Abstract
Background
Echocardiography, though non-invasive and having relatively low-cost, presents issues of variability which can limit its use in epidemiological studies.
Objective
To evaluate left ventricular mass reproducibility when assessed at acquisition (online) compared to when assessed at a reading center after electronic transmission (offline) and also when assessed by different readers at the reading center.
Methods
Echocardiographers from the 6 ELSA-Brasil study investigation centers measured the left ventricular mass online during the acquisition from 124 studies before transmitting to the reading center, where studies were read according to the study protocol. Half of these studies were blindly read by a second reader in the reading center.
Results
From the 124 echocardiograms, 5 (4%) were considered not measurable. Among the remaining 119, 72 (61%) were women, mean age was 50.2 ± 7.0 years and 2 had structural myocardial abnormalities. Images were considered to be optimal/ good by the reading center for 110 (92.4%) cases. No significant difference existed between online and offline measurements (1,29 g, CI 95% −3.60-6.19), and the intraclass correlation coefficient between them was 0.79 (CI 95% 0.71-0.85). For images read by two readers, the intraclass correlation coefficient was 0.86 (CI 95% 0.78-0.91).
Conclusion
There were no significant drifts between online and offline left ventricular mass measurements, and reproducibility was similar to that described in previous studies. Central quantitative assessment of echocardiographic studies in reading centers, as performed in the ELSA-Brasil study, is feasible and useful in clinical and epidemiological studies performed in our setting.
Keywords: Hypertrophy Left Ventricular, Echocardiography, Dimensional Measurement Accuracy, Multicenter Studies, Reproducibiity of Results
Introduction
Echocardiography is the most used noninvasive imaging method in clinical cardiology for functional and structural evaluation, and it is also employed in clinical and epidemiological research1-4. Left ventricular hypertrophy is a condition that can be measured by echocardiography and is used in clinical practice as a predictor of cardiovascular events2. Although echocardiography is the cheapest and most accessible cardiovascular imaging method, its use in epidemiological studies is limited owing to the difficulty in obtaining good-quality images for all individuals and the variability among repeated measurements5-7.
The assessment of the variability of the left ventricular mass (LVM) is important to ensure the quality control of echocardiographic measurements. In addition, it can be performed in the clinical setting and integrates several measurements acquired during examination. Notably, its calculation method may potentially cause errors in the LVM estimate with a magnitude of 10E3.
To ensure more precise and accurate measurements, the American Society of Echocardiography defends a centralized reading of echocardiography exams in multicenter trials8. This is recommended because it has been shown that echocardiography exams performed locally have a lower prognostic impact than those performed in a central laboratory9. These recommendations were implemented in the Brazilian Longitudinal Study of Adult Health (ELSA-Brasil)10, which generated an imaging protocol and digital videos corresponding to three cardiac cycles that were stored and transmitted to the reading center.
Digital technology has revolutionized the acquisition, transmission, and storage of exams and aids in the processing and use of images. However, even if these technological advances are incorporated into clinical practice, their impact in measurement reading variability in the research environment remains unknown. Therefore, the objective of this study was to assess the reproducibility of echocardiographic measurements that allow the estimation of LVM by comparing values obtained locally (online, in the acquisition centers) with those obtained in the reading centers (offline) and with duplicate measurements performed by different readers at the reading center. Furthermore, the study aimed to assess the reproducibility of the measurements of the left atrium and aorta and those obtained by transmitral flow Doppler and mitral annular tissue Doppler imaging.
Methods
ELSA-Brasil is a prospective multicenter trial involving 15,105 voluntary participants aged between 35 and 74 years and consisting of the staff of public universities and research institutes. The goal of ELSA-Brasil was to investigate the epidemiological, clinical, and molecular aspects of nontransmissible chronic diseases, particularly cardiovascular diseases and diabetes.10 Data were collected between August 2008 and December 2010, and approximately 10,000 participants were subjected to an echocardiographic exam as the standard procedure. The ELSA-Brasil protocol was approved by the Research Ethics Committees of all institutions involved, and all the participants signed an informed consent form.
All the tests were performed at the investigation centers using the same model equipment (Toshiba Aplio XG) and by well-trained echocardiographists who were later certified by the reading center involved in the study. The ELSA-Brasil protocol followed the methods recommended by the European and North American Echocardiography Societies8,11. We selected the sequences of three consecutive heartbeats in each echocardiographic window that best represented existing findings and recorded them in a standard digital format for medical imaging (DICOM).
For analysis of reproducibility, in addition to image acquisition according to the established protocol, the echocardiographists of the investigation center performed echocardiographic measurements during image acquisition, according to current practice (online measurements).
Subsequently, the data files were sent to the reading center, together with a completed form with an evaluation of image quality and online measurements. At the reading center, the images were analyzed in a ComPACS 10.5 workstation (Medimatic SrL, Italy). The offline measurements were performed at the reading center by another skilled echocardiographist (reader) blinded to previous readings. The offline readings involved a second qualitative assessment as well as all echocardiographic measurements using procedures similar to those adopted in the investigation center. A few exams (n = 68) were read again by a second reader at the reading center blinded to the initial online assessment and to the initial offline assessment.
LVM was calculated by making linear measurements of the final diastolic diameter and the LV parietal thickness on the two-dimensional mode and M-mode. For this purpose, the formula and the definition criteria of the leading edge technique proposed by the American Society of Echocardiography were used, as follows12:
LVM = 0.8 × [1.04 (LVIDD + PWTD + IVSTD)3 − (LVIDD)3] + 0.6 g,
where LVM: left ventricular mass; LVIDD: left ventricular internal diameter in diastole; PWTD: posterior wall thickness in diastole; and IVSTD: interventricular septum thickness in diastole.
For other measurements and Doppler studies, we used the parameters defined in the ELSA-Brasil protocol10.
Statistical Analysis
Statistical analysis was performed with SPSS 17.0 software for Windows. The categorical variables were expressed as the absolute and relative frequency and the numeric variables as means ± standard deviations.
The differences between echocardiographic measurements were represented using Bland–Altman plots13 and tested by variance analysis. Measurement variability was described using the intraclass correlation coefficient (ICC), also known as the reliability coefficient. ICC was calculated from the estimated variance components in models that considered the following to determine the reproducibility among the readers of the reading center: 1) the effect of the reading center versus the acquisition center as the fixed variable and the effect of individuals on which these measurements were performed as the random variable and 2) the effect of the first read at the reading center in relation to the second read at the reading center as the fixed variable and the effect of individuals on which these measurements were performed as the random variable.
The mean differences and ICCs were calculated using 95% confidence intervals (CIs).
A sample size of 100 exams was estimated to obtain 90% potency and identify a mean difference of 10 g in LVM among acquisition measurements and reading center measurements, with a significance level of 0.055. For convenience purposes and to compensate for losses, 124 individuals were selected for the reproducibility study, representing at least 20 individuals of each of the six investigation centers of the ELSA-Brasil study. Between July and November 2009, each center consecutively included its participants until the local target was reached, following the visit schedule of ELSA.
Results
Among the selected participants, five exams were considered to be nonmeasurable (4%). Of the 119 participants, 72 (61%) were female, with a mean age of 50.2 ± 7.0 years (minimum and maximum of 35 and 68 years, respectively), mean height of 1.64 ± 0.09 m (minimum and maximum of 1.44 and 1.83 m, respectively), and mean body mass index of 26.6 ± 4.0 kg/m2 (minimum and maximum of 19.2 and 36.9 kg/m2, respectively). Of the participating individuals, 54 (45.3%) were of Caucasian ethnicity, 32 (26.9%) were of Middle Eastern/South Asian ethnicity, 31 (26.1%) were of African ethnicity, and two (1.7%) were of Eastern/Southeast Asian ethnicity. Only two individuals were diagnosed with cardiomyopathy.
The quality of parasternal longitudinal images of 115 (96.6%) tests and 106 (92.4%) tests was considered to be excellent/good by the acquisition center and reading center, respectively. Agreement was found for 106 (89.1%) quality evaluations.
No clinically significant differences were found among the means of measurements obtained at the investigation center (online) and those obtained at the reading center (offline) for most measurements (Table 1).
Table 1.
Echocardiographic measurements obtained at the acquisition and reading centers and respective reproducibility measurements
| Measurement | Values | Reproducibility measurement | |||
|---|---|---|---|---|---|
| n | Acquisition center | Reading center | Mean difference (95% CI) | ICC (95% CI) | |
| Two-dimensional mode | |||||
| Aortic root diameter (cm) | 117 | 3.00 ± 0.45 | 2.98 ± 0.38 | 0.02 (−0.03-0.08) | 0.75 (0.66-0.82) |
| LA diameter (cm) | 118 | 3.40 ± 0.54 | 3.50 ± 0.46 | −0.10 (−0.18-0.02) | 0.63 (0.51-0.73) |
| Septal thickness(cm) | 119 | 0.88 ± 0.17 | 0.87 ± 0.17 | 0.00 (−0.03-0.03) | 0.56 (0.42-0.67) |
| LV posterior wall thickness (cm) | 119 | 0.84 ± 0.16 | 0.86 ± 0.15 | −0.02 (−0.05-0.01) | 0.56 (0.43-0.68) |
| Diastolic LV diameter (cm) | 119 | 4.58 ± 0.50 | 4.52 ± 0.47 | 0.06 (0.00-0.11) | 0.79 (0.71-0.85) |
| Systolic LV diameter (cm) | 118 | 2.92 ± 0.46 | 2.82 ± 0.43 | 0.10 (0.03-0.17) | 0.67 (0.55-0.76) |
| LV mass | 119 | 131.29 ± 42.98 | 129.99 ± 40.79 | 1.29 (−3.60-6.19) | 0.79 (0.72-0.86) |
| LA area (cm²) | 101 | 16.33 ± 3.85 | 16.63 ± 3.68 | −0.30 (−0.97-0.37) | 0.59 (0.45-0.71) |
| LV ejection fraction | 118 | 65.08 ± 10.87 | 67.31 ± 8.95 | −2.22 (−4.29-0.16) | 0.35 (0.19-0.50) |
| M-mode | |||||
| Aortic root diameter (cm) | 100 | 2.99 ± 0.40 | 2.98 ± 0.42 | 0.01 (−0.03-0.05) | 0.89 (0.84-0.92) |
| LA diameter (cm) | 100 | 3.55 ± 0.46 | 3.68 ± 0.46 | −0.13 (−0.18-0.08) | 0.86 (0.80-0.90) |
| Septal thickness(cm) | 86 | 0.88 ± 0.18 | 0.87 ± 0.19 | 0.01 (−0.02-0.04) | 0.67 (0.53-0.77) |
| LV posterior wall thickness (cm) | 86 | 0.84 ± 0.16 | 0.85 ± 0.17 | −0.01 (−0.04-0.02) | 0.60 (0.44-0.72) |
| Diastolic LV diameter (cm) | 86 | 4.72 ± 0.57 | 4.71 ± 0.56 | 0.01 (−0.04-0.06) | 0.92 (0.88-0.95) |
| Systolic LV diameter (cm) | 86 | 2.85 ± 0.54 | 2.82 ± 0.58 | 0.03 (−0.02-0.08) | 0.92 (0.88-0.95) |
| LV mass | 86 | 139.52 ± 55.18 | 138.87 ± 53.05 | 0.66 (−4.89-6.20) | 0.89 (0.83-0.92) |
| LV ejection fraction | 86 | 69.98 ± 7.62 | 70.33 ± 9.18 | −0.35 (−1.59-0.89) | 0.77 (0.66-0.84) |
| Mitral Doppler | |||||
| E wave | 119 | 0.72 ± 0.17 | 0.72 ± 0.15 | 0.01 (−0.01-0.02) | 0.88 (0.83-0.92) |
| Deceleration time | 117 | 217.50 ± 45.55 | 226.35 ± 42.31 | −8.86 (−16.22-1.49) | 0.58 (0.45-0.69) |
| A wave | 119 | 0.59 ± 0.16 | 0.60 ± 0.15 | −0.01 (−0.02-0.01) | 0.90 (0.86-0.93) |
| E/A ratio | 119 | 1.30 ± 0.45 | 1.26 ± 0.41 | 0.04 (0.01-0.07) | 0.93 (0.90-0.95) |
| Medial mitral annular TDI | |||||
| s' velocity | 111 | 7.56 ± 1.34 | 7.49 ± 1.14 | 0.07 (−0.13-0.26) | 0.65 (0.52-0.74) |
| e' velocity | 112 | 9.86 ± 2.74 | 9.92 ± 2.61 | −0.06 (−0.34-0.23) | 0.84 (0.78-0.89) |
| a' velocity | 113 | 9.71 ± 2.36 | 9.63 ± 1.74 | 0.07 (−0.28-0.43) | 0.57 (0.43-0.68) |
| Lateral mitral annular TDI | |||||
| s' velocity | 111 | 8.38 ± 2.06 | 8.35 ± 1.82 | 0.03 (−0.31-0.37) | 0.57 (0.43-0.68) |
| e' velocity | 113 | 11.98 ± 2.63 | 11.97 ± 2.55 | 0.01 (−0.23-0.26) | 0.87 (0.82-0.91) |
| a' velocity | 113 | 9.14 ± 2.57 | 9.23 ± 2.51 | −0.09 (−0.25-0.06) | 0.95 (0.92-0.96) |
ICC: intraclass correlation coefficient; difference: value obtained at the reading center − value obtained at the acquisition center; LV: left ventricle; LA: left atrium; TDI: tissue Doppler imaging. The values obtained at the acquisition and reading centers are expressed as the mean ± standard deviation.
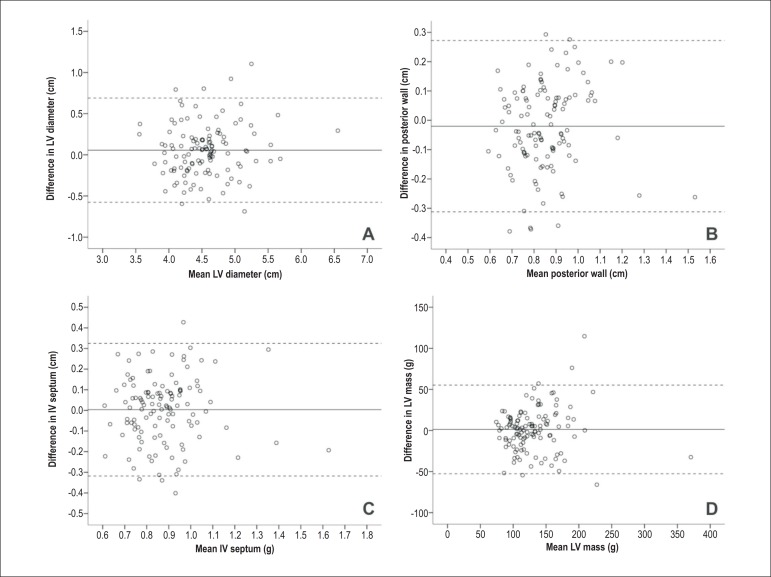
Figure 1 shows the differences between values obtained at the acquisition centers and those obtained at the reading center on the basis of the mean LVM readings, estimated using two-dimensional measurements (Bland–Altman plots). There was no notable tendency among online and offline measurements. In 95% samples, the differences were less than 0.7 cm, 0.3 cm, and 0.4 cm for the LV diastolic diameter, septum thickness, and posterior wall thickness, respectively. LVM was calculated from these three variables and showed a discrepancy of 54 g or lower in 95% of samples. There were no association trends between magnitude and amplitude differences in these variables.
Figure 1.
Differences between the measurements from which LVM was estimated, performed from images obtained on the two-dimensional mode in the acquisition and reading centers (y axis) and the mean of both measurements (x axis). A: Left ventricular diameter; B: left ventricular posterior wall thickness; C: septal thickness; D: left ventricular mass. The solid line indicates the mean difference between both measurements, and the dashed line indicates the mean ± two standard deviations.
The exclusion of the images that the reading center considered to be of regular quality (n = 9) did not change the mean differences of the following parameters measured online and offline: LV diameter (0.07 cm, 95% CI: 0.01 to 0.13), posterior LV wall thickness (−0.02 cm, 95% CI: −0.05 to 0.01), interventricular septum thickness (0 cm, 95% CI: −0.03 to 0.04), and LVM estimate (2.27 g, 95% CI: −2.77 to 7.31). Moreover, the results were quite similar after the exclusion in relation to ICC (0.80 for LV diameter, 0.48 for posterior LV wall thickness, 0.52 for interventricular septum thickness, and 0.80 for LVM estimate).
For the remaining assessments, the distribution of the differences was of the same magnitude, as well as the distribution of the ICC values (Table 1).
Table 2 shows the measurements obtained by different readers at the reading center. Although significant differences were observed between measurements, their magnitude was relatively low from a clinical point of view.
Table 2.
Echocardiographic measurements obtained at the reading center, repeated in different moments by different readers
| Measurement | Values | Reproducibility measurement | |||
|---|---|---|---|---|---|
| n | First reading at the reading center | Second reading at the reading center | Mean difference (95% CI) | ICC (95% CI) | |
| Measurement | |||||
| Aortic root diameter (cm) | 63 | 3.02 ± 0.37 | 3.02 ± 0.37 | 0.00 (−0.07-0.07) | 0.74 (0.61-0.84) |
| LA diameter (cm) | 66 | 3.58 ± 0.43 | 3.63 ± 0.43 | −0.05 (-0.11-0.01) | 0.84 (0.75-0.90) |
| Septal thickness(cm) | 66 | 0.87 ± 0.19 | 0.94 ± 0.18 | -0.07 (−0.09-0.04) | 0.84 (0.75-0.90) |
| LV posterior wall thickness (cm) | 66 | 0.87 ± 0.17 | 0.93 ± 0.15 | −0.06 (−0.10-0.02) | 0.53 (0.33-0.68) |
| Diastolic LV diameter (cm) | 66 | 4.60 ± 0.47 | 4.55 ± 0.50 | 0.05 (−0.01-0.11) | 0.88 (0.82-0.93) |
| Systolic LV diameter (cm) | 66 | 2.85 ± 0.50 | 2.90 ± 0.52 | −0.05 (−0.10-0.00) | 0.92 (0.86-0.95) |
| LV mass | 66 | 134.80 ± 46.22 | 145.30 ± 43.66 | −10.50 (−16.40-4.60) | 0.86 (0.78-0.91) |
| LA area (cm²) | 59 | 16.80 ± 4.03 | 18.07 ± 3.19 | −1.27 (−1.94-0.60) | 0.75 (0.61-0.84) |
| LV ejection fraction | 66 | 68.04 ± 8.97 | 65.79 ± 9.44 | 2.25 (0.76-3.75) | 0.78 (0.67-0.86) |
| M-mode | |||||
| Aortic root diameter (cm) | 57 | 3.00 ± 0.40 | 2.98 ± 0.40 | 0.02 (−0.03-0.07) | 0.88 (0.80-0.93) |
| LA diameter (cm) | 57 | 3.73 ± 0.47 | 3.77 ± 0.47 | −0.04 (−0.10-0.01) | 0.89 (0.83-0.94) |
| Septal thickness(cm) | 35 | 0.86 ± 0.14 | 1.04 ± 0.18 | −0.18 (−0.24-0.13) | 0.54 (0.26-0.74) |
| LV posterior wall thickness (cm) | 35 | 0.83 ± 0.16 | 1.01 ± 0.19 | −0.18 (−0.22-0.13) | 0.74 (0.55-0.70) |
| Diastolic LV diameter (cm) | 35 | 4.90 ± 0.60 | 4.79 ± 0.63 | 0.11 (0.03-0.18) | 0.93 (0.87-0.97) |
| Systolic LV diameter (cm) | 35 | 2.99 ± 0.77 | 3.12 ± 0.65 | −0.13 (−0.22-0.04) | 0.88 (0.88-0.97) |
| LV mass | 35 | 143.42 ± 41.58 | 178.04 ± 47.58 | −34.61 (-42.89-26.34) | 0.86 (0.73-0.92) |
| LV ejection fraction | 35 | 68.81 ± 11.93 | 63.92 ± 9.26 | 4.89 (2.20-7.58) | 0.73 (0.53-0.86) |
| Mitral Doppler | |||||
| E wave | 66 | 0.72 ± 0.15 | 0.72 ± 0.16 | 0.00 (−0.02-0.02) | 0.91 (0.86-0.94) |
| Deceleration time | 66 | 222.59 ± 44.18 | 214.03 ± 35.73 | 8.56 (0.42-16.69) | 0.66 (0.50-0.78) |
| A wave | 66 | 0.58 ± 0.15 | 0.58 ± 0.15 | 0.01 (−0.01-0.02) | 0.92 (0.87-0.95) |
| E/A ration | 66 | 1.31 ± 0.41 | 1.32 ± 0.42 | −0.02 (−0.03-0.00) | 0.99 (0.98-0.99) |
| Medial mitral annular TDI | |||||
| s' velocity | 64 | 7.69 ± 1.13 | 7.74 ± 1.18 | −0.06 (−0.31-0.19) | 0.62 (0.45-0.75) |
| e' velocity | 64 | 10.09 ± 2.49 | 9.70 ± 2.54 | 0.39 (0.03-0.76) | 0.83 (0.74-0.89) |
| a' velocity | 64 | 9.49 ± 1.61 | 9.33 ± 1.55 | 0.16 (0.00-0.31) | 0.92 (0.88-0.95) |
| Lateral mitral annular TDI | |||||
| s' velocity | 64 | 8.50 ± 1.74 | 9.11 ± 1.83 | −0.61 (−1.01-0.20) | 0.59 (0.40-0.73) |
| e' velocity | 64 | 12.41 ± 2.36 | 12.36 ± 2.36 | 0.05 (−0.16-0.27) | 0.93 (0.89-0.96) |
| a' velocity | 63 | 9.42 ± 2.37 | 9.22 ± 2.18 | 0.20 (0.00-0.40) | 0.94 (0.90-0.96) |
ICC: intraclass correlation coefficient; difference: value obtained at the reading center − value obtained at the acquisition center; LV: left ventricle; LA: left atrium; TDI: tissue Doppler imaging. The values obtained at the acquisition and reading centers are expressed as the mean ± standard deviation.
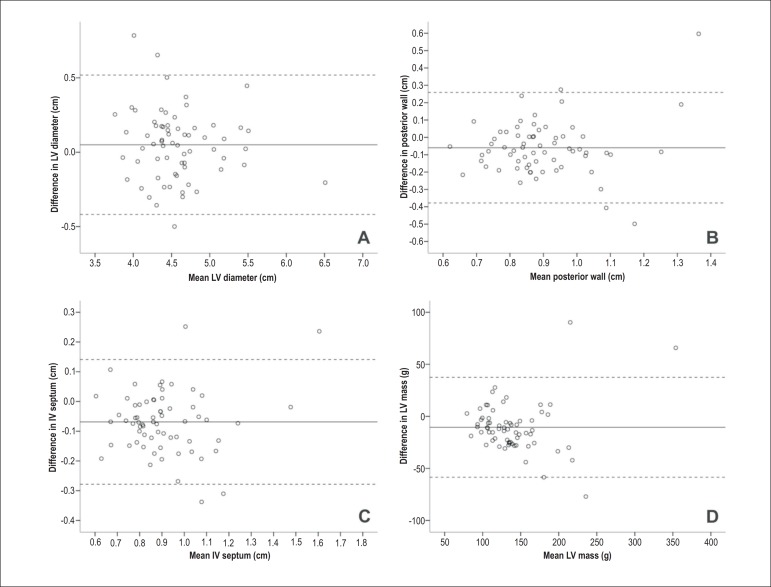
Figure 2 shows the measurement differences obtained in both readings, according to the mean LV values. The LVM difference did not surpass 58 g in 95% samples. There were no association trends between magnitude and amplitude differences in these variables. After the exclusion of regular-quality exams (n = 8), the results were quite similar in terms of the mean differences between both offline readings of LV diameter (0.04 cm, 95% CI: −0.02 to 0.10), posterior LV wall thickness (−0.08 cm, 95% CI: −0.11 to −0.04), interventricular septum thickness (−0.07 cm, 95% CI: −0.10 to −0.04), and LVM estimate (−13.2 g, 95% CI: −18.5 to −7.96) and the respective ICC values (0.89 for LV diameter, 0.57 for posterior LV wall thickness, 0.79 for interventricular septum thickness, and 0.90 for LVM estimate).
Figure 2.
Differences between the measurements from which LVM was estimated, performed by different readers at the reading center (y axis) from images obtained on the two-dimensional mode, and the mean of both measurements (x axis). A: Left ventricular diameter; B: left ventricular posterior wall thickness; C: septal thickness; D: left ventricular mass. The solid line indicates the mean difference between both measurements, and the dashed line indicates the mean ± two standard deviations
In addition to LV measurements using the two-dimensional mode, we investigated the reproducibility of other measurements performed as part of the echocardiography protocol of ELSA-Brasil. We observed CCI values in the same range for measurements obtained using the M-Mode and transmitral flow Doppler and mitral annular tissue Doppler imaging. This was true not only for offline and online measurements but also for measurements performed by distinct readers of the reading center (Tables 1 and 2).
Discussion
In this study, the differences observed between online and offline measurements were practically null. The intraclass correlation coefficient, used for reproducibility assessment, was considered to be satisfactory for the LVM estimates obtained in the acquisition and reading centers (ICC = 0.79). For most tests, the online and offline LVM estimates did not surpass 50 g. In a similar comparative study involving 274 hypertensive individuals14, ICC was not reported for the comparison of measurements performed in the acquisition centers and the reading center; however, the Pearson correlation was 0.76 and the mean difference was 8 ± 20 g (p < 0.001), and this discrepancy was similar to that obtained in the present study for most individuals.
With regard to reproducibility of measurements performed at the reading center by different readers, despite the existence of differences between the mean LVM estimates (−10.50 g, CI 95%: −16.40 to −4.60), the magnitude of this difference was relatively small from the clinical point of view, and ICC of both estimates was quite satisfactory (ICC = 0.86). In a previous report,14 the agreement between the readers of the reading center was only calculated for 10 high-quality echocardiography exams after repeated measurements, and it was considered to be very satisfactory (ICC = 0.96 to 0.99, depending on the reader).
With regard to other assessed echocardiographic measurements, we also observed small differences among the readers, and the reproducibility estimates were better when both the assessments were performed at the reading center. In general, these values were similar and had the same result patterns for the LVM findings. A similar performance was observed in other studies assessing the reproducibility of echocardiographic measurements5,6,15.
Although the reading center was apparently more demanding in the assessment of image quality than the investigation center (92% versus 97% for images considered to have excellent/good quality), the proportion of exams considered to be nonmeasureable was much lower than that observed in other population studies. In the Framingham Heart Study, only 28% of the echocardiography exams performed during the first 5 months were considered to be acceptable, reaching an acceptability of 74% to 81% in 2 years16. In the Atherosclerosis Risk in Communities (ARIC) study, despite the fact that the echocardiogram was acquired in one study center, only 70% of the exams were considered to be appropriate for estimating LVM1,7. This phenomenon may explain the variability in our study, and we can assume that the echocardiographist of the investigation center caused more interference in the measurements owing to the larger sample size when performing the exams. In contrast, it is possible that the image quality assessment was too permissive. Considering the increased number of images whose measurement was difficult in comparison with that in other studies, the technological benefits may have not been sufficient to compensate for the inadequate image quality.
Study Limitations
Among the limitations of the study, the first noteworthy aspect is that the reproducibility was not evaluated in all investigation centers; therefore, it is not possible to infer whether the measurements repeated at the reading center are more reproducible than those repeated at each acquisition center. Potential difficulties in the standardization of acquisition readings in different centers are one of the main reasons to perform all measurements in a single center. The reproducibility of offline measurements was only determined in 50% of the samples. This percentage is significant in comparison with that observed previously14, and it seems to be appropriate because there are fewer sources of variability in these comparisons.
Another limitation of the study is that data collected for the evaluation of reproducibility were from the initial phases, during the learning curve, as observed in the Framingham Heart Study16. This may have caused systematic temporal drifts, consequently influencing the results, corroborating the need for permanent quality control protocols in ELSA-Brasil and subsequent studies, and it may help implement additional reading control measures that are effective for most exams that were included and read in the present study.
ICC of the LVM measurement obtained on the M-mode (86 exams, 69.4%) was higher than that obtained on the two-dimensional mode (119 exams, 96.0%). These findings suggest that exams using poor-quality images are less reproducible; however, when these were excluded, there was no significant improvement in reproducibility. We focused our conclusions on the two-dimensional measurements because they best reflect current practices. Moreover, higher reproducibility does not necessarily imply increased accuracy because of the systematic errors inherent to the M-mode17.
Conclusion
There were no relevant systematic differences in the offline and online LVM echocardiographic measurements. The reproducibility measurements were similar to those found in previous studies, despite the fact that these studies avoided the exclusion of a high percentage of images. Several variability sources persisted in the present study, even in the exams performed with current technology and guided by a research protocol. This may indicate the need for an increased sample size to identify LVM differences among population and/or therapeutic interventions. The strategy of performing echocardiography measurements in reading centers (offline), as used in ELSA-Brasil, is feasible and can be important in clinical and epidemiological studies. This is also true for institutes where exams are analyzed by the echocardiographist during image acquisition (online).
Funding
The ELSA-Brasil study was funded by the Health Ministry (Department of Science and Technology), the Ministry of Science and Technology (FINEP– Funding Authority for Studies and Projects, and the National Council for Scientific Research), process numbers: 01 06 0010.00 RS, 01 06 0212.00BA, 01 06 0300.00 ES, 01 06 0278.00 MG, 01 06 0115.00SP, and 01 06 0071.00 RJ.
Acknowledgments
We are grateful to the participants of the ELSA-Brasil study and the researchers who made their achievement possible.
Footnotes
Author contributions
Conception and design of the research: Tognon AP, Foppa M, Duncan BB; Acquisition of data: Foppa M, El Aoua LMM, Fernandes LP; Analysis and interpretation of the data: Tognon AP, Luft VC, Chambless L; Statistical analysis: Tognon AP, Chambless L; Obtaining financing: Lotufo P, Duncan BB; Writing of the manuscript: Tognon AP, Foppa M; Critical revision of the manuscript for intellectual content: Luft VC, Chambless L, Lotufo P, El Aoua LMM, Fernandes LP, Duncan BB.
Potential Conflict of Interest
No potential conflict of interest relevant to this article was reported.
Sources of Funding
This study was funded by Ministério da Saúde (Departamento de Ciência e Tecnologia), Ministério da Ciência e Tecnologia (Financiadora de Estudos e Projetos e Conselho Nacional de Pesquisa).
Study Association
This article is part of the thesis of master submitted by Alexandre Pereira Tognon, from Alexandre Pereira Tognon.
References
- 1.Burchfiel CM, Skelton TN, Andrew ME, Garrison RJ, Arnett DK, Jones DW, et al. Metabolic syndrome and echocardiographic left ventricular mass in blacks: the Atherosclerosis Risk in Communities (ARIC) Study. Circulation. 2005;112(6):819–827. doi: 10.1161/CIRCULATIONAHA.104.518498. [DOI] [PubMed] [Google Scholar]
- 2.Levy D, Garrison RJ, Savage DD, Kannel WB, Castelli WP. Prognostic implications of echocardiographically determined left ventricular mass in the Framingham Heart Study. N Engl J Med. 1990;322(22):1561–1566. doi: 10.1056/NEJM199005313222203. [DOI] [PubMed] [Google Scholar]
- 3.Gardin JM, Wagenknecht LE, Anton-Culver H, Flack J, Gidding S, Kurosaki T, et al. Relationship of cardiovascular risk factors to echocardiographic left ventricular mass in healthy young black and white adult men and women. The CARDIA study. Coronary Artery Risk Development in Young Adults. Circulation. 1995;92(3):380–387. doi: 10.1161/01.cir.92.3.380. [DOI] [PubMed] [Google Scholar]
- 4.Gardin JM, McClelland R, Kitzman D, Lima JA, Bommer W, Klopfenstein HS, et al. M-mode echocardiographic predictors of six- to seven-year incidence of coronary heart disease, stroke, congestive heart failure, and mortality in an elderly cohort (the Cardiovascular Health Study) Am J Cardiol. 2001;87(9):1051–1057. doi: 10.1016/s0002-9149(01)01460-6. [DOI] [PubMed] [Google Scholar]
- 5.De Simone G, Muiesan ML, Ganau A, Longhini C, Verdecchia P, Palmieri V, et al. Reliability and limitations of echocardiographic measurement of left ventricular mass for risk stratification and follow-up in single patients: the RES trial. Working Group on Heart and Hypertension of the Italian Society of Hypertension. Reliability of M-mode Echocardiographic Studies. Pt2J Hypertens. 1999;17(12):1955–1963. doi: 10.1097/00004872-199917121-00027. [DOI] [PubMed] [Google Scholar]
- 6.Gottdiener JS, Livengood SV, Meyer PS, Chase GA. Should echocardiography be performed to assess effects of antihypertensive therapy? Test-retest reliability of echocardiography for measurement of left ventricular mass and function. J Am Coll Cardiol. 1995;25(2):424–430. doi: 10.1016/0735-1097(94)00375-z. [DOI] [PubMed] [Google Scholar]
- 7.Skelton TN, Andrew ME, Arnett DK, Burchfiel CM, Garrison RJ, Samdarshi TE, et al. Echocardiographic left ventricular mass in African-Americans: the Jackson cohort of the Atherosclerosis Risk in Communities Study. Echocardiography. 2003;20(2):111–120. doi: 10.1046/j.1540-8175.2003.03000.x. [DOI] [PubMed] [Google Scholar]
- 8.Douglas PS, DeCara JM, Devereux RB, Duckworth S, Gardin JM, Jaber WA, et al. Echocardiographic imaging in clinical trials: American Society of Echocardiography Standards for echocardiography core laboratories: endorsed by the American College of Cardiology Foundation. J Am Soc Echocardiogr. 2009;22(7):755–765. doi: 10.1016/j.echo.2009.05.020. [DOI] [PubMed] [Google Scholar]
- 9.Hole T, Otterstad JE, St John Sutton M, Froland G, Holme I, Skjaerpe T. Differences between echocardiographic measurements of left ventricular dimensions and function by local investigators and a core laboratory in a 2-year follow-up study of patients with an acute myocardial infarction. Eur J Echocardiogr. 2002;3(4):263–270. [PubMed] [Google Scholar]
- 10.Aquino EM, Barreto SM, Bensenor IM, Carvalho MS, Chor D, Duncan BB, et al. Brazilian Longitudinal Study of Adult Health (ELSA-Brasil): objectives and design. Am J Epidemiol. 2012;175(4):315–324. doi: 10.1093/aje/kwr294. [DOI] [PubMed] [Google Scholar]
- 11.Lang RM, Bierig M, Devereux RB, Flachskampf FA, Foster E, Pellikka PA, et al. Recommendations for chamber quantification. Eur J Echocardiogr. 2006;7(2):79–108. doi: 10.1016/j.euje.2005.12.014. [DOI] [PubMed] [Google Scholar]
- 12.Gottdiener JS, Bednarz J, Devereux R, Gardin J, Klein A, Manning WJ, et al. American Society of Echocardiography recommendations for use of echocardiography in clinical trials. J Am Soc Echocardiogr. 2004;17(10):1086–1119. doi: 10.1016/j.echo.2004.07.013. [DOI] [PubMed] [Google Scholar]
- 13.Bland JM, Altman DG. Statistical methods for assessing agreement between two methods of clinical measurement. Lancet. 1986;1(8476):307–310. [PubMed] [Google Scholar]
- 14.Gosse P, Guez D, Gueret P, Dubourg O, Beauchet A, de Cordoue A, et al. Centralized echocardiogram quality control in a multicenter study of regression of left ventricular hypertrophy in hypertension. J Hypertens. 1998;16(4):531–535. doi: 10.1097/00004872-199816040-00015. [DOI] [PubMed] [Google Scholar]
- 15.Ogah OS, Adebanjo AT, Otukoya AS, Jagusa TJ. Echocardiography in Nigeria: use, problems, reproducibility and potentials. Cardiovasc Ultrasound. 2006;4:13. doi: 10.1186/1476-7120-4-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Savage DD, Garrison RJ, Kannel WB, Anderson SJ, Feinleib M, Castelli WP, et al. Considerations in the use of echocardiography in epidemiology. The Framingham Study. Pt 2Hypertension. 1987;9(2):II40–II44. doi: 10.1161/01.hyp.9.2_pt_2.ii40. [DOI] [PubMed] [Google Scholar]
- 17.Foppa M, Duncan BB, Rohde LE. Echocardiography-based left ventricular mass estimation. How should we define hypertrophy? Cardiovasc Ultrasound. 2005;3:17. doi: 10.1186/1476-7120-3-17. [DOI] [PMC free article] [PubMed] [Google Scholar]