Abstract
Objective: International and societal conflicts and natural disasters can leave physical and mental scars in people who are directly affected by these traumatic experiences. Posttraumatic stress disorder (PTSD) is the clinical manifestation of these experiences in the form of re-experiencing the trauma, avoidance of trauma-related stimuli, and persistent symptoms of hyperarousal. There is growing evidence that sleep disruption that occurs following trauma exposure may in fact contribute to the pathophysiology of PTSD and poor clinical outcomes. The purpose of this review is to highlight the importance of recognition and management of sleep disorders in patients with PTSD.
Data Sources: English-language, adult research studies published between 1985 and April 2014 were identified via the PubMed database. The search terms used were PTSD AND sleep disorders.
Study Selection: The search identified 792 original and review articles. Of these, 53 articles that discussed or researched sleep disorders in PTSD were selected. Fourteen randomized controlled trials of therapy for PTSD are included in this review.
Results: Impaired sleep is a common complaint mainly in the form of nightmares and insomnia among people with PTSD. Sleep apnea and periodic limb movement disorder are particularly prevalent in patients with PTSD and, yet, remain unrecognized. Although selective serotonin reuptake inhibitors are effective in improving PTSD global symptoms, they have a variable and modest effect on sleep disorder symptoms. Cognitive-behavioral treatment targeted to sleep and/or the use of the centrally acting selective α1 antagonist prazosin have been more successful in treating insomnia and nightmares in PTSD than other classes of medications. In view of the high occurrence of sleep apnea and periodic leg movement disorder, a thorough sleep evaluation and treatment are warranted.
Conclusions: Patients with PTSD have a high prevalence of sleep disorders and should be queried for insomnia, nightmares, periodic limb movement disorder, and sleep-disordered breathing.
Clinical Points
■ Sleep disorders in the form of insomnia, nightmares, sleep apnea, and movement disorders during sleep are common in posttraumatic stress disorder (PTSD).
■ While antidepressants are effective in the management of global symptoms of PTSD, they have variable and at best a modest effect on sleep disorder complaints.
■ Cognitive-behavioral treatment targeted to PTSD and selective α1 antagonists such as prazosin are standard therapeutic options for sleep disorders associated with PTSD.
International and societal conflicts and natural disasters can leave physical and mental scars in people who are directly affected by these traumatic experiences. Violent crimes, including rape and physical assaults, combat exposure, and natural disasters constitute examples of traumatic events.1 Posttraumatic stress disorder (PTSD) is the clinical manifestation of these experiences due to the difficulty in justifying these events or ameliorating the mental agony resulting from these traumatic exposures. Following exposure to a traumatic event, individuals who develop PTSD experience different clusters of symptoms, which include re-experiencing the trauma, avoidance of trauma-related stimuli, and persistent symptoms of hyperarousal.1 Nightmares and insomnia are diagnostic symptoms of PTSD1; however, other sleep disturbances such as sleep avoidance, sleep terrors, nocturnal anxiety attacks, acting out dreams, sleep apnea, and periodic leg movement disorder are also frequently reported and observed in PTSD patients.2–4
There is growing evidence that sleep disruption that occurs following trauma exposure may in fact contribute to the pathophysiology of PTSD and poor clinical outcomes.5,6 This review highlights the importance of sleep disorders in patients with PTSD and the challenges that physicians face in their management.
METHOD
English-language, adult research studies published between 1985 and April 2014 were identified via the PubMed database. The search terms used were PTSD AND sleep disorders. We identified 792 original and review articles. Of these, 53 articles discussed or researched sleep disorders in PTSD. Fourteen randomized controlled trials of therapy for PTSD were included in this review.7–20
RESULTS
Epidemiology
Epidemiologic studies indicate that the community prevalence of PTSD ranges from 1% to 10%,21,22 with higher estimates reported in victims of interpersonal violence (20%–30%) and combat veterans (15%–30%). Reports continue to show a 20% prevalence of PTSD in veterans of foreign wars.23 Difficulty initiating or maintaining sleep is reported by 44% of veterans with PTSD, 5.5% of veterans without PTSD, and 5% of civilians without the disorder.24 Another common sleep-related symptom of PTSD is nightmares. Nightmares have been reported by 19% to 71% of patients with PTSD.25 This wide variation in incidence of nightmares has been attributed to differences in the severity of PTSD,26 exposure to combat24 and other forms of aggression,25 and the presence of comorbid psychiatric diagnosis.27
Normal Sleep
According to the US Department of Health and Human Services,28 adults require 7 to 9 hours of sleep. Sleep comprises 2 main stages: non–rapid eye movement (NREM) and rapid eye movement (REM) sleep. Most dreams occur in REM sleep. In order to prevent acting out the dreams during REM sleep, the central nervous system inhibits voluntary muscles, with the exception of the diaphragm and extraocular muscles. Research shows the importance of sleep in memory consolidation and learning.29
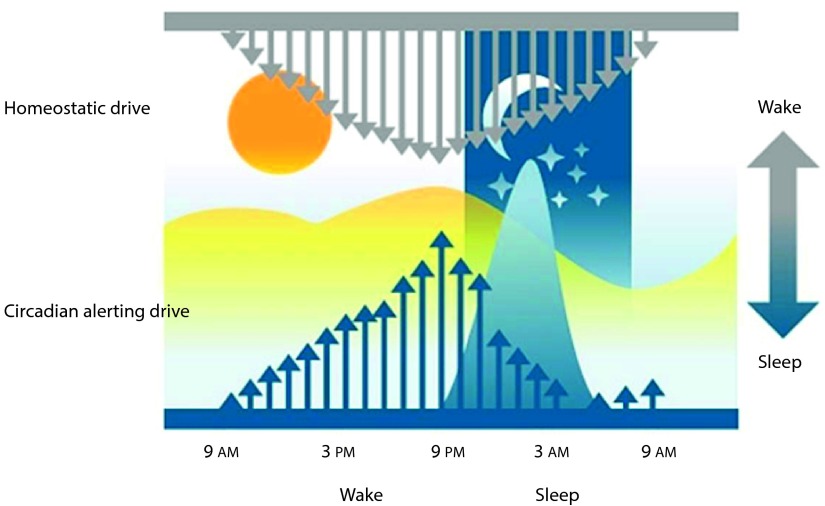
The sleep-wake cycle is regulated by 2 processes: homeostatic and circadian drives. Homeostatic drive increases as a function of the extended wakefulness period, and its effect diminishes during sleep.30 The biochemical basis of this drive is not entirely clear, but it has been shown that sustained neuronal activity can increase adenosine levels in the brain—adenosine levels rise in the basal forebrain during prolonged wakefulness and fall during sleep.31 Circadian drive originates from a rhythmic internal biological clock or circadian pacemaker in the suprachiasmatic nucleus; its rhythmicity is synchronized by entraining the external light-dark cycle. Circadian drive is at its peak around 9 pm. Thus, the balance between the homeostatic and circadian systems results in the strongest sleep drive generally between 2:00 and 4:00 am and a modest sleep drive in the afternoon between 1:00 and 3:00 pm (Figure 1). It has been shown that these drives are also shaped by emotional and cognitive inputs. Cognitive and emotional systems that may be able to override the normal homeostatic and circadian circuitry are doing so by means of inputs to the arousal system.32 Under some conditions, such as in shift work or during an emergency situation, this ability to overcome the more basic drives can be adaptive. However, when emotional states such as stress prevent sleep, the balance between homeostatic and circadian systems is perturbed as in poor sleep hygiene and irregular sleep-wake cycles, leading to insomnia as seen in PTSD.
Figure 1.
The Sleep-Wake Cyclea
aBased on Dijk and Edgar.82
bThe sleep-wake cycle is regulated by 2 processes: homeostatic and circadian drives. The homeostatic drive increases as a function of the extended wakefulness period; its effect diminishes during sleep. The circadian drive originates from a rhythmic internal biological clock or circadian pacemaker in the suprachiasmatic nucleus; its rhythmicity is synchronized by entraining the external light-dark cycle. The circadian drive is at its peak at around 9 pm. So, the balance between the homeostatic and circadian processes results in the strongest sleep drive generally between 2 and 4 am and a modest propensity for sleepiness in the afternoon between 1 and 3 pm.
Sleep in PTSD
Nightmares are highly prevalent and considered hallmarks of PTSD.4 Nightmares are reported in as many as 71% of patients with PTSD.2 Nightmares are primarily a REM sleep phenomenon since dream recalls are more common in REM than in NREM sleep. Nightmares may cause short or prolonged awakenings from sleep. Large studies of patients who had experienced a range of traumas indicate an increase of 60% in prevalence of disturbed sleep compared to those without PTSD.25,33 Insomnia is thought to arise primarily from NREM sleep disruption. Other NREM sleep disturbances often observed in trauma-exposed patients with PTSD include nocturnal panic attacks and sleep terrors.34–36 Presence of both nightmares and insomnia within 1 month posttrauma predicted the development of PTSD 6 months later.37 Further, there is evidence that disturbed sleep prior to a traumatic event poses an increased risk of PTSD.3,38 However, despite a high prevalence of sleep disorder symptoms, objective measures of sleep efficiency and fragmentation have been inconsistent. Some polysomnographic studies in PTSD patients have reported REM sleep anomalies,39,40 whereas others have not.41,42 NREM sleep anomalies such as reduced slow-wave sleep have also been reported in some.41 A meta-analysis of polysomnographic studies conducted on military veterans and civilian adults with PTSD43 found a modest increase in REM density and in percentage of stage 1 sleep and reduced slow wave sleep in PTSD compared to non-PTSD groups. The detailed analysis of electroencephalogram (EEG)-for the detection of the cyclic alternating pattern (CAP) and microarousals that are closely tied to autonomic and muscle functions-is more common in patients with PTSD compared to those without PTSD.40 The cyclic alternating pattern during sleep study is characterized by sequences of transient electrocortical events that are distinct from background EEG activity and recur at up to 1-minute intervals. This periodic activity is proposed as a measure of sleep instability and fragmentation and is a stronger predictor of subjective reports of insomnia than conventional definitions of arousals.44,45 So, increased quantities of the cyclic alternating pattern and microarousals could result in nonrestorative sleep and serve to reinforce the perception of constant sleeplessness in these patients.
The exact neurologic mechanisms of sleep disturbances in PTSD are not established. There is accumulating evidence that PTSD is associated with altered brain responses in limbic and paralimbic brain areas—namely, the amygdala and insula—in response to emotional (and typically trauma-related) stimuli.46,47 Recently, resting-state functional magnetic resonance imaging techniques have been applied to investigate the brain basal functional activity and connectivity between brain regions in PTSD.47,48 Specifically, there is some emerging evidence that altered resting-state connectivity between the posterior cingulate cortex and the amygdala may be a reliable prognostic indicator of PTSD symptomatology.49,50 Furthermore, studies have shown altered metabolic activity in frontal, parietal, temporal cortex, and limbic regions in patients with PTSD in comparison with those of controls.51 Thus, clinical observations focusing on the nature of sleep complaints in PTSD, polysomnographic studies, and functional neuroimaging point to a dysregulation in both REM and NREM sleep.
In addition to insomnia and nightmares,52 patients with PTSD have a higher prevalence of sleep apnea and periodic leg movement disorder of sleep.53 Of 110 active duty military personnel with recent combat exposures with a mean age of 33.6 years and a mean body mass index of 30.0 kg/m2, 63% met diagnostic criteria for sleep apnea and 64% for insomnia.4 Those diagnosed with insomnia had the highest rates of PTSD, depression, and mild traumatic brain injury and were more likely to have pain syndrome.4 Sleep disorders are increasingly recognized by medical providers; nonetheless, it is common to ascribe sleep disturbances solely to insomnia or an associated diagnosis, delaying or forgoing a definitive sleep evaluation.
A growing body of research suggests that periodic leg movements are more common in patients with PTSD than in controls. In a study of 25 Vietnam veterans with severe PTSD, 76% of patients had clinically significant periodic leg movement disorder, with a mean index (movements/h) of 38 (normal being < 15/h).54 In another study, periodic leg movements were experienced in 33% of veterans with PTSD and not at all in controls.55 The mechanism for the association between PTSD and periodic leg movements is not clear. It is possible that periodic leg movements are the result of the same neural mechanisms underlying exaggerated daytime startle responses in patients with PTSD, or, alternatively, periodic leg movement disorder may be a risk factor for PTSD.56 Periodic leg movements can be associated with restless legs syndrome and sleep disruption, resulting in complaints of insomnia or excessive daytime sleepiness.
Diagnostic Approach to Patients With PTSD
Individuals with history of physical or mental exposure to traumatic events and symptomatology consistent with PTSD based on DSM-5 criteria should be queried for sleep disorders. The initial screening for sleep disorder may include 2 questions: “How is your sleep?” and “How do you feel when you should be awake?” If either question suggest difficulty falling asleep or staying asleep, waking up unrested, or having excessive daytime sleepiness, more detailed questionnaires containing a sleep-wake diary, Epworth Sleepiness Scale,57 STOP-Bang Questionnaire58 for Sleep-Disordered Breathing, and questions pertaining to restless legs syndrome and periodic leg movements59 are available to further define the nature of the sleep problems. In view of the high prevalence of multiple sleep disorders associated with PTSD, including sleep-disordered breathing and periodic leg movement disorders, a consultation with a sleep medicine specialist might be in order for treatment planning and management. Patients with PTSD who report excessive daytime sleepiness, habitual snoring, witnessed apneas, restless legs, and hypertension on the questionnaires should be considered for sleep study. However, if symptomatology primarily suggests sleep-disordered breathing, home-based respiratory monitoring may suffice.60 Most home-based studies use type III monitors for assessment of respiration and oxygen saturation but not sleep architecture (EEG) or movement disorders (electromyography); therefore, sleep fragmentation and leg movements cannot be assessed. Actigraphy might be a useful tool for assessment of sleep-wake rhythm in subjects with inconsistent sleep pattern and poor sleep hygiene.
Management of Sleep Disorders in PTSD
Nonpharmacologic treatment.
The overall management of PTSD is beyond the scope of this review. Readers are referred to Bernardy and Friedman61 for more information. The primary management strategies for insomnia incorporate sleep restriction (which involves curtailing the amount of time spent in bed to approximate the subjective amount of asleep) and stimulus control.62
Cognitive-behavioral treatment for insomnia has been shown to improve sleep disturbances and is considered the first-line therapy.7,8,63,64 In a randomized, 3-arm placebo-controlled trial of sleep behavioral intervention versus prazosin (a centrally acting selective α1 antagonist) and placebo in 57 US military veterans, sleep behavioral intervention and prazosin were more effective than placebo for self-reported and clinician-rated global clinical improvements, reductions in prospective self-reported and diary-based measures of sleep continuity, and nightmare frequency.9 Sleep improvements were found in 62% of those who completed the active treatments and 25% of those randomized to placebo. The core sleep behavioral intervention components included education about nightmares and implementation of imagery rehearsal therapy, education about sleep and insomnia, and stimulus control and sleep restriction.65
A web-based application for smart phones was developed by the US Department of Veterans Affairs National Center for PSTD Dissemination and Training Division (http://www.ptsd.va.gov/public/pages/PTSDcoach.asp) based on fundamentals of cognitive-behavioral treatment targeted for better understanding and self-management of PTSD symptoms. The smart phone application provides educational information about PTSD (eg, symptoms, prevalence, risk factors), various treatment options, self-assessment with interpretative feedback about the severity of their symptoms, ability to track their symptoms over time, coping tools to help address acute PTSD symptoms, and links to find community-based support. In a pilot study,66 the majority of 45 veterans who used the program reported improvement in their symptoms of PTSD. Other modalities, such as an exercise program, have shown some promising results, with a significant reduction in PTSD, anxiety, and depression symptoms that lasted during 1-month follow-up.67,68 There is also growing evidence that mind-body practices are a viable intervention to improve the constellation of PTSD symptoms such as intrusive memories, avoidance, and increased emotional arousal.69
Pharmacologic Treatment
Selective serotonin-norepinephrine reuptake inhibitors.
Given the high degree of comorbidity between PTSD and major depressive disorder, and the documented efficacy of selective serotonin reuptake inhibitors (SSRIs) for depressed populations (as well as for a number of other discrete anxiety disorders), SSRIs and selective serotonin-norepinephrine reuptake inhibitors (SNRIs) are first-line medications for the treatment of PTSD.70 In a meta-analysis of 7 randomized trials, patients treated with SSRIs were more likely to experience improvement in symptoms (on the Clinician-Administered PTSD Scale or CAPS) and functioning than the group receiving placebo (RR = 1.59, 95% CI, 1.39–1.82).71 There is a great deal of variation in response to pharmacologic treatment, with few robust individual predictors of response available.72 Some ancillary symptoms of PTSD, such as sleep disturbance, can be particularly difficult to treat and are among the symptoms that result in the use of polypharmacy that is so common in the treatment of PTSD. Selected pharmacologic classes of medications for PTSD that are shown to be effective in randomized controlled trials are listed in Table 1.10–16 Specifically, sertraline and paroxetine improved PTSD symptoms on the CAPS and the clinician-administered Clinical Global Impressions–Improvement (CGI) scale compared to placebo in several randomized controlled trials (Table 1). However, sertraline and paroxetine had no significant effect on sleep disturbance symptoms, including insomnia and nightmare. For a more detailed evidence-based review, the reader is referred to Ipser and Stein.73
Table 1.
Pharmacotherapy Agents for Treating Posttraumatic Stress Disorder and Sleep Disturbances
| Drugs | Study | Sample Size (n) | Duration (wk) | Response Rate (%) |
Response Criteria | Efficacya | |
| Drug | Control | ||||||
| SSRIs | |||||||
| Sertraline | RCT10 | 134 | 12 | 43 | 31 | CAPS (primary outcome) | ↑ |
| 43 | 33 | IES | ↔ | ||||
| 27 | 18 | CGI-S | ↑ | ||||
| Sertraline | RCT11 | 208 | 12 | 45 | 36 | CAPS-2 (primary outcome) | ↑ |
| 50 | 35 | IES | ↑ | ||||
| 28 | 22 | CGI-S | ↑ | ||||
| 26 | 21 | PSQI | ↔ | ||||
| Paroxetine | RCT (pooled)12 | 1,180 | 12 | 46 | 32 | CAPS-2 | ↑ |
| 57 | 39 | CGI-I | ↑ | ||||
| SNRIs | |||||||
| Venlafaxine | RCT13 | 329 | 24 | 64 | 54 | CAPS-Sx | ↑ |
| Non-SSRIs | |||||||
| Nefazodone versus sertraline | RCT14 | 37 | 12 | 61 | 58 | CAPS-2 | ↔ |
| 44 | 46 | CGI-I | ↔ | ||||
| 43 | 43 | PSQI | ↔ | ||||
| Olanzapine | RCT15 | 19 | 8 | 17 | 3 | CAPS | ↑ |
| 30 | 11 | CGI-I | ↔ | ||||
| 20 | 10 | PSQI | ↑ | ||||
| Prazosin | RCT16 | 40 | 8 | 49 | 15 | CAPS (distressing dreams) | ↑ |
| 71 | 12 | CGI-C | ↑ | ||||
| 28 | 6 | PSQI | ↑ | ||||
Significant differences in PTSD symptom severity in favor of medication are indicated by ↑ and nonsignificant differences by ↔.
Abbreviations: CAPS = Clinician-Administered PTSD Scale, CGI-C = Clinical Global Impression of Change, CGI-I = Clinical Global Impressions–Improvement, CGI-S = Clinical Global Impressions–Severity, IES = Impact of Event Scale, PSQI = Pittsburgh Sleep Quality Index, RCT = randomized controlled trial, SNRI = selective serotonin-norepinephrine reuptake inhibitor, SSRI = selective serotonin reuptake inhibitor.
Dopamine, serotonin, histamine receptor antagonists.
In patients with SSRI-resistant PTSD, olanzapine augmentation was associated with a significantly greater reduction in sleep disturbance, as well as other symptoms of PTSD and depression, compared with placebo.15 Mirtazapine, an antidepressant with serotonin and histamine receptor antagonism, has shown some benefits in PTSD as an alternative to SSRIs (sertraline) in an open-label trial, in part, due to its sedating side effect that can be therapeutically useful to some patients.17 Trazodone, a histamine and α1-adrenergic receptor antagonist, appears to be effective for the treatment of insomnia and nightmares associated with chronic PTSD, but it is not recommended as a first-line therapy for PTSD.61
Selective α1-adrenergic antagonists.
Most of the drug trials focused on global PTSD symptoms, with few reporting sleep disturbances as outcome measures. Clinical studies suggest that enhanced postsynaptic adrenergic receptor responsiveness to central nervous system norepinephrine contributes to the pathophysiology of PTSD.74,75 Preclinical studies provide rationale for specific involvement of the postsynaptic α1 adrenoreceptor in this pathophysiologic process. Specifically, central nervous system α1-adrenergic receptor stimulation disrupts sleep physiology and enhances sleep-stage phenomena associated with emergence of trauma nightmares.76 On the basis of the putative noradrenergic alterations seen in PTSD, several pharmacologic agents have been proposed as possible treatments. Prazosin has been more effective than other agents, providing the basis for the findings that α1 receptor stimulation is linked to sleep disruption, stress-induced disruptions in prefrontal cortex cognitive processing, and increased release of corticotropin-releasing hormone,75,77 all phenomena commonly seen in PTSD.46,78 The principal findings of note from these trials were decreased sleep disruption and nightmares and increase in total sleep time and REM sleep.16,18,19 In addition, the improvements in sleep with prazosin were accompanied by significant improvements in daytime symptoms of PTSD. The US Department of Veterans Affairs/Department of Defense practice guidelines recommend prazosin for sleep disturbances and nightmares in PTSD but not for global PTSD.61
Hypnotics.
There is insufficient evidence for beneficial effect of hypnotics in PTSD.73 In a small randomized double-blind placebo-controlled crossover trial of escopiclone for 3 weeks in 24 patients with PTSD and associated sleep disturbance, escopiclone improved PTSD symptoms as well as sleep latency and subjective sleep quality.20 However, the current guidelines by the US Department of Veterans Affairs/Department of Defense caution health care providers against the prescription of benzodiazepines in the management of PTSD.61 Additionally, there is evidence that benzodiazepines may interfere with psychotherapy treatments that are first-line intervention in PTSD.79
Treatment of Sleep Apnea
There are several treatment options available for sleep-disordered breathing. These options include positive airway pressure treatment, oral appliance therapy, and upper airway surgery. Positive airway pressure treatment using a nasal or full face mask is the most commonly used therapy. However, it is best for the patient to be referred to a sleep medicine center for evaluation and management.80
Treatment of Periodic Leg Movement Disorder
Many central nervous system–acting medications, particularly SSRIs, can cause or exacerbate periodic leg movement disorders. Dose modification of SSRIs or consideration for the addition of specific therapeutic agents for periodic leg movement disorder may be necessary.81
SUMMARY
Among victims of violence and combat veterans, PTSD is prevalent and is associated with significant burden of anxiety and depression and poor quality of life. In addition, PTSD is associated with high risk for sleep disturbances in the form of sleep fragmentation, nightmares, sleep apnea, and periodic leg movement disorder. All of these sleep disturbances can exacerbate symptoms of PTSD. A thorough clinical evaluation including sleep quality assessment should be part of the overall management of patients with PTSD.
Drug names: mirtazapine (Remeron and others), olanzapine (Zyprexa and others), paroxetine (Paxil, Pexeva, and others), prazosin (Minipress and others), sertraline (Zoloft and others), trazodone (Oleptro and others), venlafaxine (Effexor and others).
Disclosure of off-label usage: The authors have determined that, to the best of their knowledge, mirtazapine, olanzapine, prazosin, trazodone, venlafaxine, and nefazodone are not approved by the US Food and Drug Administration for the treatment of PTSD.
Author contributions: Both authors have contributed equally to the preparation of this manuscript.
Financial disclosure: Drs Mohsenin and Mohsenin have no personal affiliations or financial relationships with any commercial interest to disclose relative to the article..
Funding/support: None reported.
Footnotes
CME Background
Articles are selected for credit designation based on an assessment of the educational needs of CME participants, with the purpose of providing readers with a curriculum of CME articles on a variety of topics throughout each volume. Activities are planned using a process that links identified needs with desired results.
To obtain credit, read the article, correctly answer at least 70% of the questions in the Posttest, and complete the Evaluation. The Posttest and Evaluation are available at http://www.cmeinstitute.com/activities/Pages/journal.aspx.
CME Objective
- Provide evidence-based treatment for patients with PTSD who have sleep disturbances and sleep disorders
Accreditation Statement
The CME Institute of Physicians Postgraduate Press, Inc., is accredited by the Accreditation Council for Continuing Medical Education to provide continuing medical education for physicians.
Credit Designation
The CME Institute of Physicians Postgraduate Press, Inc., designates this journal-based CME activity for a maximum of 1.0 AMA PRA Category 1 Credit™. Physicians should claim only the credit commensurate with the extent of their participation in the activity.
Note: The American Academy of Physician Assistants (AAPA) accepts certificates of participation for educational activities certified for AMA PRA Category 1 Credit™ from organizations accredited by ACCME or a recognized state medical society. Physician assistants may receive a maximum of 1.0 hour of Category I credit for completing this program.
Date of Original Release/Review
This educational activity is eligible for AMA PRA Category 1 Credit™ through December 31, 2017. The latest review of this material was December 2014.
Financial Disclosure
All individuals in a position to influence the content of this activity were asked to complete a statement regarding all relevant personal financial relationships between themselves or their spouse/partner and any commercial interest. The CME Institute has resolved any conflicts of interest that were identified. In the past year, Larry Culpepper, MD, MPH, Editor in Chief, has been a consultant for Forest, Lundbeck, Merck, Sunovion, and Takeda. No member of the CME Institute staff reported any relevant personal financial relationships. Faculty financial disclosure appears with the article.
1. Ms A was robbed at gunpoint in a carjacking a year ago, and she reports symptoms of avoidance, hyperarousal, and re-experiencing. When you ask, “How is your sleep?” Ms A says it is inconsistent, and she always feels tired. She watches television when she can’t sleep. Which of the following is the best next step to assess Ms A’s sleep problem?
| a. | Refer her to a sleep specialist |
| b. | Have her undergo sleep study at a sleep center |
| c. | Use a questionnaire with a sleep-wake diary |
| d. | Set up home-based respiratory monitoring |
2. Ms A is diagnosed with posttraumatic stress disorder (PTSD), and insomnia is a treatment target. Which one of the following is a first-line treatment for her insomnia?
| a. | Cognitive-behavioral therapy for insomnia |
| b. | An exercise program |
| c. | Mind-body practices |
| d. | A nightly benzodiazepine for 3 weeks |
3. Mr B, who is obese, visits you for the first time because he recently moved to the area. He survived a major earthquake at his previous residence and has been taking a selective serotonin reuptake inhibitor (SSRI) for PTSD. Although the SSRI has helped, he mentions not feeling rested when he wakes up and being sleepy during the day. To help Mr B sleep better, you should take all of the following steps except:
| a. | Prescribe a hypnotic for bedtime and encourage daily exercise |
| b. | Evaluate him for periodic leg movement disorder |
| c. | Evaluate him for sleep apnea |
| d. | Ask him whether he has problems with nightmares |
4. Mr C experienced heavy combat in Vietnam and saw his best friend die. He has had a long-standing problem with nightmares, and he finally sought treatment at a sleep center. Their report found no sleep disorders and recommended an evaluation for PTSD. Your evaluation confirms that Mr C does have PTSD. He currently refuses cognitive-behavioral therapy. What is the best evidence-based strategy to help Mr C with PTSD, including nightmares?
| a. | Prescribe an SSRI and olanzapine |
| b. | Prescribe an SSRI, and, if his nightmares do not resolve, add prazosin |
| c. | Prescribe mirtazapine and help him find community-based support |
| d. | Prescribe trazodone, and, if his nightmares do not resolve, add an SSRI |
References
- 1.Svenaeus F. Diagnostic and Statistical Manual of Mental Disorders. Fifth Edition. American Psychiatric Publishing; Washington, DC: 2013. Diagnosing mental disorders and saving the normal. [Google Scholar]
- 2.Krakow B, Haynes PL, Warner TD, et al. Nightmares, insomnia, and sleep-disordered breathing in fire evacuees seeking treatment for posttraumatic sleep disturbance. J Trauma Stress. 2004;17(3):257–268. doi: 10.1023/B:JOTS.0000029269.29098.67. [DOI] [PubMed] [Google Scholar]
- 3.Hoge CW, McGurk D, Thomas JL, et al. Mild traumatic brain injury in US soldiers returning from Iraq. N Engl J Med. 2008;358(5):453–463. doi: 10.1056/NEJMoa072972. [DOI] [PubMed] [Google Scholar]
- 4.Mysliwiec V, Gill J, Lee H, et al. Sleep disorders in US military personnel: a high rate of comorbid insomnia and obstructive sleep apnea. Chest. 2013;144(2):549–557. doi: 10.1378/chest.13-0088. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Koren D, Arnon I, Lavie P, et al. Sleep complaints as early predictors of posttraumatic stress disorder: a 1-year prospective study of injured survivors of motor vehicle accidents. Am J Psychiatry. 2002;159(5):855–857. doi: 10.1176/appi.ajp.159.5.855. [DOI] [PubMed] [Google Scholar]
- 6.Mellman TA, Bustamante V, Fins AI, et al. REM sleep and the early development of posttraumatic stress disorder. Am J Psychiatry. 2002;159(10):1696–1701. doi: 10.1176/appi.ajp.159.10.1696. [DOI] [PubMed] [Google Scholar]
- 7.Krakow B, Hollifield M, Johnston L, et al. Imagery rehearsal therapy for chronic nightmares in sexual assault survivors with posttraumatic stress disorder: a randomized controlled trial. JAMA. 2001;286(5):537–545. doi: 10.1001/jama.286.5.537. [DOI] [PubMed] [Google Scholar]
- 8.Krakow B, Johnston L, Melendrez D, et al. An open-label trial of evidence-based cognitive behavior therapy for nightmares and insomnia in crime victims with PTSD. Am J Psychiatry. 2001;158(12):2043–2047. doi: 10.1176/appi.ajp.158.12.2043. [DOI] [PubMed] [Google Scholar]
- 9.Germain A, Richardson R, Moul DE, et al. Placebo-controlled comparison of prazosin and cognitive-behavioral treatments for sleep disturbances in US military veterans. J Psychosom Res. 2012;72(2):89–96. doi: 10.1016/j.jpsychores.2011.11.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Brady K, Pearlstein T, Asnis GM, et al. Efficacy and safety of sertraline treatment of posttraumatic stress disorder: a randomized controlled trial. JAMA. 2000;283(14):1837–1844. doi: 10.1001/jama.283.14.1837. [DOI] [PubMed] [Google Scholar]
- 11.Davidson JR, Rothbaum BO, van der Kolk BA, et al. Multicenter, double-blind comparison of sertraline and placebo in the treatment of posttraumatic stress disorder. Arch Gen Psychiatry. 2001;58(5):485–492. doi: 10.1001/archpsyc.58.5.485. [DOI] [PubMed] [Google Scholar]
- 12.Stein DJ, Davidson J, Seedat S, et al. Paroxetine in the treatment of posttraumatic stress disorder: pooled analysis of placebo-controlled studies. Expert Opin Pharmacother. 2003;4(10):1829–1838. doi: 10.1517/14656566.4.10.1829. [DOI] [PubMed] [Google Scholar]
- 13.Davidson J, Baldwin D, Stein DJ, et al. Treatment of posttraumatic stress disorder with venlafaxine extended release: a 6-month randomized controlled trial. Arch Gen Psychiatry. 2006;63(10):1158–1165. doi: 10.1001/archpsyc.63.10.1158. [DOI] [PubMed] [Google Scholar]
- 14.McRae AL, Brady KT, Mellman TA, et al. Comparison of nefazodone and sertraline for the treatment of posttraumatic stress disorder. Depress Anxiety. 2004;19(3):190–196. doi: 10.1002/da.20008. [DOI] [PubMed] [Google Scholar]
- 15.Stein MB, Kline NA, Matloff JL. Adjunctive olanzapine for SSRI-resistant combat-related PTSD: a double-blind, placebo-controlled study. Am J Psychiatry. 2002;159(10):1777–1779. doi: 10.1176/appi.ajp.159.10.1777. [DOI] [PubMed] [Google Scholar]
- 16.Raskind MA, Peskind ER, Hoff DJ, et al. A parallel group placebo controlled study of prazosin for trauma nightmares and sleep disturbance in combat veterans with posttraumatic stress disorder. Biol Psychiatry. 2007;61(8):928–934. doi: 10.1016/j.biopsych.2006.06.032. [DOI] [PubMed] [Google Scholar]
- 17.Chung MY, Min KH, Jun YJ, et al. Efficacy and tolerability of mirtazapine and sertraline in Korean veterans with posttraumatic stress disorder: a randomized open-label trial. Hum Psychopharmacol. 2004;19(7):489–494. doi: 10.1002/hup.615. [DOI] [PubMed] [Google Scholar]
- 18.Raskind MA, Peskind ER, Kanter ED, et al. Reduction of nightmares and other PTSD symptoms in combat veterans by prazosin: a placebo-controlled study. Am J Psychiatry. 2003;160(2):371–373. doi: 10.1176/appi.ajp.160.2.371. [DOI] [PubMed] [Google Scholar]
- 19.Taylor FB, Martin P, Thompson C, et al. Prazosin effects on objective sleep measures and clinical symptoms in civilian trauma posttraumatic stress disorder: a placebo-controlled study. Biol Psychiatry. 2008;63(6):629–632. doi: 10.1016/j.biopsych.2007.07.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Pollack MH, Hoge EA, Worthington JJ, et al. Eszopiclone for the treatment of posttraumatic stress disorder and associated insomnia: a randomized, double-blind, placebo-controlled trial. J Clin Psychiatry. 2011;72(7):892–897. doi: 10.4088/JCP.09m05607gry. [DOI] [PubMed] [Google Scholar]
- 21.Breslau N, Kessler RC, Chilcoat HD, et al. Trauma and posttraumatic stress disorder in the community: the 1996 Detroit Area Survey of Trauma. Arch Gen Psychiatry. 1998;55(7):626–632. doi: 10.1001/archpsyc.55.7.626. [DOI] [PubMed] [Google Scholar]
- 22.Kessler RC, Sonnega A, Bromet E, et al. Posttraumatic stress disorder in the National Comorbidity Survey. Arch Gen Psychiatry. 1995;52(12):1048–1060. doi: 10.1001/archpsyc.1995.03950240066012. [DOI] [PubMed] [Google Scholar]
- 23.Hoge CW, Castro CA, Messer SC, et al. Combat duty in Iraq and Afghanistan, mental health problems, and barriers to care. N Engl J Med. 2004;351(1):13–22. doi: 10.1056/NEJMoa040603. [DOI] [PubMed] [Google Scholar]
- 24.Neylan TC, Marmar CR, Metzler TJ, et al. Sleep disturbances in the Vietnam generation: findings from a nationally representative sample of male Vietnam veterans. Am J Psychiatry. 1998;155(7):929–933. doi: 10.1176/ajp.155.7.929. [DOI] [PubMed] [Google Scholar]
- 25.Ohayon MM, Shapiro CM. Sleep disturbances and psychiatric disorders associated with posttraumatic stress disorder in the general population. Compr Psychiatry. 2000;41(6):469–478. doi: 10.1053/comp.2000.16568. [DOI] [PubMed] [Google Scholar]
- 26.Bustamante V, Mellman TA, David D, et al. Cognitive functioning and the early development of PTSD. J Trauma Stress. 2001;14(4):791–797. doi: 10.1023/A:1013050423901. [DOI] [PubMed] [Google Scholar]
- 27.Leskin GA, Woodward SH, Young HE, et al. Effects of comorbid diagnoses on sleep disturbance in PTSD. J Psychiatr Res. 2002;36(6):449–452. doi: 10.1016/s0022-3956(02)00025-0. [DOI] [PubMed] [Google Scholar]
- 28.Office of Disease Prevention and Health Promotion. Washington, DC: US Department of Health and Human Services; 2011. Healthy People 2020 Objective Topic Areas. [Google Scholar]
- 29.Stickgold R. Neuroscience: a memory boost while you sleep. Nature. 2006;444(7119):559–560. doi: 10.1038/nature05309. [DOI] [PubMed] [Google Scholar]
- 30.Fuller PM, Gooley JJ, Saper CB. Neurobiology of the sleep-wake cycle: sleep architecture, circadian regulation, and regulatory feedback. J Biol Rhythms. 2006;21(6):482–493. doi: 10.1177/0748730406294627. [DOI] [PubMed] [Google Scholar]
- 31.Strecker RE, Morairty S, Thakkar MM, et al. Adenosinergic modulation of basal forebrain and preoptic/anterior hypothalamic neuronal activity in the control of behavioral state. Behav Brain Res. 2000;115(2):183–204. doi: 10.1016/s0166-4328(00)00258-8. [DOI] [PubMed] [Google Scholar]
- 32.Saper CB, Cano G, Scammell TE. Homeostatic, circadian, and emotional regulation of sleep. J Comp Neurol. 2005;493(1):92–98. doi: 10.1002/cne.20770. [DOI] [PubMed] [Google Scholar]
- 33.Foa EB, Riggs DS, Gershuny BS. Arousal, numbing, and intrusion: symptom structure of PTSD following assault. Am J Psychiatry. 1995;152(1):116–120. doi: 10.1176/ajp.152.1.116. [DOI] [PubMed] [Google Scholar]
- 34.Freed S, Craske MG, Greher MR. Nocturnal panic and trauma. Depress Anxiety. 1999;9(3):141–145. doi: 10.1002/(sici)1520-6394(1999)9:3<141::aid-da8>3.0.co;2-5. [DOI] [PubMed] [Google Scholar]
- 35.Germain A, Hall M, Krakow B, et al. A brief sleep scale for posttraumatic stress disorder: Pittsburgh Sleep Quality Index Addendum for PTSD. J Anxiety Disord. 2005;19(2):233–244. doi: 10.1016/j.janxdis.2004.02.001. [DOI] [PubMed] [Google Scholar]
- 36.Krakow B, Lowry C, Germain A, et al. A retrospective study on improvements in nightmares and posttraumatic stress disorder following treatment for comorbid sleep-disordered breathing. J Psychosom Res. 2000;49(5):291–298. doi: 10.1016/s0022-3999(00)00147-1. [DOI] [PubMed] [Google Scholar]
- 37.Harvey AG, Bryant RA. The relationship between acute stress disorder and posttraumatic stress disorder: a prospective evaluation of motor vehicle accident survivors. J Consult Clin Psychol. 1998;66(3):507–512. doi: 10.1037//0022-006x.66.3.507. [DOI] [PubMed] [Google Scholar]
- 38.Bryant RA, Creamer M, O’Donnell M, et al. Sleep disturbance immediately prior to trauma predicts subsequent psychiatric disorder. Sleep. 2010;33(1):69–74. doi: 10.1093/sleep/33.1.69. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Mellman TA, Nolan B, Hebding J, et al. A polysomnographic comparison of veterans with combat-related PTSD, depressed men, and non-ill controls. Sleep. 1997;20(1):46–51. doi: 10.1093/sleep/20.1.46. [DOI] [PubMed] [Google Scholar]
- 40.Engdahl BE, Eberly RE, Hurwitz TD, et al. Sleep in a community sample of elderly war veterans with and without posttraumatic stress disorder. Biol Psychiatry. 2000;47(6):520–525. doi: 10.1016/s0006-3223(99)00201-2. [DOI] [PubMed] [Google Scholar]
- 41.Woodward SH, Bliwise DL, Friedman MJ, et al. Subjective versus objective sleep in Vietnam combat veterans hospitalized for PTSD. J Trauma Stress. 1996;9(1):137–143. doi: 10.1007/BF02116839. [DOI] [PubMed] [Google Scholar]
- 42.Hurwitz TD, Mahowald MW, Kuskowski M, et al. Polysomnographic sleep is not clinically impaired in Vietnam combat veterans with chronic posttraumatic stress disorder. Biol Psychiatry. 1998;44(10):1066–1073. doi: 10.1016/s0006-3223(98)00089-4. [DOI] [PubMed] [Google Scholar]
- 43.Kobayashi I, Boarts JM, Delahanty DL. Polysomnographically measured sleep abnormalities in PTSD: a meta-analytic review. Psychophysiology. 2007;44(4):660–669. doi: 10.1111/j.1469-8986.2007.537.x. [DOI] [PubMed] [Google Scholar]
- 44.Parrino L, Ferrillo F, Smerieri A, et al. Is insomnia a neurophysiological disorder? the role of sleep EEG microstructure. Brain Res Bull. 2004;63(5):377–383. doi: 10.1016/j.brainresbull.2003.12.010. [DOI] [PubMed] [Google Scholar]
- 45.Parrino L, Ferri R, Bruni O, et al. Cyclic alternating pattern (CAP): the marker of sleep instability. Sleep Med Rev. 2012;16(1):27–45. doi: 10.1016/j.smrv.2011.02.003. [DOI] [PubMed] [Google Scholar]
- 46.Germain A, Buysse DJ, Nofzinger E. Sleep-specific mechanisms underlying posttraumatic stress disorder: integrative review and neurobiological hypotheses. Sleep Med Rev. 2008;12(3):185–195. doi: 10.1016/j.smrv.2007.09.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Sripada RK, King AP, Garfinkel SN, et al. Altered resting-state amygdala functional connectivity in men with posttraumatic stress disorder. J Psychiatry Neurosci. 2012;37(4):241–249. doi: 10.1503/jpn.110069. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Rabinak CA, Angstadt M, Welsh RC, et al. Altered amygdala resting-state functional connectivity in posttraumatic stress disorder. Front Psychiatry. 2011;2:62. doi: 10.3389/fpsyt.2011.00062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Lanius RA, Bluhm RL, Coupland NJ, et al. Default mode network connectivity as a predictor of posttraumatic stress disorder symptom severity in acutely traumatized subjects. Acta Psychiatr Scand. 2010;121(1):33–40. doi: 10.1111/j.1600-0447.2009.01391.x. [DOI] [PubMed] [Google Scholar]
- 50.Zhou Y, Wang Z, Qin LD, et al. Early altered resting-state functional connectivity predicts the severity of posttraumatic stress disorder symptoms in acutely traumatized subjects. PLoS ONE. 2012;7(10):e46833. doi: 10.1371/journal.pone.0046833. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Shin LM, Lasko NB, Macklin ML, et al. Resting metabolic activity in the cingulate cortex and vulnerability to posttraumatic stress disorder. Arch Gen Psychiatry. 2009;66(10):1099–1107. doi: 10.1001/archgenpsychiatry.2009.138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Krakow B, Germain A, Tandberg D, et al. Sleep breathing and sleep movement disorders masquerading as insomnia in sexual assault survivors. Compr Psychiatry. 2000;41(1):49–56. doi: 10.1016/s0010-440x(00)90131-7. [DOI] [PubMed] [Google Scholar]
- 53.Krakow B, Melendrez D, Pedersen B, et al. Complex insomnia: insomnia and sleep-disordered breathing in a consecutive series of crime victims with nightmares and PTSD. Biol Psychiatry. 2001;49(11):948–953. doi: 10.1016/s0006-3223(00)01087-8. [DOI] [PubMed] [Google Scholar]
- 54.Brown TM, Boudewyns PA. Periodic limb movements of sleep in combat veterans with posttraumatic stress disorder. J Trauma Stress. 1996;9(1):129–136. doi: 10.1007/BF02116838. [DOI] [PubMed] [Google Scholar]
- 55.Mellman TA, Kulick-Bell R, Ashlock LE, et al. Sleep events among veterans with combat-related posttraumatic stress disorder. Am J Psychiatry. 1995;152(1):110–115. doi: 10.1176/ajp.152.1.110. [DOI] [PubMed] [Google Scholar]
- 56.Ross RJ, Ball WA, Dinges DF, et al. Motor dysfunction during sleep in posttraumatic stress disorder. Sleep. 1994;17(8):723–732. doi: 10.1093/sleep/17.8.723. [DOI] [PubMed] [Google Scholar]
- 57.Johns MW. Sensitivity and specificity of the Multiple Sleep Latency Test (MSLT), the Maintenance of Wakefulness Test and the Epworth Sleepiness Scale: failure of the MSLT as a gold standard. J Sleep Res. 2000;9(1):5–11. doi: 10.1046/j.1365-2869.2000.00177.x. [DOI] [PubMed] [Google Scholar]
- 58.Farney RJ, Walker BS, Farney RM, et al. The STOP-Bang equivalent model and prediction of severity of obstructive sleep apnea: relation to polysomnographic measurements of the apnea/hypopnea index. J Clin Sleep Med. 2011;7(5):459–65B. doi: 10.5664/JCSM.1306. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Hilbert J, Mohsenin V. Can periodic limb movement disorder be diagnosed without polysomnography? a case-control study. Sleep Med. 2003;4(1):35–41. doi: 10.1016/s1389-9457(02)00238-1. [DOI] [PubMed] [Google Scholar]
- 60.Mohsenin V. Portable monitoring for obstructive sleep apnea: the horse is out of the barn-avoiding pitfalls. Am J Med. 2013;126(4):e1–e3. doi: 10.1016/j.amjmed.2012.05.016. [DOI] [PubMed] [Google Scholar]
- 61.Bernardy NC, Friedman MJ. 2010 VA/DOD Clinical Practice Guideline for Management of Posttraumatic Stress: how busy clinicians can best adopt updated recommendations. J Rehabil Res Dev. 2012;49(5):vii–viii. doi: 10.1682/jrrd.2012.02.0036. [DOI] [PubMed] [Google Scholar]
- 62.Morgenthaler TI, Kapen S, Lee-Chiong T, et al. Standards of Practice Committee; American Academy of Sleep Medicine. Practice parameters for the medical therapy of obstructive sleep apnea. Sleep. 2006;29(8):1031–1035. [PubMed] [Google Scholar]
- 63.Nishith P, Duntley SP, Domitrovich PP, et al. Effect of cognitive-behavioral therapy on heart rate variability during REM sleep in female rape victims with PTSD. J Trauma Stress. 2003;16(3):247–250. doi: 10.1023/A:1023791906879. [DOI] [PubMed] [Google Scholar]
- 64.Zayfert C, DeViva JC. Residual insomnia following cognitive-behavioral therapy for PTSD. J Trauma Stress. 2004;17(1):69–73. doi: 10.1023/B:JOTS.0000014679.31799.e7. [DOI] [PubMed] [Google Scholar]
- 65.Germain A, Shear MK, Hall M, et al. Effects of a brief behavioral treatment for PTSD-related sleep disturbances: a pilot study. Behav Res Ther. 2007;45(3):627–632. doi: 10.1016/j.brat.2006.04.009. [DOI] [PubMed] [Google Scholar]
- 66.Kuhn E, Greene C, Hoffman J, et al. Preliminary evaluation of PTSD Coach, a smartphone app for posttraumatic stress symptoms. Mil Med. 2014;179(1):12–18. doi: 10.7205/MILMED-D-13-00271. [DOI] [PubMed] [Google Scholar]
- 67.Manger TA, Motta RW. The impact of an exercise program on posttraumatic stress disorder, anxiety, and depression. Int J Emerg Ment Health. 2005;7(1):49–57. [PubMed] [Google Scholar]
- 68.Tsatsoulis A, Fountoulakis S. The protective role of exercise on stress system dysregulation and comorbidities. Ann N Y Acad Sci. 2006;1083(1):196–213. doi: 10.1196/annals.1367.020. [DOI] [PubMed] [Google Scholar]
- 69.Kim EJ, Dimsdale JE. The effect of psychosocial stress on sleep: a review of polysomnographic evidence. Behav Sleep Med. 2007;5(4):256–278. doi: 10.1080/15402000701557383. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Jeffreys M, Capehart B, Friedman MJ. Pharmacotherapy for posttraumatic stress disorder: review with clinical applications. J Rehabil Res Dev. 2012;49(5):703–715. doi: 10.1682/jrrd.2011.09.0183. [DOI] [PubMed] [Google Scholar]
- 71.Stein DJ, Ipser JC, Seedat S. Pharmacotherapy for posttraumatic stress disorder (PTSD) Cochrane Database Syst Rev. 2006;(1):CD002795. doi: 10.1002/14651858.CD002795.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Ravindran LN, Stein MB. Pharmacotherapy of PTSD: premises, principles, and priorities. Brain Res. 2009;1293:24–39. doi: 10.1016/j.brainres.2009.03.037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Ipser JC, Stein DJ. Evidence-based pharmacotherapy of posttraumatic stress disorder (PTSD) Int J Neuropsychopharmacol. 2012;15(6):825–840. doi: 10.1017/S1461145711001209. [DOI] [PubMed] [Google Scholar]
- 74.Charney DS, Deutch AY, Krystal JH, et al. Psychobiologic mechanisms of posttraumatic stress disorder. Arch Gen Psychiatry. 1993;50(4):295–305. doi: 10.1001/archpsyc.1993.01820160064008. [DOI] [PubMed] [Google Scholar]
- 75.Southwick SM, Krystal JH, Morgan CA, et al. Abnormal noradrenergic function in posttraumatic stress disorder. Arch Gen Psychiatry. 1993;50(4):266–274. doi: 10.1001/archpsyc.1993.01820160036003. [DOI] [PubMed] [Google Scholar]
- 76.Pellejero T, Monti JM, Baglietto J, et al. Effects of methoxamine and alpha-adrenoceptor antagonists, prazosin and yohimbine, on the sleep-wake cycle of the rat. Sleep. 1984;7(4):365–372. doi: 10.1093/sleep/7.4.365. [DOI] [PubMed] [Google Scholar]
- 77.Southwick SM, Vythilingam M, Charney DS. The psychobiology of depression and resilience to stress: implications for prevention and treatment. Annu Rev Clin Psychol. 2005;1(1):255–291. doi: 10.1146/annurev.clinpsy.1.102803.143948. [DOI] [PubMed] [Google Scholar]
- 78.Germain A, Nofzinger EA, Kupfer DJ, et al. Neurobiology of non-REM sleep in depression: further evidence for hypofrontality and thalamic dysregulation. Am J Psychiatry. 2004;161(10):1856–1863. doi: 10.1176/ajp.161.10.1856. [DOI] [PubMed] [Google Scholar]
- 79.van Minnen A, Arntz A, Keijsers GP. Prolonged exposure in patients with chronic PTSD: predictors of treatment outcome and dropout. Behav Res Ther. 2002;40(4):439–457. doi: 10.1016/s0005-7967(01)00024-9. [DOI] [PubMed] [Google Scholar]
- 80.Kushida CA, Littner MR, Morgenthaler T, et al. Practice parameters for the indications for polysomnography and related procedures: an update for 2005. Sleep. 2005;28(4):499–521. doi: 10.1093/sleep/28.4.499. [DOI] [PubMed] [Google Scholar]
- 81.Aurora RN, Kristo DA, Bista SR, et al. American Academy of Sleep Medicine. The treatment of restless legs syndrome and periodic limb movement disorder in adults: an update for 2012: practice parameters with an evidence-based systematic review and meta-analyses: an American Academy of Sleep Medicine Clinical Practice Guideline. Sleep. 2012;35(8):1039–1062. doi: 10.5665/sleep.1988. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Dijk DJ, Edgar DM. Circadian and homeostatic control of wakefulness and sleep. In: Turek FW, Zee PC, editors. Regulation of Sleep and Circadian Rhythms. New York, NY: Marcel Dekker; 1999. pp. 111–147. [Google Scholar]