Abstract
Objectives:
To assess the prevalence, clinical characteristics, and predictors of obesity hypoventilation syndrome (OHS) in a large sample of Saudi patients with obstructive sleep apnea (OSA).
Methods:
This prospective observational study consisted of 1693 patients who were diagnosed to have sleep-disordered breathing using type I attended polysomnography (PSG) between January 2002 and December 2012 in the University Sleep Disorders Center (USDC) at King Saud University Hospital, Riyadh, Kingdom of Saudi Arabia.
Results:
Out of 1693 OSA patients, OHS was identified in 144 (8.5%) (women 66.7%). Compared with the pure OSA patients, the OHS patients were significantly older (57.4±13.4 years versus 46.8±13.7 years), had a higher body mass index (44.6±10.8 versus 35.7±9.2 kg/m2), a higher daytime partial pressure of carbon dioxide (PaCO2) (56.5±12.7 versus 41.6±6.7 mmHg), a longer duration of nocturnal oxygen saturation (nSaO2) <90% (71.0±34.3 versus 10.5±20.5 minutes), and a higher apnea hypopnea index (68.2±47.1 versus 46.5±34.1 events/hour). A multivariate logistic regression analysis showed that serum bicarbonate (odds ratio [OR]=1.17, p=0.0001, confidence interval [CI]=1.10-1.25), and duration of nSaO2 <90% (OR=1.05, p=0.0001, CI=1.04-1.06) were predictors of OHS.
Conclusion:
Obesity hypoventilation syndrome is common among Saudi OSA patients referred to the Sleep Disorders Center. Serum bicarbonate and duration of nSaO2 <90% are independent predictors of OHS among patients with OSA.
Sleep-related breathing disorders, also referred to as sleep-disordered breathing (SDB), are common conditions that encompass several disorders characterized by an abnormality in the frequency, pattern, upper airway resistance, and/or depth of breathing during sleep. Each disorder has its own diagnostic criteria. The most common SDB disorder is obstructive sleep apnea (OSA).1 The spectrum of SDB syndromes also includes obesity hypoventilation syndrome (OHS).2 Obesity hypoventilation syndrome was first described in 1955 as “Pickwickian syndrome.”3 Because most patients with OHS have frequent episodes of obstructive respiratory events during sleep and significant desaturation, OHS was incorrectly considered by some to be a severe form of OSA.2 The International Classification of Sleep Disorders, third edition (ICSD-3), defines OHS as the combined presence of obesity (BMI>30 kg/m²) with awake arterial hypercapnia (partial pressure of carbon dioxide (PaCO2)>45 mmHg) and SDB in the absence of other causes of alveolar hypoventilation.4 The OHS is under recognized, with only approximately 30% of hospitalized patients receiving a correct diagnosis when admitted with acute-on-chronic hypercapnia respiratory failure.5,6 Because OHS patients have more progressive disease courses, higher health-care utilization, poorer prognoses, and higher risks of hospitalization and death compared with pure OSA patients,7,8 it is essential to study the clinical characteristics of this group of patients to aid general physicians in understanding and recognizing the disorder. Therefore, this study was conducted to assess the prevalence, clinical characteristics, and predictors of OHS in a large sample of Saudi OSA patients presenting to the Sleep Disorders Clinic with clinical suspicion of SDB.
Methods
Subjects
This observational study was conducted in the University Sleep Disorders Center (USDC) at King Saud University Hospital, a tertiary-care university center in the Kingdom of Saudi Arabia. The USDC is a tertiary referral center that receives patients from various regions of the Kingdom. The local ethics committee approved the study, and informed consent was obtained from all participants. We included consecutive patients (≥18 years old) who were referred to the Sleep Disorders Clinic (SDC) with symptoms suggestive of OSA, underwent polysomnography (PSG) between January 2002 and December 2012, and chose to participate in the study. A detailed history and physical examination were performed by a sleep medicine specialist during the initial assessment, and spirometry was performed according to the American Thoracic Society/European Respiratory Society task force guidelines using a Master Screen (Jaeger, Würzburg, Germany).9 Arterial blood gases (ABGs) were drawn after 15 minutes of rest while the subjects were awake, seated and breathing room air, and they were analyzed using a GEM® Premier™ 4000 analyzer (Instrumentation Laboratory, Lexington, MA, USA). Spirometry and ABGs are part of the work-up of patients with diagnosed SDB in the USDC. Comorbidities data were obtained by history from the patient and from the medical chart of the patient. Daytime sleepiness was evaluated using the Epworth Sleepiness Scale (ESS),10 a validated, specialized sleep questionnaire containing 8 items that assess the likelihood of dozing in a variety of daily living situations. We excluded patients with congestive heart failure, chronic lung and neurological diseases, and thoracic vertebrae abnormalities, as well as those taking hypnotic medications. During the study period, 1973 patients were referred to the sleep disorders center with clinical suspicion of OSA. Among those, 1693 patients were diagnosed to have SDB, agreed to participate, and completed the required investigations.
Sleep study
Standard in-lab type I PSG was performed to monitor brain activity (electroencephalogram with electrodes placed at C3A2, C4A1, O1A2, and O2A1), muscle tone (electromyogram of both the legs and chin), eye movements (electrooculogram), electrocardiogram, oxygen saturation (finger pulse oximeter), chest and abdominal wall movements (thoracic and abdominal belts), airflow (thermistor and nasal prong pressure transducer), sleep position (body-position sensor), and snoring (microphone). The PSG recording was performed using Alice® 5 and Alice® 6 diagnostic equipment (Respironics Inc., Murrysville, PA, USA). Manual scoring of the electronic raw data was performed manually by expert certified sleep technologists in accordance with established criteria.11 Apnea was defined as a drop in the peak thermal sensor excursion greater than or equal to 90% of baseline for at least 10 seconds. The event was scored as obstructive apnea in the presence of continued respiratory effort and central apnea if associated with absent inspiratory effort throughout the entire period of absent airflow. Hypopnea was defined as a reduction in airflow of ≥30% of baseline that lasted for at least 10 seconds and resulted in either a ≥3% decrease in oxygen saturation from the pre-event baseline or an arousal. The apnea-hypopnea index (AHI) score was defined as the number of apneas and hypopneas per hour of sleep and was calculated for the entire sleep duration. The OSA was defined according to the International Classification of Sleep Disorders (ICSD 2014): 1) AHI ≥5 obstructive events/hour associated with one of the following: excessive daytime sleepiness or unrefreshing sleep, gasping, or choking during sleep, observed apnea or loud snoring or the patient has been diagnosed with hypertension, coronary artery disease, atrial fibrillation, or type 2 diabetes mellitus; or 2) AHI ≥15 obstructive events/hr.4 The desaturation index was defined as the number of desaturation events (≥3% decrease in oxygen saturation from the pre-event baseline) per hour of sleep. Sleep efficiency was calculated as the total sleep time/time in bed x 100.
The OHS was diagnosed if the following criteria were met: the presence of hypercapnia during wakefulness (PaCO2 >45 mm Hg), as measured by arterial PCO2; the presence of obesity (BMI >30 kg/m2); and hypoventilation not primarily due to a lung parenchymal or airway disease, pulmonary vascular pathology, a chest wall disorder (other than mass loading from obesity), medication uses, a neurological disorder, muscle weakness, or a known congenital or idiopathic central alveolar hypoventilation syndrome.4 Sleep hypoventilation was defined by an increase in end-tidal PCO2 to a value >55 mm Hg for ≥10 minutes or by an increase in end-tidal PCO2 of ≥10 mm Hg during sleep (compared with an awake supine value) to a value exceeding 50 mm Hg for ≥10 minutes.11 The OHS patients were divided into 2 groups: OHS with OSA if OHS criteria were met and the AHI score was ≥5 events/hour and pure OHS if the OHS criteria were met and the AHI score was <5 events/hour.
Statistical analysis
The data are expressed as the mean and standard deviation (SD) in both the text and tables. Student’s t-tests were used to compare the means for continuous data. For categorical data, the Chi square test was used. The results were considered statistically significant if p<0.05. To explore predictors of OHS, a univariate logistic regression model was used in a preliminary analysis; one explanatory variable was tested in the model at a time. Subsequently, variables with significant p-values were further evaluated using a multivariate logistic regression model.12 The multicollinearity was assessed by the correlation matrix among variables included in the model. The variables with high correlation were removed from the model. After fixing the multicollinearity, it was also re-assed by evaluating the standard error in the model. The overall accuracy of this model to predict OHS subjects (with a predicted probability of ≥0.5) is 93.3%. The sensitivity is given by 66% and the specificity is 96.7%. The area under the curve (ROC) is 0.962. The Nagelkerke R Square shows that approximately 63.8% of the variation in the outcome variable (OHS) is explained by this logistic model. Hosmer-Lemeshow goodness of fit test assured the model fit (p=0.218).
Results
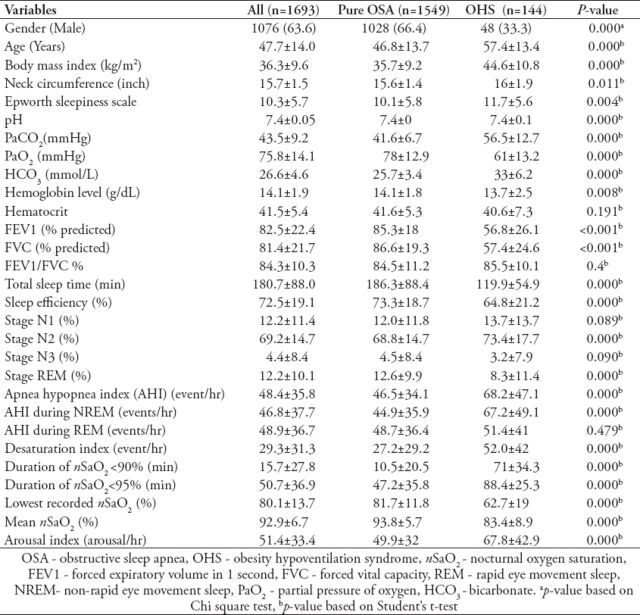
During the study period, 1973 patients were referred to the sleep disorders center with clinical suspicion of OSA. Among those, 1693 patients (1076 men and 617 women) were diagnosed to have SDB (OSA and OHS). Figure 1 shows the study population flow diagram. Table 1 presents the baseline characteristics and PSG findings of the overall study group, as well as of the OHS and pure OSA patients. The participants had a mean age of 47.7±14.0 years, a BMI of 36.3±9.6 kg/m2, and an ESS score of 10.3±5.7. Among patients diagnosed to have SDB, 8.5% (144/1693) patients met the criteria for OHS. Among the OSA patients with a BMI>40 kg/m2 (n=379), the OHS prevalence was 21% (n=79). The OHS patients had a mean age of 57.4±13.4 years, a BMI of 44.6±10.8 kg/m2, and an ESS score of 11.7±5.7. The mean BMI of OHS women was 44.9±9.7 kg/m2 and of men was 44.1±12.4 kg/m2 (p=0.7). The postmenopausal status among pure OSA women was 61.9% (n=323), and among OHS women was 88.5% (n=85), (p=0.0001). Among the OHS patients, 84 (58%) were recruited from the Sleep Disorders Clinic for an elective sleep study, and 61 (42%) were initially admitted with hypercapnic respiratory failure. In the latter patient group, the sleep study was performed once the patient was stable and prior to their discharge from the hospital.
Figure 1.
Study population flow diagram among patients referred for obstructive sleep apnea. OSA - obstructive sleep apnea, PSG - polysomnography, OHS - obesity hypoventilation syndrome
Table 1.
Demographic and sleep characteristics of all participants and comparisons between pure OSA and OHS patients.
Comparisons of the anthropometric, spirometric, and sleep characteristics of both the pure OSA and OHS groups are displayed in Table 1. The OHS patients were older and had higher BMIs, greater neck circumferences, and higher ESS and AHI scores. The OHS group had a higher proportion of women than the OSA group (66.7% versus 33.6%, p=0.0001). Among patients with SDB, the prevalence of OHS was significantly higher among women than among men (15.6% [96/617] versus 4.5% [48/1076]), (p=0.0001). An analysis of pulmonary function tests showed that the OHS patients had lower PaO2 values, higher PaCO2 and HCO3 values, and a more restrictive spirometric pattern reflected by lower FEV1 and FVC values. Sleep study analyses revealed that OHS patients spent more time in the N2 stage and less time in the N3 and REM stages compared with OSA patients. In addition, AHI scores, desaturation indexes, and duration of nocturnal oxygen saturation (nSaO2) <90% were significantly higher in the OHS group.
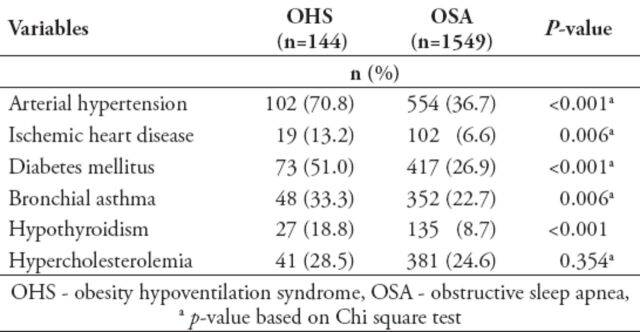
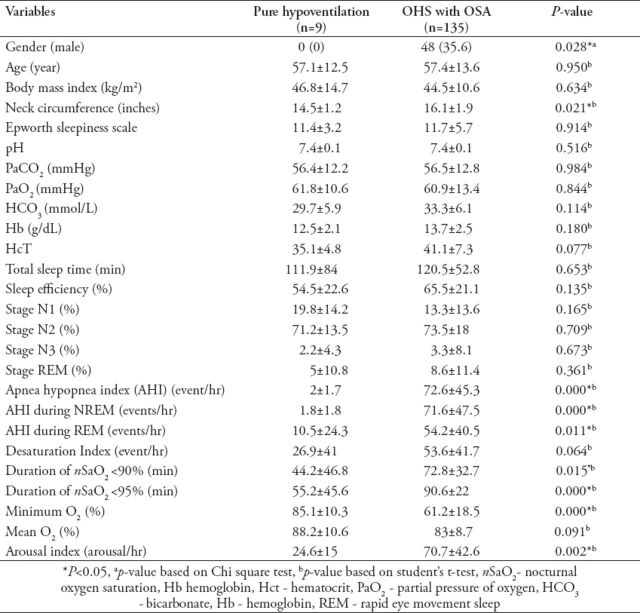
Table 2 compares the prevalence of comorbidities in the OHS and OSA patients. Although all included comorbidities were prevalent in both groups (pure OSA and OHS), comorbidities were significantly more prevalent among the OHS patients. The most prevalent comorbidities were hypertension 70.8%, diabetes mellitus 51.0%, and bronchial asthma 33.3%. The OHS patients were then divided into 2 groups (Table 3): OHS with OSA (135 patients, 93.75%, mean AHI: 72.6±45.3) and pure OHS (9 patients, 6.25%, mean AHI: 2.0±1.7/hour). The comparison between the 2 groups showed no differences in the anthropometric features. However, the OHS with OSA patients had longer durations of nSaO2 <90% (72.8±32.7% versus 44.2±46.8%), and they exhibited a lower minimum nSaO2 (61.2±18.5% versus 85.1±10.3%) and a higher arousal index (70.7±42.6 arousals/hour versus 24.6±15 arousals/hour).
Table 2.
Comparison between comorbidities in obstructive sleep apnea and obesity hypoventilation syndrome among 1693 patients referred to the sleep disorder center.
Table 3.
Comparison between patients with pure hypoventilation (OHS) and patients with OHS and obstructive sleep apnea (OSA).
A univariate regression analysis revealed that age (OR=1.06), female gender (OR=3.95), BMI ≥30 kg/m2 (OR=6.83), HCO3 (OR=1.37), and duration of nSaO2 <90% (OR=1.05) were predictors of OHS. A multivariate logistic regression analysis adjusted for other variables then showed that HCO3 (OR=1.17, p<0.001, CI=1.10-1.25) and duration of nSaO2 <90% (OR=1.05, p<0.001, CI=1.04-1.06) were predictors of OHS.
Discussion
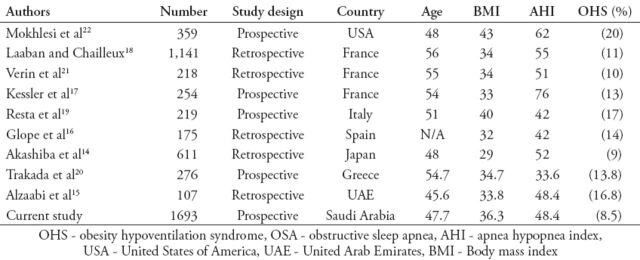
This study is one of the largest studies to describe the clinical characteristics of OHS patients and to determine the prevalence of OHS among OSA patients (Table 4). This investigation revealed that the prevalence of OHS among patients referred to the Sleep Disorders Clinic with OSA was 8.5%. Previous studies reported a prevalence of OHS among patients with OSA that ranged from 9-20% (Table 4).13-22 In a large French retrospective study (n=1141), the prevalence of OHS was 11% among OSA patients.18 Studies that reported a high prevalence of OHS recruited patients with high BMIs (≥40 kg/m2). Mokhlesi et al22 reported a prevalence of 20% in a sample of obese OSA patients with a mean BMI of 43 kg/m2. In a subgroup analysis of subjects with a BMI >40 kg/m2 in the French study, the prevalence of OHS was 24%.18 In our study, the mean BMI in the studied group was 36.3 kg/m2. We found that the prevalence of OHS among OSA patients with a BMI ≥40 kg/m2 was 21%, which is similar to that in previous studies in populations with a BMI >40 kg/m2. In our study, among patients diagnosed with OHS, the proportion of women was higher (66.7%). Based on previously published studies, the proportion of diagnosed patients with OHS tends to be higher among men (60%);13 however, male predominance is not as clear as in OSA patients. In fact, some studies demonstrated a higher proportion of OHS among women.15,23-25 Most of the previous studies did not assess the gender difference in the prevalence of OHS among patients diagnosed with SDB. In fact, the majority of the previous studies reported the gender proportion among OHS patients, which was misinterpreted by some as prevalence. Among patients with OSA, Akashiba et al14 reported higher prevalence of OHS among women (11.6%, [5/43]) compared with men (8.8% [50/568]) in Japan. In a recent study from the United Arab Emirates,15 although the proportion of men with OHS was higher (77.4%); however, the prevalence of OHS among women diagnosed with OSA was higher (31.8% [7/22] versus 12.9% [11/85]). The OHS was more prevalent among women and the women with OHS were older than the men with OHS.15 In our study, the prevalence of OHS among patients diagnosed with SDB was higher among women (15.6% [96/617] versus 4.5% [48/1076]). Therefore, it seems that women are at a higher risk for OHS. The cause for this is unknown. However, this finding can be related to postmenopausal status, as most of the OHS women in our study (88.5%) were postmenopausal. The risk of SDB has been reported to be at least 2.5 times higher among postmenopausal than premenopausal women.26,27 It is well documented as well that obesity in general is more common among women.28 In Saudi Arabia, obesity is more prevalent among women with a prevalence in women of 44% and in men of 26.4%.29 As OHS is a disease of the morbidly obese, this is a possible explanation for the higher prevalence of OHS among women. Another possible explanation is leptin resistance. Recent data suggests that leptin may act as a powerful respiratory stimulant. A mouse model of obesity and leptin deficiency exhibited abnormal patterns of breathing with elevated levels of CO2 and reduced ventilatory response to CO2 during wakefulness and sleep in a manner similar to that seen in humans with OHS.30 In obese subjects, serum leptin levels are significantly higher compared with lean subjects, which suggest that a central resistance to leptin may occur in obesity.29 Moreover, obese hypercapnic patients had higher fasting serum leptin levels than eucapnic patients and that serum leptin levels were shown to be better predictors of hypercapnia than body fat percentage.31,32 Gender differences in leptin concentration in obese subject have been reported. Serum leptin levels have been reported to be up to 4 times higher in obese women than men.33 It is possible that obese women may develop more resistance to the central effects of leptin compared with men and hence have a higher prevalence of OHS.
Table 4.
Comparison of obesity hypoventilation among patients with obstructive sleep apnea in previous studies.
An additional analysis revealed that 6.25% of our patients had hypoventilation without obstructive events (pure OHS). Previous studies have shown that the majority of patients with OHS have concomitant OSA (90%). The remaining 10% of patients have non-obstructive sleep hypoventilation (characterized by an AHI <5), which is defined as either an increase in PaCO2 of >10 mmHg above that of wakefulness or significant oxygen desaturation, neither of which is the result of apneas or hypopneas.2,23
Previous studies that attempted to determine risk factors or predictors of hypercapnia (OHS) in cohorts of patients with OSA reported mixed results.23 In the current study, OHS patients had higher AHI scores than those for pure OSA patients (68.2 versus 46.5 events/hour). Even when we compared OHS patients with OSA patients with a BMI >30 kg/m2, AHI scores were higher among the OHS patients (68.2 versus 51.3 events/hour). However, AHI was not identified as a predictor of OHS. In a previous study, Mokhlesi et al22 defined an AHI of 100/h as a highly specific threshold for the detection of patients with OHS. Nevertheless, the severity of AHI is not universally accepted as a good predictor of OHS. The use of AHI severity as a predictor of OHS may lead to significant under recognition of this serious medical problem.34
Serum bicarbonate was identified as an independent predictor of OHS in our study. Because serum bicarbonate is a continuous variable, a one-unit increase in serum bicarbonate causes a 14% increase in the probability of having OHS. In their prospective sample of patients with OSA, Mokhlesi et al22 reported that a serum bicarbonate threshold of 27 mmol/L had a sensitivity of 92% and specificity of 50% in predicting OHS. Duration of nSaO2 <90% was identified as an independent predictor of OHS in our study. Our findings concur with those of previous studies that showed that severe prolonged oxygen desaturation during sleep is a predictor of hypercapnia in OSA patients.18,35
An important finding of this study is the high prevalence of comorbidities in OHS patients. We know from previously published data that SDB is associated with increased cardiovascular comorbidities and diabetes mellitus.36 However, OHS patients have a much higher prevalence of serious comorbidities compared with OSA patients. Arterial hypertension was the most prevalent comorbidity, affecting more than two-thirds of OHS patients, followed by diabetes mellitus and bronchial asthma. Our data is consistent with those of previous studies that assessed comorbidities in OHS patients.20,37,38 However, our study had a larger sample size. obesity hypoventilation syndrome is a systemic process that involves multiple organ systems. Therefore, it is imperative to approach the obese patient with a multidisciplinary view to optimize therapy for each affected system.
In the present study, 42% of the OHS patients were admitted with acute hypercapnic respiratory failure. Obesity hypoventilation syndrome is generally overlooked as a cause of acute hypercapnic respiratory failure in morbidly obese patients.8 These patients may frequently be misdiagnosed as having chronic obstructive pulmonary disease (COPD) or chronic heart disease, resulting in delays in receiving the appropriate treatment.6 As a result, many patients may be treated inappropriately and may not have undergone an assessment of their hypoventilation and SDB.6,39 Previous studies have shown that only one-third of OHS patients receive the correct diagnosis when admitted with acute hypercapnic respiratory failure.6,40 The OHS is a serious disorder if left untreated, associated with increased morbidity and mortality.41 Therefore, early recognition is essential to prevent complications. Additionally, several previous studies have reported improved survival and a reduction in the need for hospitalization in treated compared with untreated OHS patients.41
The current study has several limitations that need to be addressed. The studied sample comprised patients referred to the Sleep Disorders Center with a clinical suspicion of OSA; therefore, they do not represent the general population. Future studies should aim to determine the prevalence of OHS in the general population. Another limitation is the small number of patients with pure OHS. However, pure OHS represents approximately 10% of OHS patients in previously published studies. Therefore, it is difficult to recruit a large number of patients.
In summary, this study showed that OHS is common among Saudi patients referred to the Sleep Disorders Center with OSA. Our study showed that OHS among Saudis is more prevalent among women. The prevalence of serious comorbidities is very high among patients with OHS. Serum bicarbonate and duration of nSaO2 <90% are independent predictors of OHS among patients with OSA. As a result of the obesity epidemic, the prevalence of OHS is likely to increase. Therefore, a high index of suspicion is necessary to facilitate early diagnosis and treatment of OHS.
Footnotes
Related Articles
Guven SF, Ciftci B, Lakadamyali H, Ciftci TU. The high dependency of supine position in obstructive sleep apnea. Saudi Med J 2013; 34: 147-152.
Alharbi MS, Sharif MM, Alotaibi DA, Shaikh S, BaHammam AS. Prevalence and predictors of hypertension in Saudi patients with obstructive sleep apnea. Saudi Med J 2010; 31: 585-586.
Bahammam AS, Al-Rajeh MS, Al-Ibrahim FS, Arafah MA, Sharif MM. Prevalence of symptoms and risk of sleep apnea in middle-aged Saudi women in primary care. Saudi Med J 2009; 30: 1572-1576.
References
- 1.Punjabi NM. The epidemiology of adult obstructive sleep apnea. Proc Am Thorac Soc. 2008;5:136–143. doi: 10.1513/pats.200709-155MG. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Al Dabal L, Bahammam AS. Obesity hypoventilation syndrome. Ann Thorac Med. 2009;4:41–49. doi: 10.4103/1817-1737.49411. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Auchincloss JH, Jr, Cook E, Renzetti AD. Clinical and physiological aspects of a case of obesity, polycythemia and alveolar hypoventilation. J Clin Invest. 1955;34:1537–1545. doi: 10.1172/JCI103206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.American Academy of Sleep Medicine. International classification of sleep disorders (ICSD) 3rd ed. Darien (IL): American Academy of Sleep Medicine; 2014. [Google Scholar]
- 5.Pépin JL, Borel JC, Janssens JP. Obesity hypoventilation syndrome: an underdiagnosed and undertreated condition. Am J Respir Crit Care Med. 2012;186:1205–1207. doi: 10.1164/rccm.201210-1922ED. [DOI] [PubMed] [Google Scholar]
- 6.BaHammam A, Syed S, Al-Mughairy A. Sleep-related breathing disorders in obese patients presenting with acute respiratory failure. Respir Med. 2005;99:718–725. doi: 10.1016/j.rmed.2004.10.021. [DOI] [PubMed] [Google Scholar]
- 7.Berg G, Delaive K, Manfreda J, Walld R, Kryger MH. The use of health-care resources in obesity-hypoventilation syndrome. Chest. 2001;120:377–383. doi: 10.1378/chest.120.2.377. [DOI] [PubMed] [Google Scholar]
- 8.BaHammam A. Acute ventilatory failure complicating obesity hypoventilation: update on a ’critical care syndrome’. Curr Opin Pulm Med. 2010;16:543–551. doi: 10.1097/MCP.0b013e32833ef52e. [DOI] [PubMed] [Google Scholar]
- 9.Miller MR, Hankinson J, Brusasco V, Burgos F, Casaburi R, Coates A, et al. Standardisation of spirometry. Eur Respir J. 2005;26:319–338. doi: 10.1183/09031936.05.00034805. [DOI] [PubMed] [Google Scholar]
- 10.Johns MW. Reliability and factor analysis of the Epworth Sleepiness Scale. Sleep. 1992;15:376–381. doi: 10.1093/sleep/15.4.376. [DOI] [PubMed] [Google Scholar]
- 11.Berry RB, Brooks R, Gamaldo CE, Harding SM, Lloyd RM, Marcus CL, et al. The AASM Manual for the Scoring of Sleep and Associated Events: Rules, Terminology and Technical Specifications. Version 2.1. Darien (IL): American Academy of Sleep Medicine; 2014. [updated January 2014]. Available from URL: http://www.aasmnet.org. [Google Scholar]
- 12.Bursac Z, Gauss CH, Williams DK, Hosmer DW. Purposeful selection of variables in logistic regression. Source Code Biol Med. 2008;3:17. doi: 10.1186/1751-0473-3-17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Mokhlesi B, Kryger MH, Grunstein RR. Assessment and management of patients with obesity hypoventilation syndrome. Proc Am Thorac Soc. 2008;5:218–225. doi: 10.1513/pats.200708-122MG. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Akashiba T, Akahoshi T, Kawahara S, Uematsu A, Katsura K, Sakurai S, et al. Clinical characteristics of obesity-hypoventilation syndrome in Japan: a multi-center study. Intern Med. 2006;45:1121–1125. doi: 10.2169/internalmedicine.45.1747. [DOI] [PubMed] [Google Scholar]
- 15.Alzaabi A, Fizal S, Moilothkandy R, Mahboub B, Nagelkerke N. Obesity hypoventilation syndrome in obstructive sleep apnea patients in the United Arab Emirates: a retrospective cross-sectional study. JRSM Short Rep. 2013;4 doi: 10.1177/2042533313510156. 2042533313510156. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Golpe R, Jiménez A, Carpizo R. Diurnal hypercapnia in patients with obstructive sleep apnea syndrome. Chest. 2002;122:1100–1101. doi: 10.1378/chest.122.3.1100. [DOI] [PubMed] [Google Scholar]
- 17.Kessler R, Chaouat A, Schinkewitch P, Faller M, Casel S, Krieger J, et al. The obesity-hypoventilation syndrome revisited: a prospective study of 34 consecutive cases. Chest. 2001;120:369–376. doi: 10.1378/chest.120.2.369. [DOI] [PubMed] [Google Scholar]
- 18.Laaban JP, Chailleux E. Daytime hypercapnia in adult patients with obstructive sleep apnea syndrome in France, before initiating nocturnal nasal continuous positive airway pressure therapy. Chest. 2005;127:710–715. doi: 10.1378/chest.127.3.710. [DOI] [PubMed] [Google Scholar]
- 19.Resta O, Foschino Barbaro MP, Bonfitto P, Talamo S, Mastrosimone V, Stefano A, et al. Hypercapnia in obstructive sleep apnoea syndrome. Neth J Med. 2000;56:215–222. doi: 10.1016/s0300-2977(00)00024-3. [DOI] [PubMed] [Google Scholar]
- 20.Trakada GP, Steiropoulos P, Nena E, Constandinidis TC, Bouros D. Prevalence and clinical characteristics of obesity hypoventilation syndrome among individuals reporting sleep-related breathing symptoms in northern Greece. Sleep Breath. 2010;14:381–386. doi: 10.1007/s11325-010-0360-5. [DOI] [PubMed] [Google Scholar]
- 21.Verin E, Tardif C, Pasquis P. Prevalence of daytime hypercapnia or hypoxia in patients with OSAS and normal lung function. Respir Med. 2001;95:693–696. doi: 10.1053/rmed.2001.1120. [DOI] [PubMed] [Google Scholar]
- 22.Mokhlesi B, Tulaimat A, Faibussowitsch I, Wang Y, Evans AT. Obesity hypoventilation syndrome: prevalence and predictors in patients with obstructive sleep apnea. Sleep Breath. 2007;11:117–124. doi: 10.1007/s11325-006-0092-8. [DOI] [PubMed] [Google Scholar]
- 23.Mokhlesi B. Obesity hypoventilation syndrome: a state-of-the-art review. Respir Care. 2010;55:1347–1362. discussion 1363-1365. [PubMed] [Google Scholar]
- 24.Nowbar S, Burkart KM, Gonzales R, Fedorowicz A, Gozansky WS, Gaudio JC, et al. Obesity-associated hypoventilation in hospitalized patients: prevalence, effects, and outcome. Am J Med. 2004;116:1–7. doi: 10.1016/j.amjmed.2003.08.022. [DOI] [PubMed] [Google Scholar]
- 25.Masa JF, Celli BR, Riesco JA, Hernández M, Sánchez De Cos J, Disdier C. The obesity hypoventilation syndrome can be treated with noninvasive mechanical ventilation. Chest. 2001;119:1102–1107. doi: 10.1378/chest.119.4.1102. [DOI] [PubMed] [Google Scholar]
- 26.Alotair H, Bahammam A. Gender differences in Saudi patients with obstructive sleep apnea. Sleep Breath. 2008;12:323–329. doi: 10.1007/s11325-008-0184-8. [DOI] [PubMed] [Google Scholar]
- 27.Young T, Finn L, Austin D, Peterson A. Menopausal status and sleep-disordered breathing in the Wisconsin Sleep Cohort Study. Am J Respir Crit Care Med. 2003;167:1181–1185. doi: 10.1164/rccm.200209-1055OC. [DOI] [PubMed] [Google Scholar]
- 28.Kanter R, Caballero B. Global gender disparities in obesity: a review. Adv Nutr. 2012;3:491–498. doi: 10.3945/an.112.002063. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Martin SS, Qasim A, Reilly MP. Leptin resistance: a possible interface of inflammation and metabolism in obesity-related cardiovascular disease. J Am Coll Cardiol. 2008;52:1201–1210. doi: 10.1016/j.jacc.2008.05.060. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Polotsky VY, Wilson JA, Smaldone MC, Haines AS, Hurn PD, Tankersley CG, et al. Female gender exacerbates respiratory depression in leptin-deficient obesity. Am J Respir Crit Care Med. 2001;164:1470–1475. doi: 10.1164/ajrccm.164.8.2101100. [DOI] [PubMed] [Google Scholar]
- 31.Phipps PR, Starritt E, Caterson I, Grunstein RR. Association of serum leptin with hypoventilation in human obesity. Thorax. 2002;57:75–76. doi: 10.1136/thorax.57.1.75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Shimura R, Tatsumi K, Nakamura A, Kasahara Y, Tanabe N, Takiguchi Y, et al. Fat accumulation, leptin, and hypercapnia in obstructive sleep apnea-hypopnea syndrome. Chest. 2005;127:543–549. doi: 10.1378/chest.127.2.543. [DOI] [PubMed] [Google Scholar]
- 33.Kapsimalis F, Kryger MH. Gender and obstructive sleep apnea syndrome, part 2: mechanisms. Sleep. 2002;25:499–506. [PubMed] [Google Scholar]
- 34.BaHammam A. Is apnea hypopnea index a good predictor for obesity hypoventilation syndrome in patients with obstructive sleep apnea? Sleep Breath. 2007;11:201. doi: 10.1007/s11325-007-0121-2. author reply 203-204. [DOI] [PubMed] [Google Scholar]
- 35.Kaw R, Hernandez AV, Walker E, Aboussouan L, Mokhlesi B. Determinants of hypercapnia in obese patients with obstructive sleep apnea: a systematic review and metaanalysis of cohort studies. Chest. 2009;136:787–796. doi: 10.1378/chest.09-0615. [DOI] [PubMed] [Google Scholar]
- 36.Borel JC, Borel AL, Monneret D, Tamisier R, Levy P, Pepin JL. Obesity hypoventilation syndrome: from sleep-disordered breathing to systemic comorbidities and the need to offer combined treatment strategies. Respirology. 2012;17:601–610. doi: 10.1111/j.1440-1843.2011.02106.x. [DOI] [PubMed] [Google Scholar]
- 37.Budweiser S, Riedl SG, Jörres RA, Heinemann F, Pfeifer M. Mortality and prognostic factors in patients with obesity-hypoventilation syndrome undergoing noninvasive ventilation. J Intern Med. 2007;261:375–383. doi: 10.1111/j.1365-2796.2007.01765.x. [DOI] [PubMed] [Google Scholar]
- 38.Borel JC, Burel B, Tamisier R, Dias-Domingos S, Baguet JP, Levy P, et al. Comorbidities and mortality in hypercapnic obese under domiciliary noninvasive ventilation. PLoS One. 2013;8:e52006. doi: 10.1371/journal.pone.0052006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Quint JK, Ward L, Davison AG. Previously undiagnosed obesity hypoventilation syndrome. Thorax. 2007;62:462–463. doi: 10.1136/thx.2006.075945. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Pérez de Llano LA, Golpe R, Ortiz Piquer M, Veres Racamonde A, Vázquez Caruncho M, Caballero Muinelos O, et al. Short-term and long-term effects of nasal intermittent positive pressure ventilation in patients with obesity-hypoventilation syndrome. Chest. 2005;128:587–594. doi: 10.1378/chest.128.2.587. [DOI] [PubMed] [Google Scholar]
- 41.Bahammam AS, Al-Jawder SE. Managing acute respiratory decompensation in the morbidly obese. Respirology. 2012;17:759–771. doi: 10.1111/j.1440-1843.2011.02099.x. [DOI] [PubMed] [Google Scholar]