Abstract
With an increase in the number of transplants happening globally, hematopoietic stem cells (HSC) transplantation from matched unrelated donor (MUD) has begun. The increasing trend of MUD transplants across countries has been largely facilitated with the conspicuous growth of volunteer HSC donor noted in the last decade i.e. 8 million HSC donors in 2002 to more than 22 million in 2013 registered in 71 member registries of the Bone Marrow Donor Worldwide (BMDW). Some populations of the world are still very poorly represented in these registries. Since, the chances of successful engraftment and disease free survival are directly proportional to the HLA compatibility between the recipient and the prospective donor, the diversity of the HLA system at the antigenic and allelic level and the heterogeneity of HLA data of the registered donors has a bearing on the probability of finding a volunteer unrelated HSC donor for patients from such populations. In the present study 126 patients were identified suffering from hematological diseases requiring MUD transplant. Their HLA typing was performed and search was done using BMDW database. The search results for these Indian patients in the multinational registry as well as in the Indian Registries were analyzed using mean, range, standard deviation and finally evaluated in terms of probability for finding matched donor (MUD). Total Asian population is only 11 % in the BMDW making it difficult to find a MUD for an Asian patient. The current study supports this, experimentally; revealing that the probability of finding an allele match for an Indian patient in the multinational Human Leukocyte Antigen (HLA) registries is 16 % and a dismal 0.008 % in the Indian registries (donors in Indian registries is just 33,678 as compared to 22.5 million in BMDW). This greatly, emphasizes on enhancing the number of Indian donors in Indian and multi-national registries.
Keywords: Allelic, Antigenic, HLA, HSC, MUD
Introduction
Hematopoietic stem cell transplantation (HSCT) is one of the most appropriate clinical applications of stem cells. HSCT is used as a curative treatment in haematological ailments, malignant (for e.g. Leukemia) as well as benign (for e.g. Thalassemia).
According to the reports of Gratwohl [1] there were 50, 417 HSCTs performed in 2006, worldwide. Out of which, 28901 were autologous (57 %). And remaining 21,516 were the allogenic (43 %). In America 58 % were autologous while 42 % were allogenic transplants. In other countries like Asia, Europe, EMRO/Africa (WHO regions Eastern Mediterranean and Africa) the percentage of allogenic transplants was 57, 38 and 62 respectively. When this data was further studied, it came out that amongst the 42 % the allogenic transplants in America 23.94 % were from family donor and 18.06 % from unrelated match donor. Similarly in Asia out of 57 % allogenic transplants 27.36 % were from family donor and 29.64 % from MUD. In Europe and other EMRO/African countries the MUD was 17.48 and 0.62 % respectively. These percentage showed some slight positive changes in 2008 [2] (Table 1).
Table 1.
Signifying the transplant data of various countries
| Name of the continent | Type of transplants | ||
|---|---|---|---|
| Autologous | Allogenic | ||
| Total no. of transplants worldwide in 2006 | |||
| Europe | 62 % | 38 % | |
| Family donor | Match unrelated donor | ||
| 20.52 % | 17.48 % | ||
| America | 58 % | 42 % | |
| Family donor | Match unrelated donor | ||
| 23.94 % | 18.06 % | ||
| Asia | 43 % | 57 % | |
| Family donor | Match unrelated donor | ||
| 27.36 % | 29.64 % | ||
| EMRO/African | 38 % | 62 % | |
| Family donor | Match unrelated donor | ||
| 61.38 % | 0.62 % | ||
| Total No. of transplants worldwide in 2008 | |||
| Europe | 61 % | 39 % | |
| Family donor | Match unrelated donor | ||
| 19.89 % | 19.11 % | ||
| America | 54 % | 46 % | |
| Family donor | Match unrelated donor | ||
| 23.92 % | 22.08 % | ||
| Asia | 40 % | 60 % | |
| Family Donor | Match Unrelated Donor | ||
| 30.60 % | 29.40 % | ||
| EMRO/African | 37 % | 63 % | |
| Family donor | Match unrelated donor | ||
| 62.37 % | 0.63 % | ||
According to one of the published report it is very clear that out of 48 % MUD in Asia [1], Japan alone is contributing more than half (32 %) of it, while China is contributing 16 % [3]. The contribution from India is very small. Data from the Indian Transplant Registry show that the number of bone marrow transplants (BMT) in 1990 was negligible.
By 2010, considering the data from the two highly populated Asian countries: Japan and China, it is speculated that in China alone 91 % of the total allogenic transplants of Asian origin are taking place, contributing about 16 % of MUD (Table 2). This data indicates that when we are talking about the occurrence of MUD in Asian countries, China is one of the most important contributor for performing these transplants, signifying that other Asian countries especially India is far lacking behind in this contribution. This could be attributed due to several factors for e.g. population size; number of health insurance; less number of donors registered in Indian registries; poor representation of Indians in International registries etc. making the MUD search difficult.
Table 2.
Representing the transplant data of China
| Transplant data of china in % | ||||
|---|---|---|---|---|
| Total % of transplants | Type of transplant | |||
| 1986–2005 | ||||
| Autologous | Allogenic | |||
| 100 | 44.5 | 55.5 | ||
| Identical sibling | Mismatch/Haploidenticals | MUD | ||
| 36 | 11.5 | 8 | ||
| 2006 | ||||
| Autologous | Allogenic | |||
| 100 | 20 | 80 | ||
| Identical sibling/Mismatch-Haploidenticals | MUD | |||
| 60 | 20 | |||
| 2007–2008 | ||||
| Autologous | Allogenic | |||
| 100 | 1.8 | 98.2 | ||
| Identical sibling | Mismatch-Haploidenticals | MUD | ||
| 48 | 31.4 | 18.8 | ||
| 2010–2011 | ||||
| Autologous | Allogenic | |||
| 100 | 9 | 91 | ||
| Identical sibling | Mismatch-Haploidenticals | MUD/MUD Mismatch | ||
| 45 | 30 | 16 | ||
While considering the data provided by BMDW [4] in annual report 2012, it is clearly indicated that the number of stem cell donors in Asia is just 11 %, stating that of the world population only 0.3 % is registered as a HSC’ s donor. With such a small number of donors registered in these donor database, it is really difficulty as well as tedious to find a match unrelated donor.
Later on, Chandy [5], reported 1,540 BMT performed at six BMT centres across India which has grown by 63 % (in 2010), indicating that the infrastructure, trained personnel and processes all exist for performing transplants in India. Almost all these transplants have been done from sibling donors.
Number of Leukaemia is increasing globally i.e. approximately 1,04,239 cases in 2010, which is expected to increase up to 1,17,649 in 2015 and 1,32,574 in 2020 (Ref. the ICMR incidence data generated by population-based cancer registries in India). Besides, this each year we would have approximately 20 million carriers and 10,000 children born with Thalassemia Major. The only cure/option remained for these patents are the stem cell transplants. The amount of representation of a particular ethnic or racial group is one of the important factors in finding a matched unrelated donor in these registries. As these antigen/tissue types are inherited, and some are unique to racial or ethnic backgrounds, the greatest chance of locating a donor may come from the same group. A lack of donors of a particular ethnic or racial group makes it more difficult to locate a match. The present study was thus designed to estimate the probability of finding a MUD for patients of Indian origin.
Keeping the above lacunae in mind and with this rapid change (MUD search) there seems to be an urgent need to take the dedicated initiatives to raise the number of volunteer donors to make the suitable HLA–MUD for the patients who do not have the matched sibling donor [6]. For this several countries has generated a database system that share the information and renders the search for MUD easier.
Currently, 71 individual national registries from 51 countries are working together and pooled their HLA donor data to make Bone Marrow Donor Worldwide (BMDW). National registries also have access to this multi-national data of around 22 million HLA typed voluntary donors. At present 2 Indian registries have approximately 33,678 odd Indian donors registered with BMDW [7]. These registries also have the access to Indian donors as well as donors from other countries represented in BMDW database. However, finding a MUD for an Indian patient is still difficult since the number of Indian HLA donors is as low as few thousands in 22 million.
Looking at the current scenario, there is an increase in number of patients seeking MUD transplants. So far there is perhaps no study reported on the probability of finding a MUD in Indian or multi-national database for a prospective MUD transplant recipient. Therefore a simulation study was conducted with actual HLA data of 126 patients with haematological and other disorders. These patients were selected with the criteria of finding a Match Unrelated Donor for their PBSC transplants, as the HLA typing of their siblings and relative does not found to be appropriated for their transplants. Therefore, the search for the Match unrelated donor was initiated using the BMDW database (considering all the volunteer donors typed till October 2013). The study was performed at Bharat Stem Cell, an organization currently working in the area of MUD transplantation [8].
Materials and Methods
Study Type
This was an observational study where HLA data of patients was used to simulate a search in a multi-national/international database. This study was carried out in October 2013 at Bharat Stem Cell (BSC)
Patient HLA Data
The patients who approached BSC for their HLA typing tests and got it done by sequence based typing in an American Society of Haematology and Immunogenetics (ASHI) accredited lab were included in this study.
International Database
The international database against which these searches were simulated was that of BMDW and the study was conducted in the month of October 2013. During the analysis the complete database was considered for the study as it contains the HLA Typing information of all the individuals which are registered till October 2013
Typing Methodology and Resolution
Sequence specific primers (SSP), sequence specific oligonucleotide probes (SSOP) and sequence-based typing (SBT) are few of the methods that have been utilized over the last several years by the HLA scientific community. Due to the limitations faced by former methods (SSP and SOP) in sometimes giving false negative hybridization and lacking in precise allelic typing, the most comprehensive methods engaged for a complete HLA typing is sequence based typing (SBT).
Low resolution represents only the antigenic specificity (for e.g. A: 01), while those with intermediate resolution represents the antigenic and allelic specificity with the help of National Marrow Donor Program (NMDP) bioinformatics code (e.g. A:01:02). High resolution typing denotes antigenic, allelic and sub allelic specificity (for e.g. A: 01:02:02) and therefore considered to be highly reliable for the transplants. For this study only high resolution typing results were considered.
Donor Search Process
While conducting this search, the data of 176 patients was available but only patients’ typed for all the 10 alleles i.e. for HLA-A,-B,-C,-DQB1 and DRB1 by SBT typing (126 patients) were considered. Those with intermediate resolution typing (32) and few patients from outside India (18) were not considered. The MUD search for the identified cases was made using BMDW database. To conduct the search, age, gender, clinical diagnosis and patient HLA data was entered in BMDW database. The search-results were made considering 6/6 and 10/10 match and both for exact (antigenic-allelic-sub allelic) and potential matches (which are not fully typed and may turn out to be fully matched or with some mismatch at the allelic level when typed completely). For the present analysis, the patients were divided into three groups: Group I, Group II and Group III, representing allele, potential and no match respectively. All the necessary information regarding the selected patients have been represented in Table 3.
Table 3.
Representing the geographical distribution, age and other relevant information of the patients selected for study
| S. no. | Data analysis of finding probability for MUD | ||||||
|---|---|---|---|---|---|---|---|
| Potential match | Allele match | ||||||
| G | Age | 6/6 | 10/10 | 6/6 | 10/10 | Comments | |
| 1 | M | 58 | 34 | 34 | 0 | 0 | New Delhi |
| 2 | M | 42 | 8 | 8 | 0 | 0 | Punjab |
| 3 | M | 26 | 2 | 2 | 2 | 2 | New Delhi |
| 4 | M | 17 | 11 | 10 | 0 | 0 | Gurgaon |
| 5 | F | 32 | 14 | 12 | 0 | 0 | Singapore |
| 6 | F | 43 | 2 | 2 | 0 | 0 | Gurgaon |
| 7 | M | 11 | 2 | 1 | 0 | 0 | Patiala |
| 8 | M | 5 | 1 | 1 | 0 | 0 | Gurgaon |
| 9 | M | 0.7 | 11 | 11 | 0 | 0 | New Delhi |
| 10 | M | 8 | 8 | 8 | 0 | 0 | Gujarat |
| 11 | M | 36 | 23 | 23 | 1 | 1 | Jaipur |
| 12 | F | 45 | 0 | 0 | 0 | 0 | New Delhi |
| 13 | M | 26 | 46 | 33 | 1 | 1 | Gurgaon |
| 14 | M | 40 | 26 | 26 | 0 | 0 | UP |
| 15 | M | 7 | 49 | 49 | 0 | 0 | Gurgaon |
| 16 | M | 37 | 3 | 3 | 0 | 0 | New Delhi |
| 17 | M | 46 | 2 | 2 | 0 | 0 | UP |
| 18 | M | 26 | 1 | 1 | 0 | 0 | UP |
| 19 | M | 35 | 0 | 0 | 0 | 0 | Haryana |
| 20 | M | 26 | 46 | 46 | 1 | 1 | Gurgaon |
| 21 | M | 25 | 29 | 29 | 0 | 0 | Sirsa |
| 22 | F | 33 | 5 | 5 | 0 | 0 | Haryana |
| 23 | M | 22 | 0 | 0 | 0 | 0 | New Delhi |
| 24 | F | 40 | 170 | 170 | 1 | 1 | Haryana |
| 25 | M | 38 | 43 | 43 | 1 | 1 | UP |
| 26 | F | 47 | 98 | 98 | 1 | 1 | UK |
| 27 | M | 25 | 9 | 9 | 0 | 0 | Haryana |
| 28 | M | 9 | 196 | 191 | 0 | 0 | UP |
| 29 | M | 0.9 | 11 | 11 | 0 | 0 | UP |
| 30 | M | 58 | 0 | 0 | 0 | 0 | Haryana |
| 31 | F | 57 | 111 | 77 | 4 | 2 | UP |
| 32 | F | 48 | 6 | 6 | 0 | 0 | New Delhi |
| 33 | M | 12 | 120 | 99 | 2 | 2 | Punjab |
| 34 | F | 67 | 35 | 31 | 11 | 9 | New Delhi |
| 35 | M | 55 | 5 | 5 | 0 | 0 | Punjab |
| 36 | M | 18 | no match | no match | no match | no match | Gurgaon |
| 37 | F | 12 | 119 | 75 | 10 | 0 | Rajasthan |
| 38 | M | 9 | 154 | 150 | 10 | 10 | Madurai |
| 39 | M | 43 | 6 | 5 | 0 | 0 | New Delhi |
| 40 | F | 52 | 3 | 3 | 0 | 0 | New Delhi |
| 41 | M | 39 | 24 | 23 | 0 | 0 | Kanpur |
| 42 | M | 37 | 46 | 29 | 1 | 1 | Baran |
| 43 | M | 44 | 12 | 10 | 0 | 0 | Delhi |
| 44 | F | 37 | 0 | 0 | 0 | 0 | Bihar |
| 45 | M | 17 | 5 | 5 | 0 | 0 | New Delhi |
| 46 | F | 39 | 20 | 10 | 0 | 0 | New Delhi |
| 47 | F | 28 | 147 | 135 | 4 | 2 | New Delhi |
| 48 | M | 16 | 19 | 18 | 0 | 0 | New Delhi |
| 49 | M | 8 | 2 | 2 | 0 | 0 | Haryana |
| 50 | M | 28 | 8 | 7 | 0 | 0 | UP |
| 51 | F | 62 | 18 | 17 | 0 | 0 | Tamilnadu |
| 52 | M | 7 | 0 | 0 | 0 | 0 | New Delhi |
| 53 | M | 32 | 18 | 18 | 0 | 0 | Tamilnadu |
| 54 | M | 41 | 19 | 17 | 0 | 0 | Haryana |
| 55 | M | 55 | 45 | 45 | 0 | 0 | New Delhi |
| 56 | F | 30 | 20 | 18 | 0 | 0 | Haryana |
| 57 | M | 35 | 9 | 10 | 0 | 0 | MP |
| 58 | F | 30 | 9 | 7 | 1 | 0 | Noida |
| 59 | M | 7 MONTH | 28 | 28 | 0 | 0 | New Delhi |
| 60 | F | 55 | 8 | 7 | 0 | 0 | Delhi |
| 61 | M | 55 | no match | no match | no match | no match | New Delhi |
| 62 | F | 31 | no match | no match | no match | no match | Narwal |
| 63 | F | 47 | 57 | 42 | 1 | 0 | Haryana |
| 64 | M | 27 | 45 | 33 | 0 | 0 | UP |
| 65 | M | 56 | 89 | 89 | 0 | 0 | Delhi |
| 66 | F | 31 | 7 | 7 | 0 | 0 | Punjab |
| 67 | M | 10 | 84 | 84 | 1 | 1 | Haryana |
| 68 | F | 44 | 148 | 117 | 0 | 0 | New Delhi |
| 69 | M | 38 | 0 | 0 | 0 | 0 | UP |
| 70 | M | 47 | 1 | 1 | 0 | 0 | New Delhi |
| 71 | M | 24 | 0 | 0 | 0 | 0 | |
| 72 | M | 34 | 27 | 1 | 0 | 0 | New Delhi |
| 73 | M | 58 | 1 | 1 | 0 | 0 | New Delhi |
| 74 | F | 13 | 29 | 26 | 0 | 0 | Lucknow |
| 75 | F | 19 | 0 | 0 | 0 | 0 | New Delhi |
| 76 | M | 14 | 2 | 2 | 0 | 0 | New Delhi |
| 77 | M | 27 | 111 | 100 | 1 | 1 | New Delhi |
| 78 | M | 27 | 5 | 5 | 0 | 0 | Haryana |
| 79 | M | 5 | 27 | 24 | 1 | 0 | New Delhi |
| 80 | M | 28 | New Delhi | ||||
| 81 | M | 25 | 16 | 13 | 0 | 0 | Assam |
| 82 | F | 45 | 289 | 2 | 6 | 0 | Rajasthan |
| 83 | F | 50 | no match | no match | no match | no match | Delhi |
| 84 | M | 58 | 26 | 26 | 2 | 2 | Delhi |
| 85 | M | 39 | 9 | 7 | 0 | 0 | Tamilnadu |
| 86 | M | 30 | 252 | 233 | 0 | 0 | New Delhi |
| 87 | M | 41 | 5 | 4 | 0 | 0 | Rajasthan |
| 88 | M | 34 | 397 | 361 | 21 | 3 | Amritsar |
| 89 | F | 32 | 2 | 2 | 0 | 0 | Madhya Pradesh |
| 90 | F | 35 | 2 | 2 | 0 | 0 | Chennai |
| 91 | F | 45 | 3 | 3 | 0 | 0 | UP |
| 92 | M | 57 | 4 | 4 | 0 | 0 | Uttrakhand |
| 93 | F | 20 | 277 | 177 | 7 | 0 | UP |
| 94 | M | 8 | 16 | 15 | 1 | 0 | UP |
| 95 | M | 12 | 3 | 2 | 0 | 0 | Punjab |
| 96 | F | 48 | 119 | 105 | 3 | 0 | Haryana |
| 97 | M | 43 | 39 | 37 | 0 | 0 | Punjab |
| 98 | F | 31 | 1 | 1 | 0 | 0 | Jhalwar |
| 99 | M | 20 | 26 | 19 | 0 | 0 | Madhya Pradesh |
| 100 | M | 1 | 1 | 1 | 2 | 2 | Punjab |
| 101 | M | 21 | 1 | 1 | 0 | 0 | Tamilnadu |
| 102 | M | 44 | no match | no match | no match | no match | UP |
| 103 | M | 26 | 37 | 37 | 0 | 0 | MP |
| 104 | M | 38 | 387 | 5 | 0 | 0 | UP |
| 105 | F | 60 | 8 | 8 | 0 | 0 | Haryana |
| 106 | M | 35 | 70 | 64 | 0 | 0 | Haryana |
| 107 | M | 38 | 10 | 10 | 0 | 0 | Delhi |
| 108 | M | 25 | 12 | 11 | 0 | 0 | Delhi |
| 109 | M | 2 | 0 | 0 | 0 | 0 | West Bengal |
| 110 | F | 11 | 13 | 11 | 0 | 0 | Mahe |
| 111 | M | 27 | 2 | 3 | 0 | 0 | UP |
| 112 | F | 23 | 408 | 408 | 15 | 15 | Delhi |
| 113 | M | 36 | 7 | 7 | 0 | 0 | Pune |
| 114 | M | 16 | 57 | 52 | 0 | 0 | Delhi |
| 115 | M | 19 | 33 | 33 | 0 | 0 | Delhi |
| 116 | M | 8 | 44 | 44 | 0 | 0 | Chennai |
| 117 | F | 13 | 13 | 13 | 0 | 0 | Chennai |
| 118 | M | 3 | 4 | 4 | 0 | 0 | Delhi |
| 119 | M | 4 | 7 | 7 | 0 | 0 | Delhi |
| 120 | M | 8 | 123 | 123 | 0 | 0 | Chennai |
| 121 | F | 32 | 3 | 3 | 0 | 0 | Chennai |
| 122 | M | 66 | 108 | 102 | 2 | 1 | Delhi |
| 123 | M | 21 | 1 | 1 | 0 | 0 | UP |
| 124 | M | 35 | 0 | 0 | 0 | 0 | Delhi |
| 125 | M | 27 | 1 | 1 | 0 | 0 | Haryana |
| 126 | M | 14 | 23 | 23 | 3 | 0 | Haryana |
UP UTTAR PRADESH, UK UTTRAKHAND
This search was conducted between 24th and 27th of October when the total number of registered BMDW donors was 22,55,0071, of which 33,678 were Indian donors shared amongst the two Indian donor registries viz. BSC and Datri [8, 9] with both having the access to BMDW database. There was no chance of change in the number of donors during the study period of four days, as this data was updated on weekly basis (on Tuesday).
Statistical Analysis
The recorded data of the search was subjected to statistical analysis for calculating mean and range. Thereafter, probability and test of significance were also performed using SAS9.1.3.
Results
For the present study the data of 126 patients was used out of which 88 were males with an average age 27 and 38 females with an average age of 31 years (range of-66 and standard deviation-6), were identified and were suffering from various disorders for which HSC transplant is the only curative therapy.
All searches gave the final result of two types: (i). Allele-matched, where all donor alleles exactly match with the alleles of the patient and (ii). Potential match where all alleles of donors corresponding to that of patient were not typed and they could or could not be the match on subsequent confirmatory typing for all alleles.
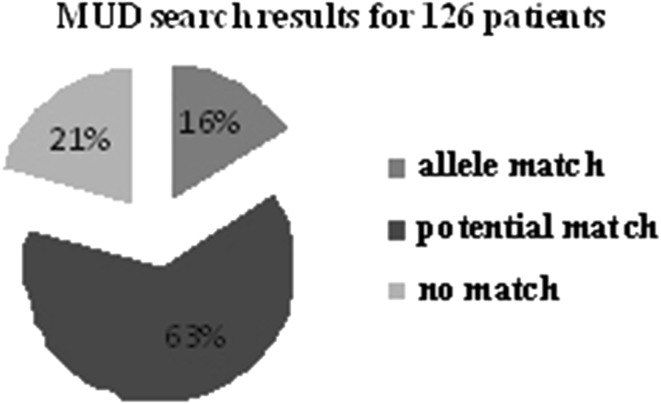
Of the 126 cases selected the allele-matched donor(s) was successfully screened for only 20 (group I) cases (16 %), with the complete allele-matched donors as 59 (using BMDW database) leading to an average of 3 donors (range;1–14) per case. The observed results were communicated to the transplant physician so that they could proceed with the MUD transplants in these cases.
Besides group I, group II contains 80 cases, of few potential matches (n = 1,721) whereas, group III comprises of 26 patients neither have neither an allele-match nor a potential match. This confirms that in group II, if the prospective donors were typed for additional alleles, they could be a probable allele-match. The number of potential matches was statistically higher in the group I (mean; 100) as compared to group II (mean; 21.51) (Table 4).
Table 4.
Representing the probability of finding an allele match for MUD
| Total number of patients- 126 | |||
|---|---|---|---|
| Type of match | Number of patients | ||
| Group I | Allelic match | 20 | |
| 10/10 | 6/6 | ||
| 59 | 2018 | ||
| Group II | Potential match | 80 | |
| 10/10 | 6/6 | ||
| 0 | 1721 | ||
| Group III | No match | 26 | |
| 0 | 0 | 0 | |
By analyzing the data for potential matches (n = 3,739) for group I and II, with the total donors (n = 22,55,0071) in BMDW and the subset of cases (n = 3) with Indian sub-set of donors mentioned in Indian registries in BMDW (n = 33,678) the probability of finding a potential donor is 0.00001 % in the entire database and it comes up to 0.008 % while considering the Indian donors registered in Indian registries.
Discussion
HLA system is considered as one of the most polymorphic and complex set of genetic markers with massive significance in anthropological, immunological and clinical studies [10]. These cell-surface antigens play an important role in the activation of immune-competent cells, thereby promoting immune response. Their extensive polymorphism is associated with a large peptide repertoire for initiating immune responses against a wide range of foreign antigens (pathogens). There are 5,674 HLA alleles detected with wide variability in the HLA B and HLA DRB1 loci.
HLA typing is used to find a compatible match donor for HSC transplant or in fewer instances a bone marrow or cord cell transplant. The implementation of high resolution typed recipient and donor in the clinical practice has shown its clear contribution in improving and achieving the success of transplantation through a better matching [11, 12]. On the other hand the polymorphism of HLA genes turns out to be much higher than anticipated, resulting in larger difficulties in identifying a perfectly matched donor [13].
HLA matching is commonly based on exons 2 and 3 polymorphism for MHC class I loci and on exon 2 polymorphism for class II loci. Their polymorphic nature is contributed due to the reshuffling of gene segments coding for just a few amino acids, proffering it to be a challenging task.
Matching for HLA-A, B, C, DRB1, and DQB1 alleles, a so-called 10/10 match [14] and more recently for HLA-DPB1, are variably preferred as this decreases the risk of acute graft-versus-host disease (aGVHD) and mortality after haematopoietic stem cell transplant [15, 16].
In India we have a large potential load of patients, suffering from thalassaemia major. In such condition stem cell transplant is the only cure, being cost effective than other conventional methods. Fortunately, in India transplant facilities are increasing at an encouraging rate [17–19], but awareness concerning its optimal utilization is still lacking.
While studying the data of MUD transplants carried out in 2006 and 2008 it is very clear that much of these are contributed by China and Japan leaving the India is far behind.
Contrarily, as an HSC donor, ideally a sibling is essential for HSCT source of hematopoietic stem cells is usually from the peripheral blood used for stem cell transplantation (PBSCT). As, reported earlier, the probability of getting a HLA matched donor within a family is extremely low (30–35 %) and difficult as the family sizes are getting smaller [20]. In such circumstances the MUD is required. Smaller family size and unique HLA profile are the two existing limitations occurring in Asia but can be overcome by developing unrelated volunteer marrow donor registries.
Secondly, patients from certain ethnic populations who are poorly represented in BMDW database would not find access to match voluntary HSC donors and therefore would be at a disadvantage as compared to similar patients who belong to populations which are better represented in this database.
To make the search for match unrelated donor (MUD) easy, all over the world efforts have been made, to make unrelated stem cell registries to cater for patients who do not have a compatible family donor and are in need of allogenic stem cell transplantation. Unfortunately, donors of Indian origin are poorly represented in all these registries.
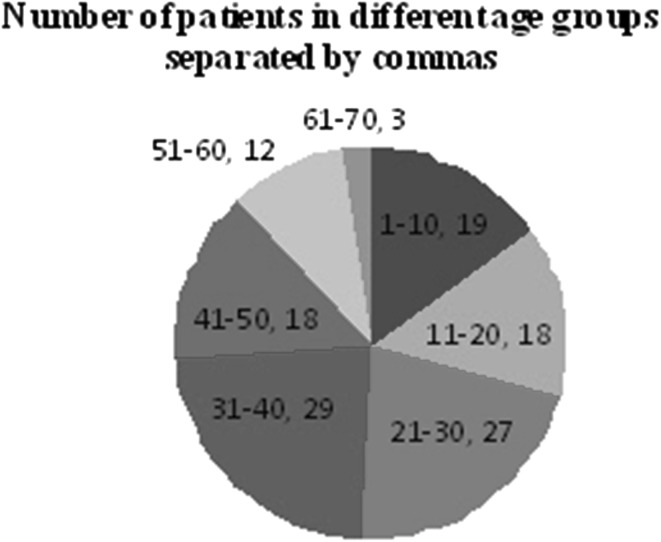
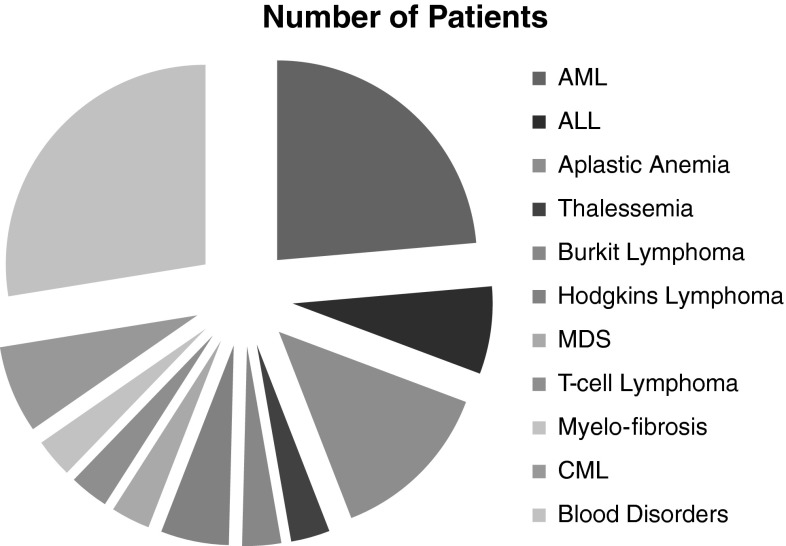
In the current study patients of 10–70 years of age had been identified (Fig. 1) and were suffering blood disorders (Fig. 2), similar results were obtained where the number of allele-matched donors found (n = 59) in a database of 22,55,0071 is very low (Fig. 3) with, the probability of finding an allele match as 0.00026 %.Also this was the first study reported signifying the probability of finding MUD for an Indian patient from Multi-national Human Leukocyte Antigen (HLA) Registry.
Fig. 1.
Representing the number of patients of the relevant age group
Fig. 2.
Denoting the number of patients suffering from various diseases
Fig. 3.
Signifying number of allele match found for (MUD)
However, these registries are heavily biased towards the Caucasian population and are not helpful when an Indian patient needs unrelated donors for various life threatening disease [21].
Based on the NMDP data, it has been notified that “Asian” patients have a two-fold higher probability to have a mismatched donor compared to “Caucasian” patients. In a single centre the donor (7–8/8 match) identification rate was about 90 % for patients classified as “US or European Caucasians”, 76 % for “Hispanics”, 62 % for “Black/African American”, and 33 % for “Asians” [13].
By searching international databases, which contain more than 10 million potential volunteer donors, a matched unrelated donor can be found for an additional 50–80 % of patients, depending upon the ethnic group.
In the present study we have evaluated that probability of finding a donor is 16 % for the patients seeking MUD. This is far less as compared to China or Japan.
The probability of finding the HLA matched unrelated donor, can be increased by studying the HLA polymorphism and halotype frequency distribution amongst different geographical regions, and suggesting that it would have been proper to enlarge the number of donors in the registries in India to resolve this problem This also means that greater is the representation of Indians in Stem Cell Registries, better is the chance of patient finding a match, which seems to be obvious since the HLA makeup of Indian patients is likely to similar to Indian donors with similar gene-pool.
The another important observation drawn from the present study was that while seeking A, B, C, DR, DQ match (10/10 match) and A, B, DR match (6/6 match) for the patients keeping the patient HLA data fixed (all 10 alleles entered) the search results remained similar as most of the registries have majority of their donors typed for only A, B, DR in BMDW database as a fundamental protocol.
Though with the passage time eventually the numbers of donors are increasing but still there is a need to aware the population of India (1.237 billion) that being the second largest in population we are lacking behind in number in these registries making the probability of finding the MUD for an Indian patient exceptionally squat.
Conclusion
With the advent of new technologies which are highly sensitive and specific, the high resolution typing of HLA has gained momentum, leading to a significant success in MUD transplants. However, finding the donor for stem cell transplant is again a difficult proposition, as the population of certain ethnic or racial group which is poorly represented in these registries will find it difficult to find a MUD donor. It has already been specified by the BMDW that of the total Asian population only 11 % is represented in these registries making it difficult to find a MUD for these population. The registries working in the area plays a major role in finding MUD but as the probability of finding a compatible MUD in BMDW depends on race or ethnicity, revealing that there is 60–80 % probability of successfully find allele match MUD donor in their national database/multi-national database system. Contrarily, only 26 % Indians found one or more allele-matched donor(s). The current study experimentally showed the probability of finding an allele match in Indian population is 16 % which greatly emphasizes on increasing the number of Indian donors in these registries.
References
- 1.Gratwohl A, Baldomero H, Aljurf M, et al. Hematopoietic stem cell transplantation: a global perspective. JAMA. 2010;303(16):1617–1624. doi: 10.1001/jama.2010.491. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Gratwohl A, Baldomero H, Gratwohl M, et al. Quantitative and qualitative differences in use and trends of hematopoietic stem cell transplantation: a global observational study. Haematologica. 2013;98(8):1282–1290. doi: 10.3324/haematol.2012.076349. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Xu LP, Huang XJ. Current status and development of hematopoietic stem cell transplantation in China: a report from Chinese Hematopoietic Stem Cell Transplantation Register Group. Chin Med J (Engl) 2011;124(16):2548–2555. [PubMed] [Google Scholar]
- 4.Bone Marrow Donor Worldwide- Annual Report -2012
- 5.Chandy M. Stem cell transplants in India. Bone Marrow Transpl. 2008;42:81–84. doi: 10.1038/bmt.2008.124. [DOI] [PubMed] [Google Scholar]
- 6.Silberstein LE, Jefferies LC. Placental blood banking: a new frontier in transfusion medicine. N Eng J Med. 1996;335:199–201. doi: 10.1056/NEJM199607183350310. [DOI] [PubMed] [Google Scholar]
- 7.Bone Marrow Donor Worldwide [Internet]. Netherlands: Bone Marrow Donor Worldwide; 1989 [cited 2013 February 05]. Available from: http://www.bmdw.org/index.php?id=90
- 8.Bharat Stem Cell Registry [Internet]. India: Bharat Stem Cell Registry; 2012 [cited 2013 February]. Available from: http://www.bharatstemcellregistry.org/
- 9.Datri [Internet]. India: Datri; 2009 [cited 2013 February]. Available from: http://datriworld.org/
- 10.Shankarkumar U, Pawar A, Devaraj JP, Bhupali K, Ghosh K. The HLA system: a review. Anthropol Anz. 2010;6:183–197. [Google Scholar]
- 11.Petersdorf EW. Optimal HLA matching in hematopoietic cell transplantation. Curr Opin in Immunol. 2008;20(5):588–593. doi: 10.1016/j.coi.2008.06.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Shaw BE, Arguello R, Garcia-Sepulveda CA, Madrigal JA. The impact of HLA genotyping on survival following unrelated donor haematopoietic stem cell transplantation: review. Br J Haematol. 2010;150(3):251–258. doi: 10.1111/j.1365-2141.2010.08224.x. [DOI] [PubMed] [Google Scholar]
- 13.Tiercy JM. Unrelated Hematopoietic Stem Cell Donor Matching Probability and Search Algorithm. Bone Marrow Transpl. 2012 doi: 10.1155/2012/695018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Lee SJ, Klein J, Haagenson M, et al. High-resolution donor-recipient HLA matching contributes to the success of unrelated donor marrow transplantation. Blood. 2007;110(13):4576–4583. doi: 10.1182/blood-2007-06-097386. [DOI] [PubMed] [Google Scholar]
- 15.Fleischhauer K, Shaw BE, Gooley T, et al. Effect of T-cell epitope matching at HLADPB1 in recipients of unrelated-donor haematopoietic-cell transplantation : a retrospective study. Lancet Oncology. 2012;13:366–374. doi: 10.1016/S1470-2045(12)70004-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Bettens F, Passweg J, Schanz U, et al. HLA-DPB1 haplotypes on outcome of 10/10 matched unrelated hematopoietic stem cell donor transplantation depends on MHC-linked microsatellite polymorphisms. Biol Blood Marrow Transpl. 2012;18:608–616. doi: 10.1016/j.bbmt.2011.09.011. [DOI] [PubMed] [Google Scholar]
- 17.George B, Mathews V, Srivastava V, et al. Tuberculosis among allogenic bone marrow transplant recipients in India. Bone Marrow Transpl. 2001;27:972–975. doi: 10.1038/sj.bmt.1702993. [DOI] [PubMed] [Google Scholar]
- 18.Saikia TK, Advani SH, Parikh PM, et al. Results of allogenic bone marrow transplant in chronic myeloid leukaemia following conditioning with busulfan and cyclophosphamide. J Assoc Physicians India. 1999;47:770–773. [PubMed] [Google Scholar]
- 19.Rajat K, Venniyoor AJ, Bhardwaj R, et al. Allogenic bone marrow stem cell transplants at Army Hospitals R&R. J Asso Physician India. 2001;49:94. [Google Scholar]
- 20.Rajat K. Stem cell transplant: indian prospective. JIACM. 2002;3(2):182–188. [Google Scholar]
- 21.Gosh K, Shankarkumar U, Mohamty D. Common human leukocyte antigen haplotypes in India: its implications in finding unrelated compatible bone marrow donors. Transfus Med. 2002;12:43–48. doi: 10.1046/j.1365-3148.2002.00351.x. [DOI] [PubMed] [Google Scholar]