Key Points
NF-κB differentially regulates CXCR4 expression on naïve and pathogenic CD8+ T cells.
CXCR4 expression on pathogenic T cells facilitates their trafficking to the BM in a mouse model of AA.
Abstract
Aplastic anemia (AA) is a disease characterized by T-cell–mediated destruction of bone marrow (BM) hematopoietic stem and progenitor cells. Physiologically, T cells migrate to the BM in response to chemokines, such as SDF-1α, the ligand for CXCR4. However, how T cells traffic to the BM in AA is poorly understood. CXCR4 is aberrantly expressed in immune-mediated diseases and its regulation by nuclear factor-κB (NF-κB) in cancer models is well documented. In this study, we show that CXCR4 is highly expressed on BM-infiltrating CD4+ and CD8+ T cells in a mouse model of AA. Inhibiting CXCR4 in AA mice, using CXCR4−/− splenocytes or AMD3100, significantly reduced BM infiltration of T cells. We also report that NF-κB occupancy at the CXCR4 promoter is enhanced in BM-infiltrating CD8+ T cells of AA mice. Moreover, inhibiting NF-κB signaling in AA mice using Bay11 or dehydroxymethylepoxyquinomicin, or transferring p50−/− splenocytes, decreased CXCR4 expression on CD8+ T cells, significantly reduced BM infiltration of T cells, and strongly attenuated disease symptoms. Remarkably, therapeutic administration of Bay11 significantly extended survival of AA mice. Overall, we demonstrate that CXCR4 mediates migration of pathogenic T cells to the BM in AA mice, and inhibiting NF-κB signaling may represent a novel therapeutic approach to treating AA.
Introduction
Aplastic anemia (AA) is a rare bone marrow failure (BMF) disease characterized by peripheral pancytopenia and hypoplastic bone marrow (BM).1 Most cases of acquired AA are idiopathic occurring both in children and adults, with roughly equal frequency in both genders.1,2 Studies of AA patients and animal models of BMF suggest acquired AA is an immune-mediated disease.3,4 Aberrant responses mediated by T helper type-1 (Th1), Th17, and cytotoxic CD8+ T cells, together with impaired function of regulatory T cells,5-10 culminate in BM destruction. Although the pathophysiology of AA is well defined, the molecular mechanisms responsible for T-cell infiltration into the BM during AA progression are poorly understood.
Small populations of mature CD4+ and CD8+ T cells reside in the BM. It is a priming site for antigen-specific T cells,11-13 as well as a homing site for memory T cells.14-16 Physiologically, T cells migrate to the BM in response to chemokines, such as stromal-cell derived factor-1α (SDF-1α) which is highly expressed by BM stromal cells.17,18 SDF-1α, also known as CXCL12, is the natural ligand for the chemokine receptor, CXCR4.19 SDF-1α–CXCR4 interactions initiate multiple signaling pathways that augment T cell co-stimulation, proliferation, cytokine production, migration, and survival.20-25 In T cells, activation through the T-cell receptor, polyclonal stimulation, SDF-1α interaction, and IFN-γ are stimuli that downregulate CXCR4, whereas signaling through IL-2, IL-4, IL-7, and IL-15 upregulates its expression.26-31
The nuclear factor-κB (NF-κB) family of transcription factors consists of five subunits, RelA (p65), RelB, c-Rel, NF-κB1 (p50), and NF-κB2 (p52), that function as homo- or heterodimers. NF-κB signaling plays a central role in T-cell activation, proliferation, differentiation, and survival.32
Dysregulated CXCR4 and NF-κB signaling pathways contribute to disease pathology in multiple immune-mediated diseases including multiple sclerosis, systemic lupus erythematosus, rheumatoid arthritis, and type 1 diabetes.33-41 Both signaling pathways have also been associated with hematopoietic and nonhematopoietic malignancies.42-44 Moreover, NF-κB–mediated regulation of CXCR4 expression and function in breast, pancreatic, gastric, prostatic, and ovarian cancers is well documented.45-51 However, the contribution of CXCR4 and NF-κB signaling pathways to the pathology of acquired AA has not previously been explored.
Through pharmacologic and genetic approaches, we demonstrate that CXCR4 mediates migration of pathogenic T cells to the BM in an established mouse model of immune-mediated AA.5 We further show that CXCR4 is differentially regulated by NF-κB in naïve and BM-infiltrating CD8+ T cells. Inhibiting NF-κB signaling in AA mice decreased CXCR4 expression on BM-infiltrating CD8+ T cells, significantly reduced BM infiltration of T cells, and strongly attenuated disease symptoms. Finally, we show that therapeutic inhibition of NF-κB signaling significantly prolonged the survival of AA mice.
Materials and methods
Animals
Animal studies were conducted in compliance with the Institutional Animal Care and Use Committee of the University of Massachusetts Amherst. F1 progeny were obtained by crossing BALB/c females with C57BL/6 males. Conditional Cxcr4 knockout (CXCR4−/−) mice were generated on a C57BL/6J background by crossing Cxcr4fl/fl mice (B6.129P2-Cxcr4tm2Yzo/J) to Mx1-cre+/− mice (B6.Cg-Tg[Mx1-cre]1Cgn/J). Cxcr4fl/flMx1-cre+/− (CXCR4−/−), Cxcr4fl/flMx1-cre−/−, and Mx1-cre+/− mice were administered polyI:polyC (12 to 15 μg/g body weight; Imgenex, San Diego, CA) via IP injection every other day for 5 days. Mice were rested for 3 weeks and then used as a source of donor splenocytes. p50 knockout (B6.Cg-Nfkb1tm1Bal/J; p50−/−), BALB/c, C57BL/6, Cxcr4fl/fl, and Mx1-cre+/− parental strains were obtained from the Jackson Laboratory (Bar Harbor, ME). Mice between 7 to 12 weeks were used in experiments.
BMF induction and analyses
F1 progeny were irradiated (3Gy,137Cs source); 4 to 6 hours later, BMF was induced with 5 × 107 splenocytes (IP injection) from age- and gender-matched C57BL/6 (wild-type [WT] or knockout) donors.5 Mice were harvested on day +17. For survival studies, mice were humanely euthanized when they could no longer eat or drink. BM cells were flushed from tibias and femurs of legs using 5% fetal bovine serum (FBS)/phosphate-buffered saline (PBS). Splenocytes were passed through a 40 μM filter, red blood cells (RBCs) lysed with ACK buffer, and white blood cells (WBCs) enumerated using trypan blue exclusion. Circulating WBCs and RBCs were counted using a HemaTrue Hematology Analyzer (Heska). For quantitative real-time polymerase chain reaction (qRT-PCR) studies, T cells were isolated from spleens or BM of AA mice using anti-mouse CD4 and CD8 magnetic particles (BD Biosciences) and separated using the BD IMag system.
In vivo administration of CXCR4 and NF-κB inhibitors
For CXCR4 inhibition studies, mice were treated on day +7 postdisease induction with AMD3100 (5 mg/kg per day; Calbiochem) administered via IP injection continuing until day +16. Control mice received equivalent volumes of PBS. For NF-κB inhibition studies, mice were administered dehydroxymethylepoxyquinomicin (DHMEQ) (30 mg/kg per day; provided by A. Fauq) or Bay11-7085 (Bay11; 5 mg/kg every other day; Calbiochem) via IP injection, beginning 1 hour after disease induction and continuing until day +16 postdisease induction. Control mice received equivalent volumes of dimethylsulfoxide (DMSO). For survival studies, mice were given Bay11 via IP injection (5 mg/kg every other day) from days +7 to +17 postdisease induction, at which time treatment was discontinued. Control mice received equivalent volumes of DMSO.
Histology
On day +17 postdisease induction, sterna were harvested, fixed overnight in 10% neutral buffered formalin (VWR), decalcified for 48 hours in Cal-Rite (Richard-Allan Scientific), then preserved in 70% ethanol at 4°C until processed, paraffin-embedded, sectioned, and stained with hematoxylin and eosin.
Mixed lymphocyte reaction and chemotaxis assay
To generate BM-derived dendritic cells (BMDCs), BM cells from F1 progeny were cultured (106 cells/mL) in RPMI 1640 medium supplemented with 10% FBS (Gibco), 2 mM l-glutamine, 100 U/mL penicillin, 100 μg/mL streptomycin, and 20 ng/mL granulocyte macrophage colony-stimulating factor (R&D Systems), and incubated at 37°C with 5% CO2. On days 2 and 4 postculture, half the media was removed and replaced with fresh supplemented media. On day 6 postculture, nonadherent cells were harvested and cultured in fresh supplemented media for 2 additional days. For mixed leukocyte reaction, BMDCs were cocultured with bulk splenocytes (1:10 from age- and gender-matched C57BL/6 mice) in a 1:1 mixture of RPMI 1640 and Dulbecco’s modified Eagle medium supplemented with 10% FBS, 2 mM l-glutamine, 1 mM sodium pyruvate, 100 U/mL penicillin, and 100 μg/mL streptomycin in 96-well round-bottom plates and incubated at 37°C with 7% CO2 for 12 days. To inhibit NF-κB, 1 μM Bay11 or an equivalent volume of DMSO was added at time of plating. From days 6 to 12 postculture, nonadherent cells were harvested every other day, and CXCR4 expression on CD4+ and CD8+ T cells was analyzed by flow cytometry. On day 8 postculture, nonadherent cells were harvested to evaluate their chemotactic response to SDF-1α. Chemotaxis assays were performed in 24-well plate Transwell inserts (5 μm polycarbonate membrane, 6.5 mm insert; Corning Costar); 600 μl of RPMI with 10% FBS with or without 100 ng/mL of SDF-1α (R&D Systems) was added to wells and 0.5 × 106 cells in 0.1 μl of RPMI with 10% FBS were added to inserts, and incubated at 37°C with 5% CO2. After 3 hours, inserts were removed and migrated cells harvested from wells. CD4+ and CD8+ T cells were enumerated by flow cytometry. Results are expressed as chemotactic index (number of cells migrated into 100 ng/mL SDF-1α wells divided by number of cells migrated into 0 ng/mL SDF-1α wells). Media and supplements were from Lonza Group, unless otherwise specified.
Flow cytometry
Single-cell suspensions from spleens and BM were surface-stained with PerCP-conjugated anti-CD4 (RM4-5; BD Pharmingen), PE-Cy7-conjugated anti-CD8a (53-6.7; eBioscience), APC-conjugated anti-CXCR4 (2B11; eBioscience), APC-conjugated anti-CXCR7 (11G8; R&D Systems), APC-conjugated anti-CX3CR1 (polyclonal; R&D Systems), PE-conjugated anti-CCR5 (CTC5; R&D Systems), and PE-conjugated anti-CXCR3 (220803; R&D Systems). Samples were acquired on an LSRII flow cytometer and analyzed using FACSDiva acquisition software (Becton Dickinson). Analyses of fluorescence-activated cell sorter data were performed using FACSDiva or FloJo software (Tree Star, Ashland, OR).
Cytometric bead array
Plasma cytokine levels were determined using Th1/Th2 cytometric bead array kits (BD Biosciences) following the manufacturer’s protocol. Data were acquired on an LSRII flow cytometer and analyzed using FCAP array software (BD Biosciences).
RNA isolation and qRT-PCR
Total RNA was extracted using RNAqueous Kits (Ambion) according to the manufacturer’s protocol. RNA (1 μg) was reverse transcribed to complementary DNA using dNTPs (Roche), M-MuLV reverse transcriptase reaction buffer (New England Biolabs, Inc.), oligo-(dT)12–18 (Invitrogen), RNase inhibitor (Promega), and M-MuLV reverse transcriptase (New England Biolabs, Inc.) on a Mastercycler Gradient Thermal Cycler (Eppendorf). qRT-PCR was performed in duplicate with SYBR Premix Ex Taq (Takara Bio, Inc.) on a Stratagene Mx3000P quantitative PCR system (Agilent Technologies). Primer sequences were as follows: Cxcr4: forward, 5′-GAC TGG CAT AGT CGG CAA TG-3′; reverse, 5′-AGA AGG GGA GTG TGA TGA CAA A-3′; and Actb: forward, 5′-GGC TGT ATT CCC CTC CAT CG-3′; reverse, 5′-CCA GTT GGT AAC AAT GCC ATG T-3′. qRT-PCR conditions were as follows: 95°C for 1 minute, 95°C for 25 seconds, 62°C for 25 seconds (35 cycles), 95°C for 1 minute, 62°C for 1 minute, and 95°C for 30 seconds. Relative expression of Cxcr4 was determined using the 2−ΔΔCt method. Results are reported as fold-change in gene expression, normalized to Actb and relative to irradiation controls.
ChIP
Chromatin immunoprecipitation (ChIP) was performed as described.5 Briefly, cells were crosslinked with 1% formaldehyde, lysed in sodium dodecyl sulfate (SDS) lysis buffer (1% SDS, 10 mM EDTA, and 50 mM Tris, pH8.1), and sonicated with a Bioruptor Sonicator (Diagenode). Cell lysates were precleared overnight with 5 μg anti–c-Rel (clone C), anti–NF-κB p50 (clone C-19), normal rabbit IgG, or normal goat IgG at 4°C (all from Santa Cruz Biotechnology, Inc.). Protein–DNA complexes were recovered with ChIP-grade protein G agarose beads, washed, eluted with elution buffer (1% SDS, 0.1 M NaHCO3), and reverse crosslinked overnight at 65°C. DNA was purified by proteinase K digestion and extracted with QIAEX II gel extraction kit (QIAGEN). Two regions of the Cxcr4 promoter containing putative NF-κB p50 and c-Rel binding sites were amplified by PCR. Primer sets were as follows: primer set I (product size 185 bp) forward, 5′-GGC TGA CCT CCT CTT TGT CAT C-3′; reverse, 5′-TGT TGG TGG CGT GGA CAA TA-3′; and primer set II (product size 331 bp) forward, 5′-CAT CAG TCA GGG GGA TGA CA-3′; reverse, 5′-GAT GGA GAT CCA CTT GTG CA-3′. PCR conditions were 95°C for 2 minutes, 95°C for 30 seconds, 56°C for 30 seconds, 72°C for 1 minute (38 cycles), and 72°C for 5 minutes.
Statistical analysis
Results are the mean ± SEM. Statistical analyses were performed using GraphPad Prism 5.0 (GraphPad Software). P values were calculated using an unpaired two-tailed Student t test, one- or two-way analysis of variance (ANOVA) with post-tests as indicated. Survival curves were generated using the Kaplan–Meier method and survival differences were determined with a Mantel-Cox log-rank test. P values ≤ .05 were considered statistically significant.
Results
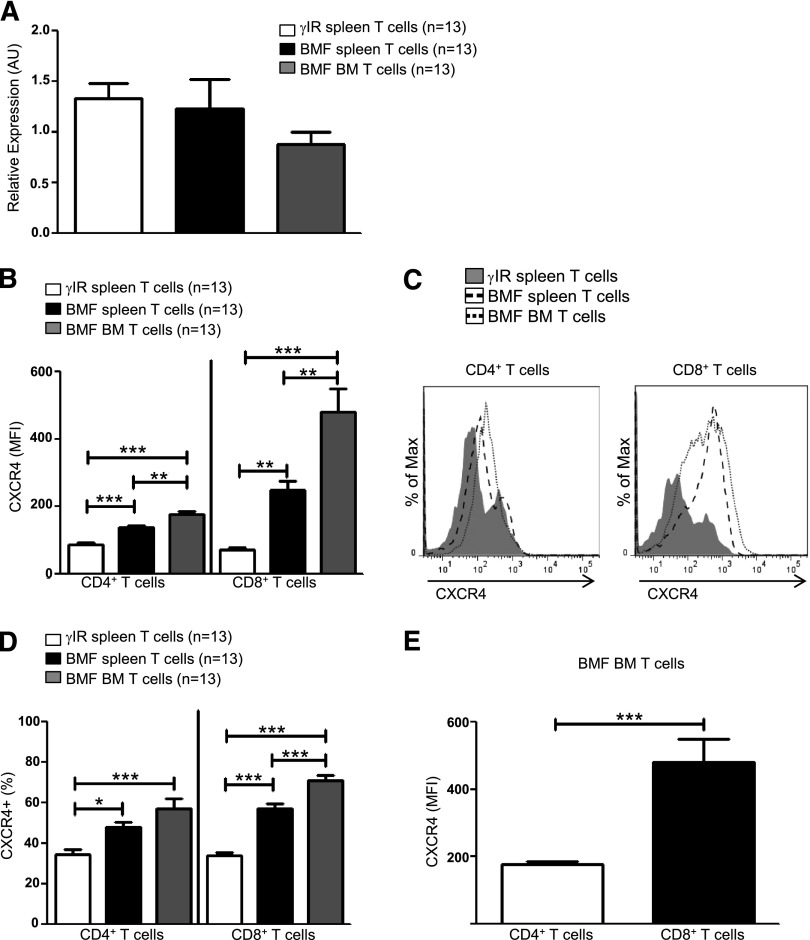
CXCR4 is highly expressed on T cells of AA mice
T cells use CXCR4–SDF-1α interactions to traffic to the BM during homeostatic processes,17,18 but how pathogenic T cells are targeted to the BM during AA is not well understood. Here, we sought to determine whether CXCR4 contributes to the pathogenesis of immune-mediated AA. Using a well-characterized, lymphocyte transfer mouse model of AA,5 we first assessed transcript and protein expression of CXCR4. Seventeen days postdisease induction, Cxcr4 transcripts in T cells from spleens and BM were expressed at similar levels both in AA mice and irradiation controls (Figure 1A); however, for many genes, there is only a modest correlation between messenger RNA levels and their translated proteins.52 When we further assessed protein levels, we found that the surface expression of CXCR4 was significantly higher on T cells isolated from spleens and BM of AA mice (Figure 1B-C), as were percentages of CXCR4+ T cells (Figure 1D), suggesting that posttranscriptional regulation of CXCR4 differs between control and pathogenic T cells. We further noted that CXCR4 was expressed more highly on a per cell basis on BM-infiltrating CD8+ T cells, compared with CD4+ T cells (Figure 1E).
Figure 1.
CXCR4 is highly expressed on T cells of AA mice. F1 hybrid mice were irradiated only (γIR control) or AA was induced with 5 × 107 WT C57BL/6 splenocytes. Mice were sacrificed on day +17 postdisease-induction and T cells were isolated. (A) Relative expression of Cxcr4 transcript levels in T cells from spleens (BMF spleen) and BM (BMF BM) of AA mice were determined by quantitative PCR and compared with expression in T cells of spleens (γIR spleen) from irradiation controls; n = 13 mice per group. (B) Median fluorescence intensity (MFI), a measure of CXCR4 protein expression, on spleen and BM T cells of AA mice was determined by flow cytometry and compared with expression on spleen T cells of irradiated controls; n = 13 mice per group. (C) Representative comparative histograms of CXCR4 MFI on T cells from spleens and BM from (B). (D) Percent CXCR4 positive T cells on T cells from spleens and BM of AA mice, compared with T cells isolated from spleens of irradiation controls; n = 13 mice per group. (E) Comparison of CXCR4 expression on BM-infiltrating CD4+ and CD8+ T cells of AA mice; n = 13 mice per group. Data represent the mean ± SEM, and were analyzed by one-way ANOVA plus Tukey post-test (A-B,D), or two-tailed unpaired Student t test (E). *P < .05; **P < .01; ***P < .001.
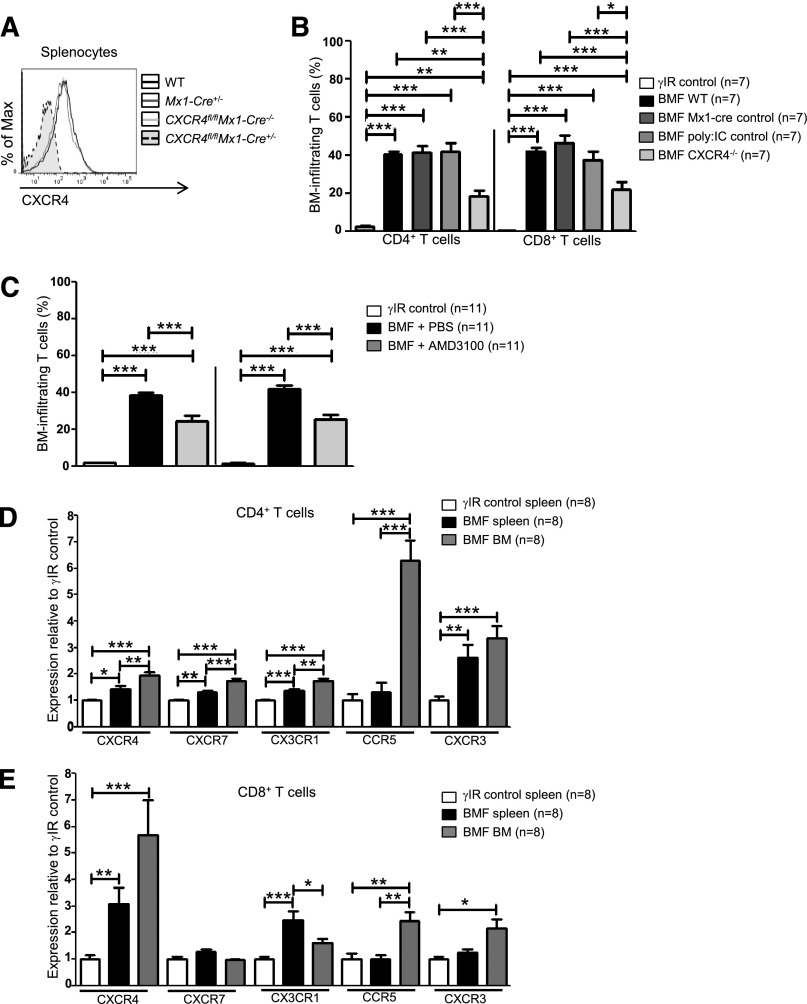
Inhibiting CXCR4 in AA mice reduces T-cell homing to the BM
The natural ligand for CXCR4, SDF-1α, is present in the BM at high concentrations.53 We hypothesized that sustained CXCR4 expression on activated T cells might aid in their trafficking to the BM in diseased animals. Therefore, we asked whether reducing the CXCR4 expression or preventing SDF-1α–CXCR4 interactions would affect BM infiltration of T cells in a mouse model of AA.
Cxcr4 knockout mice are embryonic lethal due to defects in B-cell lymphopoiesis and myelopoiesis, heart and cerebellar development, and vascularization.54,55 Therefore, we used Cre/loxP DNA recombination to conditionally delete Cxcr4 from splenocytes of Cxcr4fl/flMx1-cre+/− (CXCR4−/−) donor mice via serial injections of polyinosinic:polycytidylic acid (poly:IC) (Figure 2A).56 AA mice receiving CXCR4−/− splenocytes had significantly fewer BM-infiltrating CD4+ and CD8+ T cells compared with mice who received control splenocytes (Cxcr4fl/flMx1- cre−/−, Mx1-cre+/−, or WT splenocytes; Figure 2B).
Figure 2.
Inhibiting CXCR4 in AA mice reduces T-cell homing to the BM. (A) Representative histograms of CXCR4 expression on splenocytes from WT C57BL/6 mice, poly:IC-treated Mx1-cre+/− mice (Mx1-cre+/−; Mx1-cre only control), poly:IC-treated CXCR4fl/flMx1-cre−/− mice (CXCR4fl/flMx1-cre−/−; poly:IC control), or poly:IC-treated CXCR4fl/flMx1-cre+/− mice (CXCR4fl/flMx1-cre+/−; CXCR4−/−). (B) Donor splenocytes from (A) were used to induce AA in F1 recipient mice (BMF). On day +17 postdisease induction, percentages of BM-infiltrating CD4+ and CD8+ T cells in AA mice were assessed by flow cytometry and compared with mice that were irradiated only (γIR control); n = 7 mice per group. (C) Mice were induced with AA (BMF), and from days +7 to +16 postdisease induction, were treated with PBS (BMF + PBS) or with the CXCR4 antagonist, AMD3100 (BMF + AMD3100). Percentages of BM-infiltrating CD4+ and CD8+ T cells in AA mice were determined as in (B); n = 11 mice per group. (D-E) F1 hybrid mice were irradiated only (γIR control) or AA was induced by transferrin 5 × 107 WT C57BL/6 splenocytes (BMF). On day +17 postdisease induction, the MFI of CXCR4, CXCR7, CX3CR1, CCR5, and CXCR3 on (D) CD4+ and (E) CD8+ T cells from the spleens and BM of AA mice or irradiation controls was assessed by flow cytometry. Expression was relative to γIR control and was calculated by dividing the MFI of BMF samples by the mean MFI of γIR controls; n = 8 mice per group. Data are the mean ± SEM, and were analyzed by one-way ANOVA plus Tukey post-test. *P < .05; **P < .01; ***P < .001.
We next abrogated SDF-1α–CXCR4 binding using the highly selective CXCR4 antagonist, AMD3100.57 To prevent SDF-1α–CXCR4 interactions during T-cell expansion, AA mice were given AMD3100 (5 mg/kg per day) for 10 days, beginning day +7 postdisease induction. On day +17, we assessed T-cell accumulation in the BM and noted a significant, albeit incomplete reduction, in BM-infiltrating CD4+ and CD8+ T cells in AA mice treated with AMD3100, compared with those treated with vehicle (Figure 2C). Therefore, we analyzed the expression of additional chemokine receptors associated with BM trafficking. Compared with irradiated controls, T cells from spleens and BM of AA mice showed modestly increased CXCR7, CX3CR1, CCR5, and CXCR3 (Figure 2D-E). Among these, CCR5 showed the greatest relative increase on BM CD4+ T cells, whereas CXCR4 was the most highly upregulated on CD8+ T cells (Figure 2D-E). Taken together, these data provide evidence that in AA mice, pathogenic CD8+ T cells aberrantly express and use CXCR4 to traffic to the BM, although additional chemokine receptors may also contribute to this process.
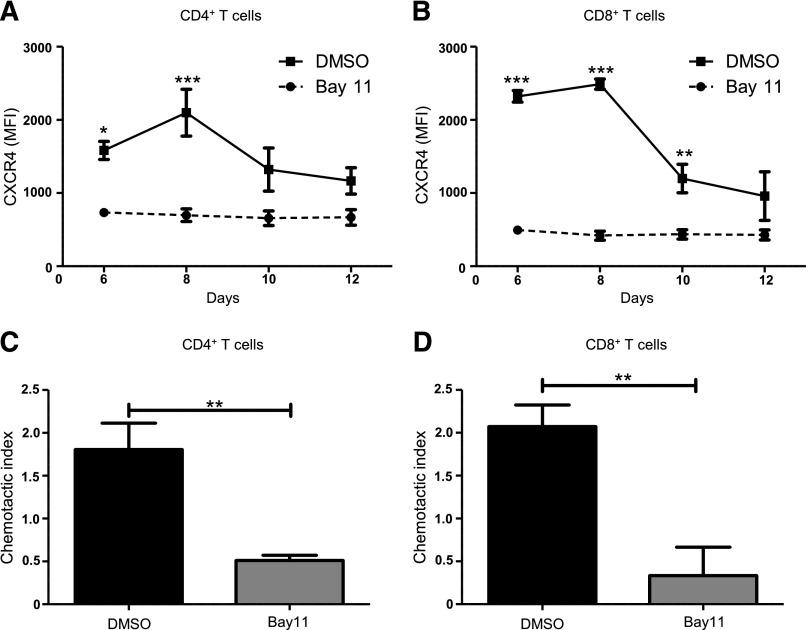
Inhibiting NF-κB signaling reduces CXCR4 expression and abrogates T-cell migration
NF-κB signaling is central to the activation, proliferation, differentiation, and survival of T cells.32 NF-κB regulates CXCR4 expression and subsequent metastasis in a range of malignancies including breast, pancreatic, gastric, prostatic, and ovarian cancers.45-51 However, NF-κB–mediated regulation of CXCR4 expression on T cells has not been previously investigated. Therefore, we asked whether blocking NF-κB signaling would modulate CXCR4 expression on T cells. We used a mixed lymphocyte reaction in which C57BL/6 splenocytes treated with the NF-κB inhibitor, Bay11 (1 μM), or vehicle only, were cocultured with BMDCs from F1 progeny (C57BL / 6×BALB/c), and then analyzed T cells for CXCR4 expression using flow cytometry. Compared with controls, Bay11-treated CD4+ T cells showed significantly diminished CXCR4 expression after 6 and 8 days of culture (Figure 3A), whereas Bay11-treated CD8+ T cells displayed diminished CXCR4 levels on days 6, 8, and 10 of culture (Figure 3B). This is in contrast to DMSO-treated CD4+ and CD8+ T cells, which display elevated CXCR4 expression. We next determined how abrogating NF-κB signaling affects T-cell migration in response to SDF-1α. Treating CD4+ or CD8+ T cells with Bay11 significantly impaired their ability to migrate toward SDF-1α, compared with control cells treated with vehicle only (Figure 3C-D). These findings support the notion that NF-κB signaling regulates CXCR4 expression on CD4+ and CD8+ T cells, which, in turn, mediates their migration across an SDF-1α gradient.
Figure 3.
Inhibiting NF-κB signaling reduces CXCR4 expression and abrogates T-cell migration. Splenocytes from C57BL/6 mice were treated with DMSO or Bay11 (1 μM) and cocultured for 12 days with BMDCs from F1 hybrids. CXCR4 expression was assessed by flow cytometry on (A) CD4+ and (B) CD8+ T cells; n = 3. On day 8 postculture, nonadherent cells were harvested from cocultures (as above) and their chemotactic response to SDF-1α was analyzed. Cells were added to Transwell inserts; 0 or 100 ng/ml SDF-1α was added to wells. Cultures were incubated for 3 hours, at which time migrated cells were harvested from wells and CD4+ and CD8+ T cells were enumerated by flow cytometry. The chemotactic index (number of cells migrated into 100 ng/ml SDF-1α wells/number of cells migrated into 0 ng/ml SDF-1α wells) was calculated for DMSO- or Bay11-treated (C) CD4+ and (D) CD8+ T cells; n = 3. Data are the mean ± SEM, and were analyzed using two-way ANOVA plus Bonferroni post-test (A-B) or two-tailed unpaired Student t test (C-D). *P < .05; **P < .01; ***P < .001.
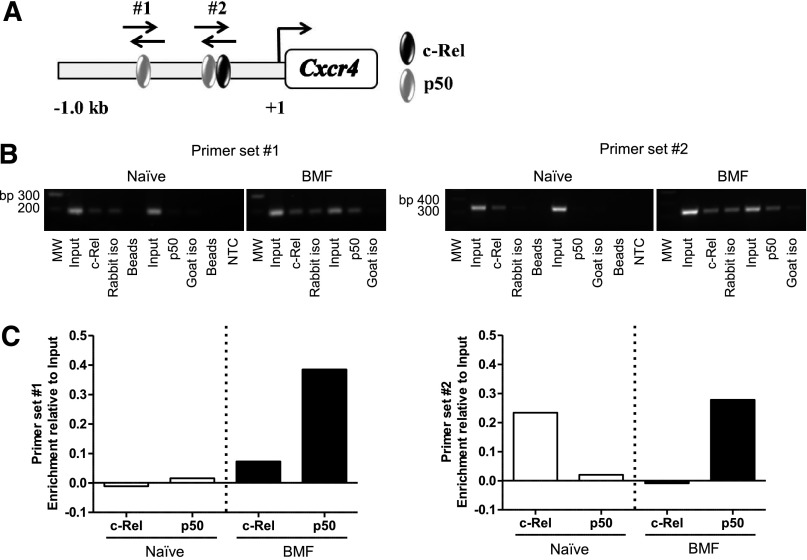
The NF-κB p50 subunit differentially binds the Cxcr4 promoter in T cells of AA mice
Previous reports using human cancer cell lines confirmed NF-κB binding sites in the CXCR4 promoter; however, Cxcr4 regulation in T cells is ill-defined.45,47-50 Therefore, we asked whether NF-κB directly regulates Cxcr4 in BM-infiltrating T cells from AA mice. We analyzed a 1 Kb region upstream of the transcriptional start site in the Cxcr4 promoter and identified 2 putative binding sites for NF-κB subunits, c-Rel and p50 (Figure 4A). Using chromatin derived from naïve CD8+ T cells or from BM-infiltrating CD8+ T cells isolated from AA mice, we performed ChIP with antibodies specific for c-Rel and p50. Unlike in naïve cells, we detected increased p50 occupancy at both sites in the Cxcr4 promoter in pathogenic CD8+ T cells. We also observed differential binding of c-Rel in naïve and BM-infiltrating CD8+ T cells (Figure 4B-C). Collectively, these data reveal that NF-κB–binding to the Cxcr4 promoter is increased in BM-infiltrating CD8+ T cells from AA mice. Furthermore, differences in NF-κB occupancy at the regions we investigated suggest that NF-κB differentially regulates Cxcr4 in naïve and pathogenic CD8+ T cells.
Figure 4.
The NF-κB p50 subunit differentially binds the Cxcr4 promoter in T cells of AA mice. (A) Schematic representation of the Cxcr4 promoter showing relative location of predicted binding sites for NF-κB subunits, p50 and c-Rel, and regions amplified by primer sets #1 and #2 (not shown to scale). (B) Representative image of agarose gel showing 2 amplified regions of the Cxcr4 promoter. Chromatin was from BM-infiltrating CD8+ cells of mice induced with AA (BMF; right) or spleen-infiltrating CD8+ T cells of noninduced mice (Naïve; left) immunoprecipitated using antibodies specific for p50 and c-Rel. (C) Quantification of band intensities of Naïve and BMF samples subjected to ChIP in (B). Data are representative of 2 independent experiments.
Inhibiting NF-κB signaling in AA mice reduces CXCR4 expression in T cells and attenuates AA
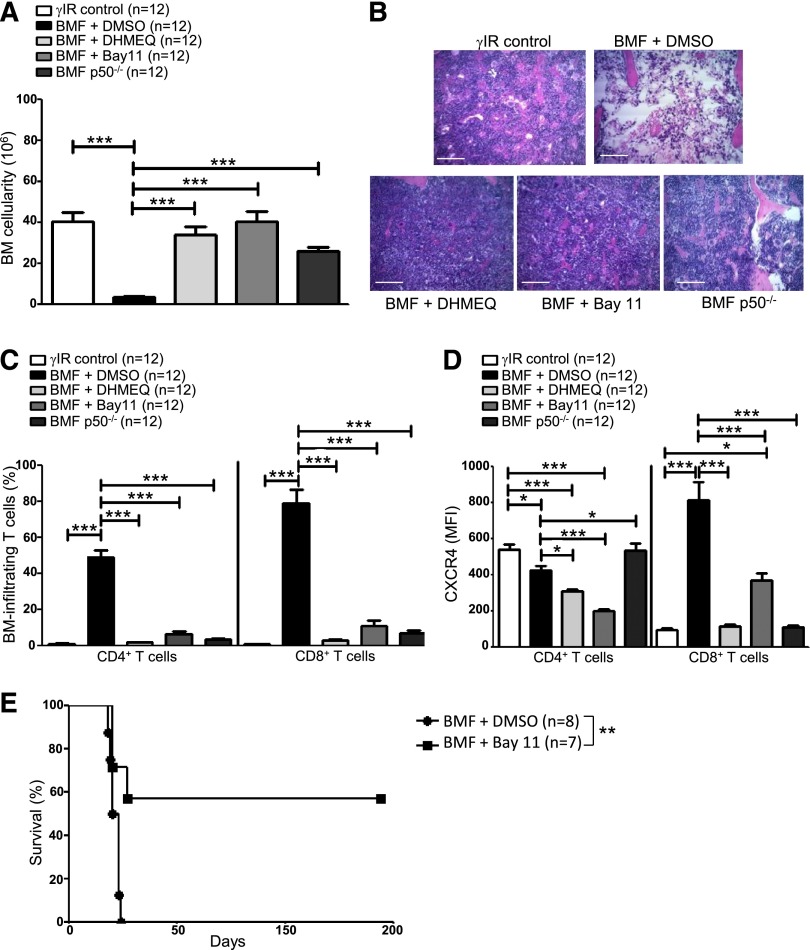
Blocking NF-κB signaling impairs bone metastasis in experimental breast cancer models by preventing CXCR4 expression.58 We inhibited NF-κB signaling in AA mice pharmacologically, using DHMEQ or Bay11, or by transferring p50−/− splenocytes, to determine what effect this would have on T-cell infiltration to the BM and disease progression overall. AA mice were treated with DHMEQ (30 mg/kg per day) or Bay11 (5 mg/kg every other day) beginning 1 hour after disease induction and continuing for 16 days. On day +17 postdisease induction, mice were humanely euthanized to assess disease severity. Inhibiting NF-κB activity in AA mice robustly protected BM cellularity (Figure 5A-B), and this protection extended to circulating WBCs and RBCs (see supplemental Figure 1A-B, available on the Blood Web site). BM-infiltrating CD4+ and CD8+ T cells (Figure 5C), and circulating IFN-γ and tumor necrosis factor (supplemental Figure 1C-D) were negligible in AA mice with impaired NF-κB signaling, compared with vehicle-treated controls.
Figure 5.
Inhibiting NF-κB signaling in AA mice reduces CXCR4 expression in T cells and attenuates AA. F1 hybrid mice were irradiated only (γIR control) or AA was induced with 5 × 107 WT C57BL/6 splenocytes. Mice were treated with DMSO (BMF + DMSO), DHMEQ (BMF + DHMEQ), or Bay11 (BMF + Bay11). In some mice, AA was induced with 5 × 107 p50−/− splenocytes (BMF p50−/−). On day +17 postdisease induction, mice were harvested and (A) total BM cellularity was determined by trypan blue exclusion; n = 12 mice per group. (B) Representative hematoxylin and eosin staining of sternum from 1 representative animal each of irradiation control (γIR control), DMSO-treated AA mouse (BMF + DMSO), DHMEQ-treated AA mouse (BMF + DHMEQ), Bay11-treated AA mouse (BMF + Bay11), and 1 mouse that received p50−/− splenocytes (BMF p50−/−). Scale bar = 200 μM. (C) Percentages of BM-infiltrating CD4+ and CD8+ T cells in irradiation controls or AA mice that received DMSO, DHMEQ, Bay11, or p50−/− splenocytes were determined by flow cytometry; n = 12 mice per group. (D) MFI of CXCR4 protein expression on BM-infiltrating CD4+ and CD8+ T cells of AA mice that received DMSO, DHMEQ, Bay11, or p50−/− splenocytes was assessed by flow cytometry and compared with CXCR4 MFI on BM-infiltrating T cells of irradiation controls; n = 12. (E) Kaplan–Meier survival estimates of AA mice whose disease was induced with WT splenocytes and treated with DMSO (n = 8) or Bay11 (n = 7), beginning on day +7 postdisease induction and continuing until day +17 postdisease induction. Data are the mean ± SEM, and analyzed using one-way ANOVA plus Tukey post-test or log-rank test for survival estimates. *P < .05; **P < .01; ***P < .001.
Moreover, when AA mice received NF-κB inhibitors or p50−/− splenocytes, a significantly lower percentage of BM CD8+ T cells expressed CXCR4 (supplemental Figure 1E), and the per cell expression of CXCR4 on BM CD8+ T cells was significantly lower compared with control-treated AA mice (Figure 5D). Consistent with the results of the ChIP (Figure 4), these data support the notion that NF-κB, and more specifically p50, play an important role in regulating CXCR4 expression in pathogenic CD8+ T cells.
Finally, we evaluated the survival benefit of pharmacologically limiting NF-κB signaling in AA mice under clinically relevant conditions. AA mice were treated with Bay11 (5 mg/kg every other day) or vehicle only (DMSO) from days +7 to +17 postdisease induction, at which time treatment was discontinued. Compared with DMSO-treated mice, for which the median survival time was 19.5 days (range, 18 to 24 days), Bay11 treatment significantly extended survival in AA mice, with 4 of 7 mice fully rescued from lethal BMF (P < .01) (Figure 5E). Collectively, our data demonstrate that attenuating NF-κB signaling in a mouse model of AA reduces CXCR4 expression on CD8+ T cells, prevents T-cell homing to the BM, and ameliorates disease symptoms.
Discussion
AA is primarily driven by an aberrant Th1 immune response, whereby activated T cells traffic to the BM and mediate destruction. Differential expression of chemokine receptors and adhesion molecules on Th-cell subsets endow these T cells with distinct migratory abilities and selective recruitment into peripheral tissues.27,59-62 The chemokine receptor, CXCR4, facilitates cellular chemotaxis in response to its natural ligand, SDF-1α, found in high concentrations in the BM.17,18,63-65 Aberrantly elevated CXCR4 has been reported in numerous autoimmune conditions, and is also thought to provide a means for certain cancerous cells to home to SDF-1α–enriched sites, such as the BM.33-39,47 CXCR4 is highly-expressed on resting T cells, including naïve and memory T cells, and is downregulated during T-cell activation.26,30,31,60 Using inhibitors and genetic approaches, we provide evidence that BM-infiltrating CD4+ and CD8+ T cells from AA mice show high CXCR4 expression, suggesting CXCR4–SDF-1α interaction may be one mechanism pathogenic T cells use to traffic to the BM during AA progression.
Chemokine receptors, including CX3CR1 and CCR5, facilitate migration of normal and malignant cells to the BM, whereas CXCR7 has been identified as an additional receptor for SDF-1α.66-69 Data presented in this study (Figure 2D-E) are in concordance with previous reports describing elevated CX3CR1 on peripheral and BM T cells, and increased expression of CX3CR1 and CXCR3 in BM T cells of patients with severe AA.67,70,71 Reports also indicate peripheral and BM CD4+ regulatory T cells from patients with severe AA have reduced CXCR4 expression, compared with those of healthy controls, with impaired ability to home to the BM and suppress pathogenic T cells.10 In AA mice, CCR5 expression on BM-infiltrating CD4+ T cells showed the greatest increase, whereas on BM CD8+ T cells, CXCR4 exhibited the highest relative gain. Residual BM T cells could be detected in AA mice whose disease was induced with CXCR4−/− splenocytes or were treated with AMD3100, indicating chemokine receptors other than CXCR4 may aid in T cell trafficking to the BM. Indeed, we observed modestly augmented CXCR7, CX3CR1, and CXCR3 on BM T cells and their expression levels remained unchanged when CXCR4 was inhibited (data not shown). Thus, dysregulated expression of chemokine receptors may be a general feature of AA progression in mice and in humans.
In breast cancer cell lines, NF-κB directly regulates Cxcr4 expression, which enhances motility in vitro and in vivo metastasis to the BM in animal models.47 Consistent with this notion, we observed increased p50 occupancy at two distinct NF-κB binding sites in the Cxcr4 promoter in BM-infiltrating CD8+ T cells. These sites were not similarly bound in naïve CD8+ T cells, suggesting that differential NF-κB binding to the Cxcr4 promoter in BM-infiltrating CD8+ T cells contributes to aberrant CXCR4 expression. Inhibitory or genetic approaches that limited NF-κB signaling decreased CXCR4 expression on CD8+ T cells, and this further correlated with their reduced trafficking to the BM. However, compared with approaches that only abrogated CXCR4–SDF-1α interactions in AA mice, limiting NF-κB activity resulted in a more profound reduction in T-cell infiltration to the BM and negligible circulating IFN-γ and tumor necrosis factor. Finally, inhibiting NF-κB in AA mice under therapeutic conditions prolonged their survival, with >50% of mice fully rescued from lethal BMF, and underscoring the important role for NF-κB in regulating additional proinflammatory pathways that mediate BMF in mice.
Herein, we provide evidence that NF-κB–regulated, aberrant CXCR4 expression may be one means by which CD8+ T cells infiltrate the BM during AA progression in mice. The AA mice used in this study represent an additional tool with which to better understand a rare and complex BMF disorder; however, as with all animal models, care must be taken when extrapolating results to the human disease. Further studies of paired samples of peripheral blood and BM from patients with AA will be needed to confirm the relevance of our findings. Determining the full array of chemokine receptors and adhesion molecules that endow pathogenic CD4+ and CD8+ T cells with the ability to traffic to the BM during AA will undoubtedly add to our understanding of the molecular mechanisms that drive this disease.
Acknowledgments
The authors thank the animal care staff for their excellent support, M. Klingbeil for sonicator use, and A. Fauq for DMHEQ.
This study was supported by the Aplastic Anemia and MDS International Foundation, Inc., the American Heart Association, Inc., a Charles H. Hood Foundation Child Health Research Award, the National Institutes of Health, National Cancer Institute (1P01 CA166009-01A1) (L.M.M.), and the National Science Foundation (MRI BD1-1126366) to the Flow Cytometry Core Facility, University of Massachusetts Amherst.
Footnotes
The online version of this article contains a data supplement.
The publication costs of this article were defrayed in part by page charge payment. Therefore, and solely to indicate this fact, this article is hereby marked “advertisement” in accordance with 18 USC section 1734.
Authorship
Contribution: C.A.K. and G.G.-P. performed experiments, collected, and analyzed data; L.M.M. designed and supervised experiments with contributions from C.A.K. and G.G.-P; and G.G.-P. wrote the manuscript, with critical input from C.A.K. and L.M.M.
Conflict-of-interest disclosure: The authors declare no competing financial interests.
Correspondence: Lisa M. Minter, 427K Integrated Sciences Bldg, 661 N. Pleasant St, Department of Veterinary and Animal Sciences, University of Massachusetts Amherst, Amherst, MA 01003; e-mail: lminter@vasci.umass.edu.
References
- 1.Dolberg OJ, Levy Y. Idiopathic aplastic anemia: diagnosis and classification. Autoimmun Rev. 2014;13(4-5):569–573. doi: 10.1016/j.autrev.2014.01.014. [DOI] [PubMed] [Google Scholar]
- 2.Hartung HD, Olson TS, Bessler M. Acquired aplastic anemia in children. Pediatr Clin North Am. 2013;60(6):1311–1336. doi: 10.1016/j.pcl.2013.08.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Young NS, Scheinberg P, Calado RT. Aplastic anemia. Curr Opin Hematol. 2008;15(3):162–168. doi: 10.1097/MOH.0b013e3282fa7470. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Scheinberg P, Chen J. Aplastic anemia: what have we learned from animal models and from the clinic. Semin Hematol. 2013;50(2):156–164. doi: 10.1053/j.seminhematol.2013.03.028. [DOI] [PubMed] [Google Scholar]
- 5.Roderick JE, Gonzalez-Perez G, Kuksin CA, et al. Therapeutic targeting of NOTCH signaling ameliorates immune-mediated bone marrow failure of aplastic anemia. J Exp Med. 2013;210(7):1311–1329. doi: 10.1084/jem.20112615. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Solomou EE, Keyvanfar K, Young NS. T-bet, a Th1 transcription factor, is up-regulated in T cells from patients with aplastic anemia. Blood. 2006;107(10):3983–3991. doi: 10.1182/blood-2005-10-4201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.de Latour RP, Visconte V, Takaku T, et al. Th17 immune responses contribute to the pathophysiology of aplastic anemia. Blood. 2010;116(20):4175–4184. doi: 10.1182/blood-2010-01-266098. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Kook H, Zeng W, Guibin C, Kirby M, Young NS, Maciejewski JP. Increased cytotoxic T cells with effector phenotype in aplastic anemia and myelodysplasia. Exp Hematol. 2001;29(11):1270–1277. doi: 10.1016/s0301-472x(01)00736-6. [DOI] [PubMed] [Google Scholar]
- 9.Solomou EE, Rezvani K, Mielke S, et al. Deficient CD4+ CD25+ FOXP3+ T regulatory cells in acquired aplastic anemia. Blood. 2007;110(5):1603–1606. doi: 10.1182/blood-2007-01-066258. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Shi J, Ge M, Lu S, et al. Intrinsic impairment of CD4(+)CD25(+) regulatory T cells in acquired aplastic anemia. Blood. 2012;120(8):1624–1632. doi: 10.1182/blood-2011-11-390708. [DOI] [PubMed] [Google Scholar]
- 11.Feuerer M, Beckhove P, Garbi N, et al. Bone marrow as a priming site for T-cell responses to blood-borne antigen. Nat Med. 2003;9(9):1151–1157. doi: 10.1038/nm914. [DOI] [PubMed] [Google Scholar]
- 12.Feuerer M, Beckhove P, Mahnke Y, et al. Bone marrow microenvironment facilitating dendritic cell: CD4 T cell interactions and maintenance of CD4 memory. Int J Oncol. 2004;25(4):867–876. [PubMed] [Google Scholar]
- 13.Schirrmacher V, Feuerer M, Fournier P, Ahlert T, Umansky V, Beckhove P. T-cell priming in bone marrow: the potential for long-lasting protective anti-tumor immunity. Trends Mol Med. 2003;9(12):526–534. doi: 10.1016/j.molmed.2003.10.001. [DOI] [PubMed] [Google Scholar]
- 14.Di Rosa F, Pabst R. The bone marrow: a nest for migratory memory T cells. Trends Immunol. 2005;26(7):360–366. doi: 10.1016/j.it.2005.04.011. [DOI] [PubMed] [Google Scholar]
- 15.Feuerer M, Rocha M, Bai L, et al. Enrichment of memory T cells and other profound immunological changes in the bone marrow from untreated breast cancer patients. Int J Cancer. 2001;92(1):96–105. [PubMed] [Google Scholar]
- 16.Tokoyoda K, Zehentmeier S, Hegazy AN, et al. Professional memory CD4+ T lymphocytes preferentially reside and rest in the bone marrow. Immunity. 2009;30(5):721–730. doi: 10.1016/j.immuni.2009.03.015. [DOI] [PubMed] [Google Scholar]
- 17.Zou L, Barnett B, Safah H, et al. Bone marrow is a reservoir for CD4+CD25+ regulatory T cells that traffic through CXCL12/CXCR4 signals. Cancer Res. 2004;64(22):8451–8455. doi: 10.1158/0008-5472.CAN-04-1987. [DOI] [PubMed] [Google Scholar]
- 18.Chaix J, Nish SA, Lin WH, et al. Cutting edge: CXCR4 is critical for CD8+ memory T cell homeostatic self-renewal but not rechallenge self-renewal. J Immunol. 2014;193(3):1013–1016. doi: 10.4049/jimmunol.1400488. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Bleul CC, Farzan M, Choe H, et al. The lymphocyte chemoattractant SDF-1 is a ligand for LESTR/fusin and blocks HIV-1 entry. Nature. 1996;382(6594):829–833. doi: 10.1038/382829a0. [DOI] [PubMed] [Google Scholar]
- 20.Suzuki Y, Rahman M, Mitsuya H. Diverse transcriptional response of CD4+ T cells to stromal cell-derived factor SDF-1: cell survival promotion and priming effects of SDF-1 on CD4+ T cells. J Immunol. 2001;167(6):3064–3073. doi: 10.4049/jimmunol.167.6.3064. [DOI] [PubMed] [Google Scholar]
- 21.Kumar A, Humphreys TD, Kremer KN, et al. CXCR4 physically associates with the T cell receptor to signal in T cells. Immunity. 2006;25(2):213–224. doi: 10.1016/j.immuni.2006.06.015. [DOI] [PubMed] [Google Scholar]
- 22.Nanki T, Lipsky PE. Cutting edge: stromal cell-derived factor-1 is a costimulator for CD4+ T cell activation. J Immunol. 2000;164(10):5010–5014. doi: 10.4049/jimmunol.164.10.5010. [DOI] [PubMed] [Google Scholar]
- 23.Patrussi L, Baldari CT. Intracellular mediators of CXCR4-dependent signaling in T cells. Immunol Lett. 2008;115(2):75–82. doi: 10.1016/j.imlet.2007.10.012. [DOI] [PubMed] [Google Scholar]
- 24.Molon B, Gri G, Bettella M, et al. T cell costimulation by chemokine receptors. Nat Immunol. 2005;6(5):465–471. doi: 10.1038/ni1191. [DOI] [PubMed] [Google Scholar]
- 25.Contento RL, Molon B, Boularan C, et al. CXCR4-CCR5: a couple modulating T cell functions. Proc Natl Acad Sci USA. 2008;105(29):10101–10106. doi: 10.1073/pnas.0804286105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Abbal C, Jourdan P, Hori T, Bousquet J, Yssel H, Pène J. TCR-mediated activation of allergen-specific CD45RO(+) memory T lymphocytes results in down-regulation of cell-surface CXCR4 expression and a strongly reduced capacity to migrate in response to stromal cell-derived factor-1. Int Immunol. 1999;11(9):1451–1462. doi: 10.1093/intimm/11.9.1451. [DOI] [PubMed] [Google Scholar]
- 27.Annunziato F, Cosmi L, Galli G, et al. Assessment of chemokine receptor expression by human Th1 and Th2 cells in vitro and in vivo. J Leukoc Biol. 1999;65(5):691–699. doi: 10.1002/jlb.65.5.691. [DOI] [PubMed] [Google Scholar]
- 28.Jourdan P, Vendrell JP, Huguet MF, et al. Cytokines and cell surface molecules independently induce CXCR4 expression on CD4+ CCR7+ human memory T cells. J Immunol. 2000;165(2):716–724. doi: 10.4049/jimmunol.165.2.716. [DOI] [PubMed] [Google Scholar]
- 29.Signoret N, Oldridge J, Pelchen-Matthews A, et al. Phorbol esters and SDF-1 induce rapid endocytosis and down modulation of the chemokine receptor CXCR4. J Cell Biol. 1997;139(3):651–664. doi: 10.1083/jcb.139.3.651. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Bermejo M, Martín-Serrano J, Oberlin E, et al. Activation of blood T lymphocytes down-regulates CXCR4 expression and interferes with propagation of X4 HIV strains. Eur J Immunol. 1998;28(10):3192–3204. doi: 10.1002/(SICI)1521-4141(199810)28:10<3192::AID-IMMU3192>3.0.CO;2-E. [DOI] [PubMed] [Google Scholar]
- 31.Langenkamp A, Nagata K, Murphy K, Wu L, Lanzavecchia A, Sallusto F. Kinetics and expression patterns of chemokine receptors in human CD4+ T lymphocytes primed by myeloid or plasmacytoid dendritic cells. Eur J Immunol. 2003;33(2):474–482. doi: 10.1002/immu.200310023. [DOI] [PubMed] [Google Scholar]
- 32.Gerondakis S, Siebenlist U. Roles of the NF-kappaB pathway in lymphocyte development and function. Cold Spring Harb Perspect Biol. 2010;2(5):a000182. doi: 10.1101/cshperspect.a000182. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.McCandless EE, Piccio L, Woerner BM, et al. Pathological expression of CXCL12 at the blood-brain barrier correlates with severity of multiple sclerosis. Am J Pathol. 2008;172(3):799–808. doi: 10.2353/ajpath.2008.070918. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Moll NM, Cossoy MB, Fisher E, et al. Imaging correlates of leukocyte accumulation and CXCR4/CXCL12 in multiple sclerosis. Arch Neurol. 2009;66(1):44–53. doi: 10.1001/archneurol.2008.512. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Wang A, Guilpain P, Chong BF, et al. Dysregulated expression of CXCR4/CXCL12 in subsets of patients with systemic lupus erythematosus. Arthritis Rheum. 2010;62(11):3436–3446. doi: 10.1002/art.27685. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Chung SH, Seki K, Choi BI, et al. CXC chemokine receptor 4 expressed in T cells plays an important role in the development of collagen-induced arthritis. Arthritis Res Ther. 2010;12(5):R188. doi: 10.1186/ar3158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Nanki T, Hayashida K, El-Gabalawy HS, et al. Stromal cell-derived factor-1-CXC chemokine receptor 4 interactions play a central role in CD4+ T cell accumulation in rheumatoid arthritis synovium. J Immunol. 2000;165(11):6590–6598. doi: 10.4049/jimmunol.165.11.6590. [DOI] [PubMed] [Google Scholar]
- 38.Leng Q, Nie Y, Zou Y, Chen J. Elevated CXCL12 expression in the bone marrow of NOD mice is associated with altered T cell and stem cell trafficking and diabetes development. BMC Immunol. 2008 doi: 10.1186/1471-2172-9-51. doi:10.1186/1471-2172-9-51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Zhao Y, Guo C, Hwang D, et al. Selective destruction of mouse islet beta cells by human T lymphocytes in a newly-established humanized type 1 diabetic model. Biochem Biophys Res Commun. 2010;399(4):629–636. doi: 10.1016/j.bbrc.2010.07.128. [DOI] [PubMed] [Google Scholar]
- 40.Kuryłowicz A, Nauman J. The role of nuclear factor-kappaB in the development of autoimmune diseases: a link between genes and environment. Acta Biochim Pol. 2008;55(4):629–647. [PubMed] [Google Scholar]
- 41.Pai S, Thomas R. Immune deficiency or hyperactivity-Nf-kappab illuminates autoimmunity. J Autoimmun. 2008;31(3):245–251. doi: 10.1016/j.jaut.2008.04.012. [DOI] [PubMed] [Google Scholar]
- 42.Burger JA, Kipps TJ. CXCR4: a key receptor in the crosstalk between tumor cells and their microenvironment. Blood. 2006;107(5):1761–1767. doi: 10.1182/blood-2005-08-3182. [DOI] [PubMed] [Google Scholar]
- 43.Braun T, Carvalho G, Fabre C, Grosjean J, Fenaux P, Kroemer G. Targeting NF-kappaB in hematologic malignancies. Cell Death Differ. 2006;13(5):748–758. doi: 10.1038/sj.cdd.4401874. [DOI] [PubMed] [Google Scholar]
- 44.Sethi G, Sung B, Aggarwal BB. Nuclear factor-kappaB activation: from bench to bedside. Exp Biol Med (Maywood) 2008;233(1):21–31. doi: 10.3181/0707-MR-196. [DOI] [PubMed] [Google Scholar]
- 45.Shanmugam MK, Manu KA, Ong TH, et al. Inhibition of CXCR4/CXCL12 signaling axis by ursolic acid leads to suppression of metastasis in transgenic adenocarcinoma of mouse prostate model. Int J Cancer. 2011;129(7):1552–1563. doi: 10.1002/ijc.26120. [DOI] [PubMed] [Google Scholar]
- 46.Manu KA, Shanmugam MK, Ramachandran L, et al. First evidence that γ-tocotrienol inhibits the growth of human gastric cancer and chemosensitizes it to capecitabine in a xenograft mouse model through the modulation of NF-κB pathway. Clin Cancer Res. 2012;18(8):2220–2229. doi: 10.1158/1078-0432.CCR-11-2470. [DOI] [PubMed] [Google Scholar]
- 47.Helbig G, Christopherson KW, II, Bhat-Nakshatri P, et al. NF-kappaB promotes breast cancer cell migration and metastasis by inducing the expression of the chemokine receptor CXCR4. J Biol Chem. 2003;278(24):21631–21638. doi: 10.1074/jbc.M300609200. [DOI] [PubMed] [Google Scholar]
- 48.Chua AW, Hay HS, Rajendran P, et al. Butein downregulates chemokine receptor CXCR4 expression and function through suppression of NF-κB activation in breast and pancreatic tumor cells. Biochem Pharmacol. 2010;80(10):1553–1562. doi: 10.1016/j.bcp.2010.07.045. [DOI] [PubMed] [Google Scholar]
- 49.Manu KA, Shanmugam MK, Rajendran P, et al. Plumbagin inhibits invasion and migration of breast and gastric cancer cells by downregulating the expression of chemokine receptor CXCR4. Mol Cancer. 2011 doi: 10.1186/1476-4598-10-107. doi:10.1186/1476-4598-10-107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Arora S, Bhardwaj A, Singh S, et al. An undesired effect of chemotherapy: gemcitabine promotes pancreatic cancer cell invasiveness through reactive oxygen species-dependent, nuclear factor κB- and hypoxia-inducible factor 1α-mediated up-regulation of CXCR4. J Biol Chem. 2013;288(29):21197–21207. doi: 10.1074/jbc.M113.484576. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Miyanishi N, Suzuki Y, Simizu S, Kuwabara Y, Banno K, Umezawa K. Involvement of autocrine CXCL12/CXCR4 system in the regulation of ovarian carcinoma cell invasion. Biochem Biophys Res Commun. 2010;403(1):154–159. doi: 10.1016/j.bbrc.2010.11.007. [DOI] [PubMed] [Google Scholar]
- 52.Ghazalpour A, Bennett B, Petyuk VA, et al. Comparative analysis of proteome and transcriptome variation in mouse. PLoS Genet. 2011;7(6):e1001393. doi: 10.1371/journal.pgen.1001393. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Sugiyama T, Kohara H, Noda M, Nagasawa T. Maintenance of the hematopoietic stem cell pool by CXCL12-CXCR4 chemokine signaling in bone marrow stromal cell niches. Immunity. 2006;25(6):977–988. doi: 10.1016/j.immuni.2006.10.016. [DOI] [PubMed] [Google Scholar]
- 54.Ma Q, Jones D, Borghesani PR, et al. Impaired B-lymphopoiesis, myelopoiesis, and derailed cerebellar neuron migration in CXCR4- and SDF-1–deficient mice. Proc Natl Acad Sci USA. 1998;95(16):9448–9453. doi: 10.1073/pnas.95.16.9448. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Zou YR, Kottmann AH, Kuroda M, Taniuchi I, Littman DR. Function of the chemokine receptor CXCR4 in haematopoiesis and in cerebellar development. Nature. 1998;393(6685):595–599. doi: 10.1038/31269. [DOI] [PubMed] [Google Scholar]
- 56.Kühn R, Schwenk F, Aguet M, Rajewsky K. Inducible gene targeting in mice. Science. 1995;269(5229):1427–1429. doi: 10.1126/science.7660125. [DOI] [PubMed] [Google Scholar]
- 57.Hatse S, Princen K, Bridger G, De Clercq E, Schols D. Chemokine receptor inhibition by AMD3100 is strictly confined to CXCR4. FEBS Lett. 2002;527(1-3):255–262. doi: 10.1016/s0014-5793(02)03143-5. [DOI] [PubMed] [Google Scholar]
- 58.Rahman KM, Sarkar FH, Banerjee S, et al. Therapeutic intervention of experimental breast cancer bone metastasis by indole-3-carbinol in SCID-human mouse model. Mol Cancer Ther. 2006;5(11):2747–2756. doi: 10.1158/1535-7163.MCT-06-0221. [DOI] [PubMed] [Google Scholar]
- 59.Zlotnik A, Yoshie O. The chemokine superfamily revisited. Immunity. 2012;36(5):705–716. doi: 10.1016/j.immuni.2012.05.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Sallusto F, Lenig D, Mackay CR, Lanzavecchia A. Flexible programs of chemokine receptor expression on human polarized T helper 1 and 2 lymphocytes. J Exp Med. 1998;187(6):875–883. doi: 10.1084/jem.187.6.875. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Siveke JT, Hamann A. T helper 1 and T helper 2 cells respond differentially to chemokines. J Immunol. 1998;160(2):550–554. [PubMed] [Google Scholar]
- 62.Bonecchi R, Bianchi G, Bordignon PP, et al. Differential expression of chemokine receptors and chemotactic responsiveness of type 1 T helper cells (Th1s) and Th2s. J Exp Med. 1998;187(1):129–134. doi: 10.1084/jem.187.1.129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Burger JA, Spoo A, Dwenger A, Burger M, Behringer D. CXCR4 chemokine receptors (CD184) and alpha4beta1 integrins mediate spontaneous migration of human CD34+ progenitors and acute myeloid leukaemia cells beneath marrow stromal cells (pseudoemperipolesis). Br J Haematol. 2003;122(4):579–589. doi: 10.1046/j.1365-2141.2003.04466.x. [DOI] [PubMed] [Google Scholar]
- 64.Zhao E, Wang L, Dai J, et al. Regulatory T cells in the bone marrow microenvironment in patients with prostate cancer. OncoImmunology. 2012;1(2):152–161. doi: 10.4161/onci.1.2.18480. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Beider K, Nagler A, Wald O, et al. Involvement of CXCR4 and IL-2 in the homing and retention of human NK and NK T cells to the bone marrow and spleen of NOD/SCID mice. Blood. 2003;102(6):1951–1958. doi: 10.1182/blood-2002-10-3293. [DOI] [PubMed] [Google Scholar]
- 66.Jamieson-Gladney WL, Zhang Y, Fong AM, Meucci O, Fatatis A. The chemokine receptor CX₃CR1 is directly involved in the arrest of breast cancer cells to the skeleton. Breast Cancer Res. 2011;13(5):R91. doi: 10.1186/bcr3016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Ren J, Hou XY, Ma SH, et al. Elevated expression of CX3C chemokine receptor 1 mediates recruitment of T cells into bone marrow of patients with acquired aplastic anaemia. J Intern Med. 2014;276(5):512–524. doi: 10.1111/joim.12218. [DOI] [PubMed] [Google Scholar]
- 68.Balabanian K, Lagane B, Infantino S, et al. The chemokine SDF-1/CXCL12 binds to and signals through the orphan receptor RDC1 in T lymphocytes. J Biol Chem. 2005;280(42):35760–35766. doi: 10.1074/jbc.M508234200. [DOI] [PubMed] [Google Scholar]
- 69.Trentin L, Miorin M, Facco M, et al. Multiple myeloma plasma cells show different chemokine receptor profiles at sites of disease activity. Br J Haematol. 2007;138(5):594–602. doi: 10.1111/j.1365-2141.2007.06686.x. [DOI] [PubMed] [Google Scholar]
- 70.Zeng W, Kajigaya S, Chen G, Risitano AM, Nunez O, Young NS. Transcript profile of CD4+ and CD8+ T cells from the bone marrow of acquired aplastic anemia patients. Exp Hematol. 2004;32(9):806–814. doi: 10.1016/j.exphem.2004.06.004. [DOI] [PubMed] [Google Scholar]
- 71.Franzke A, Geffers R, Hunger JK, et al. Identification of novel regulators in T-cell differentiation of aplastic anemia patients. BMC Genomics. 2006 doi: 10.1186/1471-2164-7-263. doi:10.1186/1471-2164-7-263. [DOI] [PMC free article] [PubMed] [Google Scholar]