CI: 1.61–2.24). For CB/E, similar findings were also evident, though to a lesser extent (Tables 2 and 3).
Although AFO prevalence in never-smokers was lower in urban than in rural areas, the association of AFO with regular smoking was more extreme in urban areas for both men and women. The OR of AFO also increased with increasing age, probably mainly reflecting the effects of increased smoking duration (Table 4). AFO prevalence was inversely associated with annual income in never-smokers, but the OR of AFO for regular versus never-smokers was more extreme in those with higher household income (Table 4).
Table 4.
ORs for prevalent AFO and self-reported chronic bronchitis/emphysema in regular versus never-smokers by sociodemographic factors
| Characteristics of regular smokers (crude mean or prevalence)
|
AFO
|
Bronchitis/emphysema
|
|||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Prevalence (%) | Age started (years) | Age at baseline (years) | Amount smoked (g tobacco/day) | Always inhaled to lungs (%) | Prevalence (%)‡
|
OR (95% CI)† | Prevalence (%)‡
|
OR (95% CI)† | |||
| Never-smokers | Regular smokers | Never-smokers | Regular smokers | ||||||||
| Men | |||||||||||
| Study area | |||||||||||
| Urban | 70.1 | 22.6 | 52.9 | 18.0 | 42.7 | 3.1 | 5.2 | 1.72 (1.56–1.90) | 3.2 | 3.1 | 1.13 (1.01–1.26) |
| Rural | 77.6 | 22.4 | 52.8 | 18.6 | 31.1 | 7.0 | 8.7 | 1.28 (1.19–1.37) | 3.3 | 3.2 | 0.96 (0.87–1.06) |
| P trend | <0.0001 | 0.0311 | |||||||||
| Age at baseline, years | |||||||||||
| <50 | 73.7 | 20.9 | 42.6 | 18.7 | 38.1 | 2.2 | 2.5 | 1.11 (0.96–1.27) | 1.8 | 1.2 | 0.73 (0.62–0.87) |
| 50–59 | 77.8 | 22.7 | 54.7 | 19.0 | 36.4 | 4.9 | 6.3 | 1.30 (1.15–1.46) | 3.3 | 2.6 | 0.82 (0.71–0.95) |
| 60–69 | 73.0 | 24.6 | 64.7 | 17.3 | 31.8 | 9.1 | 13.2 | 1.51 (1.37–1.66) | 5.1 | 5.8 | 1.17 (1.03–1.32) |
| 70–79 | 68.0 | 25.1 | 72.5 | 15.6 | 31.3 | 14.9 | 21.2 | 1.63 (1.45–1.83) | 6.5 | 8.1 | 1.39 (1.18–1.62) |
| P trend | <0.0001 | <0.0001 | |||||||||
| Annual household income (yuan, thousands) | |||||||||||
| <5 | 76.5 | 23.3 | 58.7 | 17.0 | 27.7 | 9.3 | 9.5 | 1.33 (1.17–1.52) | 5.1 | 3.7 | 1.08 (0.88–1.32) |
| 5–9 | 76.0 | 22.7 | 52.9 | 17.7 | 34.8 | 6.6 | 8.3 | 1.26 (1.11–1.44) | 3.7 | 3.4 | 0.91 (0.76–1.08) |
| 10–19 | 74.1 | 22.2 | 52.7 | 18.3 | 38.1 | 6.1 | 7.3 | 1.34 (1.20–1.49) | 3.2 | 3.0 | 1.07 (0.93–1.24) |
| 20–34 | 74.0 | 22.2 | 51.8 | 18.6 | 37.2 | 4.1 | 6.1 | 1.62 (1.41–1.85) | 3.2 | 3.2 | 1.02 (0.87–1.18) |
| ≥35 | 72.9 | 22.7 | 51.3 | 19.1 | 35.8 | 3.3 | 5.5 | 1.81 (1.53–2.14) | 4.5 | 2.8 | 1.10 (0.93–1.30) |
| P trend | 0.0005 | 0.5173 | |||||||||
| Women | |||||||||||
| Study area | |||||||||||
| Urban | 2.9 | 29.5 | 61.0 | 9.7 | 29.1 | 3.4 | 5.5 | 2.04 (1.75–2.37) | 2.4 | 2.6 | 1.51 (1.28–1.78) |
| Rural | 3.5 | 25.6 | 59.6 | 9.5 | 22.9 | 5.0 | 7.1 | 1.44 (1.33–1.56) | 2.0 | 2.3 | 1.17 (1.02–1.34) |
| P trend | <0.0001 | 0.0195 | |||||||||
| Age at baseline, years | |||||||||||
| <50 | 1.2 | 27.5 | 43.9 | 10.1 | 31.0 | 2.3 | 2.9 | 1.44 (1.14–1.81) | 1.3 | 0.9 | 0.88 (0.57–1.36) |
| 50–59 | 2.9 | 26.3 | 55.0 | 10.0 | 25.8 | 4.0 | 6.7 | 1.35 (1.18–1.54) | 2.4 | 2.8 | 1.10 (0.88–1.37) |
| 60–69 | 7.5 | 27.3 | 65.4 | 9.4 | 23.4 | 7.5 | 12.0 | 1.74 (1.56–1.94) | 3.6 | 4.9 | 1.45 (1.25–1.69) |
| 70–79 | 10.1 | 27.7 | 72.5 | 9.0 | 23.3 | 13.4 | 18.8 | 1.61 (1.38–1.87) | 4.6 | 7.6 | 1.47 (1.17–1.84) |
| P trend | 0.0497 | 0.0099 | |||||||||
| Annual household income (yuan, thousands) | |||||||||||
| <5 | 8.2 | 25.4 | 62.4 | 9.6 | 20.3 | 5.8 | 7.2 | 1.38 (1.22–1.55) | 2.8 | 1.8 | 1.10 (0.90–1.33) |
| 5–9 | 4.1 | 26.5 | 58.9 | 9.7 | 28.0 | 4.8 | 6.4 | 1.38 (1.21–1.59) | 2.3 | 2.5 | 1.26 (1.02–1.57) |
| 10–19 | 3.2 | 27.2 | 59.5 | 9.7 | 26.6 | 4.1 | 6.0 | 1.72 (1.49–1.98) | 2.2 | 2.5 | 1.28 (1.04–1.57) |
| 20–34 | 1.8 | 30.0 | 60.1 | 9.5 | 28.0 | 3.6 | 6.2 | 1.95 (1.57–2.43) | 2.3 | 3.6 | 1.73 (1.32–2.27) |
| ≥35 | 1.4 | 29.7 | 59.3 | 9.5 | 24.2 | 3.5 | 7.6 | 1.90 (1.40–2.59) | 2.4 | 1.5 | 1.22 (0.82–1.84) |
| P trend | 0.0005 | 0.0553 | |||||||||
Notes:
ORs are for all regular smokers versus never-smokers, adjusted for 5-year age group, region, age group × region interaction, education, and income.
Prevalences of the disease are directly standardized to the age and area structure of the population in the China Kadoorie Biobank.
Abbreviations: OR, odds ratio; AFO, airflow obstruction; CI, confidence interval.
Discussion
In this large nationwide study of smoking and chronic respiratory disease among adult men and women in the Mainland China, the prevalence of spirometrically-defined AFO, as well as self-reported CB/E among never-smokers varied considerably across the ten areas of study. Compared with never-smokers, male regular smokers had, on average, about 50% excess risk of AFO and the disease prevalence was associated strongly and positively with the amount smoked and a younger age of starting to smoke regularly. For AFO, the OR was particularly large among smokers who had quit due to illness or those who had recently reduced the amount smoked. Among women, despite an extremely low smoking prevalence, smokers also had significant excess risk of AFO and CB/E.
Although our study comprised of cross-sectional analyses of baseline data from a prospective study, the observed excess risk of AFO among regular smokers was broadly consistent with the results of previous large prospective studies of smoking and cause-specific mortality in the Mainland China, and with the two meta-analyses of Asian prospective studies,6–10 which showed a 50% excess respiratory mortality in smokers and elevated risks in ex-smokers similar to those in current smokers.9,10 Our results are also in agreement with the findings from two other much smaller cross-sectional studies from the Mainland China on smoking with physician-diagnosed COPD or spirometrically-defined COPD.13,24
The large number of prevalent cases in our study allowed for the appropriate assessment of association between prevalent COPD cases with smoking status, frequency and habits, not only overall, but also in certain subgroups of the study population. The risk associated with smoking varied by area, age, sex, and income. The increasing trend of OR with increasing baseline age probably mainly reflected the effects of a longer duration of smoking among older smokers. Compared with younger smokers, however, the older smokers were less likely to start to smoke regularly at an earlier age, less likely to ever smoke cigarettes, less likely to smoke a large number of cigarettes/day, and less likely to inhale to the lung, all limiting their risk. The tobacco-attributed risk is more likely to increase significantly in the Mainland China when the older generation is replaced by younger ones. Similarly, the stronger associations of AFO with smoking in urban areas and in those with higher annual household incomes probably also reflected, at least in part, differences in past smoking patterns. The excess risk of AFO associated with smoking was similar in women compared to men, despite the fact that female smokers had started at an older age and smoked only about half as much – compared to their male counterparts. Other studies, including a Chinese study, have also reported similar findings.24,25 Further investigations of this apparent greater susceptibility of female smokers to COPD are needed.
To our knowledge, the present study is the only large study of AFO and smoking that contained detailed information on smoking cessation and recent changes in the amount smoked. Our results are in line with several earlier small studies of Chinese and Asian smokers that have found elevated risks of COPD (but not other diseases) in ex-smokers compared to current smokers.9,10,12,13 The significant excess risk of AFO among smokers who had quit because of ill health in the present study confirms the suggested notion that many smokers do not attempt to quit until they are ill with COPD. This is further supported by the elevated risk of AFO observed among smokers who had recently reduced their smoking intensity. In contrast, the little excess risk among ex-smokers who had quit by choice rather than due to ill health is consistent with the beneficial effect of quitting smoking that has been observed in Western populations.11
In our study, CB/E was associated only weakly with regular smoking, but strongly with quitting smoking because of ill health. Less than 15% of participants with AFO also had CB/E, suggesting that there may be considerable underdiagnosis of this condition in the population. In contrast to AFO, the general lack of association with regular smoking suggests an even greater degree of underdiagnosis of CB/E in regular smokers than in never-smokers. It is possible that smokers may be relatively unaware or unwilling to accept the serious health implications of early respiratory symptoms.
As well as several important strengths, our study also has a number of limitations. First, the association is based on cross-sectional data so we cannot be sure about the direction of causality, but smoking has been established as the main risk factor for COPD.4,5,15 In CKB, the mean age of starting to smoke was 22 years in men and 27 years in women, compared to a mean age of >40 years for the initial diagnosis of CB/E in both sexes. Therefore, reverse causality is probably not a concern in comparing regular smokers to never-smokers. However, the possibility of reverse causality or recall bias in the reporting of specific smoking habits by regular smokers cannot be excluded, in particular in the amount smoked at baseline. A tendency to adjust tobacco consumption in response to respiratory symptoms might also explain the relatively weak association of AFO with daily tobacco consumption at baseline. Second, as we did not use a bronchodilator, we may have overestimated the prevalence of COPD, but the degree of overestimation is likely to be small as the prevalence of asthma is quite low in the Mainland China when compared to Western countries.26,27 In addition, bronchodilator reversibility does not always distinguish well between asthma and COPD.28 Third, the spirometer used at the baseline survey did not produce a spirogram to allow for the assessment of the acceptability of blows, even though participants were carefully instructed and requested to make practice blows during the survey. Incomplete inhalation or early termination of a blow would have resulted in a reduced FVC and hence in the underestimation of AFO. If this misclassification were nondifferential across categories of smokers, we would expect it to bias associations towards the null.
With rapid economic development and improvements in living standards in the Mainland China, the age-standardized COPD rates in never-smokers may well decrease significantly over time. However, the present study showed that although the proportional risk of COPD associated with smoking is currently still very modest, the overall burden of tobacco-attributed COPD is already high because of the high background rate in the population. The prevalence of smoking in women is very low and is decreasing, but the relative risk of COPD in female smokers appears at least as great as in male smokers. Quitting smoking could have a beneficial effect on COPD providing it is done before ill health develops, but our data suggest that many smokers in the Mainland China did not fully appreciate the risks of smoking and tended to quit only after they had developed serious illness.
Acknowledgments
The chief acknowledgment is to the participants, the project staff, and the China National Centre for Disease Control and Prevention (CDC) and its regional offices for assisting with the fieldwork. Margaret Smith did some of the analysis and produced the initial draft of the paper. Baseline survey: Kadoorie Charitable Foundation, Hong Kong. Long-term continuation: UK Wellcome Trust (088158/Z/09/Z, 104085/Z/14/Z), Chinese Ministry of Science and Technology (2011BAI09B01), and the Chinese National Natural Science Foundation (81390541). The British Heart Foundation, UK Medical Research Council and Cancer Research UK provide core funding to the Oxford CTSU.
The China Kadoorie Biobank collaborative group members were as follows. International Steering Committee: Junshi Chen; Zhengming Chen (PI); Rory Collins; Liming Li (PI); and Richard Peto. International Co-ordinating Centre, Oxford: Derrick Bennett; Yumei Chang; Yiping Chen; Zhengming Chen; Robert Clarke; Huaidong Du; Xuejuan Fan; Haiyan Gao; Simon Gilbert; Andri Iona; Rene Kerosi; Ling Kong; Om Kurmi; Garry Lancaster; John McDonnell; Winnie Mei; Iona Millwood; Qunhua Nie; Jayakrishnan Radhakrishnan; Paul Ryder; Sam Sansome; Dan Schmidt; Paul Sherliker; Rajani Sohoni; Robin Walters; Jenny Wang; Lin Wang; Alex Williams; Ling Yang; and Xiaoming Yang. National Co-ordinating Centre, Beijing: Zheng Bian; Ge Chen; Lei Guo; Yu Guo; Bingyang Han; Can Hou; Peng Liu; Jun Lv; Pei Pei; Shuzhen Qu; Yunlong Tan; Canqing Yu; and Huiyan Zhou. 10 Regional Co-ordinating Centres, Qingdao Qingdao CDC: Zengchang Pang; Shaojie Wang; Yun Zhang; and Kui Zhang. Licang CDC: Silu Liu and Wei Hou. Heilongjiang Provincial CDC: Zhonghou Zhao; Shumei Liu; and Zhigang Pang. Nangang CDC: Weijia Feng; Shuling Wu; Liqiu Yang; Huili Han; Hui He; and Bo Yu. Hainan Provincial CDC: Xianhai Pan; Shanqing Wang; and Hongmei Wang. Meilan CDC: Xinhua Hao; Chunxing Chen; Shuxiong Lin; and Xiangyang Zheng. Jiangsu Provincial CDC: Xiaoshu Hu; Minghao Zhou; Ming Wu; and Ran Tao. Suzhou CDC: Yeyuan Wang; Yihe Hu; Liangcai Ma; Renxian Zhou; Guanqun Xu; and Yan Lu. Guangxi Provincial CDC: Baiqing Dong; Naying Chen; and Ying Huang. Liuzhou CDC: Mingqiang Li; Jinhuai Meng; Zhigao Gan; Jiujiu Xu; Yun Liu; and Jingxin Qing. Sichuan Provincial CDC: Xianping Wu; Yali Gao; and Ningmei Zhang. Pengzhou CDC: Guojin Luo; Xiangsan Que; and Xiaofang Chen. Gansu Provincial CDC: Pengfei Ge; Jian He; and Xiaolan Ren. Maiji CDC: Hui Zhang; Enke Mao; Guanzhong Li; Zhongxiao Li; Jun He; Yulong Lei; and Xiaoping Wang. Henan Provincial CDC: Guohua Liu; Baoyu Zhu; Gang Zhou; and Shixian Feng. Huixian CDC: Yulian Gao; Tianyou He; Li Jiang; Jianhua Qin; and Huarong Sun. Zhejiang Provincial CDC: Liqun Liu; Min Yu; Yaping Chen; and Ruying Hu. Tongxiang CDC: Zhixiang Hu; Jianjin Hu; Yijian Qian; Zhiying Wu; Chunmei Wang; and Lingli Chen. Hunan Provincial CDC: Wen Liu; Guangchun Li; and Huilin Liu. Liuyang CDC: Xiangquan Long; Xin Xu; Youping Xiong; Zhongwen Tan; Xuqiu Xie; Yunfang Peng; and Weifang Jia.
Footnotes
Disclosure
The authors report no conflicts of interest in this work.
References
- 1.Global Strategy for the Diagnosis, Management and Prevention of COPD [webpage on the Internet] Global Initiative for Chronic Obstructive Lung Disease (GOLD) 2014. [Accessed June 24, 2014]. Available from: http://www.goldcopd.org/
- 2.Yang G, Wang Y, Zeng Y, et al. Rapid health transition in China, 1990–2010: findings from the Global Burden of Disease Study 2010. Lancet. 2013;381(9882):1987–2015. doi: 10.1016/S0140-6736(13)61097-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Fang X, Wang X, Bai C. COPD in China: the burden and importance of proper management. Chest. 2011;139(4):920–929. doi: 10.1378/chest.10-1393. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Doll R, Peto R, Boreham J, Sutherland I. Mortality in relation to smoking: 50 years’ observations on male British doctors. BMJ. 2004;328(7455):1519. doi: 10.1136/bmj.38142.554479.AE. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Thun MJ, Carter BD, Feskanich D, et al. 50-year trends in smoking-related mortality in the United States. N Engl J Med. 2013;368(4):351–364. doi: 10.1056/NEJMsa1211127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Gu D, Kelly TN, Wu X, et al. Mortality attributable to smoking in China. N Engl J Med. 2009;360(2):150–159. doi: 10.1056/NEJMsa0802902. [DOI] [PubMed] [Google Scholar]
- 7.Liu BQ, Peto R, Chen ZM, et al. Emerging tobacco hazards in China: 1. Retrospective proportional mortality study of one million deaths. BMJ. 1998;317(7170):1411–1422. doi: 10.1136/bmj.317.7170.1411. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Niu SR, Yang GH, Chen ZM, et al. Emerging tobacco hazards in China: 2. Early mortality results from a prospective study. BMJ. 1998;317(7170):1423–1424. doi: 10.1136/bmj.317.7170.1423. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Zheng W, McLerran DF, Rolland BA, et al. Burden of total and cause-specific mortality related to tobacco smoking among adults aged ≥45 years in Asia: a pooled analysis of 21 cohorts. PLoS Med. 2014;11(4):e1001631. doi: 10.1371/journal.pmed.1001631. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Nakamura K, Huxley R, Ansary-Moghaddam A, Woodward M. The hazards and benefits associated with smoking and smoking cessation in Asia: a meta-analysis of prospective studies. Tob Control. 2009;18(5):345–353. doi: 10.1136/tc.2008.028795. [DOI] [PubMed] [Google Scholar]
- 11.Godtfredsen NS, Lam TH, Hansel TT, et al. COPD-related morbidity and mortality after smoking cessation: status of the evidence. Eur Respir J. 2008;32(4):844–853. doi: 10.1183/09031936.00160007. [DOI] [PubMed] [Google Scholar]
- 12.Lam TH, He Y, Shi QL, et al. Smoking, quitting, and mortality in a Chinese cohort of retired men. Ann Epidemiol. 2002;12(5):316–320. doi: 10.1016/s1047-2797(01)00258-7. [DOI] [PubMed] [Google Scholar]
- 13.Zhong N, Wang C, Yao W, et al. Prevalence of chronic obstructive pulmonary disease in China: a large, population-based survey. Am J Respir Crit Care Med. 2007;176(8):753–760. doi: 10.1164/rccm.200612-1749OC. [DOI] [PubMed] [Google Scholar]
- 14.Chen Z, Chen J, Collins R, et al. China Kadoorie Biobank (CKB) collaborative group China Kadoorie Biobank of 0.5 million people: survey methods, baseline characteristics and long-term follow-up. Int J Epidemiol. 2011;40(6):1652–1666. doi: 10.1093/ije/dyr120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.China Kadoorie Biobank [webpage on the Internet] China Kadoorie Biobank. Oxford UK: University of Oxford; 2014. [Accessed June 24, 2014]. Available from: http://www.ckbiobank.org. [Google Scholar]
- 16.Kurmi OP, Li L, Smith M, et al. Regional variations in the prevalence and misdiagnosis of air flow obstruction in China: baseline results from a prospective cohort of the China Kadoorie Biobank (CKB) BMJ Open Respir Res. 2014;1(1):e000025. doi: 10.1136/bmjresp-2014-000025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Smith M, Li L, Augustyn M, et al. China Kadoorie Biobank collaborative group Prevalence and correlates of airflow obstruction in ~317,000 never-smokers in China. Eur Respir J. 2014;44(1):66–77. doi: 10.1183/09031936.00152413. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Chen Z, Lee L, Chen J, et al. Cohort profile: the Kadoorie Study of Chronic Disease in China (KSCDC) Int J Epidemiol. 2005;34(6):1243–1249. doi: 10.1093/ije/dyi174. [DOI] [PubMed] [Google Scholar]
- 19.Chen JS, Petro R, Pan WH, Liu BQ, Campbell TC, Boreham J, editors. Geographic Study of Mortality, Biochemistry, Diet and Lifestyle in Rural China. Oxford, UK: Oxford University Press; 2006. [Google Scholar]
- 20.Zhang Q, Li L, Smith M, et al. China Kadoorie Biobank study collaboration Exhaled carbon monoxide and its associations with smoking, indoor household air pollution and chronic respiratory diseases among 512,000 Chinese adults. Int J Epidemiol. 2013;42(5):1464–1475. doi: 10.1093/ije/dyt158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Standardization of spirometry, 1994 update American Thoracic Society. Am J Respir Crit Care Med. 1995;152(3):1107–1136. doi: 10.1164/ajrccm.152.3.7663792. [DOI] [PubMed] [Google Scholar]
- 22.Miller MR, Hankinson J, Brusasco V, et al. ATS/ERS Task Force Standardisation of spirometry. Eur Respir J. 2005;26(2):319–338. doi: 10.1183/09031936.05.00034805. [DOI] [PubMed] [Google Scholar]
- 23.Plummer M. Improved estimates of floating absolute risk. Stat Med. 2004;23(1):93–104. doi: 10.1002/sim.1485. [DOI] [PubMed] [Google Scholar]
- 24.Xu F, Yin X, Zhang M, Shen H, Lu L, Xu Y. Prevalence of physician-diagnosed COPD and its association with smoking among urban and rural residents in regional mainland China. Chest. 2005;128(4):2818–2823. doi: 10.1378/chest.128.4.2818. [DOI] [PubMed] [Google Scholar]
- 25.Gan WQ, Man SF, Postma DS, Camp P, Sin DD. Female smokers beyond the perimenopausal period are at increased risk of chronic obstructive pulmonary disease: a systematic review and meta-analysis. Respir Res. 2006;7:52. doi: 10.1186/1465-9921-7-52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.To T, Stanojevic S, Moores G, et al. Global asthma prevalence in adults: findings from the cross-sectional world health survey. BMC Public Health. 2012;12:204. doi: 10.1186/1471-2458-12-204. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Wang D, Xiao W, Ma D, et al. Cross-sectional epidemiological survey of asthma in Jinan, China. Respirology. 2013;18(2):313–322. doi: 10.1111/resp.12005. [DOI] [PubMed] [Google Scholar]
- 28.Hanania NA, Celli BR, Donohue JF, Martin UJ. Bronchodilator reversibility in COPD. Chest. 2011;140(4):1055–1063. doi: 10.1378/chest.10-2974. [DOI] [PubMed] [Google Scholar]