Abstract
Iron deficiency anemia is extremely common, particularly in the developing world, reaching a state of global epidemic. Iron deficiency during pregnancy is one of the leading causes of anemia in infants and young children. Many women go through the entire pregnancy without attaining the minimum required intake of iron. This review aims to determine the impact of maternal iron deficiency and iron deficiency anemia on infants and young children. Extensive literature review revealed that iron deficiency is a global nutritional problem affecting up to 52% of pregnant women. Many of these women are symptomatic. Lack of proper weight gain during pregnancy is an important predictor of iron deficiency.
Anemia is generally defined according to hemoglobin levels, which may vary according to many factors most importantly age, gender, and ethnicity. Any level below 13 g/dL for males, and below 12 g/dL for females is considered abnormal.1 Hemoglobin levels of less than 11 g/dL at any time during pregnancy are considered abnormal. Once anemia is recognized, the possibility of iron deficiency should be considered.2 Abnormalities in red blood cell indices on complete blood count typically precede the development of lowered hemoglobin levels.3 Iron deficiency usually develops slowly over time, and may not be symptomatic, or clinically obvious. Once iron stores are completely depleted, iron accessibility to the tissues decline leading to symptomatic anemia. The objective of this review is to outline the impact of maternal iron deficiency, and iron deficiency anemia on infants and young children.
Iron metabolism
Iron is a crucial component in the metabolic processes involved in tissue oxygenation. An average individual contains a total of 3-5 grams of iron. A standard diet could supply up to 15 mg of iron per day. The acidic environment aids iron absorption, which takes place in the first, and second parts of the small intestine. Iron absorption is therefore enhanced by the co-administration of acidic compounds, such as ascorbic acid. Iron absorption is also normally enhanced in response to heightened needs. After absorption, protein-bound iron is transported into the bone marrow for incorporation in the production of red blood cells.4 Excess iron is stored as ferritin, a labile, and easily available provider of iron.
Epidemiology
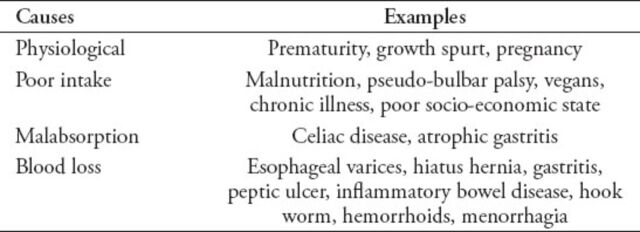
Iron deficiency is the most globally prevalent nutritional problem reaching an epidemic level in many developing countries.5 In addition, it is the most common nutritional deficiency encountered in the developed world;6 up to 50% of cases are the result of insufficient iron intake.7 Pregnancy is associated with increased iron demand, and therefore, increase the risk of iron deficiency anemia. Up to 52% of pregnant women in the developing world are affected.8 Lowered iron stores in their newborn baby will increase the risk of subsequent iron deficiency anemia. Prematurity and early weaning off breastfeeding increases the risk further, because of reduced iron stores. Other causes and risk factors for developing iron deficiency anemia are summarized in Table 1, and include restricted diets, growth spurt, and heavy blood loss.9
Table 1.
Common causes of iron deficiency anemia.9
Iron deficiency anemia
Typical features of iron deficiency anemia are caused by lowered oxygen delivery to the tissues, and include pallor, fatigue, apathy, fainting, and breathlessness.2,9 Additional features include headaches, palpitation, hair loss, and tinnitus. Chronic iron deficiency anemia lowers work tolerance, productivity, and the quality of life. This leads to further socio-economic difficulties. Dysfunction in the immune system results in increased risks for infections.9
With more severe degrees of anemia, cardiac failure may develop. During pregnancy, iron deficiency anemia correlates with negative perinatal outcomes including premature labor, intrauterine growth retardation, low birth weight, birth asphyxia, and neonatal anemia.2,6
Nutritional factors
Pregnancy and lactation result in increased iron demands. The nutritional status is the key in preventing iron deficiency. A healthy varied diet can be routinely supplemented by prophylactic doses of iron to prevent depletion of iron stores. The total iron intake during pregnancy should not be less than 1000 mg.10
A recent study9 found that most pregnant women were not receiving adequate amounts of iron, despite taking fortified food and supplementation. Even in developed countries, such as the United Kingdom (UK), up to 50% of women during their reproductive age have poor iron residual supplies, and are at risk of developing anemia if they conceive.9 Another UK study11 found that 40% of women aged between 19-34 years had iron levels below the recommended doses.
Normal weight gain is an indicator of proper maternal nourishment. Healthy weight prior to conception and an average weight gain of 12 kg (10-14 kg) is linked to favorable perinatal outcomes.12 This results in the delivery of a baby with a healthy birth weight of 3.1-3.6 kg.12,13 Ideal maternal weight gain may be difficult to achieve in practice. Therefore, enhanced physical activity should be combined with nutritious food that does not promote excessive weight gain, which is also a risk factor for iron deficiency. Vegetarians and vegans may require additional iron fortified food and supplementation to prevent the possible shortages of dietary intake.12
Teenage mothers are another group of women at increased risk. They have a greater nutritional requirement due to their own growth spurts.14,15 Teenage pregnancies are usually unplanned, and therefore these mothers may already experience suboptimal nutritional status prior to conception making them at an even higher risk for developing iron deficiency anemia.14
Impact of iron deficiency anemia
Throughout pregnancy, iron deficiency anemia adversely affects the maternal and fetal well-being, and is linked to increased morbidity and fetal death. Affected mothers frequently experience breathing difficulties, fainting, tiredness, palpitations, and sleep difficulties.16 They also have an increased risk of developing perinatal infection, pre-eclampsia, and bleeding. Post-partum cognitive impairment and behavioral difficulties were also reported.17-19 Adverse perinatal outcomes include intrauterine growth retardation, prematurity, and low birth weight, all with significant mortality risks, particularly in the developing world.20-22 Iron deficiency during the first trimester, has a more negative impact on fetal growth than anemia developing later in pregnancy.23,24 This is also true for risk of premature labor.25 Poor socio-economic status contributes significantly to all aspects of these inter-linked problems that are more commonly encountered in the developing world. Any successful public prevention or treatment program should put into consideration all these contributing and correlating factors.
Lowered iron stores of the newborn child may persist for up to one year and result in iron deficiency anemia.26 Such a state should be identified and treated promptly because of the possible long term consequences. Iron is essential for neural metabolism and functioning. Iron deficiency anemia results in changes in energy metabolism within the brain with defects in neurotransmitter function and myelination.27 Therefore, infants and young children with iron deficiency anemia are at risk of developmental difficulties involving cognitive, social-emotional, and adaptive functions.28,29 Other studies have documented delays in both language and motor development. Breastfeeding is usually protective, but not if the mother is iron deficient. It has been noted that iron levels in breast milk fall as lactation progresses over time.30 Careful monitoring and adequate supplementation is therefore needed for infants at risk.
Iron supplementation
Routine maternal iron supplementation is a vital mean in correcting the global problem of iron deficiency and preventing its negative effects.31 Whilst oral supplementation is most prevalent, it is also possible to provide iron parentally (intramuscular or intravenous). Prophylactic oral iron supplementation can be associated with some side effects, such as nausea and constipation, which are normally more common during pregnancy. It is ideal to start iron supplementation before conception, or as soon as possible, in order to reduce the risks of prematurity and low birth weight.32 It is also important to note the importance of other micronutrients, such as zinc, copper, vitamin A and E, on fetal growth and development.33 Further research is required to clarify the need for such supplementation and the recommended doses.
Iron treatment should be started once iron deficiency anemia is recognized in infants and young children. However, several randomized control trials found no benefits on future psychomotor development.34Another review of several randomized controlled trials of children found that iron treatment did not result in an enhanced cognitive function in children less than 5 years of age.35 This suggests that early prophylaxis is better than delayed treatment. However, recent studies indicated some cognitive and motor benefits from treating children less than 5 years of age.36 In addition, iron supplementation improved the attention and concentration of adolescents and adult women with symptomatic iron deficiency anemia, suggesting more positive effects of treating severe degrees of anemia.37-39
In conclusion, adequate iron intake is crucial for healthy pregnancy. However, adequate nutrition may not be possible in many developing countries. Iron supplementation should be considered early in these cases. There is an increasing need for public health strategies to educate the population as to the need for a healthy diet and iron supplementation before conception, or at least at the beginning of the pregnancy. Integrating this information into educational curricula, pre-marital counselling, and prenatal care is needed. Mothers should receive appropriate nutritional advice and supplementation at their first point of contact with healthcare professionals.
Footnotes
Related Articles
Al-Farsi SH, Al-Khabori MK, Al-Hunieni MN, Al-Riyami NM. Fetal outcomes in pregnant women with sickle cell disease. Saudi Med J 2014; 35: 472-476.
Hendaus MA. Hemolytic anemia in an immuno-competent infant due to acute cytomegalovirus infection. Saudi Med J 2012; 33: 908-909.
Shuaib AA, Frass KA, Al-Harazi AH, Ghanem NS. Pregnancy outcomes of mothers aged 17 years or less. Saudi Med J 2011; 32: 166-170.
References
- 1.Thum T, Anker S. Nutritional iron deficiency in patients with chronic illnesses. Lancet. 2007;370:1906. doi: 10.1016/S0140-6736(07)61810-8. [DOI] [PubMed] [Google Scholar]
- 2.Shill KB, Karmakar P, Kibria G, Das A, Rahman MA, Hossain MS, et al. Prevalence of iron-deficiency anaemia among university students in Noakhali region, Bangladesh. J Health Popul Nutr. 2014;32:103–110. [PMC free article] [PubMed] [Google Scholar]
- 3.Burke RM, Leon JS, Suchdev PS. Identification, prevention and treatment of iron deficiency during the first 1000 Days. Nutrients. 2014;6:4093–4114. doi: 10.3390/nu6104093. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Lee JO, Lee JH, Ahn S, Kim JW, Chang H, Kim YJ, et al. Prevalence and risk factors for iron deficiency anemia in the Korean population: Results of the Fifth Korea National Health and Nutrition Examination Survey. J Korean Med Sci. 2014;29:224–229. doi: 10.3346/jkms.2014.29.2.224. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Sirdah MM, Yaghi A, Yaghi AR. Iron deficiency anemia among kindergarten children living in the marginalized areas of Gaza Strip, Palestine. Rev Bras Hematol Hemoter. 2014;36:132–138. doi: 10.5581/1516-8484.20140030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Zimmerman MB, Hurrell RF. Nutritional iron deficiency. Lancet. 2007;370:511–520. doi: 10.1016/S0140-6736(07)61235-5. [DOI] [PubMed] [Google Scholar]
- 7.Kassebaum NJ, Jasrasaria R, Naghavi M, Wulf SK, Johns N, Lozano R, et al. A systematic analysis of global anemia burden from 1990 to 2010. Blood. 2014;30(123):615–624. doi: 10.1182/blood-2013-06-508325. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Sato APS, Fujimori E, Szarfarc SC, Borges ALV, Tsunechiro MA. Food consumption and iron intake of pregnant and reproductive aged women. Revista Latino-Americana de Enfermagem. 2010;18:247–254. doi: 10.1590/s0104-11692010000200016. [DOI] [PubMed] [Google Scholar]
- 9.Abbaspour N, Hurrell R, Kelishadi R. Review on iron and its importance for human health. J Res Med Sci. 2014;19:164–174. [PMC free article] [PubMed] [Google Scholar]
- 10.Bothwell TH. Iron requirements in pregnancy and strategies to meet them. Am J Clin Nutr. 2000;72:257–264. doi: 10.1093/ajcn/72.1.257S. [DOI] [PubMed] [Google Scholar]
- 11.Beck KL, Conlon CA, Kruger R, Coad J. Dietary determinants of and possible solutions to iron deficiency for young women living in industrialized countries: a review. Nutrients. 2014;6:3747–3776. doi: 10.3390/nu6093747. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Brabin L, Brabin BJ, Gies S. Maternal iron - infection interactions and neonatal mortality, with an emphasis on developing countries. Nutr Rev. 2013;71:528–540. doi: 10.1111/nure.12049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Kefiyalew F, Zemene E, Asres Y, Gedefaw L. Anemia among pregnant women in Southeast Ethiopia: prevalence, severity and associated risk factors. BMC Res Notes. 2014;7:771. doi: 10.1186/1756-0500-7-771. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Dainty JR, Berry R, Lynch SR, Harvey LJ, Fairweather-Tait SJ. Estimation of dietary iron bioavailability from food iron intake and iron status. PLoS One. 2014;9:e111824. doi: 10.1371/journal.pone.0111824. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.de Jersey SJ, Nicholson JM, Callaway LK, Daniels LA. A prospective study of pregnancy weight gain in Australian women. Aust N Z J Obstet Gynaecol. 2012;52:545–551. doi: 10.1111/ajo.12013. [DOI] [PubMed] [Google Scholar]
- 16.Lee KA, Zaffke ME, Baratte-Beebe K. Restless legs syndrome and sleep disturbance during pregnancy: the role of folate and iron. J Womens Health Gend Based Med. 2004;10:335–341. doi: 10.1089/152460901750269652. [DOI] [PubMed] [Google Scholar]
- 17.Murray-Kolb LE. Iron and brain functions. Curr Opin Clin Nutr Metab Care. 2013;16:703–707. doi: 10.1097/MCO.0b013e3283653ef8. [DOI] [PubMed] [Google Scholar]
- 18.Beard J. Iron deficiency alters brain development and functioning. J Nutr. 2003;133:1468–1472. doi: 10.1093/jn/133.5.1468S. [DOI] [PubMed] [Google Scholar]
- 19.Milman N. Postpartum anemia II: prevention and treatment. Ann Hematol. 2012;91:143–154. doi: 10.1007/s00277-011-1381-2. [DOI] [PubMed] [Google Scholar]
- 20.Bhutta ZA, Darmstadt GL, Hasan BS, Haws RA. Community-based interventions for improving perinatal and neonatal health outcomes in developing countries: A review of the evidence. Pediatrics. 2005;115:519–617. doi: 10.1542/peds.2004-1441. [DOI] [PubMed] [Google Scholar]
- 21.Gambling L, Danzeisen R, Fosset C, Andersen HS, Dunford S, Srai SKS, et al. Iron and copper interactions in development and the effect on pregnancy outcome, metal-binding proteins and trace element metabolism. J Nutr. 2003;133:1554–1556. doi: 10.1093/jn/133.5.1554S. [DOI] [PubMed] [Google Scholar]
- 22.Scholl TO, Johnson WG. Folic acid: influence on the outcome of pregnancy. Am J Clin Nutr. 2000;7:1295–1303. doi: 10.1093/ajcn/71.5.1295s. [DOI] [PubMed] [Google Scholar]
- 23.Gautam CS, Saha L, Sekhri K, Saha PK. Iron deficiency in pregnancy and the rationality of iron supplements prescribed during pregnancy. Medscape J Med. 2008;10:283. [PMC free article] [PubMed] [Google Scholar]
- 24.Allen LH. Anemia and iron deficiency: effects on pregnancy outcome. Am J Clin Nutr. 2000;71:1280–1284. doi: 10.1093/ajcn/71.5.1280s. [DOI] [PubMed] [Google Scholar]
- 25.Kramer MS, Séguin L, Lydon J, Goulet L. Socio-economic disparities in pregnancy outcome: Why do the poor fare so poorly? Paediatr Peri Epid. 2000;14:194–210. doi: 10.1046/j.1365-3016.2000.00266.x. [DOI] [PubMed] [Google Scholar]
- 26.Goldenberg RL, Culhane JF. Low birth weight in the United States. Am J Clin Nut. 2007;85:584–590. doi: 10.1093/ajcn/85.2.584S. [DOI] [PubMed] [Google Scholar]
- 27.Falkingham M, Abdelhamid A, Curtis P, Fairweather-Tait S, Dye L, Hooper L. The effects of oral iron supplementation on cognition in older children and adults: A systematic review and meta-analysis. Nutr J. 2010;9:4. doi: 10.1186/1475-2891-9-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Felt BT, Lozoff B. Brain iron and behavior of rats are not normalized by treatment of iron deficiency anemia during early development. J Nutr. 1996;126:693–701. doi: 10.1093/jn/126.3.693. [DOI] [PubMed] [Google Scholar]
- 29.Bener A, Kamal M, Bener H, Bhugra D. Higher prevalence of iron deficiency as strong predictor of attention deficit hyperactivity disorder in children. Ann Med Health Sci Res. 2014;4(Suppl 3):291–297. doi: 10.4103/2141-9248.141974. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Lauwers J. Mentoring and precepting lactation consultants. J Hum Lact. 2007;23:10–11. doi: 10.1177/0890334406297687. [DOI] [PubMed] [Google Scholar]
- 31.Schaefer RM, Huch R, Krafft A Anaemia Working Group. Current recommendations for the treatment of iron deficiency anemia. Rev Med Suisse. 2007;3:874–880. [PubMed] [Google Scholar]
- 32.Logan S, Martins S, Gilbert R. Iron therapy for improving psychomotor development and cognitive function in children under the age of three with iron deficiency anaemia. Cochrane Database Syst Rev. 2001;2:CD001444. doi: 10.1002/14651858.CD001444. [DOI] [PubMed] [Google Scholar]
- 33.Tsuzuki S, Morimoto N, Hosokawa S, Matsushita T. Associations of maternal and neonatal serum trace element concentrations with neonatal birth weight. PLoS One. 2013;8:e75627. doi: 10.1371/journal.pone.0075627. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Sachdev HPS, Gera T, Nestel P. Effect of iron supplementation on mental and motor development in children: Systematic review of randomised controlled trials. Pub Health Nutr. 2005;8:117–132. doi: 10.1079/phn2004677. [DOI] [PubMed] [Google Scholar]
- 35.Sachdev HPS, Gera T, Nestel P. Effect of iron supplementation on physical growth in children: Systematic review of randomised controlled trials. Pub Health Nutr. 2006;9:904–920. doi: 10.1017/phn2005918. [DOI] [PubMed] [Google Scholar]
- 36.Low M, Farrell A, Biggs BA, Pasricha SR. Effects of daily iron supplementation in primary-school-aged children: systematic review and meta-analysis of randomized controlled trials. CMAJ. 2013;19:791–802. doi: 10.1503/cmaj.130628. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Grantham-McGregor S, Ani C. A review of studies on the effect of iron deficiency on cognitive development in children. J Nutr. 2001;131:649–668. doi: 10.1093/jn/131.2.649S. [DOI] [PubMed] [Google Scholar]
- 38.Coad J, Pedley K. Iron deficiency and iron deficiency anemia in women. Scand J Clin Lab Invest Suppl. 2014;244:82–89. doi: 10.3109/00365513.2014.936694. [DOI] [PubMed] [Google Scholar]
- 39.Earl R, Woteki CE, editors. Institute of Medicine (US) Committee on the Prevention, Detection, and Management of Iron Deficiency Anemia Among U.S. Children and Women of Childbearing Age. Iron Deficiency Anemia: Recommended Guidelines for the Prevention, Detection, and Management Among U.S. Children and Women of Childbearing Age. Washington (DC): National Academies Press (US); 1993. [PubMed] [Google Scholar]