Abstract
AIM: To investigate the clinical features of Crohn’s disease (CD) and intestinal tuberculosis (ITB) with a scoring system that we have developed.
METHODS: A total of 25 CD and 40 ITB patients were prospectively enrolled from August 2011 to July 2012. Their characteristics and clinical features were recorded. Laboratory, endoscopic, histologic and radiographic features were determined. The features with a high specificity were selected to establish a scoring system. The features supporting CD scored +1, and those supporting ITB scored -1; each patient received a final total score. A receiver operating characteristic (ROC) curve was used to determine the best cut-off value for distinguishing CD from ITB.
RESULTS: Based on a high specificity of differentiating between CD and ITB, 12 features, including longitudinal ulcers, nodular hyperplasia, cobblestone-like mucosa, intestinal diseases, intestinal fistula, the target sign, the comb sign, night sweats, the purified protein derivative test, the interferon-γ release assay (T-SPOT.TB), ring ulcers and ulcer scars, were selected for the scoring system. The results showed that the average total score of the CD group was 3.12 ± 1.740, the average total score of the ITB group was -2.58 ± 0.984, the best cutoff value for the ROC curve was -0.5, and the diagnostic area under the curve was 0.997, which was statistically significant (P < 0.001). The patients whose total scores were higher than -0.5 were diagnosed with CD; otherwise, patients were diagnosed with ITB. Overall, the diagnostic accuracy rate and misdiagnosis rate of this scoring system were 97% and 3%, respectively.
CONCLUSION: Some clinical features are valuable for CD and ITB diagnosis. The described scoring system is key to differentiating between CD and ITB.
Keywords: Crohn’s disease, Intestinal tuberculosis, Clinical features, Differential diagnosis, Scoring system
Core tip: Using various traditional diagnostic methods and currently emerging techniques, such as computed tomography enterography, this large-sample, prospective study identified specific indicators for differential diagnoses of Crohn’s disease and intestinal tuberculosis and used these indicators to establish a highly valuable scoring system for differential diagnosis.
INTRODUCTION
Crohn’s disease (CD) and intestinal tuberculosis (ITB) are frequently misdiagnosed due to their high similarity in clinical manifestations[1-7]. In spite of new emerging diagnostic techniques and recent advances in the exploration of the pathogenesis of both diseases, the specific diagnostic indicators for a differential diagnosis of those two diseases remain to be further developed.
Both CD and ITB share some symptoms, including abdominal pain, diarrhea, fever and weight loss, but they lack specificity. Lee et al[8] argued that the T-SPOT.TB test (T-SPOT.TB is an interferon-gamma release assay that detects T-cell responses to early secreting antigen target 6 and culture filtrate protein 10 peptides by enzyme-linked immunospot assay for tuberculosis diagnosis. The test is highly sensitive and specific and is not affected by the subject’s immune status or bacillus Calmette-Guerin vaccination.) was highly valuable for the differential diagnosis of both diseases, given that its positive and negative predictive values were 60% and 100%, respectively, for diagnosing ITB. However, large-sample studies are still needed to confirm the diagnostic value of this technique because it has just arrived in China and has failed to be widely promoted. Some scholars believe that longitudinal ulcers, aphthous ulcers and a cobblestone-like appearance are frequently found in typical CD, and circular or linear ulcers, an open ileocecal valve opening and fixed inflammatory polyps are frequently found with an endoscopy in typical ITB[9-11]. However, these specific indicators show low positive rates, and they are atypical findings with endoscopy when used clinically. Both CD and ITB lack specific pathological indicators. Caseous granulomas can be used as the gold standard for the diagnosis of ITB[12], but their low positive rates make early differential diagnoses of both diseases difficult. In recent years, computed tomography enterography (CTE) has been a frequently used technique for the clinical diagnosis of CD. CTE can show abnormalities, the intestinal wall, the intestines and the intestinal mucosa, and contrast-enhanced CTE can also show the involved intestinal segments and the range[13]. However, this technique is just emerging in China, and its diagnostic value requires the same large-sample research and confirmation as T-SPOT.TB.
By using various traditional diagnostic methods and currently emerging techniques, such as T-SPOT.TB and CTE, this prospective study (including sufficient follow-up time) identified specific indicators for the differential diagnosis of CD and ITB and used these indicators to establish a highly valuable scoring system for differential diagnosis.
MATERIALS AND METHODS
Patients with CD or ITB at the gastroenterology outpatient clinic of First Affiliated Hospital of Nanchang University were enrolled from August 2011 to July 2012. All of the patients were newly diagnosed cases in our hospital and were 18-75 years old; CD patients had not received infliximab therapy or AZA/6-MP/MTX, and ITB patients had not received anti-TB treatment. The study was approved by the ethics committee of First Affiliated Hospital of Nanchang University, and informed consent was obtained from all patients.
Patients with CD or ITB who were admitted to the hospital were found in the endoscopy room or as outpatients and were divided into the CD and ITB groups. Their characteristics and clinical features were recorded. Laboratory, endoscopic, histologic and radiographic features were determined. The diagnostic indicators were identified through statistical analyses. The diagnostic indicators with a high specificity were selected to establish a scoring system. Each indicator supporting CD scored +1, and each indicator supporting ITB scored -1. Based on this system, the total score for each patient was calculated, and the best cutoff value for the diagnosis of these two diseases was calculated based on a receiver operating characteristic (ROC) curve. Patients whose total scores were higher than this value were diagnosed with CD; patients with scores lower than this value were diagnosed with ITB. Finally, the accuracy rate and misdiagnosis rate of this scoring system for the diagnosis of these two diseases were calculated.
Active or past TB lesions on chest X-rays and the purified protein derivative (PPD) test could be very helpful in making a differential diagnosis between CD and ITB. In our study, all patients had chest X-rays and PPD tests, but only three patients had positive chest X-rays, which was not statistically significant (P > 0.05). Therefore, we did not select this test to establish our scoring system. There were 41 patients with positive PPD tests, which was statistically significant (P < 0.05), so we selected this test.
For PPD testing, 1 mL tuberculin purified protein derivative and 1 mL physiological saline solution were used. Using a 1-mL syringe, 0.1 mL concentrate was removed and diluted with saline to 0.25 mL, 0.1 mL of which was then intradermally into the medial forearm of the patient. The result is positive (+) if the scleroma diameter is more than 5 mm but less than or equal to 10 mm and positive (++) if the scleroma diameter is more than 10 mm but less than or equal to 20 mm. The test is strongly positive (+++) if the scleroma diameter is more than 20 mm or has local blisters, necrosis or lymphangitis and is negative if the scleroma diameter is less than 5 mm.
Diagnostic criteria for ITB and CD
A diagnosis of CD was made according to the World Health Organization diagnostic criteria based on clinical, radiographic, colonoscopic, and histologic features and the criteria previously established in the literature[14]. A diagnosis of ITB was made according to the following criteria: (1) the identification of Mycobacterium tuberculosis by acid-fast staining or culture of biopsied specimens; (2) the presence of caseating granulomas on histological examination; and (3) an improvement of clinical and endoscopic disease activity after at least 3 mo of anti-TB therapy.
In patients in whom the differentiation between ITB and CD was uncertain, antituberculous therapy was administered for 3 mo, and the final diagnosis was made based on the clinical and endoscopic responses to antituberculous therapy. The clinical response was determined by the loss of subjective symptoms. The endoscopic response was determined by the disappearance of ulcerations.
Statistical analysis
All statistical calculations were performed using SPSS software (SPSS version 17.0; SPSS Inc., Chicago, IL, United States). Measurement data are expressed as the mean ± SD, and variables between the two groups were assessed using the t-test. Count data were assessed using the χ2 test, and rates were expressed as a percentage. The total score data of the scoring system were not normally distributed, and the Wilcoxon test was used. Odds ratio (OR) values were calculated to analyze the relevance of the diagnostic criteria, and the best cutoff value for the diagnosis of these two diseases was calculated based on the ROC curve. P < 0.05 was considered significant.
RESULTS
General CD and ITB information
From August 2011 to July 2012, 80 patients with suspected ITB or CD were prospectively enrolled in this study. Of the 80 patients, 12 were lost to follow-up before the diagnosis was confirmed, and 3 were diagnosed with neither CD nor ITB. Therefore, 40 patients with ITB and 25 patients with CD were analyzed in this study. The differences in gender, age and duration of disease between these two diseases were not statistically significant (P > 0.05). The numbers of students and workers were significantly different between these two disease groups (P < 0.05), but the other jobs were not significantly different between the two groups (P > 0.05) (Table 1).
Table 1.
General information about Crohn’s disease and intestinal tuberculosis n (%)
|
Gender |
Age (yr) | Duration (mo) |
Profession |
||||
| Male | Female | Students and workers | Farmers | Others | |||
| CD, n = 25 | 18 (72) | 7 (28) | 28.57 ± 12.713 | 29.36 ± 42.423 | 15 (60) | 5 (20) | 5 (20) |
| ITB, n = 40 | 21 (53) | 19 (47) | 39.69 ± 13.172 | 17.07 ± 25.624 | 10 (25) | 15 (38) | 15 (38) |
| P value | 0.118 | 0.248 | 0.378 | 0.005 | 0.137 | 0.137 | |
Data are expressed as n (%) or the mean ± SD. CD: Crohn’s disease; ITB: Intestinal tuberculosis.
Clinical manifestations of CD and ITB
Both CD and ITB patients had abdominal pain and weight loss, but night sweats were highly specific for ITB. None of the differences in any of the clinical manifestations were statistically significant between these two diseases (P > 0.05), with the exception of night sweats.
PPD, T-SPOT.TB and biochemical tests of CD and ITB
In this study, the PPD and T-SPOT.TB positive rates were higher in ITB patients than in CD patients. There were 37 PPD-positive cases (93%) and 38 T-SPOT.TB-positive cases (95%) in ITB patients and 4 PPD-positive cases (16%) and 0 T-SPOT.TB-positive cases (0%) in CD patients. Elevated high-sensitivity C-reactive protein (hs-CRP), elevated erythrocyte sedimentation rate (ESR) and decreased serum albumin were more commonly observed in CD patients, with 19 (76%), 21 (84%) and 21 (84%) cases, respectively, whereas there were 18 (45%), 18 (45%) and 21 (53%) cases, respectively, in the ITB group. The differences in all of these indicators were statistically significant between the two diseases (P < 0.05).
Endoscopic findings in CD and ITB
Both CD and ITB patients had multiple irregular ulcers, mainly in the terminal ileum and ileocecal valve. In CD patients, there were 13 (52%) cases of visible longitudinal ulcers (Figure 1A), 4 (16%) cases of aphthous ulcers, 13 (52%) cases of nodular hyperplasia and 6 (24%) cases of cobblestone-like mucosa. In ITB patients, there were 16 (40%) cases of visible ring ulcers (Figure 1B) and 14 (35%) cases of ulcer scars. The difference in aphthous ulcers between these two diseases was not statistically significant (P > 0.05), and the differences in the remaining indicators were statistically significant between these two diseases (P < 0.05).
Figure 1.
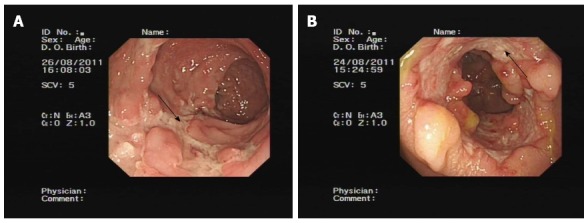
Longitudinal ulcer (A, arrow) and ring ulcer (B, arrow).
Pathological examination of CD and ITB
No caseous granulomas were detected in ITB patients, which is the gold standard for ITB diagnosis. There were patients with granulomas in both groups, including 15 (60%) cases from the CD group and 24 (60%) cases from the ITB group, but none of the granulomas were caseous. None of the differences in pathological indicators were statistically significant between these two diseases (P > 0.05).
CTE in CD and ITB
The CTE could be subjective, so two independent, blinded researchers were chosen to review each CTE. They analyzed the positive results and discussed them with the chief physician if an agreement could not be reached. The CTE results showed that the patients with CD or ITB had thickened bowel walls, so evaluations were performed to examine intestinal fistulas, target signs, comb signs and lymph node enhancement. Intestinal diseases, intestinal fistulas, comb signs (Figure 2) or target signs (Figure 3) were more commonly observed in CD patients, with 19 (76%), 9 (36%), 13 (52%) and 12 (48%) cases, respectively. These findings were significantly different (P < 0.05). There were 8 cases with lymph node enhancement in the ITB group, but this result was not statistically significant (P > 0.05).
Figure 2.
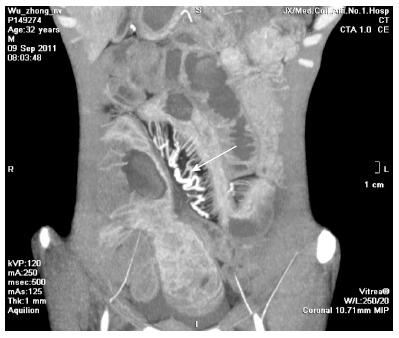
Comb sign (arrow).
Figure 3.
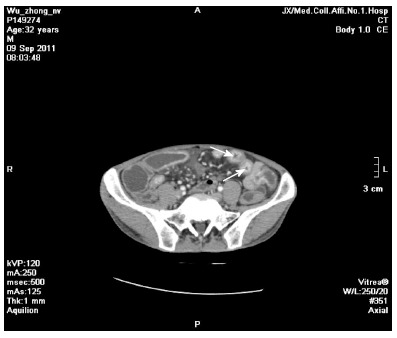
Target sign (arrows).
Value of using indicators for the differential diagnosis of CD and ITB
In our study, the following indicators were valuable for the differential diagnosis of CD or ITB: whether patients were students or workers, hs-CRP, ESR, serum albumin, longitudinal ulcers, nodular hyperplasia, cobblestone-like mucosa, intestinal diseases, intestinal fistulas, target signs, comb signs, night sweats, positive PPD tests, positive T-SPOT.TB tests, ring ulcers and ulcer scars. The OR values of whether patients were students or workers, hs-CRP, ESR, serum albumin, longitudinal ulcers, nodular hyperplasia, cobblestone-like mucosa, intestinal diseases, intestinal fistulas, target signs and comb signs were greater than 1; these indicators were risk factors of CD and were positively correlated with CD. The OR values of night sweats, positive PPD tests, positive T-SPOT.TB tests, ring ulcers, and ulcer scars were less than 1; these indicators were protective factors for CD and were negatively correlated to CD, whereas these indicators were positively correlated to ITB. The sensitivity, specificity, positive predictive value and negative predictive value of these indicators are shown in Table 2.
Table 2.
Value of indicators with Crohn’s disease and intestinal tuberculosis
| Sensitivity | Specificity | Positive predictive value | Negative predictive value | OR (95%CI) | |
| Students and workers | 60% | 75% | 60% | 75% | 4.500 (1.538-13.165) |
| Night sweats | 35% | 92% | 88% | 47% | 0.161 (0.033-0.787) |
| Purified protein derivative | 93% | 84% | 90% | 88% | 0.015 (0.003-0.076) |
| T-SPOT.TB | 95% | 100% | 100% | 93% | 0.050 (0.013-0.193) |
| High-sensitivity C-reactive protein | 76% | 55% | 51% | 79% | 3.870 (1.276-11.735) |
| Erythrocyte sedimentation rate | 84% | 55% | 54% | 85% | 6.417 (1.862-22.117) |
| Serum albumin | 84% | 48% | 50% | 83% | 4.750 (1.380-16.353) |
| Longitudinal ulcer | 52% | 95% | 87% | 76% | 20.583 (4.057-104.428) |
| Ring ulcer | 40% | 96% | 94% | 50% | 0.063 (0.008-0.509) |
| Ulcer scar | 35% | 100% | 100% | 49% | 0.650 (0.518-0.816) |
| Nodular hyperplasia | 52% | 85% | 68% | 74% | 6.139 (1.905-19.729) |
| Cobblestone appearance | 24% | 100% | 100% | 68% | 1.316 (1.056-1.640) |
| Intestinal diseases | 76% | 85% | 76% | 85% | 17.944 (5.074-63.464) |
| Intestinal fistula | 36% | 95% | 82% | 70% | 10.688 (2.074-55.081) |
| Target sign | 52% | 98% | 93% | 76% | 42.250 (4.999-357.089) |
| Comb sign | 48% | 98% | 92% | 75% | 36.000 (4.259-304.265) |
Scoring system for CD and ITB
Of these 16 indicators, 12 with a high specificity were selected to establish the scoring system: longitudinal ulcers, nodular hyperplasia, cobblestone-like mucosa, intestinal diseases, intestinal fistulas, target signs, comb signs, night sweats, positive PPD tests, positive T-SPOT.TB tests, ring ulcers and ulcer scars. The results showed that the average total score of the CD group was 3.12 ± 1.740, the average total score of the ITB group was -2.58 ± 0.984, the best cutoff value for the ROC curve was -0.5, and the diagnostic area under the curve was 0.997, which was statistically significant (P < 0.001). The diagnostic sensitivity and specificity of this scoring system were 100% and 95%, respectively. Patients whose total score was higher than -0.5 were diagnosed with CD; otherwise, they were diagnosed with ITB. The diagnostic accuracy rate and misdiagnosis rate of this scoring system were 97% and 3%, respectively.
DISCUSSION
In this study, CD was prevalent in students and workers, while ITB was prevalent in peasants, which shows that CD may be more prevalent in those who live in more developed regions, while ITB may be more prevalent in those who live in less developed regions. Due to the small sample size in this study, correlations between both diseases and living standards still require further research and confirmation. Gu et al[15] believed that bloody stools were more prevalent in patients with CD and that night sweats were more prevalent in patients with ITB. Although the presence of bloody stools was not confirmed in this study, the presence of night sweats was statistically significant. Night sweats are a typical clinical manifestation of tuberculosis and thus a useful diagnostic indicator in the differential diagnoses of both diseases.
Li et al[16] found that the sensitivity, specificity, positive predictive value and negative predictive value of T-SPOT.TB tests were 84.2%, 75.4%, 50.0% and 94.2%, respectively. Lei et al[17] recently found specificity and positive predictive values that were also very high, which is consistent with the results of the present study. Thus, the T-SPOT.TB test plays a significant role in the differential diagnosis of both diseases. The PPD test was slightly more sensitive than the T-SPOT.TB test in this study, but the specificity of the PPD test was inferior to that of the T-SPOT.TB test, and the results of the PPD test could have been influenced by factors such as the immunity of the organism and previous BCG vaccination. Therefore, the effect of the PPD test was inferior to that of the T-SPOT.TB test. However, the PPD test, which has high sensitivity and specificity, is a helpful tool for the differential diagnosis of both diseases. In this study, the positive rates of increase in patients’ hs-CRP and ESR were higher in CD, and there was greater inflammatory activity in CD. Albumin decreased in both CD and ITB, but the number of cases in which it decreased was greater in CD than in ITB, indicating that patients with CD are likely to have severe dystrophia, which contrasts with previous reports. The differences in ESR and serum albumin results may be related to severe patient conditions, a longer disease course and nutrient consumption in CD as well as to small intestine disease and relatively poor nutrition absorption. Thus, the differential diagnosis values need to be confirmed in further large-sample studies.
Endoscopy is significant for the differential diagnosis of CD or ITB and can be used for response evaluation and follow-up of both diseases. CTE can be used to identify thickened intestinal walls during the active phase of CD and intestinal diseases[18-20], and it is helpful for the differential diagnosis of CD and ITB as well. These diseases have highly specific indicators, such as longitudinal ulcers and ring ulcers on endoscopy and target signs and comb signs on CTE. However, their sensitivities and negative predictive values were not high, which may be related to the low incidence of CD in China and insufficient physician knowledge of endoscopic and CTE manifestations of both diseases. We must increase the sample size in future studies, reinforce learning and improve the diagnosis rate of both diseases using endoscopy and CTE.
The method used to establish the scoring system of specific diagnostic indicators in this study was introduced by Lee et al[21]. Their scoring system was based mainly on 8 specific endoscopic indicators: less than 4 lesions, a deformed ileocecal valve, ring ulcers, ulcer scars, anorectal lesions, longitudinal ulcers, aphthous ulcers and cobblestone appearance. In this study, to build a new scoring system, we added new indicators to the foundational endoscopy indicators, i.e., the PPD test, the T-SPOT.TB test and CTE. Compared with previous reports, there were some differences in the indicators found in this study[2,4,21-24], which might be related to the sample size and to regional disparity. If the studied patients had been diagnosed using the scoring system described by Lee et al[21], 56 of 65 patients would have been diagnosed correctly, 9 would have been misdiagnosed, and the accuracy and the misdiagnosis rate would have been 86% and 14%, respectively. However, the diagnostic accuracy of the scoring system established in this study was 97% for both diseases. Thus, the scoring system established in this study is more valuable than that proposed by Lee et al[21] for the differential diagnosis of CD and ITB.
The scoring system described herein, which was established based on high-specificity features, is valuable for the differential diagnosis of CD and ITB. In view of the small sample size and the equal weights assigned to all diagnostic indicators in this study, gradual improvement could be attained for this scoring system by further increasing the sample size and determining the weights for all diagnostic indicators.
COMMENTS
Background
Crohn’s disease (CD) and intestinal tuberculosis (ITB) are frequently misdiagnosed due to the high similarity of their clinical manifestations. Despite new emerging diagnostic techniques and recent advances in the exploration of the pathogenesis of both diseases, the specific diagnostic indicators for the differential diagnosis of these two diseases remain to be elucidated.
Research frontiers
With the emergence of new diagnostic technology, such as the interferon-γ release assay (T-SPOT.TB test), computed tomography enterography, and magnetic resonance enterography, the diagnostic accuracy of differences between CD and ITB has increased. However, these new methods have either low sensitivity and high specificity or high sensitivity and low specificity. An investigation of the clinical features of CD and ITB using a scoring system is needed.
Innovations and breakthroughs
The aim of this study was to test the differences between CD and ITB using clinical, laboratory, endoscopic, histological and radiographic features. It is suggested that the establishment of a scoring system based on high-specificity features would be valuable for the differential diagnosis of CD and ITB.
Applications
Some clinical features are valuable for the diagnosis of CD and ITB. Establishing a scoring system based on high-specificity features is key to differentiating between CD and ITB.
Peer-review
This prospective study was performed to develop a scoring system to differentiate between CD and ITB. The clinical significance of this type of study seems very high in Asian countries, in which ITB is still prevalent and the incidence of CD is continuously increasing. The authors have engaged this subject, which has been eluding clinicians for a long time, and have compared the results of several important parameters. The authors have found significant results that may be clinically valuable.
Footnotes
Open-Access: This article is an open-access article which was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution Non Commercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: http://creativecommons.org/licenses/by-nc/4.0/
Peer-review started: June 11, 2014
First decision: June 27, 2014
Article in press: January 30, 2015
P- Reviewer: Caviglia R, Desai DC, Pani SP, Yang SK, Ye BD S- Editor: Yu J L- Editor: Wang TQ E- Editor: Wang CH
References
- 1.Pulimood AB, Peter S, Ramakrishna B, Chacko A, Jeyamani R, Jeyaseelan L, Kurian G. Segmental colonoscopic biopsies in the differentiation of ileocolic tuberculosis from Crohn’s disease. J Gastroenterol Hepatol. 2005;20:688–696. doi: 10.1111/j.1440-1746.2005.03814.x. [DOI] [PubMed] [Google Scholar]
- 2.Kirsch R, Pentecost M, Hall Pde M, Epstein DP, Watermeyer G, Friederich PW. Role of colonoscopic biopsy in distinguishing between Crohn’s disease and intestinal tuberculosis. J Clin Pathol. 2006;59:840–844. doi: 10.1136/jcp.2005.032383. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Almadi MA, Ghosh S, Aljebreen AM. Differentiating intestinal tuberculosis from Crohn’s disease: a diagnostic challenge. Am J Gastroenterol. 2009;104:1003–1012. doi: 10.1038/ajg.2008.162. [DOI] [PubMed] [Google Scholar]
- 4.Amarapurkar DN, Patel ND, Rane PS. Diagnosis of Crohn’s disease in India where tuberculosis is widely prevalent. World J Gastroenterol. 2008;14:741–746. doi: 10.3748/wjg.14.741. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Wong WM, Lai KC, Yiu WC, Wong BC, Chan FL, Lai CL. Intestinal tuberculosis mimicking fistulizing Crohn’s disease. J Gastroenterol Hepatol. 2007;22:137–139. doi: 10.1111/j.1440-1746.2006.03311.x. [DOI] [PubMed] [Google Scholar]
- 6.Ouyang Q, Tandon R, Goh KL, Pan GZ, Fock KM, Fiocchi C, Lam SK, Xiao SD. Management consensus of inflammatory bowel disease for the Asia-Pacific region. J Gastroenterol Hepatol. 2006;21:1772–1782. doi: 10.1111/j.1440-1746.2006.04674.x. [DOI] [PubMed] [Google Scholar]
- 7.Shen ZK. The analysis of clinical misdiagnosis about Crohn’s disease in Chinese. Shijie Huaren Xiaohua Zazhi. 2006;14:2460–2463. [Google Scholar]
- 8.Lee JN, Ryu DY, Park SH, You HS, Lee BE, Kim DU, Kim TO, Heo J, Kim GH, Song GA, et al. [The usefulness of in vitro interferon-gamma assay for differential diagnosis between intestinal tuberculosis and Crohns disease] Korean J Gastroenterol. 2010;55:376–383. doi: 10.4166/kjg.2010.55.6.376. [DOI] [PubMed] [Google Scholar]
- 9.Venkatesh PG, Navaneethan U. Mimickers of intestinal tuberculosis: could this be Crohn’s disease? An unsolved enigma. Saudi J Gastroenterol. 2011;17:95–96. doi: 10.4103/1319-3767.77236. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Epstein D, Watermeyer G, Kirsch R. Review article: the diagnosis and management of Crohn’s disease in populations with high-risk rates for tuberculosis. Aliment Pharmacol Ther. 2007;25:1373–1388. doi: 10.1111/j.1365-2036.2007.03332.x. [DOI] [PubMed] [Google Scholar]
- 11.Leighton JA, Shen B, Baron TH, Adler DG, Davila R, Egan JV, Faigel DO, Gan SI, Hirota WK, Lichtenstein D, et al. ASGE guideline: endoscopy in the diagnosis and treatment of inflammatory bowel disease. Gastrointest Endosc. 2006;63:558–565. doi: 10.1016/j.gie.2006.02.005. [DOI] [PubMed] [Google Scholar]
- 12.Sailer J, Peloschek P, Schober E, Schima W, Reinisch W, Vogelsang H, Wunderbaldinger P, Turetschek K. Diagnostic value of CT enteroclysis compared with conventional enteroclysis in patients with Crohn’s disease. AJR Am J Roentgenol. 2005;185:1575–1581. doi: 10.2214/AJR.04.1534. [DOI] [PubMed] [Google Scholar]
- 13.Chatzicostas C, Koutroubakis IE, Tzardi M, Roussomoustakaki M, Prassopoulos P, Kouroumalis EA. Colonic tuberculosis mimicking Crohn’s disease: case report. BMC Gastroenterol. 2002;2:10. doi: 10.1186/1471-230X-2-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Bernstein CN, Fried M, Krabshuis JH, Cohen H, Eliakim R, Fedail S, Gearry R, Goh KL, Hamid S, Khan AG, et al. World Gastroenterology Organization Practice Guidelines for the diagnosis and management of IBD in 2010. Inflamm Bowel Dis. 2010;16:112–124. doi: 10.1002/ibd.21048. [DOI] [PubMed] [Google Scholar]
- 15.Gu Q, Ou YQ, Zhang WY, Li GD. A comparison of clinical and pathologic characteristics between Crohn’s disease and intestinal tuberculosis. Zhonghua Neike Zazhi. 2009;48:291–294. [PubMed] [Google Scholar]
- 16.Li Y, Zhang LF, Liu XQ, Wang L, Wang X, Wang J, Qian JM. The role of in vitro interferonγ-release assay in differentiating intestinal tuberculosis from Crohn’s disease in China. J Crohns Colitis. 2012;6:317–323. doi: 10.1016/j.crohns.2011.09.002. [DOI] [PubMed] [Google Scholar]
- 17.Lei Y, Yi FM, Zhao J, Luckheeram RV, Huang S, Chen M, Huang MF, Li J, Zhou R, Yang GF, et al. Utility of in vitro interferon-γ release assay in differential diagnosis between intestinal tuberculosis and Crohn’s disease. J Dig Dis. 2013;14:68–75. doi: 10.1111/1751-2980.12017. [DOI] [PubMed] [Google Scholar]
- 18.Wu YW, Tao XF, Tang YH, Hao NX, Miao F. Quantitative measures of comb sign in Crohn’s disease: correlation with disease activity and laboratory indications. Abdom Imaging. 2012;37:350–358. doi: 10.1007/s00261-011-9808-8. [DOI] [PubMed] [Google Scholar]
- 19.Ding HY, Zhu XQ, Du C. The applications of multislice CT in the small intestine Crohn’s disease. Fangshexue Shijian. 2009;24:1259. [Google Scholar]
- 20.Booya F, Akram S, Fletcher JG, Huprich JE, Johnson CD, Fidler JL, Barlow JM, Solem CA, Sandborn WJ, Loftus EV. CT enterography and fistulizing Crohn’s disease: clinical benefit and radiographic findings. Abdom Imaging. 2009;34:467–475. doi: 10.1007/s00261-008-9419-1. [DOI] [PubMed] [Google Scholar]
- 21.Lee YJ, Yang SK, Byeon JS, Myung SJ, Chang HS, Hong SS, Kim KJ, Lee GH, Jung HY, Hong WS, et al. Analysis of colonoscopic findings in the differential diagnosis between intestinal tuberculosis and Crohn’s disease. Endoscopy. 2006;38:592–597. doi: 10.1055/s-2006-924996. [DOI] [PubMed] [Google Scholar]
- 22.He Y, Chen MH. The diagnosis and differential diagnosis of Crohn’s disease. Xiandai Xiaohua Ji Jieru Zhenliao. 2010;4:236–240. [Google Scholar]
- 23.Larsson G, Shenoy T, Ramasubramanian R, Balakumaran LK, Småstuen MC, Bjune GA, Moum BA. Routine diagnosis of intestinal tuberculosis and Crohn’s disease in Southern India. World J Gastroenterol. 2014;20:5017–5024. doi: 10.3748/wjg.v20.i17.5017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Chen W, Fan JH, Luo W, Peng P, Su SB. Effectiveness of interferon-gamma release assays for differentiating intestinal tuberculosis from Crohn’s disease: a meta-analysis. World J Gastroenterol. 2013;19:8133–8140. doi: 10.3748/wjg.v19.i44.8133. [DOI] [PMC free article] [PubMed] [Google Scholar]


