Abstract
BACKGROUND/OBJECTIVES:
The goal of the study was to assess asthma control using asthma control test (ACT) and to explore the factors that effects asthma control among participants with bronchial asthma in the outpatient clinic setting.
METHODS:
This cross-sectional descriptive study was conducted in the outpatient primary care clinic at King Abdulaziz Medical City in Riyadh. Adult patients who were diagnosed with bronchial asthma by their primary treating physician were recruited over a 6-month period. Patients completed the ACT and questionnaires, which identified factors that affect asthma control.
RESULTS:
Four hundred asthmatic patients (n = 400) were enrolled, and 70% of these patients were women. Fifty-four percent of patients inappropriately used the inhaler device. The estimated prevalence of uncontrolled asthma at the time of the study was 39.8%. Inappropriate device use by the patient was more frequently associated with uncontrolled asthma (P—value = 0.001). Active smoking (P—value = 0.007), passive smoking (P—value = 0.019), unsealed mattress (P—value = 0.030), and workplace triggers (P—value = 0.036) were also associated with uncontrolled asthma. However, the extent of asthma control did not appear to be related to the existence of regular follow-ups, bedroom carpets, outpatient clinic visits, age, body mass index (BMI), or duration of asthma.
CONCLUSIONS:
The present study identified a high prevalence of uncontrolled asthma in the primary outpatient clinic setting and common risk factors that may contribute to poor asthma control.
Keywords: Asthma, asthma education, control, factors associated with poor asthma control, outpatients, uncontrolled
Asthma is a chronic inflammatory disorder of the airways that is characterized by airflow obstruction, bronchial hyper-responsiveness, and underlying inflammatory changes.[1] It is estimated that 300 million people are affected with asthma worldwide.[1] In Saudi Arabia, it is considered one of the common diseases, and almost 2 million patients are affected with a prevalence of approximately 20-25%.[2] Guidelines for asthma management, such as the Global Initiative for Asthma, were introduced to reduce asthma-associated mortality and morbidity by improving patient care and providing optimal asthma control.[3] According to the guidelines, the goal of asthma control is to prevent acute exacerbations and to minimize the symptoms of asthma (including night symptoms), use of bronchodilators, and limitations in activities.[4] Bronchial asthma is a major public health problem that negatively impacts patients, their families, and the community by inducing work and school loss, a poor quality of life, frequent emergency visits, hospitalizations, and death.[5,6] Large proportion of asthma direct and indirect asthma cost is due to severe and uncontrolled asthma.
In a study regarding asthma control, Marcus and colleagues showed that 81.9% of 1,009 patients had uncontrolled asthma in pulmonary clinics.[7] In 2009, Mintz and colleagues demonstrated that 58% of patients who visited their primary care clinics for various reasons had uncontrolled asthma.[8] Using the asthma control test (ACT), Al-Jahdali et al., assessed asthma control in 1,060 patients followed at five major tertiary centers in Riyadh and revealed that 64%, 31%, and 5% of patients had uncontrolled, well-controlled, and fully controlled asthma.[9] There is evidence that clinicians frequently over-estimate asthma control and under-estimate the impact of asthma on the patients’ lives.[10,11,12] The most common factors that have been identified to affect asthma control are related to environmental, physiological, and behavioral components.[13,14,15]
In a study conducted by Sanford and colleagues in 2010, the most common predictors of uncontrolled asthma in adults were low education, insurance status, current smoking status, body mass index (BMI) greater than 30 kg/m,2 and a history of gastroesophageal symptoms.[16] Another cross-sectional study in Brazil found three factors that were associated with uncontrolled asthma: Severity of asthma, access to medications, and use of inhaled corticosteroids.[17] One of the studies published locally revealed concerns regarding the side effects of and misconceptions about steroids, which are major factors for reduced compliance. However, this study did not explore other factors that may be related, such as whether the patient received proper education about asthma as a disease and the medication that was used.[18] Furthermore, Al-Jahdali and colleagues demonstrated that almost half of the patients in the emergency setting were not formally educated about asthma and majority used asthma devices improperly.[19]
Because the healthcare system differs in each country, the relative importance of factors that may contribute to asthma control is variable. There are no studies about factors associated with poor asthma control among Saudi patients. Therefore, studying and understanding these factors within the country can help in developing a local approach to control these factors and to decrease the burden and morbidity of the disease.[13] This study was undertaken to explore the factors that can affect asthma control in the outpatient clinic at primary care sitting and to measure the percentage of uncontrolled asthma, using the ACT, among participants.
Methods
This cross-sectional study was conducted at the King Abdulaziz Medical City-King Fahad National Guard Hospital in Riyadh outpatient clinics at community care clinics. We recruited all adult patients (more than 18 years old), who had a documented diagnosis of bronchial asthma (BA) by their primary treating physician and on asthma inhalers were. The following exclusion criteria were employed: Co-morbidity with similar presentation to BA (congestive heart failure, chronic obstructive pulmonary disease, and bronchiectasis), diagnosis of asthma less than 4 weeks, and undocumented diagnosis of asthma. The study was approved by the local institutional review board (Ref. RR11/138).
During the visit, the trained co-investigators asked patients to complete specific questionnaires that were developed based on a thorough review of existing literature and has been in our previous study.[20] These questionnaires specifically addressed factors that were pertinent to our patients, including demographic data, duration of the illness, medications used for asthma therapy, existence of regular follow-ups in outpatient clinics, location of follow-ups, frequency of follow-ups, number of emergency department (ED) visits or hospitalization, formal asthma education, and the participant's knowledge of asthma triggers. Co-investigators verified documented information by reviewing the medical record of each patient. Asthma control was assessed over the past 4 weeks by applying a validated, published, Arabic version of the ACT.[21] Appropriate inhaler techniques were also examined, according to previously reported procedures.[22]
Statistical analysis
The data were collected and analyzed using statistical package of social sciences (SPSS) version 21. Descriptive statistics, such as means and standard deviation, were used to summarize age, BMI, and the duration of BA. Counts and percentages were used to summarize gender, education, inhaler used, follow-ups in the clinic, education about asthma, education about therapy, and the patient's knowledge of environmental triggers. We used independent t-test to test whether the sources of asthma education effects patients’ knowledge about asthma. Demographic and clinical variables were compared in each group, according to the ACT scores and using the Chi-square test. Independent t-tests were used to compare other demographic and clinical data, such as age, BMI, and the duration of BA in patients with uncontrolled asthma and partially/fully controlled asthma. The Mann-Whitney U test was used to analyze quantitative data when the variable was not normally distributed.
Results
We enrolled 400 asthma patients in the study. Among these patients, 280 (70%) were women. The patients’ demographic and clinical characteristics are shown in Table 1. The mean age was 45.6 ± 16.2 years, and the mean duration of asthma was 9.5 ± 4.0 years. The mean BMI was 31.5 + 7.5 kg/m2. Approximately half of the patients had received a high school education or less, 38.9% had no education, and only 12% had university education. Uncontrolled asthma using ACT documented in 39.8%. There were 324 (81.4%) patients with regular physician follow-ups, whereas 74 (18.6%) patients did not have regular follow-ups. Approximately one-third (33.8%) of the asthmatic patients had reported ED visits. Improper use of inhaler devices documented in 53.8% of patients. The majority of patients received formal education about asthma (339; 84.8%) and asthma therapy (347; 87.0%). Of the 339 patients who received information about asthma, 68% received formal education from physicians, 21.2% received education from asthma educators, and 10.8% received education from pharmacists.
Table 1.
Demographics and education about bronchial asthma (BA) and asthma therapy (n = 400)
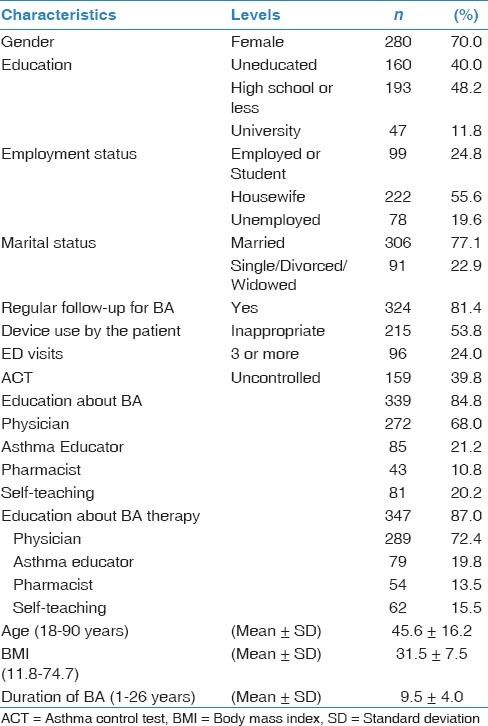
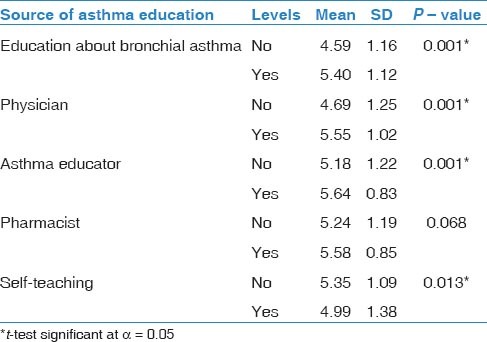
Table 2 demonstrates the patients’ knowledge of asthma and environmental factors that may trigger the disease. Two hundred and twenty-four (56.0%) patients were not aware that active smoking could trigger asthma, and the majority of participants (93.5%) reported that passive smoking was not a trigger of asthma. Most patients did not know that the bedroom carpet, unsealed mattress, or workplace triggers could trigger asthma (87.8%, 88%, and 71.2%, respectively). A significantly large number of patients (79.5%) reported that they stopped asthma therapy once they felt better, whereas 62.2% of patients increased or initiated steroid therapy when the attack was perceived. Furthermore, 368 (92.0%) patients said that they increased or started bronchodilator therapy once the attack was perceived. Only 2.5% of patients did not know what triggered their asthma. Almost half of the patients (50.8%) reported that they had prospectively discussed asthma management with their physician, and 72.8% of patients had discussed the asthma action plan. One hundred and forty-nine (37.2%) patients felt that asthma therapy was not safe for long-term use, and 138 (34.5%) patients believed that therapy was addictive [Table 2]. The relationship between the sources of asthma education and knowledge about bronchial asthma disease are illustrated in Table 3. More knowledge about asthma was observed in patients with education about bronchial asthma compared to those with no education (5.40 ± 1.12 vs. 4.59 ± 1.16, P − value = 0.001). Physician (P − value = 0.001) and Asthma Educator (P 0− value = 0.001) effects patients’ knowledge about asthma positively, while self-education about asthma (P − value = 0.013) effects patients’ knowledge about asthma negatively. Pharmacist had no effects on patients’ knowledge about asthma (P − value = 0.068).
Table 2.
Patients’ knowledge about environmental trigger for asthma and management of asthma
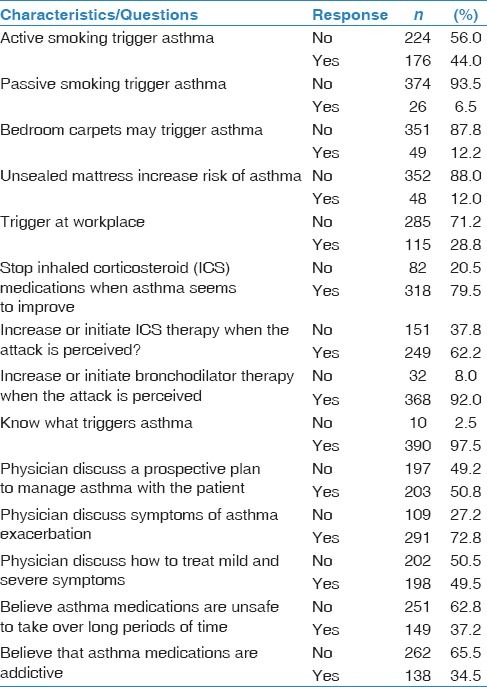
Table 3.
Patients’ knowledge about asthma and the source of asthma education
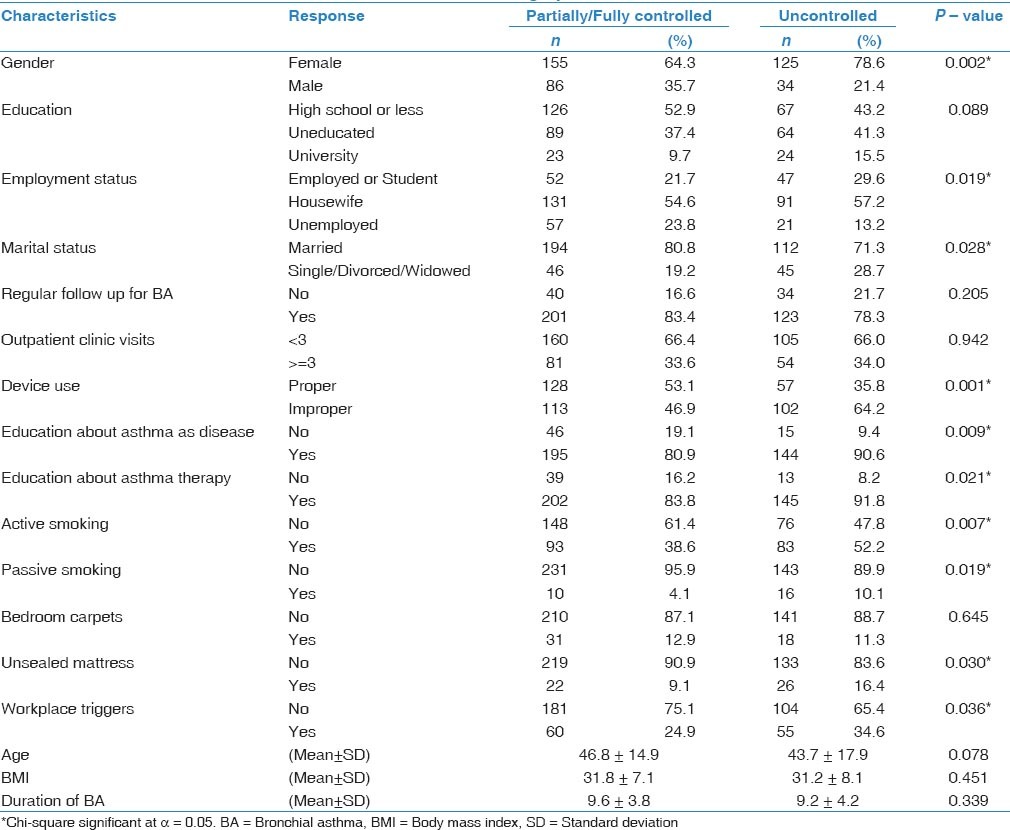
Uncontrolled asthma was defined as an ACT score ≤16. The relationship between the patients’ demographic or clinical characteristics and uncontrolled asthma are shown in Table 4. There was a significant relationship between Female gender and uncontrolled asthma (P - value =0.002). Unemployment was significantly associated with uncontrolled asthma (P − value = 0.019). In addition, uncontrolled asthma was more common in single or widowed patients (28.7%, P − value = 0.028). Improper device use by the patient was more frequently associated with uncontrolled asthma (46.9% partially/fully controlled vs. 64.2% uncontrolled asthma, P − value = 0.001). Active smoking (P − value = 0.007), passive smoking (P − value = 0.019), unsealed mattress (P − value = 0.030), and workplace triggers (P − value = 0.036) were also associated with uncontrolled asthma. However, the extent of asthma control did not appear to be related to existence of regular follow-ups, bedroom carpets, outpatient clinic visits, age, BMI, or duration of asthma.
Table 4.
The association of uncontrolled asthma with demographic and clinical characteristics
Discussion
Main findings
This study is one of the first to investigate factors that can interfere with asthma control in the outpatient setting of community care clinics in the region. Knowing the factors that hinder asthma control will help in the management of asthma and improve the quality of health care. Based on recent guidelines, experts have emphasized that patient education and regular clinic follow-ups can facilitate better asthma control. The asthma control level was demonstrated using the ACT, which is a well-validated tool. Our findings show that 39.8% of patients had uncontrolled asthma. Other studies have reported a higher percentage of uncontrolled patients.[7,8,9,23] We also investigated the common environmental factors that can trigger asthma, such as active smoking, passive smoking, and indoor/outdoor triggers. The majority of patients were not aware that all these factors could be considered asthma triggers. This observation was not unique for our population, and many studies have reported the same results.[13,14,15] A substantial number of participants (79.5%) stopped taking asthma medications when they felt that their asthma was improving. Common misconceptions and practice about asthma inhalers were revealed. Thirty-seven percent of patients believed that asthma therapy was not safe for regular use, and 34.5% of patients were concerned about the addictive effect of inhalers. These misconceptions have been previously reported.[19] These factors can be easily overcome by placing an emphasis on regular patient education, specifically regarding the role of inhalers in asthma treatment. A substantial number of participants (79.5%) stopped taking asthma medications when they felt that their asthma was improving. Common misconceptions and practice about asthma inhalers were revealed. Thirty-seven percent of patients believed that asthma therapy was not safe for regular use, and 34.5% of patients were concerned about the addictive effect of inhalers. In contrast to the study conducted by Al-Jahdali and colleagues in the emergency setting, the majority of patients (81.4%) had a regular follow-ups in the community care clinic for asthma management, most of the patients in this study received formal education about asthma either as a disease (84.8%) or therapy (87.0%).[19] Furthermore, most of the education was received from their physician (68%) with much less education received from the asthma educator. This is probably due to the lack of asthma educators in the primary care setting. A majority of patients used bronchodilators as their main inhaler, and 72.2% used it only for asthma therapy. Our findings revealed that 55.2% were using the meter-dosed inhaler as their main device, which is a common practice in Saudi Arabia, followed by a turbohaler. Similar to other studies; improper use of inhaler devices was common cause of uncontrolled asthma in our study.[18,19,22]
Strengths and limitations of this study
A major strength of this study lies in its direct interviewing of the patients and the confirmation of obtained information by reviewing medical records. The major limitation of our study is a single-center study and probably will not reflect national asthma care and control as the level of care is diverse across the country. Also we did not report the compliance because it was based on the patient report which was not reliable. Also this study did not address the quality of education given to the patients about asthma.
Interpretation of findings
Similar to previous study, this study showed that many asthmatic patients have misconceptions about asthma and its treatments.[19] Also many factors contributing to uncontrolled asthma, these factors can be easily overcome by placing an emphasis on regular patient education, specifically regarding the role of inhalers in asthma treatment.
The current study demonstrated the ineffectiveness of self-education in patients’ knowledge about asthma. This study was not designed to assess the quality of education given to the asthmatic patients by health educator, however, this study provided that asthma education given to the patient is of questionable quality in improving asthma control.
We speculate that improving communication with clear patient education and instruction of how to use inhaler devices on a regular basis and to know the asthma triggers and how to avoid them will improve asthma control.
In conclusion, the present study confirmed the high prevalence of uncontrolled asthma in the community outpatient clinic setting and identified risk factors that can contribute to poor asthma control. This studies also provided that asthma education given to the patient by health care provider is of questionable quality in improving asthma control and the need for structured asthma educational program.
Acknowledgment
We thank King Abdullah International Medical Research Center for their financial support.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
References
- 1.GINA. Global strategy for asthma management and prevention (GINA) of asthma. [Last accessed on 2013 Mar 21].
- 2.Al Frayh AR, Shakoor Z, Gad El Rab MO, Hasnain SM. Increased prevalence of asthma in Saudi Arabia. Ann Allergy Asthma Immunol. 2001;86:292–6. doi: 10.1016/s1081-1206(10)63301-7. [DOI] [PubMed] [Google Scholar]
- 3.Soriano JB, Rabe KF, Vermeire PA. Predictors of poor asthma control in European adults. J Asthma. 2003;40:803–13. doi: 10.1081/jas-120023572. [DOI] [PubMed] [Google Scholar]
- 4.NIH. Expert Panel Report 3: Guidelines for the Diagnosis and Management of Asthma. Bethesda (MD): National Heart, Lung, and Blood Institute; 2007. National Asthma Education and Prevention Program. NIH Publication No. 07-4051. NIH Publication No 07-4051. [Google Scholar]
- 5.Stewart WF, Ricci JA, Chee E, Morganstein D. Lost productive work time costs from health conditions in the United States: Results from the American Productivity Audit. J Occup Environ Med. 2003;45:1234–46. doi: 10.1097/01.jom.0000099999.27348.78. [DOI] [PubMed] [Google Scholar]
- 6.Buist AS, Vollmer WM. Reflections on the rise in asthma morbidity and mortality. JAMA. 1990;264:1719–20. [PubMed] [Google Scholar]
- 7.Marcus P, Arnold RJ, Ekins S, Sacco P, Massanari M, Stanley Young S, et al. CHARIOT Study Investigators. A retrospective randomized study of asthma control in the US: Results of the CHARIOT study. Curr Med Res Opin. 2008;24:3443–52. doi: 10.1185/03007990802557880. [DOI] [PubMed] [Google Scholar]
- 8.Mintz M, Gilsenan AW, Bui CL, Ziemiecki R, Stanford RH, Lincourt W, et al. Assessment of asthma control in primary care. Curr Med Res Opin. 2009;25:2523–31. doi: 10.1185/03007990903218655. [DOI] [PubMed] [Google Scholar]
- 9.Al-Jahdali HH, Al-Hajjaj MS, Alanezi MO, Zeitoni MO, Al-Tasan TH. Asthma control assessment using asthma control test among patients attending 5 tertiary care hospitals in Saudi Arabia. Saudi Med J. 2008;29:714–7. [PubMed] [Google Scholar]
- 10.Haughney J, Barnes G, Partridge M, Cleland J. The Living and Breathing Study: A study of patients’ views of asthma and its treatment. Prim Care Respir J. 2004;13:28–35. doi: 10.1016/j.pcrj.2003.11.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Horne R, Price D, Cleland J, Costa R, Covey D, Gruffydd-Jones K, et al. Can asthma control be improved by understanding the patient's perspective? BMC Pulm Med. 2007;7:8. doi: 10.1186/1471-2466-7-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Holgate ST, Price D, Valovirta E. Asthma out of control. A structured review of recent patient surveys? BMC Pulm Med. 2006;6:S2. doi: 10.1186/1471-2466-6-S1-S2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Chipps BE, Spahn JD. What are the determinates of asthma control? J Asthma. 2006;43:567–72. doi: 10.1080/02770900600619782. [DOI] [PubMed] [Google Scholar]
- 14.de Vries MP, van den Bemt L, Lince S, Muris JW, Thoonen BP, van Schayck CP. Factors associated with asthma control. J Asthma. 2005;42:659–65. doi: 10.1080/02770900500264903. [DOI] [PubMed] [Google Scholar]
- 15.Herjavecz I, Nagy GB, Gyurkovits K, Magyar P, Dobos K, Nagy L, et al. Cost, morbidity, and control of asthma in Hungary: The Hunair Study. J Asthma. 2003;40:673–81. doi: 10.1081/jas-120021100. [DOI] [PubMed] [Google Scholar]
- 16.Stanford RH, Gilsenan AW, Ziemiecki R, Zhou X, Lincourt WR, Ortega H. Predictors of uncontrolled asthma in adult and pediatric patients: Analysis of the Asthma Control Characteristics and Prevalence Survey Studies (ACCESS) J Asthma. 2010;47:257–62. doi: 10.3109/02770900903584019. [DOI] [PubMed] [Google Scholar]
- 17.Dalcin PT, Menegotto DM, Zanonato A, Franciscatto L, Soliman F, Figueiredo M, et al. Factors associated with uncontrolled asthma in Porto Alegre, Brazil. Braz J Med Biol Res. 2009;42:1097–103. doi: 10.1590/s0100-879x2009005000035. [DOI] [PubMed] [Google Scholar]
- 18.Al-Jahdali HH, Al-Zahrani AI, Al-Otaibi ST, Hassan IS, Al-Moamary MS, Al-Duhaim AS, et al. Perception of the role of inhaled corticosteroids and factors affecting compliance among asthmatic adult patients. Saudi Med J. 2007;28:569–73. [PubMed] [Google Scholar]
- 19.Al-Jahdali H, Anwar A, Al-Harbi A, Baharoon S, Halwani R, Al Shimemeri A, et al. Factors associated with patient visits to the emergency department for asthma therapy. BMC Pulm Med. 2012;12:80. doi: 10.1186/1471-2466-12-80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Ahmed AE, Al-Jahdali H, Al-Harbi A, Khan M, Ali Y, Al Shimemeri A, et al. Factors associated with poor asthma control among asthmatic patient visiting emergency department. Clin Respir J. 2014;8:431–6. doi: 10.1111/crj.12090. [DOI] [PubMed] [Google Scholar]
- 21.Lababidi H, Hijaoui A, Zarzour M. Validation of the Arabic version of the asthma control test. Ann Thorac Med. 2008;3:44–7. doi: 10.4103/1817-1737.39635. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Al-Jahdali H, Ahmed A, Al-Harbi A, Khan M, Baharoon S, Bin Salih S, et al. Improper inhaler technique is associated with poor asthma control and frequent emergency department visits. Allergy Asthma Clin Immunol. 2013;9:8. doi: 10.1186/1710-1492-9-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Rabe KF, Vermeire PA, Soriano JB, Maier WC. Clinical management of asthma in 1999: The Asthma Insights and Reality in Europe (AIRE) study. Eur Respir J. 2000;16:802–7. doi: 10.1183/09031936.00.16580200. [DOI] [PubMed] [Google Scholar]


