Abstract
Introduction:
The management of patients with large impacted upper ureteral stones is difficult; there is no standard treatment. We compared the outcomes of percutaneous nephrolithotomy (PCNL) and ureteroscopic lithotripsy (UL) to treat large (≥1.5 cm), impacted, upper ureteral stones.
Methods:
In total, 86 patients with large impacted upper ureteral stones were included in this study. Of these patients 41 underwent UL and 45 underwent PCNL. The inclusion criteria were: longest diameter of stone ≥1.5 cm, the localization of stone between the lower border of L4 spine and ureteropelvic junction and impacted stone.
Results:
In the UL group, we were unable to reach the stone in 3 patients because of ureteral stricture and edema despite balloon dilation. Of these 3 patients, we were unable to optimally visualize the stone in 2 patients due to bleeding and mucosal injury following balloon dilation. The stricture was too firm and could not be passed in the third patient. Also in the UL group, 15 patients had stones or big fragments which migrated into the renal collecting system. In the PCNL group, 21 patients had concurrent renal stones <1 cm and stones were successfully removed in all patients. No statistically significant difference was found between groups in terms of operation time. Mean hospital stay was significantly shorter in the UL group. Success rates were 82.3% in the UL group and 97.6% in the PCNL group (p = 0.001).
Conclusion:
The recent study confirms that PCNL is a safe and effective minimally invasive procedure with acceptable complication rates in the treatment of patients with large, impacted upper ureteral stones.
Introduction
The management of patients with large impacted upper ureteral stones is difficult and currently there is no standard treatment. Since the introduction of shock wave lithotripsy (SWL) in 1980, it has been the first-line treatment for most renal and ureteral stones.1 However, the success rate of SWL decreases in patients with impacted upper ureteral stones ≥1.5 cm.2 Ureteroscopic lithotripsy (UL) has become the preferred surgical method for most patients and surgeons due to relatively lower morbidity and shorter hospital stay. However, the success rate of UL decreases in patients with stones larger than 1 cm in diameter.3 Recently open surgery and laparoscopic procedures are rarely required to surgically manage ureteral stones. Percutaneous nephrolithotomy (PCNL) and antegrade lithotripsy are effective, minimally invasive options to surgically manage large upper ureteral stones, with reported stone-free rates between 85% and 100%.4,5
In this study we evaluated the outcomes of PCNL and UL in the treatment of large (≥1.5 cm), impacted, upper ureteral stones.
Methods
Between January 2006 and December 2013, 86 patients with large, impacted upper ureteral stones were included in this study. Of these, 41 underwent UL and 45 underwent PCNL. The demographical data and operation charecteristics of patients were retrospectively reviewed from the electronic records of the hospital. The number of patients who received each treatment over the years did not vary much (Fig. 1). The inclusion criteria were as follows; longest diameter of stone ≥1.5 cm, the localization of stone between the lower border of L4 spine and ureteropelvic junction, and impacted stone. Impacted stone was defined as the stone that did not allow any passage at contrast graphies, stayed at the same localization for more than 1 month and which resulted in dilation in the collecting system. All patients were informed about the procedures preoperatively and the surgical choice was made by the patient with counselling from the surgeon. Patients who had a non-functioning kidney and concurrent renal stones >1 cm were excluded from the study. In the PCNL group, 18 patients had a SWL history and 12 had past ipsilateral renal surgery; in the UL group, 6 had SWL and 10 had past ipsilateral renal surgery. The mean stone burden was 314 ± 64 mm2 in the PCNL group and 261 ± 47 mm2 in the UL group.
Fig. 1.
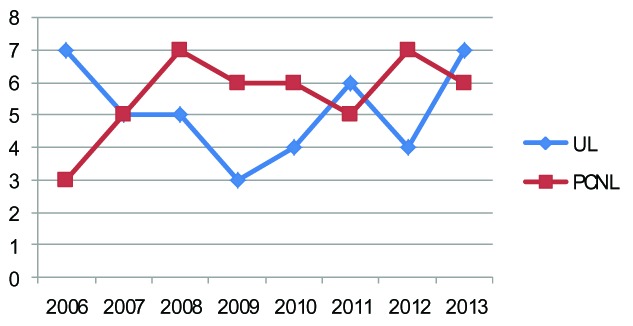
Number of patients who received either treatment over the years. PCNL: percutaneous nephrolithotomy; UL: ureteroscopic lithotomy.
UL was performed under spinal or general anaesthesia using a 8.5/9.8-F semirigid ureterorenoscopy device (Richard Wolf, Knittlingen, Germany). A 1000-µm Holmium-Yag laser (Dornier Medical Systems, Germany) was used for lithotripsy. The residual fragments were extracted using a basket catheter or grasping forceps. In cases of stone migration or big fragments into the renal collecting system, flexible ureteroscopy and laser lithotripsy were performed using the device URF type P5 (Olympus Corp.,Tokyo, Japan). A double-J stent was inserted in patients with mucosal injury, tissue edema, or ureteral stricture. An ureteral catheter was placed in the remaining patients and removed on postoperative day 1 with the urethral catheter.
All PCNLs were performed under general anesthesia. An open-ended 6-Fr ureteral catheter was placed using a cystoscope in the lithotomy position. The patient was then turned prone. Percutaneous access was performed using an 18-gauge needle under fluoroscopic guidance. Middle or upper calyx access was preferred according to the appropriate infidibulopelvic angle and relation to the ribs. A guidewire was then inserted into the collecting system and the tract was dilated using Amplatz dilators until a 28-Fr Amplatz sheath could be placed. Nephroscopy was performed under low pressure and stones were disintegrated using pneumatic or laser lithotripsy. The stone fragments were removed with forceps. A 14-Fr nephrostomy tube was placed at the end of the procedure if necessary. Nephrostomy catheter was removed on postoperative day 1. In patients with mucosal injury, edema, or ureteral stricture, a double-J stent was inserted.
On postoperative month 1, follow-up was done with non-contrast computed tomographt. Patients were accepted as stone free when no or ≤4 mm residual stones existed.
The two groups were compared according to success rates, perioperative outcomes, and complication rates. The procedure was deemed unsuccessful when the stone could not be reached in a single session and when residual stone ≥4 mm was detected at the 1-month postoperative visit.
Data were statistically analyzed using Mann-Whitney U test, chi-square test, and Fisher’s exact test with SPSS version 11.0 (SPSS Inc., Chicago, IL). Statistical significance was set at p < 0.05.
Results
The groups were similar in terms of mean age, mean pre-operative creatinine, failed SWL history, past ipsilateral renal surgery, and mean stone burden (Table 1).
Table 1.
Demographic characteristics and outcomes of the patients in both groups
| UL (n = 41) | PCNL (n = 45) | p value | |
|---|---|---|---|
|
| |||
| M/F ratio, n | 27/18 | 22/19 | 0.553 |
| Age (years), mean ± SD | 42.1 ± 14.9 | 44.7 ± 16.3 | 0.855 |
| Preoperative serum creatinine (mg/dL), mean ± SD | 1.14 ± 0.25 | 1.07 ± 0.31 | 0.144 |
| Stone burden (mm2), mean ± SD | 261 ± 47 | 314 ± 64 | 0.267 |
| Operation time (min), mean ± SD | 92 ± 32.5 | 107 ± 39.5 | 0.123 |
| Hospital stay (days), mean ± SD | 1.8 ± 1.0 | 4.3 ± 1.6 | 0.001 |
| Past ipsilateral renal surgery, % | 22.2 | 14.6 | 0.366 |
| Failed SWL history, % | 26.6 | 43.9 | 0.094 |
| Stone-free rate, % | 82.9 | 97.8 | 0.025 |
M: male; F: female; SD: standard deviation; SWL: shock wave lithotripsy; PCNL: percutaneous nephrolithotomy; UL: ureteroscopic lithotomy.
In the UL group, the stone could not be reached in 3 patients because of ureteral stricture and edema despite balloon dilation. Of these 3 patients, we were unable to optimally visualize the stone in 2 patients due to bleeding and mucosal injury following balloon dilation. The stricture was too firm and could not be passed in the third patient. Also of the 41 patients in the UL group, 15 had stones or big fragments which migrated into the renal collecting system. In 13 of these 15 patients, retrograde intrarenal surgery and laser lithotripsy were performed successfully using a flexible ureteroscope in the same session; in these 13, a double-J stent was inserted in patients who underwent retrograde intrarenal surgery. In the remaining 2 patients, a double-J stent was inserted and SWL was performed. A double-J stent was inserted in 14 patients who had mucosal injury and/or edema. The stents were removed on an outpatient basis 3 weeks postoperatively. In 5 patients, fever >38°C was encountered and controlled with antibiotics (Table 2).
Table 2.
Intraoperative characteristics and complications
|
UL n (%) |
PCNL n (%) |
|
|---|---|---|
|
| ||
| Fail to reach the stone | 3 (7.3) | 0 |
| Mucosal injury | 8 (19.5) | 2 (4.4) |
| Stone migration | 15 (36.6) | 0 |
| D-J insertion | 29 (70.7) | 17 (37.8) |
D-J: double J stent; PCNL: percutaneous nephrolithotomy; UL: ureteroscopic lithotomy.
In the PCNL group, 21 patients had concurrent renal stones <1 cm and stones were successfully removed in all patients. Upper calyx and middle calyx access were performed in 8 and 37 patients, respectively. In 17 patients, tubeless PCNL was applied and a double-J stent was inserted. None of the patients experienced neighbour organ injury or prolonged extravasation. Tranfusion was only required in 1 patient. Six patients experienced fever >38°C that was controlled with antibiotics. Postoperative complications were classified according to Clavien system (Table 3).
Table 3.
Postoperative complications by Clavien grade
| Clavien classification |
UL n (%) |
PCNL n (%) |
|---|---|---|
| Grade 0 | 34 (83) | 35 (78) |
| Grade 1 | 2 (5) | 3 (6.7) |
| Grade 2 | 5 (12) | 7 (15) |
| Grade 3 | 0 | 0 |
| Grade 4 | 0 | 0 |
| Grade 5 | 0 | 0 |
PCNL: percutaneous nephrolithotomy; UL: ureteroscopic lithotomy.
No statistically significant difference was found between groups in terms of operation time. However, the mean operation time was significantly shorter in patients whose stones were successfully managed in a single session without the need for flexible ureteroscopy. The mean hospital stay was significantly shorter in the UL group. At 1-month postoperatively, clinically significant residual fragments were detected in 2 patients in the UL group and 1 patient in the PCNL group. Success rates were 82.9% and 97.8% in the UL and PCNL groups, respectively (p = 0.001) (Table 1).
Discussion
Large, impacted upper ureteral stones may result in hydronephrosis and life-threatening conditions, including pyonephrosis and end-stage renal failure in the long term.
The success rates of SWL in proximal ureteral stones are between 57% and 96%.6,7 The factors that negatively affect success rates include stone diameter >1 cm, hydronephrosis degree, and brand of SWL.2,3 SWL is popular as a minimally invasive method that can be performed on an outpatient basis; however, severe complications, such as renal injury, subcapsular hematoma and renal scarring, are rare.8,9
The main reasons for the failure of UL in the treatment of impacted ureteral stones are migration of stones or big fragments into the renal collecting system and the difficulty to reach the stones. The edematous and inflamated mucosa surronding and partly covering the stone or fibroepithelial polyp results impede visualization of the stone and make it difficult to perform the lithotripsy.10,11 The increment of irrigation fluid pressure to obtain a clear image may result in stone migration into the renal collecting system.
Sen and colleagues reported that stone migration can be successfully prevented by using Stone Cone (Boston Scientific, Natick, MA) or Accordion (PercSys, Palo Alto, CA) in upper ureteral stones during UL.12 However, it is usually not possible to pass the guidewire behind the stone in impacted stones; repeated manipulation may cause mucosal injury. In our study, in 15 of the patients in the UL group (33 %), retrograde intrarenal surgery was performed as a second procedure because of stone migration or large fragments into the renal collecting system. These cases were also deemed successful. The success rates of UL in the treatment of upper ureteral stones >1 cm were between 77% and 81%.3 Our success rate was 82.9% in this study and consistent with previous reports.
Since its introduction in 1980, PCNL has changed the management of renal stones.13 Recently PCNL has been the preferred method to treat stones >2 cm.3 PCNL is also a good alternative to manage upper ureteral stones >1.5 cm with high stone-free rates. Moreover, it is possible to treat concurrent renal stones in the same session. The success rates of PCNL to treat upper ureteral stones >1.5 cm are between 85% and 100%.3,14,15 In our current study, the success rate was 97.8% in PCNL group.
Tubeless PCNL in select patients can significantly decrease postoperative pain scores and hospitalization time.16 In our study, we performed tubeless PCNL in 17 patients. Of these patients, 4 had a double-J stent insertion, 7 a ureteral catheter insertaion and the remaining 6 were totally tubeless. Common postoperative complications after PCNL were bleeding and fever. Studies found that transfusion is required in 2% to 5% of patients and arterial embolization is rarely required.17 In our study, only 1 patient in the PCNL group required a blood transfusion and none required arterial embolization.
Even though most of the previous studies concluded that the operation time was significantly shorter in UL compared to PCNL in the management of upper ureteral stones,18 our data do not support these findings. The migration of stones or large particles into the renal collecting system is not rare during UL; in these cases, it is necessary to continue with flexible ureteroscopy. These secondary interventions prolong the operation time significantly.
Currently, patients undergoing surgery expect to return to work and daily activities soon after. Patients undergoing UL had lower analgesic requirement, shorter hospital stay, and shorter interval to return to normal activities compared to the percutaneous approach.19,20 In our study, the mean hospital stay was significantly lower in the UL group.
Ozturk and colleagues compared SWL, retrograde intrarenal surgery and laparoscopic ureterolithotomy to treat 1- to 2-cm upper ureteral stones; they concluded that laparoscopic ureterolithotomy is superior to other modalities.21 However in the study by Ozturk and colleagues,21 it was not noted whether stones were impacted. Although stone-free rates with laparoscopic ureterolithotomy were higher, laparoscopic ureterolithotomy should not be considered a first-line treatment because recovery time is longer, complication rates higher and the procedure more invasive compared to SWL and UL.22–24 Laparoscopic ureterolithotomy may be an alternative to open surgery in patients with failed endourological interventions and SWL.
The limitations of our study were its retrospective design and lack of randomization. Also patient satisfaction was not evaluated since the primary goal of our was to evaluate stone-free rates and procedure-related outcomes.
Conclusion
Although hospital stay in the PCNL group was longer compared to UL, PCNL has lower stone migration and re-treatment rates. Our study confirmed that PCNL is a safe and effective procedure with higher stone-free rates and acceptable complication rates to treat patients with large, impacted upper ureteral stones.
Footnotes
Competing interests: Authors declare no competing financial or personal interests.
This paper has been peer-reviewed.
References
- 1.Chaussy C, Schuller J, Schmiedt E, et al. Extracorporeal shock-wave lithotripsy (ESWL) for treatment of urolithiasis. Urology. 1984;23:59–66. doi: 10.1016/0090-4295(84)90243-7. [DOI] [PubMed] [Google Scholar]
- 2.Lee YH, Tsai JY, Jiaan BP, et al. Prospective randomized trial comparing shock wave lithotripsy and ureteroscopic lithotripsy for management of large upper third ureteral stones. Urology. 2006;67:480–4. doi: 10.1016/j.urology.2005.09.067. [DOI] [PubMed] [Google Scholar]
- 3.Turk C, Knoll T, Petrik A, et al. Guidelines on urolithiasis. European Association of Urology. 2014. http://www.uroweb.org/gls/pdf/22%20Urolithiasis_LR.pdf. Accessed February 25, 2015.
- 4.Kumar V, Ahlawat R, Banjeree GK, et al. Percutenous nephrolithopaxy: The best bet to clear large bulk impacted upper ureteral calculi. Arch Esp Urol. 1996;49:86–91. [PubMed] [Google Scholar]
- 5.Sun X, Xia S, Lu J, et al. Treatment of large impacted proksimal ureteral stones: Randomized comparison of percutenous antegrade ureterolithotripsy versus retrograde ureterolithotripsy. J Endourol. 2008;22:913–7. doi: 10.1089/end.2007.0230. [DOI] [PubMed] [Google Scholar]
- 6.Segura JW, Preminger GM, Assimos DG, et al. Ureteral stones clinical guidelines panel summary report on the management of ureteral calculi. J Urol. 1997;158:1915–21. doi: 10.1016/S0022-5347(01)64173-9. [DOI] [PubMed] [Google Scholar]
- 7.Liong ML, Clayman RV, Gittes RF, et al. Treatment options for proximal ureteral urolithiasis: Review and recommendations. J Urol. 1989;141:504–9. doi: 10.1016/s0022-5347(17)40874-3. [DOI] [PubMed] [Google Scholar]
- 8.McAteer JA, Evan AP. The acute and long-term adverse effects of shock wave lithotripsy. Semin Nephrol. 2008;28:200–13. doi: 10.1016/j.semnephrol.2008.01.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Handa RK, Evan AP. A chronic outcome of shock wave lithotripsy is parenchymal fibrosis. Urol Res. 2010;38:301–5. doi: 10.1007/s00240-010-0297-y. [DOI] [PubMed] [Google Scholar]
- 10.Seitz C, Tanovic E, Kikic Z, et al. Impact of stone size, location, composition, impaction and hydronephrosis on the efficacy of holmium: YAG-laser ureterolithotripsy. Eur Urol. 2007;52:1751–9. doi: 10.1016/j.eururo.2007.04.029. [DOI] [PubMed] [Google Scholar]
- 11.Leijte JA, Oddens JR, Lock TM. Holmium laser lithotripsy for ureteral calculi: Predictive factors for complications and success. J Endourol. 2008;22:257–60. doi: 10.1089/end.2007.0299. [DOI] [PubMed] [Google Scholar]
- 12.Sen H, Bayrak O, Erturhan S, et al. Comparing of different methods for prevention stone migration during ureteroscopic lithotripsy. Urol Int. 2014;92:334–8. doi: 10.1159/000351002. . Epub 2013 Jul 4. [DOI] [PubMed] [Google Scholar]
- 13.LeRoy AJ, May GR, Bender CE, et al. Percutaneous nephrostomy for stone removal. Radiology. 1984;151:607–12. doi: 10.1148/radiology.151.3.6718717. [DOI] [PubMed] [Google Scholar]
- 14.Xiao-jian G, Lin LJ, Yan X. Treatment of large impacted proksimal ureteral stones: Randomized comparison of minimally invasive percutenous antegrade ureterolithotripsy versus retrograde ureterolithotripsy. World J Urol. 2013;31:1605–10. doi: 10.1007/s00345-013-1026-2. [DOI] [PubMed] [Google Scholar]
- 15.Juan YS, Shen JT, Li CC, et al. Comparison of percutaneous nephrolithotomy and ureteroscopic lithotripsy in the management of impacted, large, proximal ureteral stones. Kaohsiung J Med Sci. 2008;24:204–9. doi: 10.1016/S1607-551X(08)70118-9. [DOI] [PubMed] [Google Scholar]
- 16.Garofalo M, Pultrone CV, Schiavina R, et al. Tubeless procedure reduces hospitalization and pain after percutenous nephrolithotomy: Results of a multivariable analysis. Urolithiasis. 2013;41:347–53. doi: 10.1007/s00240-013-0565-8. [DOI] [PubMed] [Google Scholar]
- 17.Osman M, Wendt-Nordahl G, Heger K, et al. Percutenous nephrolithotomy with ultrasonography-guided renal access: Experience from over 300 cases. BJU Int. 2005;96:875–8. doi: 10.1111/j.1464-410X.2005.05749.x. [DOI] [PubMed] [Google Scholar]
- 18.Zhu H, Ye X, Xiao X, et al. Retrograde, antegrade and laparoscopic approaches tot he management of large upper ureteral stones after shockwave lithotripsy failure: A four-year retrospective study. J Endourol. 2014;28:100–3. doi: 10.1089/end.2013.0391. [DOI] [PubMed] [Google Scholar]
- 19.Moufid K, Abbaka N, Touiti D, et al. Large impacted upper ureteral calculi: A comparative study between retrograde ureterolithotripsy and percutaneous antegrade ureterolithotripsy in the modified lateral position. Urol Ann. 2013;5:140–6. doi: 10.4103/0974-7796.115729. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Sun X, Xia S, Lu J, et al. Treatment of large impacted proximal ureteral stones: Randomized comparison of percutaneous antegrade ureterolithotripsy versus retrograde ureterolithotripsy. J Endourol. 2008;22:913–7. doi: 10.1089/end.2007.0230. [DOI] [PubMed] [Google Scholar]
- 21.Ozturk MD, Sener NC, Goktug HN, et al. The comparison of laparoscopy, shock wave lithotripsy and retrograde intrarenal surgery for large proximal ureteral stones. Can Urol Assoc J. 2013;7:673–6. doi: 10.5489/cuaj.346. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Fan T, Xian P, Yang L, et al. Experience and learning curve of retroperitoneal laparoscopic ureterolithotomy for upper ureteral calculi. J Endourol. 2009;23:1867–70. doi: 10.1089/end.2008.0536. [DOI] [PubMed] [Google Scholar]
- 23.Khaladkar S, Modi J, Bhansali M, et al. Which ist he best option to treat large (>1.5 cm) midureteric calculi? J Laparoendosc Adv Surg Tech A. 2009;19:501–4. doi: 10.1089/lap.2008.0299. [DOI] [PubMed] [Google Scholar]
- 24.Jeong BC, Park HK, Byeon SS, et al. Retroperitoneal laparoscopic ureterolithotomy for upper ureter stones. J Korean Med Sci. 2006;21:441–4. doi: 10.3346/jkms.2006.21.3.441. [DOI] [PMC free article] [PubMed] [Google Scholar]


