Abstract
Certain nail changes are specific for various dermatological disorders. In addition, examination of nails may also provide an insight into more sinister systemic manifestations in the form of both subtle as well as specific changes. These findings may present as a defect of various anatomical components of the nail unit; nail matrix, nail plate and/or nail bed or vasculature. This article is an attempt to equip the dermatologists with a foresight to suspect and diagnose the unapparent systemic connotations that may be possible by a simple but detailed nail examination.
Keywords: Matrix, nail, nail bed, nail plate, nail unit, systemic diseases
INTRODUCTION
Subtle nail abnormalities can harbinger appalling systemic diseases. Hippocrates in the fifth century described clubbing as an important clue to myriad of systemic manifestations.[1] Since then many more nail findings have been found to be associated with systemic diseases. Therefore, examination of the nails should be an integral part of a complete dermatological examination. Clinicians must acquaint themselves with these nail findings as they can provide a clue in diagnosing certain systemic diseases. Moreover, at times, some nail changes can be a presenting feature before other signs of a systemic disease become clinically evident. With the convenience with which all 20 nails can be examined; certainly, they serve as an important diagnostic tool. Fingernails usually provide more accurate information than toenails, because clinical signs on toenails are often modified by trauma.
CLASSIFICATION
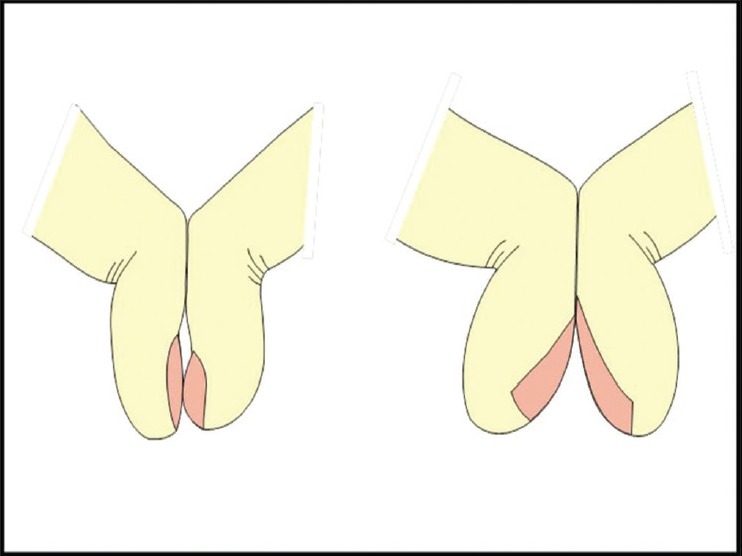
It is important to classify the nail involvement in systemic diseases according to its specificity of association [Box 1].[2]
Box 1.
Nail changes and systemic associations
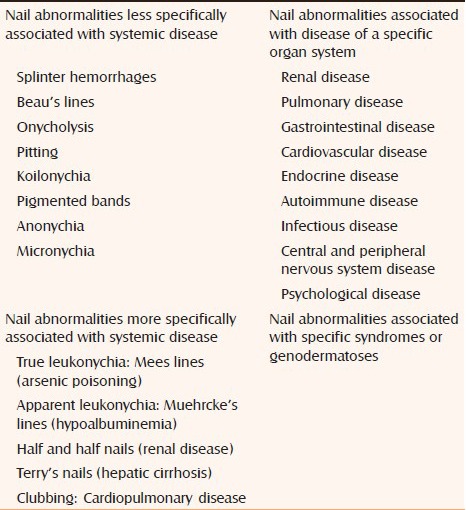
However, for a dermatologist, it is also important to classify them according to the clinical presentation, that is, morphological changes in the nail unit [Box 2]. We will discuss briefly the importance of these changes and their possible association with various systemic diseases.
Box 2.
Various morphological changes in the nail unit
Abnormalities of nail shape
Koilonychia
It is the presence of reverse curvature in the transverse and longitudinal axis, giving a concave dorsal aspect to the nail. These changes result in spooning of the nails capable of retaining a drop of water. It is appreciable more on fingernails then toenails [Figure 1]. Koilonychia can be idiopathic or associated with a variety of conditions such as iron deficiency anemia (Plummer Vinson syndrome), malnutrition, hemochromatosis, coronary disease, thyroid disorders, Upper gastrointestinal malignancy, traumatic injury, or occupational.[2,3] Koilonychia is of common occurrence in young infants but tend to disappear in early years of life in majority. Subungual hyperkeratosis accompanying koilonychias is suggestive of psoriasis. A number of factors, such as old age, digital ischemia, and so on, leading to thinning of nails may cause koilonychia. Occupational softening and iron deficiency are probably the most common causes.[4,5] Mild nail-plate thickening and discoloration are also indicative of an occupational cause. The petaloid nail is an early stage of koilonychia and is characterized by flattening of the nail.[6]
Figure 1.

Fingernails with koilonychia and trachyonychia
Hereditary and congenital forms are rare and are sometimes associated with other nail signs such as leukonychia. Transmission is dominant with high penetrance.
The exact cause of koilonychia is at best elusive. An angulation of the nail matrix secondary to connective tissue changes or spooning of the nail resulting from a relatively low distal matrix as compared with the proximal matrix, are some of the proposed hypotheses.[7]
Clubbing
It is characterized by increased nail plate curvature longitudinally and transversely with soft tissue hypertrophy of the digital pulp usually involving all 20 digits. Clubbing has been studied extensively and rationally and forms an integral component of any general physical examination in clinical practice. Because of an exhaustive list of systemic associations, it is classified into three major categories: Idiopathic, hereditary–congenital, and acquired.[6,7] It may have connotations with systemic diseases, such as cyanotic congenital heart diseases, infective endocarditis, primary and metastatic lung cancer, bronchiectasis, lung abscess, cystic fibrosis, mesothelioma, inflammatory bowel disease, and hepatic cirrhosis.[8,9]
Clubbing may be an early sign of AIDS in pediatric HIV-positive patients. It may be associated with hypertrophic osteoarthropathy, in which subperiosteal new bone formation in the distal diaphysis of the long bones of the extremities causes pain and symmetric arthritis-like changes in the shoulders, knees, ankles, wrists, and elbows.
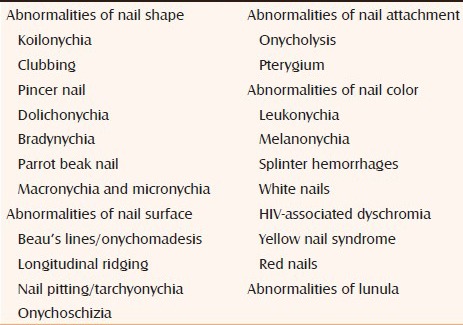
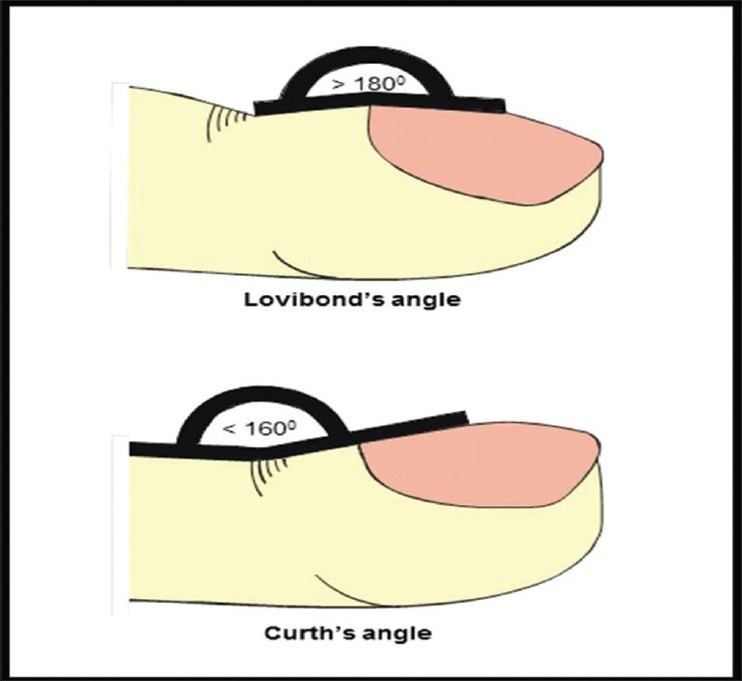
Three forms of geometric assessment can be performed in clubbing. (1) Lovibond's angle at the junction between nail plate and proximal nail fold and it is normally less than 160°. In clubbing, this is increased to over 180°. (2) Curth's angle at distal interphalangeal (DIP) joint is normally approximately 180° and this diminishes to less than 160° in clubbing [Figure 2]. (3) Schamroth sign refers to the obliteration of normally diamond-shaped space formed when dorsal sides of the distal phalanges of corresponding right and left digits are opposed [Figure 3].[10]
Figure 2.
Lovibond's angle and Curth's angle in patients with clubbing
Figure 3.
A diamond-shaped Schmaroth's window present normally is obliterated in patients with clubbing
Pincer nail
When the transverse curvature of the nail is increased along the longitudinal axis of the nail reaching to its greatest proportion toward the tip, it is called pincer nails. An association with a curved ingrown nail with bilateral penetration to the nail folds is not uncommon. Pincer nail may be hereditary or acquired. Although the mechanism of its development remains unknown, underlying systemic disease or medications are the common associations. The dorsal extension of bone caused by a subungual exostosis may also produce the pincer nail; hence the nail as well as the exostosis must be excised. The lateral borders of the nail exert a constant pressure, permanently constricting the deformed nail plate (unguis constringens). Moreover, a few reports suggest an onychomatricoma may present with a pincer nail. In addition, Kirkland and Sheth reported a case of acquired pincer nail deformity associated with end-stage renal disease secondary to diabetes mellitus.[4,11]
Dolichonychia
It is defined as the length of nails greatly exceeding the width of nail and has been associated with Marfan's syndrome and hypopituitarism.[12]
Brachyonychia
In brachyonychia, the width of the nail plate is reduced as compared to the length. It may be a feature of hyperparathyroidism and psoriatic arthropathy as an early sign of bone resorption.[10,13]
Parrot beak nail
A symmetrical overcurvature of the free edge of finger nails mimics the beak of a parrot. It is typically seen in severe acrosclerosis with distal phalangeal resorption due to scleroderma. The nail plate may bend around the shortened fingertip.[4,14]
Macronychia and micronychia
These constitute nails that are too large or too small compared with other nails on nearby digits. Macronychia may be due to local gigantism, whereas micronychia may occur in association with plexiform neuromas.[10]
Abnormalities of nail attachment
Onycholysis
Onycholysis refers to the distal separation of the nail plate from the nail bed [Figure 4]. Areas of separation appear white or yellow due to air beneath the nail and sequestered debris. It is more frequently associated with diverse local conditions such as trauma, psoriasis, fungus, and contact irritant reactions (nail cosmetics) than systemic disease. The correlation of onycholysis with the systemic diseases appears to be over-rated. Systemic associations include anemia, brochiectasis, lung cancer, cutaneous T-cell leukemia, diabetes mellitus, thyroid disorders, porphyria, lupus erythematosus, psoriatic arthritis, Sezary syndrome, drugs (psoralens and tetracyclines), and Vitamin C deficiency.[15,16] When it happens in thyrotoxicosis, the earliest stage is conversion of the curved adhesion line to a straight line. This adhesion line later dips proximally into the nail bed as a jagged projection. This description is that of Plummer's nails, which usually involves fourth and fifth fingers.[2]
Figure 4.

Onycholysis of fingernails in a patient with thyroid disorder
Pterygium
Pterygium unguis [Figure 5] results from a scarring involving the nail fold extending onto the matrix. It may be a “dorsal pterygium” where proximal nail fold fuses to matrix and later to nail bed or “ventral pterygium” where a distal extension of the hyponychium attaches to the undersurface of the nail plate thereby obliterating the distal nail groove. Dorsal pterygium is classically seen in lichen planus. It may also be seen in burns, cicatricial pemphigoid, dyskeratosis congenital, graft versus host disease, radiodermatitis, and lupus erythematosus. Also, ventral pterygium is seen in leprosy, neurofibromatosis, subungual exostosis, lupus erythematosus, and systemic sclerosis.[4,17]
Figure 5.

Pterygium in second and third fingernails in lichen planus
Abnormalities of nail surface
Longitudinal ridging (Onychorrhexis)
Longitudinal lines, or striations, may appear as indented grooves or projecting ridges and may represent long-lasting abnormalities [Figure 6]. Although a single nail fissure is most likely due to a minor trauma, systemic connotations have been found with systemic amyloidosis, nail-patella syndrome, collagen vascular diseases, graft versus host disease, and rheumatoid arthritis.[4,10]
Figure 6.

Longitudinal ridging with beading and fissuring associated with severe anemia
Central ridges can also be caused by iron, folic acid, or protein deficiency.
Beau's lines
Described first in 1846, Beau's lines are band-like depressions extending from one lateral edge of the nail to the other. It is the most common and least specific nail change in a systemic disease. Its exact cause is not known but there is temporary cessation of nail growth in the matrix by various factors, for example, trauma involving proximal nail fold, severe acute illness such as fever, heart attack, exposure to extreme cold, psychological stress, and poor nutritional status. Idiopathic and inherited forms also occur. If there is complete inhibition of nail growth for around 2 weeks, Beau's line will reach maximum depth resulting in onychomadesis [Figure 7]. Recurrent bouts of illness may lead to the formation of series of transverse furrows/grooves [Figure 7]. The width of the transverse groove relates to the duration of the disease that has affected the matrix. The distal limit of the furrow, if abrupt, indicates a sudden attack of disease; if sloping, a more protracted onset.[18] The presence of Beau's lines on all 20 nails is usually the result of systemic disease such as mumps, pneumonia, coronary thrombosis, Kawasaki disease, syphilis, and hypoparathyroidism.[4,10]
Figure 7.

Multiple Beau's lines in the middle finger and onychomadesis in the index finger
Nail pitting/trachyonychia
Pits result from a defective keratinization of the proximal matrix with persistence of parakeratotic cells in the nail plate surface.[19] Its role and diagnostic utility is doubtful as a large number of local factors affect the matrix function. It may occasionally be useful in diseases such as psoriasis, psoriatic arthritis [Figure 8], SLE, dermatomyositis, syphilis, sarcoidosis, and pemphigus vulgaris.[2,19,20]
Figure 8.

Trachyonychia in a patient with psoriatic arthritis without skin lesions
Onychochizia
Horizontal splitting of nail toward its distal portion is also called lamellar splitting of nail. Although trauma is the most common cause, it has been reported with X-linked chondrodysplasia punctata, polycythemia vera, and systemic retinoid therapy.[4,21]
Abnormalities of nail color
Leukonychia
Leukonychia refers to the white discoloration of nail. It is traditionally classified into three subtypes.[22]
True, when pathology originates in matrix and emerges in the nail plate.
Apparent, when pathology is in the nail bed.
Pseudo, when nail plate pathology is exogenous, for example, onychomycosis [Figure 9].
Figure 9.

Superficial white onychomycosis
Leukonychia associated with systemic disease is usually true or apparent
Mees lines: True leukonychia due to arsenic intoxication is characterized by a single or multiple, transverse, narrow whitish line running along the width of the nail and parallel to lunula, and may involve multiple nails. These lines do not disappear on blanching and move distally with time.[23,24] Histology shows fragmented nail plated with foci of parakeratotic cells. They have been reported with other conditions as well such as Hodgkin's disease, leprosy, tuberculosis, malaria, herpes zoster, chemotherapeutic drugs, carbon monoxide (CO) and antimony poisoning, renal and cardiac failure, pneumonia, and childbirth.
Muehrcke's lines: These are apparent leukonychia characterized by double white transverse line [Figure 10], resulting possibly from a localized edematous state in the nail bed exerting pressure on the vascular bed. They are specific for hypoalbuminic state (occur in patients albumin <2 g/dL) and disappear when the protein level normalizes. Muehrcke's lines are seen in nephrotic syndrome, glomerulonephritis, liver disease, chemotherapeutic drugs, and malnutrition.[22,25,26]
Half and half nail or Lindsay nail: Apparent leukonychia with a normal proximal half and abnormal brownish discolored distal half [Figure 11]. It is seen in patients of chronic kidney disease with uremic renal failure.[26,27]
Terry nails: Apparent leukonychia with nail that is white proximally and normal distally [Figure 12]. It is associated with congestive cardiac failure, adult-onset diabetes mellitus, peripheral vascular disease, hemodialysis, and HIV.[27,28]
Figure 10.

Muehrcke's lines in a patient with end-stage renal disease with hypoalbuminemia of <2 gm%
Figure 11.

Half and half nails in a patient with chronic kidney disease
Figure 12.

Terry's nails in a patient with congestive heart failure
Melanonychia
A longitudinal or transverse brownish black pigmentation of nail has been typically attributed to lichen planus commonly seen in our clinics. Melanonychia may be part of being racial pigmentation (constitutional). However, an underlying melanocytic nevus or malignant melanoma, drugs (antimalarials, minocycline, phenytoin, psoralens, sulfonamides, zidovudine, doxorubicin, methotrexate, azathioprine, and so on), hemochromatosis, malnutrition, thyroid disease, smoking, HIV infection [Figure 13], and Addison's disease can present similarly.[4,29]
Figure 13.

Diffuse melanonychia involving all nails in a HIV+ve patient
Cyanosis
Cyanosis may manifest as blue or purple discoloration of the nail bed and digits as a result of lower oxygen saturation causing accumulation of deoxyhemoglobin in the small blood vessels of the extremities. Central cyanosis is caused by congenital heart diseases and may manifest on mucosa and extremities, whereas peripheral cyanosis is usually diagnosed by examination of the nail and digits and is caused by vasoconstriction and diminished peripheral blood flow as occurs in cold exposure, shock, congestive cardiac failure, and peripheral vascular disease.[10]
Icterus
Yellowish discoloration of the mucosae as a result of deposition of bilirubin may extend to involve the nails in severe cases and may represent severe form of liver disease or hemolysis.[10]
Nicotine staining of nails
Heavy smokers may develop a yellow discoloration of nail due to nicotine deposition. The discoloration may be a tell tale sign of long-term chances of development of cigarette-associated diseases such as carcinoma lung, chronic obstructive airway disease, and coronary artery disease.[10,30]
Splinter hemorrhages
Splinter hemorrhages in nails are formed by the extravasation of blood from the longitudinally oriented vessels of the nail bed. They occur commonly in psoriasis but may be seen in the setting of infective endocarditis [Figure 14], rheumatic heart disease, valvular replacement, SLE, antiphospholipid syndrome, IV drug abusers, and congenital heart diseases. A simultaneous occurrence in multiple nails is indicative of a systemic cause.[2,22,31]
Figure 14.

Splinter hemorrhage with bacterial endocarditis
Yellow nail syndrome
It is characterized by thickening and yellow to yellow-green discoloration of the nails often associated with systemic disease, most commonly lymphedema and compromised respiration due to pleural effusion [Figure 15]. The condition usually occurs in adults but may occur in childhood. The lunula is obscured and there is increased transverse and longitudinal curvature with loss of cuticle.[10,32]
Figure 15.

Yellow discoloration of all nail syndrome
Red lunula
Red lunulae are seen in collagen vascular disease, cardiac failure, chronic obstructive pulmonary disease (COPD), cirrhosis, chronic urticaria, psoriasis, and CO poisoning[33] It may merge with the nail bed in the distal part of the lunula or be demarcated by a pale line and can be obliterated by pressure on the nail plate.[10]
Nail bed telangiectasia
Periungual telangiectasia is an important clue to systemic involvement in systemic sclerosis, SLE [Figure 16], and dermatomyositis influencing the prognosis of the disease. Furthermore, they may also be seen in diabetes mellitus, COPD, and rheumatoid arthritis.[2,34]
Figure 16.

Nail bed telangiectasia in a patient with disseminated lupus erythematosus
Nail abnormalities in specific organ system
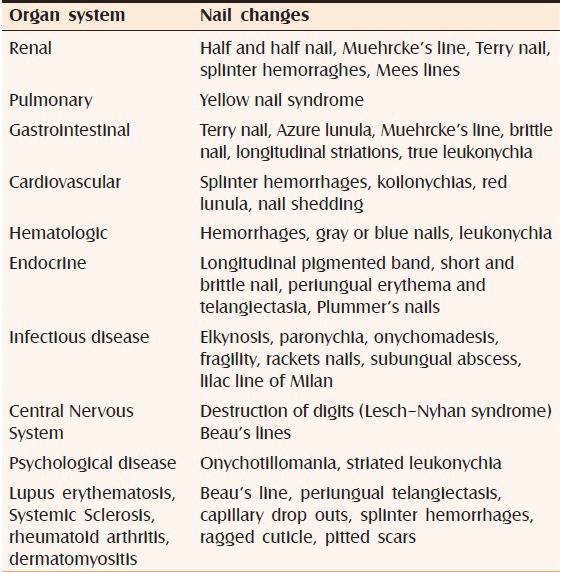
Table 1 depicts nail involvement associated with certain specific organ systems. Although overlap in findings is common, subtle changes may predict sinister internal involvement.[22]
Table 1.
Nail manifestation specific to organ system involvement
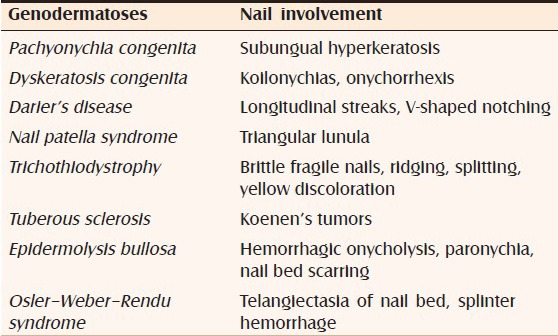
Nail involvement in genodermatosis
Genodermatosis may present with a constellation of signs and symptoms thereby clinching the diagnosis. However, many times subtle but characteristic findings in nails bring us very close to the diagnosis itself. Table 2 depicts genodermatosis associated with nail involvement.[22,35]
Table 2.
Nail manifestations in genodermatoses
Hence, nail findings may not only be window to a plethora of possible systemic associations, but also a window of opportunity as a profound knowledge of the associations may be useful in a complete and targeted workup of the patient to pre-empt the clinching of a more sinister systemic disease.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Myers KA, Farquhar DR. The rational clinical examination. Does this patient have clubbing? JAMA. 2001;286:341–7. doi: 10.1001/jama.286.3.341. [DOI] [PubMed] [Google Scholar]
- 2.Lawry M, Daniel CR., 3rd . Nails in systemic disease. In: Scher RK, Daniel CR, editors. Nails: Diagnosis, Therapy, Surgery. 3rd ed. Philadelphia: Elsevier Science Limited; 2005. pp. 147–69. [Google Scholar]
- 3.Kumar V, Aggarwal S, Sharma A, Sharma V. Nailing the diagnosis: Koilonychia. Perm J. 2012;16:65. doi: 10.7812/tpp/12.961. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Baran R, Dawber RP, Haneke E, Tosti A, Bristow I. Martin Dunitz. 3rd ed. 2005. Nail configuration abnormalities. A Text Atlas of Nail Disorders: Techniques in Investigation and Diagnosis; pp. 18–24. [Google Scholar]
- 5.Bentley-Phillips B, Bayles MA. Occupational koilonychia of the toe nails. Br J Dermatol. 1971;85:140–4. doi: 10.1111/j.1365-2133.1971.tb07199.x. [DOI] [PubMed] [Google Scholar]
- 6.Stone OJ. Spoon nails and clubbing. Cutis. 1975;16:235–41. [Google Scholar]
- 7.Stone OJ. Diseases of nail and their management. Cutis. 1975;16:235. [Google Scholar]
- 8.Braunwald E. Hypoxia and cyanosis. In: Kasper DL, Braunwald E, Fauci AS, Hauser SL, Longo DL, Jameson JL, editors. Harrison Principles of Internal Medicine. 16th ed. New York: McGraw-Hill; 2009. pp. 209–12. [Google Scholar]
- 9.Hansen-Flaschen J, Nordberg J. Clubbing and hypertrophic osteoarthropathy. Clin Chest Med. 1987;8:287–98. [PubMed] [Google Scholar]
- 10.Motswaledi MH, Mayayise MC. Nail changes in systemic diseases. SA Fam Pract. 2010;52:409–13. [Google Scholar]
- 11.Kirkland CR, Sheth P. Acquired pincer nail deformity associated with end stage renal disease secondary to diabetes. Dermatol Online J. 2009;15:17. [PubMed] [Google Scholar]
- 12.Cohen PR, Milewicz DM. Dolichonychia in women with Marfan syndrome. South Med J. 2004;97:354–8. doi: 10.1097/01.SMJ.0000110333.94390.E1. [DOI] [PubMed] [Google Scholar]
- 13.Rasi A, Soltani-Arabshahi R, Naraghi ZS. Circumscribed juvenile-onset pityriasis rubra pilaris with hypoparathyroidism and brachyonychia. Cutis. 2006;77:218–22. [PubMed] [Google Scholar]
- 14.Desai T, Magdum A, Patel T, Loghdey S. Parrot-beak nails. Clin Exp Dermatol. 2011;36:208–9. doi: 10.1111/j.1365-2230.2010.03899.x. [DOI] [PubMed] [Google Scholar]
- 15.Zaic MN, Daniel CR. Nails in systemic disease. Dermatologic Therapy. 2002;15:99–106. [Google Scholar]
- 16.Daniel CR., 3rd Onycholysis: An overview. Semi Dermatol. 1991;10:34–40. [PubMed] [Google Scholar]
- 17.Richert BJ, Patki A, Baran RL. Pterygium of the nail. Cutis. 2000;66:343–6. [PubMed] [Google Scholar]
- 18.Yassin MA, Alhijji IA, Elayoubi HR, Abbodi KR. Beaus lines. Saudi Med J. 2007;28:1922–3. [PubMed] [Google Scholar]
- 19.Jadhav VM, Mahajan PM, Mhaske CB. Nail pitting and onycholysis. Indian J Dermatol Venereol Leprol. 2009;75:631–3. doi: 10.4103/0378-6323.57740. [DOI] [PubMed] [Google Scholar]
- 20.Singh SK. Finger nail pitting in psoriasis and its relation with different variables. Indian J Dermatol. 2013;58:310–2. doi: 10.4103/0019-5154.113955. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Baran R. Therapeutic assessment and side-effects of the aromatic retinoid on the nail apparatus. Ann Dermatol Venereol. 1982;109:367–71. [PubMed] [Google Scholar]
- 22.Singh G. Nails in systemic disease. Indian J Dermatol Venereol Leprol. 2011;77:646–51. doi: 10.4103/0378-6323.86472. [DOI] [PubMed] [Google Scholar]
- 23.Daniel CR, 3rd, Osment LS. Nail pigmentation abnormalities. Their importance and proper examination. Cutis. 1980;25:595–607. [PubMed] [Google Scholar]
- 24.Chesnut G, Taylor S, Belin E. Mees lines and Beau lines. Cutis. 2013;91(150):147–1. [PubMed] [Google Scholar]
- 25.Gregoriou S, Argyriou G, Larios G, Rigopoulos D. Nail disorders and systemic disease: What the nails tell us. J Fam Pract. 2008;57:509–14. [PubMed] [Google Scholar]
- 26.Goodman GJ, Nicolopoulos J, Howard A. Diseases of the generative nail apparatus. Part II: Nail bed. Australas J Dermatol. 2002;43:157–70. doi: 10.1046/j.1440-0960.2002.00588.x. [DOI] [PubMed] [Google Scholar]
- 27.Tosti A, Daniel CR, 3rd, Piraccini BM, Iorizzo M. Heidelberg: Springer Verlag; 2010. Color Atlas of Nails; p. 3. [Google Scholar]
- 28.Saray Y, Seçkin D, Güleç AT, Akgün S, Haberal M. Nail disorders in hemodialysis patients and renal transplant recipients: A case-control study. J Am Acad Dermatol. 2004;50:197–202. doi: 10.1016/j.jaad.2003.07.014. [DOI] [PubMed] [Google Scholar]
- 29.Mendiratta V, Jain A. Nail dyschromias. Indian J Dermatol Venereol Leprol. 2011;77:652–8. doi: 10.4103/0378-6323.86473. [DOI] [PubMed] [Google Scholar]
- 30.Verghese A, Krish G, Howe D, Stonecipher M. The harlequin nail. A marker for smoking cessation. Chest. 1990;97:236–8. doi: 10.1378/chest.97.1.236. [DOI] [PubMed] [Google Scholar]
- 31.Monk BE. The prevalence of splinter haemorrhages. Br J Dermatol. 1980;103:183–5. doi: 10.1111/j.1365-2133.1980.tb06588.x. [DOI] [PubMed] [Google Scholar]
- 32.Emerson PA. Yellow nails, lymphoedema, and pleural effusion. Thorax. 1966;21:247–53. doi: 10.1136/thx.21.3.247. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Cohen PR. Red lunulae: Case report and literature review. J Am Acad Dermatol. 1992;26:292–4. doi: 10.1016/0190-9622(92)70037-g. [DOI] [PubMed] [Google Scholar]
- 34.Lin KM, Cheng TT, Chen CJ. Clinical Applications of Nailfold Capillaroscopy in Different Rheumatic Diseases. [Last accessed on 2014 May 17]. Available from: http://www.tsim.org.tw/journal/jour20-3/07.PDF .
- 35.Inamadar AC, Palit A. Nails: Diagnostic clue to genodermatoses. Indian J Dermatol Venereol Leprol. 2012;78:271–8. doi: 10.4103/0378-6323.95441. [DOI] [PubMed] [Google Scholar]


