Abstract
RATIONALE:
Sepsis is a leading cause of intensive care unit (ICU) admissions worldwide and a major cause of morbidity and mortality. Limited data exist regarding the outcomes and functional status among survivors of severe sepsis and septic shock.
OBJECTIVES:
This study aimed to determine the functional status among survivors of severe sepsis and septic shock a year after hospital discharge.
METHODS:
Adult patients admitted between April 2007 and March 2010 to the medical-surgical ICU of a tertiary hospital in Saudi Arabia, were included in this study. The ICU database was investigated for patients with a diagnosis of severe sepsis or septic shock. Survival status was determined based on hospital discharge. Patients who required re-admission, stayed in ICU for less than 24 hours, had incomplete data were all excluded. Survivors were interviewed through phone calls to determine their functional status one-year post-hospital discharge using Karnofsky performance status scale.
RESULTS:
A total of 209 patients met the eligibility criteria. We found that 38 (18.1%) patients had severe disability before admission, whereas 109 (52.2%) patients were with severe disability or died one-year post-hospital discharge. Only one-third of the survivors had good functional status one-year post-discharge (no/mild disability). After adjustment of baseline variables, age [adjusted odds ratio (aOR) = 1.03, 95% confidence interval (CI) = 1.01-1.04] and pre-sepsis functional status of severe disability (aOR = 50.9, 95% CI = 6.82-379.3) were found to be independent predictors of functional status of severe disability one-year post-hospital discharge among survivors.
CONCLUSIONS:
We found that only one-third of the survivors of severe sepsis and septic shock had good functional status one-year post-discharge (no/mild disability). Age and pre-sepsis severe disability were the factors that highly predicted the level of functional status one-year post-hospital discharge.
Keywords: Disability, functional status, severe sepsis, septic shock
Sepsis is a life-threatening condition and continues to be a major challenge for health care organizations all over the world. In the US, the incidence of severe sepsis has been reported by 300 cases of severe sepsis per 100,000 people.[1,2] The associated mortality rate is high and approaches 18% for sepsis and 29% for severe sepsis.[2,3] Although it has been noticed that the in-hospital mortality rate of sepsis dropped from 27.8 to 17.9% between 1995 and 2000, the overall number of deaths continues to rise. Sepsis is the 10th leading cause of death and the second among patients in non-coronary intensive care units (ICUs) in the US.[2] In Saudi Arabia, studies have shown a mortality rate of 40-50% for septic shock patients.[4]
Patients who develop severe sepsis commonly suffer from prolonged stay in the ICU and hospital due to multi organ failure and residual sepsis-related disabilities. Studies showed that the mortality rate during the first year after sepsis continues to be high and the risk of death may persist for up to five years after hospital discharge.[5] Thus, using the in-hospital mortality or 28-day mortality may not be an ideal outcome measure. However, the available data on the long-term outcomes and quality of life among the severe sepsis and septic shock survivors are scarce. A prospective observational study in 24 Finnish ICUs showed a mortality rate two years after severe sepsis of 44.9% and the quality of life using the European Quality of Life 5-Dimensions (EQ)-5D assessment scale were lower after the episode of sepsis than before.[6] The primary objective of this study was to examine the functional status among the survivors of severe sepsis and septic shock one-year post-hospital discharge. We also determined the predictors of functional status.
Methods
Settings and subjects
This was a study conducted in King Abdulaziz Medical City (KAMC), Riyadh, Saudi Arabia, a 900-bed tertiary-care hospital. Data were extracted from the ICU electronic database for all severe sepsis and septic shock patients who were admitted to the 21-bed medical surgical ICU between April 2007 and March 2010. Patients admitted for at least 24 hours, 18 years and above, alive at the time of hospital discharge were included. Data from the first ICU admission were used for patients with multiple ICU admissions in the same hospitalization. Patients who were admitted to the ICU with cardiac arrest or had incomplete data were excluded.
Measurement
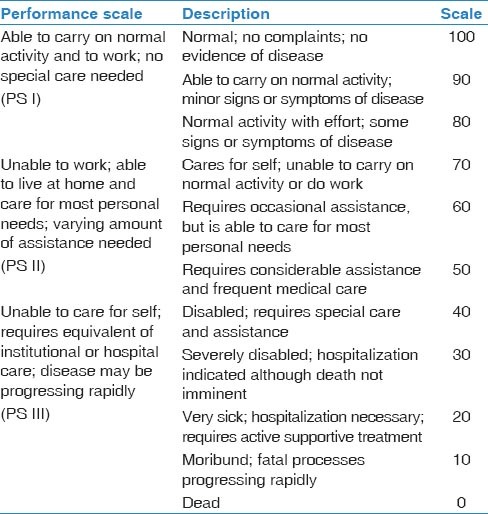
The principle investigator of this study performed telephonic interviews with the patients or next of kin to obtain data about the functional status before hospitalization for sepsis and one-year post-hospital discharge. Pre-sepsis and post-hospital discharge functional status for subjects were classified into three groups using the Karnofsky performance scale: No/mild disability, moderate disability and severe disability [Table 1].
Table 1.
Karnofsky performance scale
The following data were also obtained from the ICU database: Age, sex, chronic comorbidities, diagnostic category, admission serum lactate, creatinine, bilirubin, international normalized ratio (INR), and the acute physiology and chronic health evaluation (APACHE) II score. The following outcomes of sepsis were also noted: ICU and hospital length of stay, mechanical ventilation duration, renal replacement therapy and tracheostomy use.
Statistical analysis
Continuous variable are presented as means with standard deviations (SD) and medians with interquartile range (IQR) as appropriate. Chi-square and Fisher's exact tests were used to test for the significant association between the categorical variables as appropriate. The Student's t-test and analysis of variance (ANOVA) were used to compare the means of continuous variables as appropriate. Logistic regression was used to determine the predictors of the impaired functional status. Statistical analysis system (SAS) software was used for data statistical analysis.
Results
During the study period, we identified 209 subjects with severe sepsis and septic shock who met the study eligibility criteria.
Baseline characteristics
Table 2 describes the baseline characteristics of patients. They had a mean age of 55.9 ± 20.1 years and were predominantly males (53.6%) with APACHE II score of 24.3 ± 6.7. The main reasons for ICU referral and admission were due to cardiovascular instability (80.9%) followed by respiratory failure (10.0%). They had significant comorbid conditions. Based on the Karnofsky performance scale, 133 (63.3%) patients had no to mild disability, 38 (18.1%) had moderate disability, 38 (18.1%) had severe disability before the acute critical illness with sepsis. Data about the ICU and hospital length of stay, mechanical ventilation duration and the number of patients who received renal replacement therapy and tracheostomy are shown in Table 3.
Table 2.
Baseline characteristics of severe sepsis and septic shock survivors
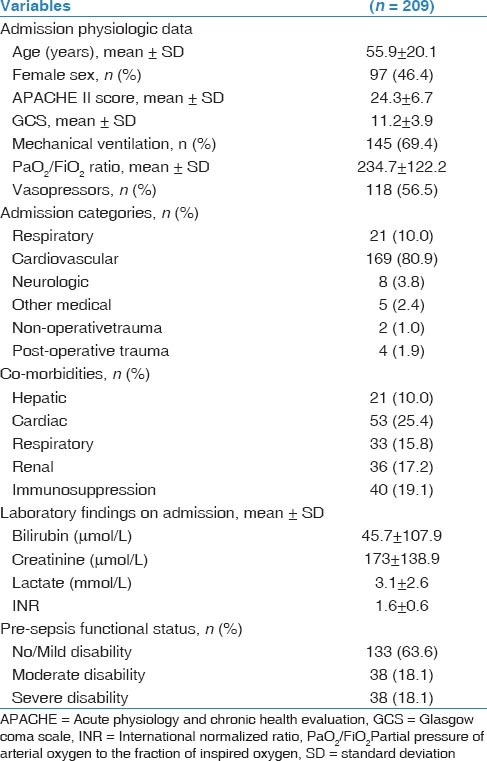
Table 3.
Outcomes among severe sepsis and septic shock survivors
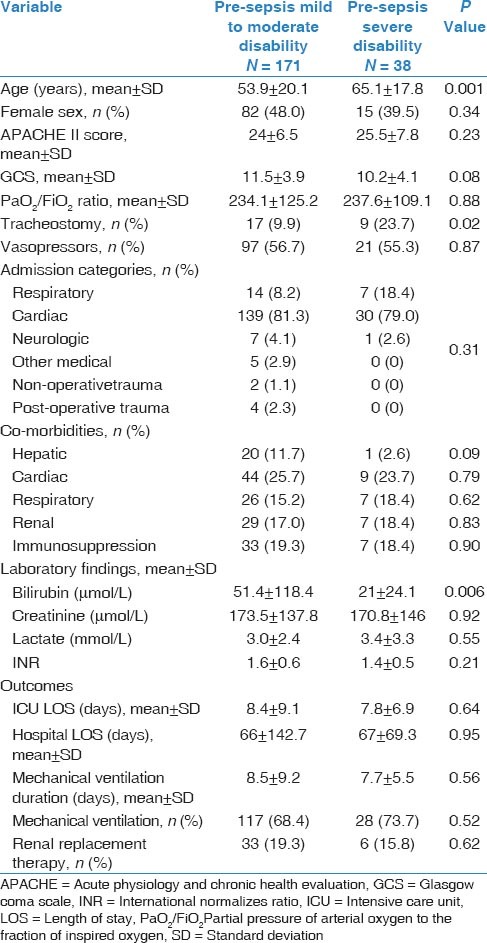
The baseline characteristics of patients who had good functional status and were with no/mild disability before sepsis were compared with the other two groups (moderate and severe disability before sepsis) and these results are shown in Table 4.
Table 4.
Comparison between patients who had mild to moderate disability with those who had severe disability pre-Sepsis
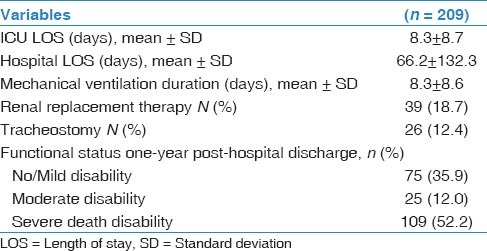
Functional one-year post-hospital discharge
One year after hospital discharge, 75 (35.9%) patients had no/mild disability, 25 (12.0%) were with moderate disability or died. The rest of the patients 109 (52.2) were severely disabled [Table 3].
Predictors of functional one-year post-hospital discharge
On bivariate analysis, severe disability before sepsis and age were associated with severe disability at one year post-discharge (odds ratio (OR) = 50.9, 95% CI = 6.82-379.3 (P < 0.0001) and 1.03, 95% CI = 1.01-1.04 (P 0.0002), respectively) [Table 5]. Multivariate analysis results demonstrated that pre-sepsis severe disability and age were independent predictors of post-sepsis severe disability (aOR 42.36, 95% CI = 5.62-319.32 (P 0.0003) and aOR 1.02, 95% CI = 1.01-1.04 (P 0.006), respectively) [Table 6].
Table 5.
Predictors of severe disability one-year posthospital discharge among severe sepsis and septic shock survivors
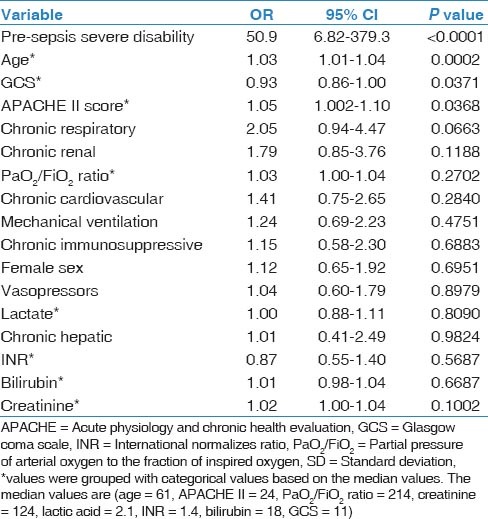
Table 6.
Results of multivariate analysis for predictors of severe disability (PS III) one-year post-hospital discharge among severe sepsis and septic shock survivors

Discussion
In this study, we found that approximately two-third (63%) of severe sepsis and septic shock patients had good functional status and no to mild disability before sepsis whereas one-third (37%) had moderate disability, and (18%) had severe disability. However, one year post-hospital discharge only one-third (36%) of the survivors had no/mild disability whereas 52% had severe disability or died.
The survivors of severe sepsis and septic shock are expected to experience various short-term disabilities due to organ dysfunctions that occur with severe sepsis. Our results suggest that severe sepsis and septic shock have significant impact on the functional status of affected patients for up to one year after hospital discharge and are consistent with the findings of other studies. Heyland et al., found that the health-related quality of life (HRQOL) for the sepsis patients was significantly lower than that of the general population.[7] A prospective study found a sharp multi-dimensional decline in the HRQOL and incomplete recovery after up to 6 months of discharge from the ICU/hospital.[8] Another finding of this was that the pre-sepsis HRQOL in patients who survived was lower in three dimensions (role-physical, mental health and vitality) when compared with the general population.[9]
Risk factors for the long-term outcomes of acute illnesses have been studied. The long-term functional status decline more significantly among elderly patients and patients with preexisting medical conditions surviving septic shock.[10,11,12] In addition, one study examined the relationship between the pre-hospitalization functional status and found that changes in the functional status related to experiencing a serious medical illness were independently related to 6-month mortality.[13] Hofhuis et al., conducted a prospective cohort study and found that the poor health related quality before sepsis could predict the patients outcomes after sepsis.[14] This finding is consistent with what was found in this study that age and pre-sepsis disability were independent predictors of the one-year functional status of survivors. Older patients and those experiencing severe disabilities before sepsis were at higher risk to die or experience more functional limitations/disabilities after sepsis.
The strengths of this study include the conduct of the study in a tertiary care hospital in Saudi Arabia, where a wide variety of complex patients were treated. Furthermore, this study evaluates the functional status pre-and post-sepsis over a long-term post hospital discharge. In term of limitations, the study was not a priori planned evaluation of functional status after discharge, and there is a possibility of recall bias. Although we adjusted for some baseline characteristics, we cannot rule out the presence of other confounders.
Conclusions
This study showed that only one-third of the survivors of severe sepsis or septic shock regained good functional status at one year after hospital discharge. In addition, age and pre-sepsis functional status of severe disability were significant factors on the survival probability and the functional status post-hospital discharge. Our findings highlight the importance of shifting the focus from trying to reduce the hospital and ICU length of stay to discharging patients with better functional status after severe sepsis and septic shock. Discharge planning and follow-up services after the hospital discharge for the survivors of severe sepsis and septic shock patients may help in producing better outcomes and better quality of life for these patients. We also recommend to conduct more interventional and observational studies that include long-term end-points to help in improving the patients’ outcomes and functionality.
Acknowledgments
We would like to thank the ICU, research committee members, medical records staff and Research team at King Abdullah International Medical Research Center (KAIMRC), Riyadh, Saudi Arabia.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
References
- 1.Angus DC, Pereira CA, Silva E. Epidemiology of severe sepsis around the world. Endocr Metab Immune Disord Drug Targets. 2006;6:207–12. doi: 10.2174/187153006777442332. [DOI] [PubMed] [Google Scholar]
- 2.Martin GS, Mannino DM, Eaton S, Moss M. The epidemiology of sepsis in the United States from 1979 through 2000. N Engl J Med. 2003;348:1546–54. doi: 10.1056/NEJMoa022139. [DOI] [PubMed] [Google Scholar]
- 3.Angus DC, Linde-Zwirble WT, Lidicker J, Clermont G, Carcillo J, Pinsky MR. Epidemiology of severe sepsis in the United States: Analysis of incidence, outcome, and associated costs of care. Crit Care Med. 2001;29:1303–10. doi: 10.1097/00003246-200107000-00002. [DOI] [PubMed] [Google Scholar]
- 4.Arabi Y, Al Shirawi N, Memish Z, Venkatesh S, Al-Shimemeri A. Assessment of six mortality prediction models in patients admitted with severe sepsis and septic shock to the intensive care unit: A prospective cohort study. Crit Care. 2003;7:R116–22. doi: 10.1186/cc2373. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Granja C, Dias C, Costa-Pereira A, Sarmento A. Quality of life of survivors from severe sepsis and septic shock may be similar to that of others who survive critical illness. Crit Care. 2004;8:R91–8. doi: 10.1186/cc2818. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Karlsson S, Ruokonen E, Varpula T, Ala-Kokko TI, Pettila V. Finnsepsis Study Group. Long-term outcome and quality-adjusted life years after severe sepsis. Crit Care Med. 2009;37:1268–74. doi: 10.1097/CCM.0b013e31819c13ac. [DOI] [PubMed] [Google Scholar]
- 7.Heyland DK, Hopman W, Coo H, Tranmer J, McColl MA. Long-term health-related quality of life in survivors of sepsis. Short Form 36: A valid and reliable measure of health-related quality of life. Crit Care Med. 2000;28:3599–605. doi: 10.1097/00003246-200011000-00006. [DOI] [PubMed] [Google Scholar]
- 8.Hofhuis JG, Spronk PE, van Stel HF, Schrijvers GJ, Rommes JH, Bakker J. The impact of critical illness on perceived health-related quality of life during ICU treatment, hospital stay, and after hospital discharge: A long-term follow-up study. Chest. 2008;133:377–85. doi: 10.1378/chest.07-1217. [DOI] [PubMed] [Google Scholar]
- 9.Hofhuis JG, Spronk PE, van Stel HF, Schrijvers AJ, Rommes JH, Bakker J. The impact of severe sepsis on health-related quality of life: A long-term follow-up study. Anesth Analg. 2008;107:1957–64. doi: 10.1213/ane.0b013e318187bbd8. [DOI] [PubMed] [Google Scholar]
- 10.Rubenfeld GD, Angus DC, Pinsky MR, Curtis JR, Connors AF, Jr, Bernard GR. Outcomes research in critical care: Results of the American Thoracic Society Critical Care Assembly Workshop on Outcomes Research. The Members of the Outcomes Research Workshop. Am J Respir Crit Care Med. 1999;160:358–67. doi: 10.1164/ajrccm.160.1.9807118. [DOI] [PubMed] [Google Scholar]
- 11.Herridge MS, Cheung AM, Tansey CM, Matte-Martyn A, Diaz-Granados N, Al-Saidi F, et al. One-year outcomes in survivors of the acute respiratory distress syndrome. N Engl J Med. 2003;348:683–93. doi: 10.1056/NEJMoa022450. [DOI] [PubMed] [Google Scholar]
- 12.Kaarlola A, Tallgren M, Pettila V. Long-term survival, quality of life, and quality-adjusted life-years among critically ill elderly patients. Crit Care Med. 2006;34:2120–6. doi: 10.1097/01.CCM.0000227656.31911.2E. [DOI] [PubMed] [Google Scholar]
- 13.Rozzini R, Sabatini T, Cassinadri A, Boffelli S, Ferri M, Barbisoni P, et al. Relationship between functional loss before hospital admission and mortality in elderly persons with medical illness. J Gerontol A Biol Sci Med Sci. 2005;60:1180–3. doi: 10.1093/gerona/60.9.1180. [DOI] [PubMed] [Google Scholar]
- 14.Hofhuis JG, Spronk PE, van Stel HF, Schrijvers AJ, Bakker J. Quality of life before intensive care unit admission is a predictor of survival. Crit Care. 2007;11:R78. doi: 10.1186/cc5970. [DOI] [PMC free article] [PubMed] [Google Scholar]


