Abstract
Epididymo-orchitis rarely leads to abscess formation and global testicular infarction/loss, particularly in the setting of appropriate antibiotic therapy. The imaging modality used when monitoring for testicular ischemia is ultrasonography. However, as described in the literature, testicular pathology may not be evident on routine imaging. We describe two cases of recurrent bacterial epididymo-orchitis, complicated by testicular abscess resulting in testicular infarction. This rare, nevertheless significant, complication occurred in both patients despite receiving appropriate extended antibiotic therapy. Both cases demonstrate the limitations of ultrasonography alone, suggesting that a high level of clinical suspicion must be maintained when ultrasound evaluation proves to be inconsistent with the clinical presentation. These cases demonstrate the importance of monitoring for warning signs of ischemia, as early recognition may lead to reperfusion interventions and ultimately testicular salvage.
Case report
There is little literature describing testicular infarction following bacterial epididymo-orchitis. With appropriate antibiotic therapy, epididymo-orchitis rarely leads to abscess formation, segmental testicular infarction, or global testicular infarction/loss.1,2 We describe two cases of recurrent bacterial epididymo-orchitis complicated by testicular abscess, resulting in testicular loss despite extended, appropriate antibiotic therapy.
Case 1
A 49-year-old HIV-positive male with no other significant medical history developed severe left-sided testicular pain and swelling associated with dysuria and macroscopic hematuria. He had a raised C-reactive protein level (380 mg/L [range: 0–5 mg/L]) and total white cell count (16 × 109/L [range: 3.9–12.7 × 109/L]). A mid-stream urine sample grew Escherichia coli sensitive to gentamicin, cephalexin, norfloxacin, and amoxicillin/clavulanic acid. Urine polymerase chain reaction (PCR) testing for N. gonorrhoeae and C. trachomatis was negative. An initial ultrasound excluded testicular torsion and demonstrated mild prostatomegaly; however, no voiding or cystoscopic studies were performed. The patient started oral trimethoprim 300 mg daily empirically, followed by a 2-week course of oral cephalexin 500 mg twice daily once susceptibilities were known.
The patient was readmitted to hospital 2 months later with recurrent left-sided epididymo-orchitis. A mid-stream urine again cultured E.coli with an identical anti-biogram to the previous isolate. Three days of empiric intravenous ceftriaxone 1 g daily were followed by a 6-week course of oral ciprofloxacin 750 mg twice daily on discharge. The patient made a full clinical recovery.
However, 7 months later, the patient presented with right-sided epididymo-orchitis that was confirmed with an ultra-sound. Both urine and blood cultures grew E. coli with an identical antibiogram to the previous isolates. This patient demonstrated good HIV-control, reflected in a robust CD4+ T-cell count (453/uL) and suppressed virus (HIV viral load <20 copies/mL). Intravenous ceftriaxone 1 g daily for 7 days resulted in substantial clinical improvement. On day 7 the patient developed worsening pain and a repeat ultrasound revealed an enlarged avascular right testicle.
An urgent orchidectomy was performed, with histology revealing an infarcted testis with localised abscess formation (Fig. 1). The patient completed another 6-week course of oral ciprofloxacin 750 mg twice daily with complete clinical response and remains well at this time.
Fig. 1.
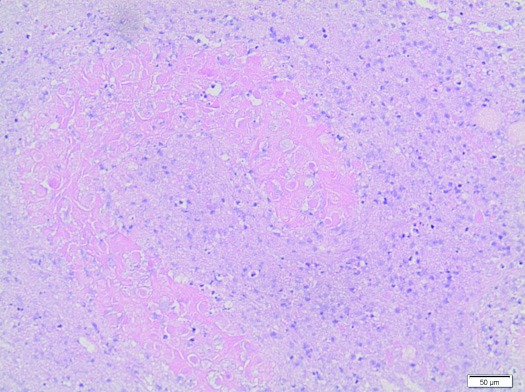
Histopathological findings of epididymoorchitis in Case 1: Infarcted seminiferous tubules associated with an acute inflammatory infiltrate; hematoxylin and eosin ×200.
Case 2
A 27-year-old man with a history of recurrent urinary tract infections was admitted to hospital with left-sided epididymo-orchitis, on a background of recently successfully treated Chlamydia trachomatis epididymo-orchitis. He had no other medical conditions.
The mid-stream urine demonstrated 101 × 106/L leucocytes (ref <10 × 106/L), but was culture-negative in the context of norfloxacin therapy previously started in the community. Urine PCR testing for Neisseria gonorrhoeae, Chlamydia trachomatis and syphilis serology were all negative. A renal tract ultrasound was normal, other than confirming left-sided-epididymo-orchitis. The patient received a single dose of 400 mg intravenous gentamicin with 4 days of intravenous ceftriaxone 1 g daily followed by 6 weeks of oral norfloxacin 400 mg twice daily on discharge from hospital. The patient received an additional single dose of 1 g oral azithromycin the following week, given his recent history of chlamydial epididymo-orchitis.
One week post-completion of all antibiotics, the patient developed recurrent, left-sided epididymo-orchitis. Urine culture and PCR testing were negative in the context of recent antibiotics. Empiric therapy consisted of intravenous ciprofloxacin 400 mg 8 hourly for 24 hours and a single dose of 1 g oral azithromycin. A rigid cystoscopy revealed no anatomical abnormality. An ultrasound revealed a small testicular abscess and reduced vascularity. Oral ciprofloxacin 500 mg twice daily was continued for 6 weeks in combination with oral doxycycline 100 mg twice daily for 2 weeks to cover for a possible chlamydial infection.
While still on ciprofloxacin, the patient underwent an ultrasound due to his recurrent testicular pain. This demonstrated an avascular left testicle, prompting subsequent orchidectomy. Histopathology showed a necrotising pyogenic abscess with secondary testicular infarction (Fig. 2). Tissue culture was positive for Klebsiella pneumonia that was sensitive to ciprofloxacin.
Fig. 2.
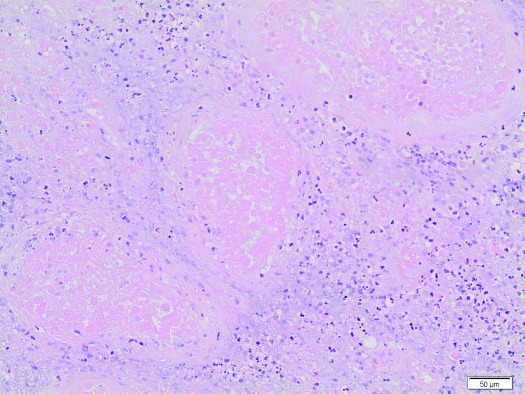
Histopathological findings of epididymoorchitis in Case 2: Infarcted seminiferous tubules associated with an acute inflammatory infiltrate, hematoxylin and eosin ×20.
Discussion
We describe two cases of testicular infarction requiring orchidectomy. Each followed bacterial epididymo-orchitis complicated by abscess formation despite extended, appropriate antibiotic therapy. These cases add to a small body of literature describing this rare, but serious complication (Table 1). Both cases demonstrate that testicular abscesses may not be evident on routine imaging, such as ultrasound. This is consistent with the literature, which demonstrates the potential for missed testicular pathology when investigated with ultrasonography alone.3 Contrast-enhanced magnetic resonance imaging (MRI) has been reported to provide additional support in evaluating indeterminate testicular pathology.
Table 1.
Reports of testicular infarction following bacterial epididymoorchitis
| Publication | Age | Medical history | Prior episodes* | Urine culture | Histopathology¥ | Antibiotics used (in order of use) | Antibiotic duration |
|---|---|---|---|---|---|---|---|
| Farber et al., 20135 | 58 | Diabetes mellitus | No | Escherichia coli | Indurated epididymis with infarcted testis. | Cef (IM), D (PO), L (IV), A (IV), G (IV), Ce (IV), Cef (IV) | 6 weeks |
| Chin et al., 19988 | 42 | Nil | No | Nil growth | Extensive thrombosis involving numerous dilated veins with concurrent epididymitis. | Not specified | Not specified |
| Eisner et al., 19919 | 65 | Unknown | No | Pseudomonas aeruginosa | Bilateral infarcted testes with marked fibrosis. Extensive vascular thromboses involving numerous veins and arteries. | A (IV), G (IV), Cip (PO), T (IV) | At least 2 weeks |
| Yusuf et al., 20131 | 55 | Colorectal cancer | No | Escherichia coli | Global ischemia with adjacent inflammatory change and multiple microabscesses. | Not specified | Not specified |
| Yusuf et al., 20131 | 64 | Diabetes mellitus Ischemic Heart Disease Hypertension | No | Not specified | Inflamed epididymis, multiple microabscesses and global testicular infarction. Thickened testicular vessels secondary to occlusion. | Not specified | At least 1 week |
| Sue et al., 19982 | 43 | Hepatitis C | No | Nil growth | Hemorrhagic necrotic infarction and chronic inflammation. | Cef (IV), G (IV). Q (PO), D (PO) | Not specified |
| Marks et al., 200910 | 50 | Nil | No | Escherichia coli | Acute and chronic epididymo-orchitis with hemorrhage and necrosis. Candida albicans grew on tissue culture. | Not specified | Not specified |
Episodes of epididymoorchitis.
Confirmed on histopathology +/− abscess. Cef: ceftriaxone; Cip: ciprofloxacin; G: gentamicin; D: doxycyline; A: ampicillin; T: tobramycin; Ce: cefuroxime; L: levofloxacin; IM: intramuscular; IV: intravenous; PO: oral.
Critical deprivation resulting in infarction is rare and may be secondary to cumulative ischemia from multiple mechanisms: inflammatory infiltration causing compression of the spermatic cord, thrombosis secondary to venous congestion and/or bacterial exotoxins.4–7 Prompt assessment and recognition of ischemia may lead to reperfusion interventions and ultimately testicular salvage.
Non-resolving infection despite appropriate antibiotic therapy, acute worsening in pain despite initial clinical improvement, spermatic cord thickening and tenderness, and recurrent epididymo-orchitis are all potential warning signs of ischemia7, and were evident in our cases.
Conclusion
In the setting of recurrent epididymo-orchitis, clinicians should be suspicious of a testicular abscess. This may not initially be evident on routine imaging, highlighting the value of additional modalities, such as MRI, when ultrasound evaluation proves to be inconclusive or inconsistent with the clinical presentation. These cases are a timely reminder about potential testicular loss following epidiymo-orchitis, even if appropriate antibiotic therapy is administered.
Footnotes
Competing interests: Authors declare no competing financial or personal interests.
This paper has been peer-reviewed.
References
- 1.Yusuf G, Sellars ME, Kooiman GG, et al. Global testicular infarction in the presence of epididymitis: Case series. JUM. 2013;32:175–80. doi: 10.7863/jum.2013.32.1.175. [DOI] [PubMed] [Google Scholar]
- 2.Sue SR, Pelucio M, Gibbs M. Testicular infarction in a patient with epididymitis. Acad Emerg Med. 1998;5:1128–30. doi: 10.1111/j.1553-2712.1998.tb02679.x. [DOI] [PubMed] [Google Scholar]
- 3.Serra AD, Hricak H, Coakley FV, et al. Inconclusive clinical and ultrasound evaluation of the scrotum: Impact of magnetic resonance imaging on patient management and cost. Urology. 1998;51:1018–21. doi: 10.1016/S0090-4295(98)00097-1. [DOI] [PubMed] [Google Scholar]
- 4.Desai KM, Gingell JC, Haworth JM. Fate of the testis following epididymitis: A clinical and ultrasound study. J R Soc Med. 1986;79:515–9. doi: 10.1177/014107688607900906. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Farber NJ, Slater RC, Maranchie JK. Multidrug resistant epididymitis progressing to testicular infarct and orchiectomy. Case Rep Urol. 2013;2013:645787. doi: 10.1155/2013/645787. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Lung PF, Jaffer OS, Sellars ME, et al. Contrast-enhanced ultrasound in the evaluation of focal testicular complications secondary to epididymitis. AJR Am J Roentgenol. 2012;199:W345–54. doi: 10.2214/AJR.11.7997. [DOI] [PubMed] [Google Scholar]
- 7.Hourihane DO. Infected infarcts of the testis: A study of 18 cases preceded by pyogenic epididymoorchitis. J Clin Pathol. 1970;23:668–75. doi: 10.1136/jcp.23.8.668. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Chin SC, Chen CY, Lee CC, et al. Giant arachnoid granulation mimicking dural sinus thrombosis in a boy with headache: MRI. Neuroradiology. 1998;40:181–3. doi: 10.1007/s002340050564. [DOI] [PubMed] [Google Scholar]
- 9.Eisner DJ, Goldman SM, Petronis J, et al. Bilateral testicular infarction caused by epididymitis. AJR Am J Roentgenol. 1991;157:517–9. doi: 10.2214/ajr.157.3.1872237. [DOI] [PubMed] [Google Scholar]
- 10.Marks R, McNeil K. Significance of reversal of diastolic blood flow in the evolution of testicular infarction as a complication of epididymo-orchitis. J Radiol Case Rep. 2009;3:21–5. doi: 10.3941/jrcr.v3i6.218. . Epub 2009 Jun 1. [DOI] [PMC free article] [PubMed] [Google Scholar]


