Abstract
Limb weakness in amyotrophic lateral sclerosis (ALS) is typically asymmetric. Previous studies have identified an effect of limb dominance on onset and spread of weakness, however relative atrophy of dominant and non-dominant brain regions has not been investigated. Our objective was to use voxel-based morphometry (VBM) to explore gray matter (GM) asymmetry in ALS, in the context of limb dominance. 30 ALS subjects were matched with 17 healthy controls. All subjects were right-handed. Each underwent a structural MRI sequence, from which GM segmentations were generated. Patterns of GM atrophy were assessed in ALS subjects with first weakness in a right-sided limb (n = 15) or left-sided limb (n = 15). Within each group, a voxelwise comparison was also performed between native and mirror GM images, to identify regions of hemispheric GM asymmetry. Subjects with ALS showed disproportionate atrophy of the dominant (left) motor cortex hand area, irrespective of the side of first limb weakness (p < 0.01). Asymmetric atrophy of the left somatosensory cortex and temporal gyri was only observed in ALS subjects with right-sided onset of limb weakness. Our VBM protocol, contrasting native and mirror images, was able to more sensitively detect asymmetric GM pathology in a small cohort, compared with standard methods. These findings indicate particular vulnerability of dominant upper limb representation in ALS, supporting previous clinical studies, and with implications for cortical organisation and selective vulnerability.
Keywords: Motor neuron disease, Amyotrophic lateral sclerosis, Voxel-based morphometry, Asymmetry, Limb dominance
Abbreviations: ALS, amyotrophic lateral sclerosis; VBM, voxel-based morphometry; GM, gray matter; UMN, upper motor neuron; LMN, lower motor neuron
Highlights
-
•
GM asymmetry was assessed, using VBM, in right-handed ALS and control subjects.
-
•
The dominant motor hand area underwent disproportionate atrophy in ALS (p ≤ 0.01).
-
•
In subjects with dominant limb onset, there was greater atrophy of language areas.
-
•
A VBM asymmetry protocol is more sensitive than standard group comparisons.
-
•
Asymmetric vulnerability of cortical GM supports a role for brain development in the pathogenesis of ALS.
1. Introduction
Amyotrophic lateral sclerosis (ALS) is a progressive neurodegenerative condition affecting upper (UMN) and lower motor neurons (LMN) (Kiernan et al., 2011; Turner et al., 2013). Understanding the pathophysiology of ALS is challenging, due to significant variability of clinical phenotype, patient characteristics and disease progression (Chiò et al., 2011; Turner et al., 2013).
Despite this variability, common patterns have been observed across a wide range of ALS subjects. A well-studied example is the “split hand” phenomenon, in which there is disproportionate weakness of the thenar/first dorsal interosseous muscle group (Eisen et al., 2014; Eisen and Kuwabara, 2012). Early weakness of ankle dorsiflexors (Eisen et al., 2014) and speech (Devine et al., 2013) has also been observed. These findings have prompted suggestions that functions which humans have evolved more recently, such as the pincer grip and upright stance, are more susceptible to ALS (Eisen et al., 2014; Eisen, 2009).
Onset of weakness in ALS is also typically asymmetric. However, the factors determining the side of onset and direction of spread remain unclear. Since humans have evolved strong population-wide upper limb dominance (Fitch and Braccini, 2013), it is important to explore this as another potential source of vulnerability in ALS. It has been shown that the dominant upper limb, but not lower limb, is more susceptible to onset of weakness (Turner et al., 2011). We have also described that spread of weakness and UMN signs are affected by dominance, suggesting importance of central factors (Devine et al., 2014).
The aim of this study was to investigate gray matter (GM) asymmetry in ALS, and thus identify regions asymmetrically affected by the disease. Applying voxel-based morphometry (VBM) analysis of structural MRI, we performed direct comparisons between ALS subjects and controls, as well as using a novel asymmetry protocol to assess interhemispheric differences (Rose et al., 2012). Our hypothesis was that this asymmetry protocol would detect patterns of disproportionate atrophy in ALS, which would be affected by whether weakness first occurred in a dominant or non-dominant limb.
2. Materials and methods
2.1. Subjects and recruitment
Ethical approval was obtained from the Royal Brisbane and Women's Hospital (RBWH) Human Research Ethics Committee. All subjects provided written informed consent, and all research was conducted in accordance with the Declaration of Helsinki.
Thirty right-handed subjects were recruited from ALS outpatient clinics at the RBWH (2008–2013). All had diagnoses of clinically probable or definite ALS, according to revised El Escorial criteria (Brooks et al., 2000). We chose to study only right-handed subjects due to their predominance in the population (Meguerditchian et al., 2013), as well as greater uniformity of motor and language lateralisation (Adamo and Taufiq, 2011). Handedness was confirmed using the Edinburgh Handedness Inventory (Oldfield, 1971). Subjects were grouped according to the index limb, defined as the first limb affected by weakness (either the limb of onset, or the first limb affected after bulbar onset) (Devine et al., 2014). Fifteen subjects had a right-sided (dominant) index limb and 15 had a left-sided (non-dominant) index limb. Each subject was administered the ALS Functional Rating Scale—Revised (ALSFRS-R) as a measure of disability. To adjust the degree of disability for the disease duration, we calculated “disease progression” as: (48 − ALSFRS-R score) / (disease duration). Seventeen right-handed healthy controls were closely age and sex-matched with each group of 15 ALS subjects. None of the control or ALS subjects had a history of cerebrovascular events, intracranial pathology, or other neurological diseases.
2.2. MRI acquisition
Each subject underwent an MRI scan acquired with a 3 T Siemens TimTrio (Siemens, Erlangen, Germany), using sequences from VB17 Neuro applications and a 12-channel head coil. A high-resolution structural image was acquired for each subject using a 1 mm3 isotropic 3D T1 MPRAGE (FOV 24 × 25.6 × 17.6 cm, TR/TE/TI 2300/2.26/900 ms, flip angle 9). Slice thickness was 1 mm and image acquisition time was 9:14 min.
2.3. Image processing
Structural images were processed according to the protocol previously reported (Rose et al., 2012). The software package FSL-VBM (Version 4.1), an optimised VBM protocol (Good et al., 2001a) carried out with FSL tools (Smith et al., 2004), was used for all image processing and analysis. The brain was extracted using BET (Smith, 2002). GM segmentation was performed using FAST (Zhang et al., 2001), with the segmentations then aligned to MNI152 standard space using affine registration, FLIRT (Jenkinson and Smith, 2001), followed by non-linear registration using FNIRT (Andersson, 2007). The resulting images were averaged to create a study-specific GM template. Each image was non-linearly re-registered to that template, before being modulated by dividing by the Jacobian determinant of the warp field and smoothed with an isotropic Gaussian kernel (sigma = 4 mm). Mirror images were then generated for each of the smoothed, modulated GM images in standard space, for each of the 47 subjects.
2.4. Statistical analysis
All statistical comparisons were performed using Randomise (Nichols and Holmes, 2002), and adjusted for multiple comparisons using threshold-free cluster enhancement (TFCE) (Smith and Nichols, 2009).
2.4.1. ALS and controls
Firstly, a voxelwise unpaired t-test was performed, comparing the GM density of all ALS subjects (n = 30) with all controls (n = 17). ALS subjects were then subdivided into two groups (15 with a right-sided index limb, and 15 with a left-sided index limb), and each group was compared with 15 age and sex-matched controls. Finally, the ALS subjects with a right-sided index limb were compared directly with those having a left-sided index limb. For each test, age and disease progression were introduced as nuisance covariates.
2.4.2. Asymmetry analysis
In order to identify areas of hemispheric asymmetry, a voxelwise paired t-test was performed between the native and mirror images. This was performed separately for each of the three groups of subjects (17 controls, 15 ALS subjects with a right-sided index limb and 15 with a left-sided index limb). The limb subscore (questions 4–9) of the ALSFRS-R was introduced as a covariate. The anatomical location of each cluster of GM asymmetry was determined using the Talairach Daemon. The threshold for statistical significance was set at p ≤ 0.01 (TFCE-corrected).
3. Results
3.1. ALS and controls
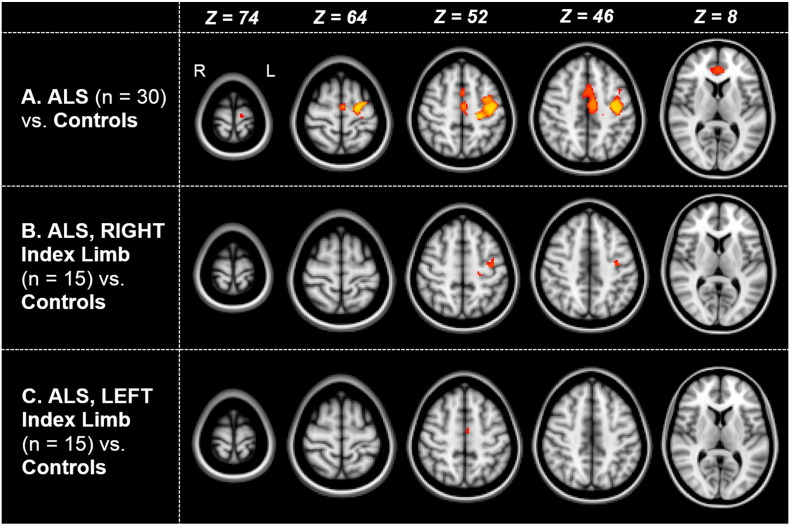
Specific subject characteristics are presented in Table 1. Compared with controls (n = 17), subjects with ALS (n = 30) showed a multifocal cluster of reduced GM density, involving the left precentral gyrus and adjacent regions of the left middle frontal gyrus and bilateral medial frontal gyri (2087 voxels; centre-of-gravity: −22, −11, 52; p ≤ 0.05). There was a separate cluster of reduced GM density involving bilateral anterior cingulate gyri (425 voxels; centre-of-gravity: 1, 39, 6; p ≤ 0.05). These patterns of atrophy are illustrated in Fig. 1A.
Table 1.
Demographics and clinical features of ALS subjects and controls.
| Controls | ALS with Right Index Limb | ALS with Left Index Limb | ||
|---|---|---|---|---|
| Number of subjects | 17 | 15 | 15 | – |
| Handedness (right:left) | 17:0 | 15:0 | 15:0 | – |
| Age (mean ± SD; range) | 56 ± 13 years (33–74 years) |
59 ± 13 years (30–76 years) |
56 ± 11 years (29–73 years) |
– |
| Sex (male:female) | 11M:6F | 11M:4F | 10M:5F | – |
| Sporadic:familial | – | 14:1 | 11:3 | – |
| Onset site | – | • 9 right upper limb • 5 Right lower limb • 1 bulbar |
• 7 left upper limb • 5 left lower limb • 3 bulbar |
– |
| Disease duration, months (mean ± SE; range) | – | 23.8 ± 6.4 months (4–104 months) |
28.7 ± 10.5 months (7–173 months) |
p = 0.69 |
| ALSFRS-R score (mean ± SD) | – | 40 ± 4 | 39 ± 6 | p = 0.58 |
| Disease progressiona (mean ± SE) | – | 0.53 ± 0.08 | 0.55 ± 0.11 | p = 0.93 |
Disease progression = (48 − ALSFRS score) / disease duration.
Fig. 1.
Gray matter atrophy in ALS versus controls. Selected axial plane reconstructions showing regions of reduced GM density in subjects with ALS, compared with controls. Regions of significantly reduced density (p ≤ 0.05, TFCE-corrected) are coloured in orange-yellow. Row A shows a comparison between all ALS subjects (n = 30) and controls (n = 17). Rows B and C show the patterns of atrophy in ALS subjects with a right-sided or left-sided index limb, respectively (n = 15 in each group).
Across all 47 subjects, there was a negative correlation (p ≤ 0.05) between age and GM density in widespread regions of the frontal, parietal, temporal and occipital lobes, representative of age-related atrophy. However, there was no confounding effect of age or disease progression on the patterns of atrophy in ALS.
3.2. ALS (according to index limb) and controls
As illustrated in Fig. 1B, ALS subjects with a right (dominant) index limb (n = 15) showed patchy reductions in GM density affecting the left precentral gyrus, at a threshold of p ≤ 0.05. These changes were not significant at a higher threshold of p ≤ 0.01. Subjects with a left (non-dominant) index limb (n = 15) did not demonstrate any significant reductions in GM density at either the left or right precentral gyri at a threshold of p ≤ 0.05 (Fig. 1C).
Direct voxelwise comparison between ALS subjects with either a right or left index limb also did not reveal any significant differences in GM density.
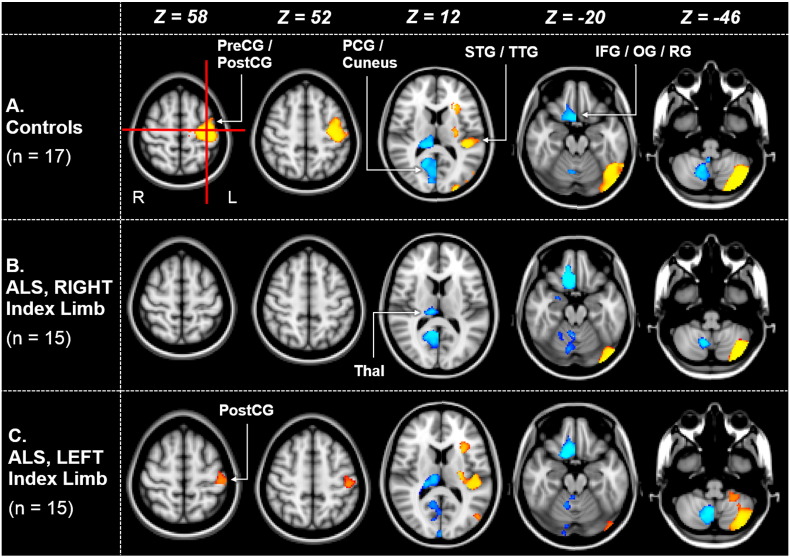
3.3. GM asymmetry in controls
In the 17 right-handed control subjects, multiple statistical clusters of both rightward and leftward asymmetries were identified (Table 2, Fig. 2A). Of particular note was an area of leftward asymmetry (p ≤ 0.01) encompassing a dorsolateral region of the precentral and postcentral gyri. This area corresponded closely with the centre-of-gravity of the dominant thenar representation area, previously defined using transcranial magnetic stimulation (TMS) (Niskanen et al., 2010). Control subjects also demonstrated significant leftward asymmetry of a region of the superior and transverse temporal gyri, adjacent to the Sylvian fissure. There were no significant asymmetries of lower limb or bulbar representation areas, indicating that these regions were of a similar density in the right and left hemispheres.
Table 2.
Statistical clusters of GM asymmetry in controls and ALS subjects.
|
Cluster Centre of Gravity (MNI) |
GM Regions Encompassed | Cluster Size (voxels)a |
T-valueb |
|||
|---|---|---|---|---|---|---|
| x | y | z | ||||
|
Controls (n = 17) |
Leftward Asymmetries (L hemisphere > R hemisphere) | |||||
| -39 | -74 | -26 | • Cerebellum (posterolateral) • Occipital lobe (posterolateral) |
5523 | 12.3 | |
| -34 | -14 | 35 | • Precentral gyrus (dorsolateral) • Postcentral gyrus (dorsolateral) • Superior and transverse temporal gyri • Anterior insula |
4120 | 9.6 | |
| Rightward Asymmetries (R hemisphere > L hemisphere) | ||||||
| 11 | -53 | 12 | • Posterior thalamus • Posterior cingulate gyrus • Cuneus and precuneus |
2007 | 10.9 | |
| 9 | -61 | -40 | • Cerebellum (inferomedial) | 1334 | 10.1 | |
| 12 | 15 | -17 | • Inferior frontal, rectal and orbital gyri | 452 | 8.2 | |
|
ALS with Right Index Limb (n = 15) |
Leftward Asymmetries (L hemisphere > R hemisphere) | |||||
| -39 | -73 | -32 | • Cerebellum (posterolateral) • Occipital lobe (posterolateral) |
2938 | 10.7 | |
| Rightward Asymmetries (R hemisphere > L hemisphere) | ||||||
| 10 | -65 | -28 | • Cerebellum (inferomedial) | 1791 | 9.4 | |
| 13 | 19 | -18 | • Inferior frontal, rectal and orbital gyri | 1011 | 12.4 | |
| 10 | -62 | 13 | • Posterior cingulate gyrus • Cuneus and precuneus |
769 | 8.5 | |
| 12 | -27 | 6 | • Posterior thalamus | 452 | 6.9 | |
|
ALS with Left Index Limb (n = 15) |
Leftward Asymmetries (L hemisphere > R hemisphere) | |||||
| -34 | -67 | -44 | • Cerebellum (posterolateral) | 2285 | 7.5 | |
| -42 | -25 | 13 | • Superior and transverse temporal gyri | 971 | 9.0 | |
| -47 | -77 | -6 | • Occipital lobe (posterolateral) | 617 | 9.7 | |
| -29 | 19 | 4 | • Anterior insula | 609 | 7.3 | |
| -29 | 40 | 30 | • Middle frontal gyrus | 498 | 7.5 | |
| -47 | -23 | 55 | • Postcentral gyrus (dorsolateral) | 185 | 6.9 | |
| Rightward Asymmetries (R hemisphere > L hemisphere) | ||||||
| 10 | -68 | -17 | • Cerebellum (inferomedial) • Posterior cingulate gyrus • Cuneus and precuneus |
3564 | 9.3 | |
| 13 | 18 | -18 | • Inferior frontal, rectal and orbital gyri | 556 | 10.3 | |
| 13 | -24 | 10 | • Posterior thalamus | 550 | 8.2 | |
Only clusters of ≥180 voxels are reported.
All regions are significant, after correction for multiple comparisons (TFCE), at a threshold of p ≤ 0.01.
Fig. 2.
Patterns of gray matter asymmetry in ALS and control subjects. Selected axial plane reconstructions from 17 right-handed controls (Row A), 15 ALS subjects with a right-sided index limb (Row B), and 15 ALS subjects with a left-sided index limb (Row C). Significant regions of GM asymmetry (p ≤ 0.01, TFCE-corrected) are shown. Regions coloured in orange-yellow represent leftward asymmetry (i.e. higher GM density in the left hemisphere), whereas blue clusters signify rightward asymmetry. In control subjects, there is a cluster of leftward GM asymmetry which incorporates the centre-of-gravity of the dominant thenar representation area (shown by the intersection of the two red lines). PreCG = precentral gyrus; PostCG = postcentral gyrus; PCG = posterior cingulate gyrus; STG = superior temporal gyrus; TTG = transverse temporal gyrus; IFG = inferior frontal gyrus; OG = orbital gyrus; RG = rectal gyrus; Thal = thalamus.
3.4. GM asymmetry in ALS
In the 15 ALS subjects with a right-sided (dominant) index limb, there was complete absence of leftward asymmetry at the precentral gyrus hand representation area, at the threshold of p ≤ 0.01 (Table 2, Fig. 2B). This indicated disproportionate loss of GM supplying the dominant hand, relative to the remainder of the bilateral motor strip (including lower limb and bulbar representation areas). Leftward asymmetry was also lost at the adjacent region of the postcentral gyrus, as well as the superior and transverse temporal gyri and anterior insula.
In contrast, leftward asymmetry of the dorsolateral postcentral gyrus, superior and transverse temporal gyri and anterior insula was preserved in the 15 ALS subjects with a left-sided (non-dominant) index limb (Table 2, Fig. 2C). However, these subjects still showed complete absence of leftward asymmetry at the precentral gyrus hand representation area. This disproportionate loss of GM density in the left motor cortex occurred despite first weakness occurring in a limb controlled by the right hemisphere. These subjects also demonstrated a new cluster of leftward asymmetry involving the middle frontal gyrus (MFG), which was not present in controls (Table 2). This may indicate either relative gain of GM density at the left MFG or GM loss at the right MFG, with the latter favoured.
Other regions of GM asymmetry were preserved across all ALS subjects and controls. These included rightward asymmetry of the inferior frontal, rectal and orbital gyri, posterior thalamus, posterior cingulate gyrus and cuneus, and leftward asymmetry of the posterolateral cerebellum and occipital lobes. Several of these regions, including rightward asymmetry of the antero-inferior frontal lobes and leftward asymmetry of the occipital lobes, have been previously reported in larger populations of healthy subjects (Toga and Thompson, 2003; Watkins et al., 2001).
4. Discussion
The objective of this study was to identify ALS-related changes to the normal patterns of GM asymmetry, and interpret these in the context of limb dominance. We have established that a VBM asymmetry protocol applied to structural T1 MRI (Rose et al., 2012) is a useful tool for assessing GM changes in both healthy and disease states, especially in smaller cohorts in which standard voxelwise comparisons are less sensitive. Using this protocol, we found that right-handed ALS subjects with dominant limb onset disproportionately lost GM in left hemispheric sensorimotor (upper limb representation) and language regions. However, unlike other regions, disproportionate atrophy of the left motor cortical hand area occurred independent of whether onset of weakness was in a dominant or non-dominant limb. These findings support previous clinical studies of ALS laterality, and have implications for cortical organisation, its evolution, and selective vulnerability.
Multiple large studies have demonstrated motor cortical atrophy in ALS, which may initially be left-hemisphere predominant (Menke et al., 2014). Furthermore, motor impairment has been shown to be focal, using both clinical examination (Ravits et al., 2007) and neuroimaging (Bede et al., 2013). However, in the current study, major differences between ALS and controls were only apparent when analysing all 30 subjects together, and at a more relaxed statistical threshold (p ≤ 0.05). Comparisons involving 15 ALS subjects only detected minor, patchy reductions in motor cortical GM density, and were unable to differentiate subjects with right or left-sided disease onset. In contrast, the VBM asymmetry protocol was sufficiently powered to identify differences in GM between the two clinical groups of ALS subjects, at a stricter threshold (p ≤ 0.01). Therefore, this method is ideal for exposing subtle asymmetric changes in less common diseases such as ALS.
Despite previous authors correlating the size or density of motor areas with handedness (Hervé et al., 2006; Rose et al., 2012; Takao et al., 2011), some have not demonstrated this (Good et al., 2001b). In the current study, we defined a significant cluster of leftward GM asymmetry in right-handed controls, incorporating the cortical hand representation area. This indicates greater size and complexity of this area in the left hemisphere. In contrast, the absence of this asymmetry across all right-handed ALS subjects suggests that the left hemisphere hand area disproportionately loses GM density relative to the remainder of the bilateral motor cortex. Our results also suggest that this region of motor cortex is particularly vulnerable to atrophy, regardless of whether the patient or clinician had noticed first weakness in a right or left-sided limb.
Vulnerability of the dominant upper limb in ALS has been previously described using history and clinical examination (Devine et al., 2014; Turner et al., 2011). Our study provides neuroimaging evidence to support this phenomenon, and suggests an important role for central factors in driving this effect. Our findings also confirm the lack of preferential involvement of either lower limb, which has been observed clinically (Turner et al., 2011). It has been proposed that certain functions, such as the “split hand”, are more vulnerable to the pathology of ALS due to more recent development in human evolution (Eisen et al., 2014). Another key feature of human development has been a population-wide bias toward right-handedness (Fitch and Braccini, 2013), which is likely to have been facilitated by the onset of upright gait (Meguerditchian et al., 2013). The current results suggest that the increased complexity of left hemispheric motor networks in right-handers may lead to greater susceptibility to ALS. The cause of neuronal vulnerability in ALS remains unknown, although potential contributory factors include cellular density, excitability, and hormonal influences (Amunts et al., 1996; Bäumer et al., 2007; Vivekananda et al., 2011).
In our study, subjects with dominant limb onset of weakness also showed disproportionate atrophy of areas involved in language and communication (left superior and transverse temporal gyri). It is known that 98% of right-handers have left hemispheric language lateralisation (Adamo and Taufiq, 2011). Although these subjects did not undergo formal cognitive testing, this finding may reflect the occurrence of language dysfunction as part of the ALS–FTD spectrum, including milder language deficits in subjects without frank dementia (Taylor et al., 2013). Alternatively, some authors have proposed that the dominant upper limb and speech form a single network for communication, with gestures and vocalisations being linked (Gentilucci et al., 2008; Meguerditchian et al., 2013).
This study has limitations. Due to the current cohort being restricted to right-handers, we were unable to assess changes to GM asymmetry in left-handed or ambidextrous subjects. However, this would require recruitment of a larger cohort, since hemispheric lateralisation of motor and language is less predictable in non-right-handed individuals (Adamo and Taufiq, 2011). The size of our cohort also limited the ability to separately analyse smaller subgroups, for example only those subjects with upper limb onset of weakness. Formal neuropsychological testing was also not performed, therefore the cognitive correlates of some changes (such as those affecting the left frontal and bilateral cingulate gyri) remain unclear. Finally, it remains to be seen whether the current results can be translated to individual subjects, for example in a diagnostic setting.
Overall, this study provides evidence that certain areas of GM are disproportionately and asymmetrically vulnerable to the pathology of ALS, and that these regions can be identified using a sensitive VBM protocol. In particular, we have identified the dominant hand area as being particularly susceptible to atrophy, supporting previous history and examination-based studies. This finding warrants further investigation, including assessment of associated white matter asymmetry using diffusion tensor imaging.
Conflicts of interest
The authors have no competing interests to declare.
Acknowledgements
We would like to acknowledge Nicole Hutchinson, Helen Woodhouse and Susan Heggie from the RBWH ALS outpatient clinics, as well as the MRI radiography staff in the RBWH Department of Medical Imaging. We thank the Royal Brisbane and Women's Hospital Foundation for providing funding for this study. The Foundation was not involved in study design, data analysis and interpretation, nor manuscript preparation.
References
- Adamo D.E., Taufiq A. Establishing hand preference: why does it matter? Hand (N Y) 2011;6(3):295–303. doi: 10.1007/s11552-011-9324-x. 22942854 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Amunts K., Schlaug G., Schleicher A. Asymmetry in the human motor cortex and handedness. Neuroimage. 1996;4(3 1):216–222. doi: 10.1006/nimg.1996.0073. 9345512 [DOI] [PubMed] [Google Scholar]
- Andersson J. 2007. Non-linear Optimisation [Online] Available at: http://www.fmrib.ox.ac.uk/analysis/techrep. Accessed January 01, 2014. [Google Scholar]
- Bäumer T., Dammann E., Bock F., Klöppel S., Siebner H.R., Münchau A. Laterality of interhemispheric inhibition depends on handedness. Exp. Brain Res. 2007;180(2):195–203. doi: 10.1007/s00221-007-0866-7. 17287992 [DOI] [PubMed] [Google Scholar]
- Bede P., Bokde A., Elamin M. Grey matter correlates of clinical variables in amyotrophic lateral sclerosis (ALS): a neuroimaging study of ALS motor phenotype heterogeneity and cortical focality. J. Neurol. Neurosurg. Psychiatry. 2013;84(7):766–773. doi: 10.1136/jnnp-2012-302674. 23085933 [DOI] [PubMed] [Google Scholar]
- Brooks B.R., Miller R.G., Swash M. El Escorial revisited: revised criteria for the diagnosis of amyotrophic lateral sclerosis. Amyotroph. Lateral Scler. Other Motor Neuron Disord. 2000;1(5):293–299. doi: 10.1080/146608200300079536. 11464847 [DOI] [PubMed] [Google Scholar]
- Chiò A., Calvo A., Moglia C., Mazzini L., Mora G., PARALS Study Group Phenotypic heterogeneity of amyotrophic lateral sclerosis: a population based study. J. Neurol. Neurosurg. Psychiatry. 2011;82(7):740–746. doi: 10.1136/jnnp.2010.235952. 21402743 [DOI] [PubMed] [Google Scholar]
- Devine M.S., Farrell A., Woodhouse H., McCombe P.A., Henderson R.D. A developmental perspective on bulbar involvement in amyotrophic lateral sclerosis. Amyotroph. Lateral Scler. Frontotemporal Degener. 2013;14(7–8):638–639. doi: 10.3109/21678421.2013.812663. 23859502 [DOI] [PubMed] [Google Scholar]
- Devine M.S., Kiernan M.C., Heggie S., McCombe P.A., Henderson R.D. Study of motor asymmetry in ALS indicates an effect of limb dominance on onset and spread of weakness, and an important role for upper motor neurons. Amyotroph. Lateral Scler. Frontotemporal Degener. 2014;15(7–8):481–487. doi: 10.3109/21678421.2014.906617. 24809721 [DOI] [PubMed] [Google Scholar]
- Eisen A. Amyotrophic lateral sclerosis — evolutionary and other perspectives. Muscle Nerve. 2009;40(2):297–304. doi: 10.1002/mus.21404. 19609920 [DOI] [PubMed] [Google Scholar]
- Eisen A., Kuwabara S. The split hand syndrome in amyotrophic lateral sclerosis. J. Neurol. Neurosurg. Psychiatry. 2012;83(4):399–403. doi: 10.1136/jnnp-2011-301456. 22100761 [DOI] [PubMed] [Google Scholar]
- Eisen A., Turner M.R., Lemon R. Tools and talk: an evolutionary perspective on the functional deficits associated with amyotrophic lateral sclerosis. Muscle Nerve. 2014;49(4):469–477. doi: 10.1002/mus.24132. 24273101 [DOI] [PubMed] [Google Scholar]
- Fitch W.T., Braccini S.N. Primate laterality and the biology and evolution of human handedness: a review and synthesis. Ann. N. Y. Acad. Sci. 2013;1288:70–85. doi: 10.1111/nyas.12071. 23631481 [DOI] [PubMed] [Google Scholar]
- Gentilucci M., Dalla Volta R., Gianelli C. When the hands speak. J. Physiol. Paris. 2008;102(1–3):21–30. doi: 10.1016/j.jphysparis.2008.03.002. 18440209 [DOI] [PubMed] [Google Scholar]
- Good C.D., Johnsrude I., Ashburner J., Henson R.N., Friston K.J., Frackowiak R.S. Cerebral asymmetry and the effects of sex and handedness on brain structure: a voxel-based morphometric analysis of 465 normal adult human brains. Neuroimage. 2001;14(3):685–700. doi: 10.1006/nimg.2001.0857. 11506541 [DOI] [PubMed] [Google Scholar]
- Good C.D., Johnsrude I.S., Ashburner J., Henson R.N.A., Friston K.J., Frackowiak R.S.J. A voxel-based morphometric study of ageing in 465 normal adult human brains. Neuroimage. 2001;14(1):21–36. doi: 10.1006/nimg.2001.0786. [DOI] [PubMed] [Google Scholar]
- Hervé P.Y., Crivello F., Perchey G., Mazoyer B., Tzourio-Mazoyer N. Handedness and cerebral anatomical asymmetries in young adult males. Neuroimage. 2006;29(4):1066–1079. doi: 10.1016/j.neuroimage.2005.08.031. 16198126 [DOI] [PubMed] [Google Scholar]
- Jenkinson M., Smith S. A global optimisation method for robust affine registration of brain images. Med. Image Anal. 2001;5(2):143–156. doi: 10.1016/s1361-8415(01)00036-6. 11516708 [DOI] [PubMed] [Google Scholar]
- Kiernan M.C., Vucic S., Cheah B.C. Amyotrophic lateral sclerosis. Lancet. 2011;377(9769):942–955. doi: 10.1016/S0140-6736(10)61156-7. 21296405 [DOI] [PubMed] [Google Scholar]
- Meguerditchian A., Vauclair J., Hopkins W.D. On the origins of human handedness and language: a comparative review of hand preferences for bimanual coordinated actions and gestural communication in nonhuman primates. Dev. Psychobiol. 2013;55(6):637–650. doi: 10.1002/dev.21150. 23955015 [DOI] [PubMed] [Google Scholar]
- Menke R.A., Körner S., Filippini N. Widespread grey matter pathology dominates the longitudinal cerebral MRI and clinical landscape of amyotrophic lateral sclerosis. Brain. 2014;137(9):2546–2555. doi: 10.1093/brain/awu162. 24951638 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nichols T.E., Holmes A.P. Nonparametric permutation tests for functional neuroimaging: a primer with examples. Hum. Brain Mapp. 2002;15(1):1–25. doi: 10.1002/hbm.1058. 11747097 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Niskanen E., Julkunen P., Säisänen L. Group-level variations in motor representation areas of thenar and anterior tibial muscles: Navigated Transcranial Magnetic Stimulation Study. Hum. Brain Mapp. 2010;31(8):1272–1280. doi: 10.1002/hbm.20942. 20082330 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Oldfield R.C. The assessment and analysis of handedness: the Edinburgh inventory. Neuropsychologia. 1971;9(1):97–113. doi: 10.1016/0028-3932(71)90067-4. 5146491 [DOI] [PubMed] [Google Scholar]
- Ravits J., Paul P., Jorg C. Focality of upper and lower motor neuron degeneration at the clinical onset of ALS. Neurology. 2007;68(19):1571–1575. doi: 10.1212/01.wnl.0000260965.20021.47. 17485643 [DOI] [PubMed] [Google Scholar]
- Rose S., Rowland T., Pannek K. Structural hemispheric asymmetries in the human precentral gyrus hand representation. Neuroscience. 2012;210:211–221. doi: 10.1016/j.neuroscience.2012.02.044. 22433295 [DOI] [PubMed] [Google Scholar]
- Smith S.M. Fast robust automated brain extraction. Hum. Brain Mapp. 2002;17(3):143–155. doi: 10.1002/hbm.10062. 12391568 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smith S.M., Jenkinson M., Woolrich M.W. Advances in functional and structural MR image analysis and implementation as FSL. Neuroimage. 2004;23(Suppl. 1):S208–S219. doi: 10.1016/j.neuroimage.2004.07.051. 15501092 [DOI] [PubMed] [Google Scholar]
- Smith S.M., Nichols T.E. Threshold-free cluster enhancement: addressing problems of smoothing, threshold dependence and localisation in cluster inference. Neuroimage. 2009;44(1):83–98. doi: 10.1016/j.neuroimage.2008.03.061. 18501637 [DOI] [PubMed] [Google Scholar]
- Takao H., Abe O., Yamasue H., Aoki S., Sasaki H., Kasai K. Gray and white matter asymmetries in healthy individuals aged 21–29 years: a voxel-based morphometry and diffusion tensor imaging study. Hum. Brain Mapp. 2011;32(10):1762–1773. doi: 10.1002/hbm.21145. 20886579 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Taylor L.J., Brown R.G., Tsermentseli S. Is language impairment more common than executive dysfunction in amyotrophic lateral sclerosis? J. Neurol. Neurosurg. Psychiatry. 2013;84(5):494–498. doi: 10.1136/jnnp-2012-303526. 23033353 [DOI] [PubMed] [Google Scholar]
- Toga A.W., Thompson P.M. Mapping brain asymmetry. Nat. Rev. Neurosci. 2003;4(1):37–48. doi: 10.1038/nrn1009. 12511860 [DOI] [PubMed] [Google Scholar]
- Turner M.R., Hardiman O., Benatar M. Controversies and priorities in amyotrophic lateral sclerosis. Lancet Neurol. 2013;12(3):310–322. doi: 10.1016/S1474-4422(13)70036-X. 23415570 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Turner M.R., Wicks P., Brownstein C.A. Concordance between site of onset and limb dominance in amyotrophic lateral sclerosis. J. Neurol. Neurosurg. Psychiatry. 2011;82(8):853–854. doi: 10.1136/jnnp.2010.208413. 20562391 [DOI] [PubMed] [Google Scholar]
- Vivekananda U., Manjalay Z.R., Ganesalingam J. Low index-to-ring finger length ratio in sporadic ALS supports prenatally defined motor neuronal vulnerability. J. Neurol. Neurosurg. Psychiatry. 2011;82(6):635–637. doi: 10.1136/jnnp.2010.237412. 21551173 [DOI] [PubMed] [Google Scholar]
- Watkins K.E., Paus T., Lerch J.P. Structural asymmetries in the human brain: a voxel-based statistical analysis of 142 MRI scans. Cereb. Cortex. 2001;11(9):868–877. doi: 10.1093/cercor/11.9.868. 11532891 [DOI] [PubMed] [Google Scholar]
- Zhang Y., Brady M., Smith S. Segmentation of brain MR images through a hidden Markov random field model and the expectation–maximization algorithm. I. E.E.E. Trans. Med. Imaging. 2001;20(1):45–57. doi: 10.1109/42.906424. 11293691 [DOI] [PubMed] [Google Scholar]